Abstract
Background
Radiation-induced necrosis is a complication of brain irradiation. Treatment options are limited.
Methods
The response to treatment with low-dose bevacizumab in 2 patients with radiation-induced necrosis was reported.
Results
Both patients with metastatic melanoma, aged 48 and 51 years, had significant symptomatic and radiological improvement with low-dose bevacizumab treatment. Doses as low as 5 mg/kg every 6 weeks and 7.5 mg/kg i.v. every 4 weeks were used and were highly effective.
Conclusions
Low-dose bevacizumab is a solid option in the management of edema associated with radiation necrosis.
Key words: Radiation-induced necrosis, Bevacizumab, Brain metastasis, Brain irradiation, Melanoma
Introduction
Radiation-induced necrosis is usually a late complication of brain irradiation. Symptoms may vary from focal neurologic deficits to generalized signs [1, 2]. Pathogenesis includes vascular endothelial cell damage that leads to vessel occlusion, resulting in coagulative necrosis and subsequent demyelination [1, 3]. The 3 most important predictors of radiation necrosis are: radiation dose, fractionation, and treatment volume [4]. The diagnosis is often challenging. MRI is usually used to help in the distinction between tumor and radiation necrosis, showing a contrast-enhancing mass with white matter changes and an edema within or adjacent to the site of the original tumor [5]. The mean interval to the onset of necrosis is around 12 months, although radiation necrosis can manifest as early as 3 months [6, 7]. Treatment of this condition is often challenging. Recently, an antibody against vascular endothelial growth factor (bevacizumab) has been reported to play a role in this condition. Informed consent from the patients was obtained.
Case 1
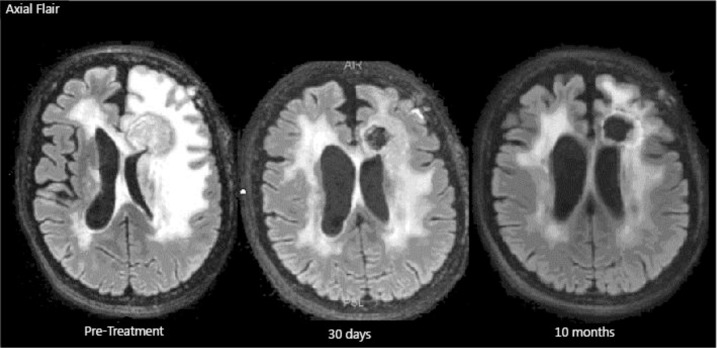
The first case is a 51-year-old woman who was diagnosed with metastatic melanoma in the lungs, with an unknown primary tumor. She underwent left inferior lobectomy. Two years later, the patient developed 3 metastatic brain lesions. The largest lesion was surgically resected. After brain surgery, she was treated with whole-brain radiation and fotemustine. Soon after the radiation had been completed, the other 2 lesions were treated with stereotactic radiosurgery (SRS). After 17 months of SRS, the patient presented with severe drowsiness and was unable to ambulate by herself. An MRI of the brain with perfusion and spectroscopy showed radionecrosis. Therapy with bevacizumab, 5 mg/kg every 2 weeks, associated with dexamethasone, 4 mg p.o. q.i.d., was used, and important clinical benefits were noted after 3 days with a complete reversal of her symptoms. During the following 2 months, dexamethasone was discontinued and the patient remained asymptomatic. After 3 months, the dose and the schedule of bevacizumab was modified to 7.5 mg/kg i.v. every 4 weeks. Seventeen months after the first bevacizumab dose was administered, the patient remained neurologically stable and was able to lead a normal life (fig. 1).
Fig. 1.
FLAIR sequence MRI of patient 1.
Case 2
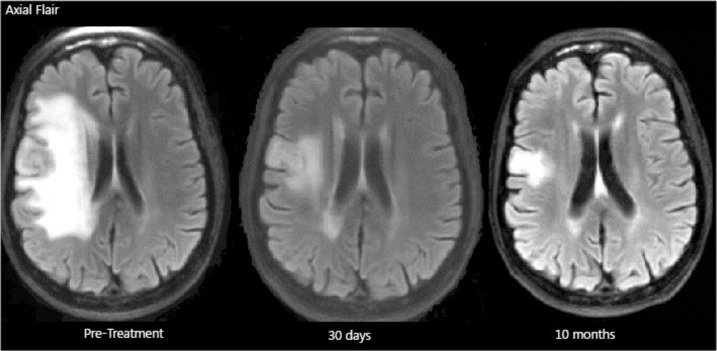
The second case is a 48-year-old woman who was initially diagnosed with cutaneous melanoma on the right deltoid region. Nine years later, she presented with subcutaneous and bone metastasis. She was treated with ipilimumab and achieved a complete systemic response. However, 3 weeks after her fourth dose of ipilimumab, a routine MRI of the brain showed a single brain metastasis. She underwent SRS followed by whole-brain irradiation. Three months later, the patient presented with partial seizures (facial tremor). A brain MRI with perfusion and spectroscopy showed severe vasogenic edema consistent with radionecrosis. A surgical approach to this lesion would have resulted in partial facial paresis; therefore, the patient refused the procedure.
The patient was started on dexamethasone, 4 mg p.o. t.i.d. for 3 months, with a partial seizure control, but during steroid taper, her seizures resumed. She was then started on bevacizumab, 5 mg/kg, with rapid clinical improvement. Due to her financial constraints, bevacizumab was scheduled every 6 weeks. Nonetheless, her symptoms disappeared and a repeat MRI of the brain showed an important reduction of the vasogenic edema (as shown in the FLAIR sequence of her MRI) (fig. 2). After only 4 weeks since starting bevacizumab, dexamethasone was discontinued.
Fig. 2.
FLAIR sequence MRI of patient 2.
Discussion
Radiation necrosis can adversely impact the quality of life as much as the primary disease. Treatment of radiation necrosis can be challenging and traditionally includes surgical decompression and corticosteroids. Side effects of long-term corticosteroid therapy are well-known and some patients do not respond to it in a satisfactory way, so new drugs are necessary to improve the treatment. Recently, bevacizumab, an antibody against vascular endothelial growth factor, has been studied with the intent to reduce edema in patients with radiation necrosis. The study revealed promising results [8, 9].
The literature regarding the use of bevacizumab for the treatment of radiation necrosis is scarce. The studies mainly consist of case reports and a series of cases; issues regarding adequate dosing in this condition are still under debate.
To our knowledge, there are no established doses for the treatment of radionecrosis with bevacizumab; in the studies available, the doses vary from 5 to 7.5 mg/kg every 2 weeks and 7.5 mg/kg every 3 weeks [10, 11, 12]. Since cost and side effects are not negligible, the minimal dose necessary to reduce brain edema is of great interest. In 1 of our cases, we observed a dramatic clinical and radiological response to bevacizumab after a single dose of 5 mg/kg, and therefore we suggest that reduced doses may be very effective for the treatment of radionecrosis. More studies addressing this issue are warranted. The largest series of patients are from a Chinese study which reported the use of bevacizumab therapy administered for a minimum of 2 cycles in 17 patients (7.5 mg/kg, at a 2-week interval); it showed clinical improvement in 10 patients and all 17 were able to reduce the corticosteroid dose [12].
Radiation necrosis can recur even months after bevacizumab treatment is discontinued, and a recent case report showed that retreatment with bevacizumab appears to be effective [12].
To summarize, bevacizumab is a solid option in the edema management associated with radiation necrosis. For the purpose of edema control, it seems that doses as low as 5 mg/kg every 6 weeks may be effective.
Disclosure Statement
The authors declare no conflict of interest.
References
- 1.Burger PC, Boyko OB. Pathology of central nervous system radiation injury. In: Gutin PH, Leibel SA, Sheline GE, editors. Radiation Injury in the Nervous System. New York: Raven Press; 1991. pp. 191–208. [Google Scholar]
- 2.Burger PC, Mahley MS, Jr, Dudka L, Vogel FS. The morphologic effects of radiation administered therapeutically for intracranial gliomas: a postmortem study of 25 cases. Cancer. 1979;44:1256–1272. doi: 10.1002/1097-0142(197910)44:4<1256::aid-cncr2820440415>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 3.Hopewell JW, Wright EA. The nature of latent cerebral irradiation damage and its modification by hypertension. Br J Radiol. 1970;43:161–167. doi: 10.1259/0007-1285-43-507-161. [DOI] [PubMed] [Google Scholar]
- 4.Giglio P, Gilbert MR. Cerebral radiation necrosis. Neurologist. 2003;9:180–188. doi: 10.1097/01.nrl.0000080951.78533.c4. [DOI] [PubMed] [Google Scholar]
- 5.Wara WM, Bauman GS, Sneed PK, et al. Brain, brain stem and cerebellum. In: Perez CA, Brady LW, editors. Principles and Practice of Radiation Oncology. ed 3. Philadelphia: Lippincott-Raven; 1998. pp. 777–828. [Google Scholar]
- 6.Ruben JD, Dally M, Bailey M, et al. Cerebral radiation necrosis: incidence, outcomes, and risk factors with emphasis on radiation parameters and chemotherapy. Int J Radiat Oncol Biol Phys. 2006;65:499–508. doi: 10.1016/j.ijrobp.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 7.Bleyer WA, Griffin TW. White matter necrosis, mineralizing microangiopathy, and intellectual abilities in survivors of childhood leukemia: associations with central nervous system irradiation and methotrexate therapy. In: Gilbert HA, Kagan AR, editors. Radiation Damage to the Nervous System: A Delayed Therapeutic Hazard. New York: Raven Press; 1980. [Google Scholar]
- 8.Torcuator R, Zuniga R, Mohan YS, et al. Initial experience with bevacizumab treatment for biopsy confirmed cerebral radiation necrosis. J Neurooncol. 2009;94:63–68. doi: 10.1007/s11060-009-9801-z. [DOI] [PubMed] [Google Scholar]
- 9.Liu AK, Macy ME, Foreman NK. Bevacizumab as therapy for radiation necrosis in four children with pontine gliomas. Int J Radiat Oncol Biol Phys. 2009;75:1148–1154. doi: 10.1016/j.ijrobp.2008.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Furuse M, Nonoguchi N, Kawabata S, et al. Treatment for symptomatic radiation necrosis diagnosed by amino acid PET. Jpn J Clin Oncol. 2013;43:337. doi: 10.1093/jjco/hys231. [DOI] [PubMed] [Google Scholar]
- 11.Furuse M, Kawabata S, Kuroiwa T, et al. Repeated treatments with bevacizumab for recurrent radiation necrosis in patients with malignant brain tumors: a report of 2 cases. J Neurooncol. 2011;102:471. doi: 10.1007/s11060-010-0333-3. [DOI] [PubMed] [Google Scholar]
- 12.Wang Y, Pan L, Sheng X, et al. Reversal of cerebral radiation necrosis with bevacizumab treatment in 17 Chinese patients. Eur J Med Res. 2012;23:17–25. doi: 10.1186/2047-783X-17-25. [DOI] [PMC free article] [PubMed] [Google Scholar]