Abstract
Background
Intimate partner violence (IPV) around the time of pregnancy is a widespread global health problem with many negative consequences. Nevertheless, a lot remains unclear about which interventions are effective and might be adopted in the perinatal care context.
Objective
The objective is to provide a clear overview of the existing evidence on effectiveness of interventions for IPV around the time of pregnancy.
Methods
Following databases PubMed, Web of Science, CINAHL and the Cochrane Library were systematically searched and expanded by hand search. The search was limited to English peer-reviewed randomized controlled trials published from 2000 to 2013. This review includes all types of interventions aiming to reduce IPV around the time of pregnancy as a primary outcome, and as secondary outcomes to enhance physical and/or mental health, quality of life, safety behavior, help seeking behavior, and/or social support.
Results
We found few randomized controlled trials evaluating interventions for IPV around the time of pregnancy. Moreover, the nine studies identified did not produce strong evidence that certain interventions are effective. Nonetheless, home visitation programs and some multifaceted counseling interventions did produce promising results. Five studies reported a statistically significant decrease in physical, sexual and/or psychological partner violence (odds ratios from 0.47 to 0.92). Limited evidence was found for improved mental health, less postnatal depression, improved quality of life, fewer subsequent miscarriages, and less low birth weight/prematurity. None of the studies reported any evidence of a negative or harmful effect of the interventions.
Conclusions and implications
Strong evidence of effective interventions for IPV during the perinatal period is lacking, but some interventions show promising results. Additional large-scale, high-quality research is essential to provide further evidence about the effect of certain interventions and clarify which interventions should be adopted in the perinatal care context.
Introduction
Intimate partner violence (IPV) is increasingly recognized as a global health problem with crucial societal and clinical implications. IPV affects women and men from all backgrounds, regardless of age, ethnicity, socio-economic status, sexual orientation or religion [1]–[3]. IPV is defined as any behavior within a current or former intimate relationship that causes physical, sexual or psychological harm, including acts of physical aggression, sexual coercion, psychological abuse and controlling behaviors [4]. It is sometimes referred to as domestic/family violence, spouse/partner abuse/assault, battering, violence against women or gender based violence. [4]–[6].
Pregnancy and childbirth are major milestones in the lives of many couples and their families. The transition to parenthood brings joy as well as new challenges to couple relationships [7],[8]. Pregnancy can be a time of particular vulnerability to IPV because of changes in physical, emotional, social and economic demands and needs. This vulnerable period, however, is not limited to the time between conception and birth. Researchers have clearly demonstrated that the risk factors for IPV associated with pregnancy encompass the timeframe of one year before conception until one year after childbirth [3],[9]–[12].
A wide range of prevalence rates, from 3 to 30% of IPV around the time of pregnancy, has been reported. Prevalence rates in African and Latin American countries are mainly situated at the high end of the continuum and the European and Asian countries at the lower end. Although estimates within regions and countries are highly variable, the majority of studies show rates within the range of 3.9% to 8.7% [2],[13]. Most studies focus mainly on physical and/or sexual partner violence, while psychological violence remains difficult to delineate and measure. Although the exact prevalence of IPV around the time of pregnancy remains unclear, it is evident that it affects a substantial group of women. In fact, IPV during the perinatal period is more common than several maternal health conditions (e.g. pre-eclampsia, placenta praevia), nevertheless IPV receives considerably less attention within perinatal care [2],[3],[14],[15].
In recent decades, research from the western world and increasingly from low and middle income countries [16] has generated growing evidence that violence is associated with detrimental effects on the physical and mental health of women, men and children [17]. IPV is associated with adverse pregnancy outcomes such as low birth weight, preterm delivery, infection, miscarriage/abortion, placental abruption, fetal injury and perinatal death. Adverse mental health consequences and behavioral risks including depression, anxiety disorders, post-traumatic stress disorder, suicide (attempts), delayed entry into prenatal care, poor maternal nutrition and use of tobacco, alcohol and illicit drugs are consistently associated with IPV around the time of pregnancy [4],[14],[17]–[29]. Most researchers and caregivers agree that perinatal care is an ideal ‘window of opportunity’ to address IPV, for it is often the only moment in the lives of many couples when there is regular contact with health care providers [2],[30]. There is a growing consensus that routine enquiry is a safe effective practice and an important first step in tackling IPV in general [24],[31]–[35]. Nevertheless, a lot remains unclear about how to deal with IPV in the perinatal care context and which interventions should be adopted.
The objective of this paper is, therefore, to provide a clear overview of the existing evidence on the effectiveness of interventions for IPV for women (and their partners/children if the intervention involves them) during the perinatal period. This review surveys randomized controlled trials (RCTs) of all types of interventions aiming to reduce IPV, and/or enhance physical and/or mental health, Quality Of Life (QOL), safety behavior, help seeking behavior, and social support.
Methods
Search strategy
This systematic literature review was based on an extensive search in the electronic databases PubMed, Web of Science, CINAHL, and the Cochrane Library. The search was limited to peer-reviewed articles reporting results from RCTs published in English from 2000 to 2013. The searches were systematically updated during the writing process, the last update taking place in March 2013. The following search strategy was used in PubMed: “((“violence”[MeSH Terms] OR “violence”[All Fields]) AND (“pregnancy”[MeSH Terms] OR “pregnancy”[All Fields]) AND (“Intervention (Amstelveen)”[Journal] OR “Interv Sch Clin”[Journal] OR “intervention”[All Fields])) AND (Randomized Controlled Trial[ptyp] AND (“2000/01/01”[PDAT] : “2013/12/31”[PDAT]) AND “humans”[MeSH Terms])”. The search strategy for Web of Science was: “Topic = (violence) AND Topic = (pregnancy) Refined by: Topic = (intervention) AND Document Types = (ARTICLE) Timespan = 2000–2013. Databases = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH”.
We started our search in PubMed and applied the same strategy in Web of Science, CINAHL and the Cochrane Library. Reference lists of retrieved articles were checked and relevant articles were added by hand search. The database search was executed by two reviewers (ASVP & AV) independently, findings were discussed and differences resolved.
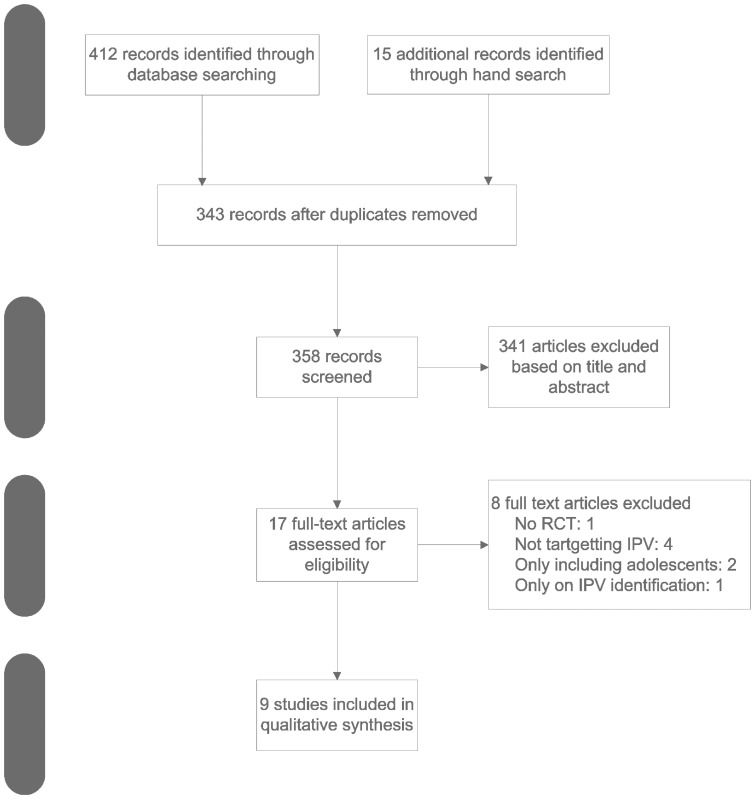
Figure 1 gives a detailed overview of the search strategy.
Figure 1. Search strategy flowchart.
Inclusion criteria
Several criteria for inclusion in the systematic review were applied.
First of all, the type of participants included in the studies for this review were pregnant women of any age and/or women who had given birth in the past year (plus their partners/children if the intervention involved them).
Second, the studies had to aim at evaluating some type of intervention for IPV. Peer-reviewed papers reporting on interventions only addressing non-partner violence, reproductive coercion, child abuse/neglect, parenting, teen pregnancies, substance abuse, and disclosure of IPV were therefore excluded. Publications were also examined to ensure that they did not display the same data set as that displayed in other articles.
Third, the primary outcome of the studies had to be any measure of IPV. The secondary outcomes were physical and/or psychosocial health (e.g. pregnancy and neonatal outcome, depression, anxiety, QOL, substance use, stress), help seeking behavior, safety behavior and social support.
Fourth, we included only published RCTs, regardless of the nature, intensity or duration of the intervention, length of follow-up, or country or setting in which the participants were recruited.
Quality assessment
After full text evaluation, the risk of bias and the quality of the selected studies was assessed by two reviewers (ASVP & AV) separately, based on “The Cochrane Collaboration's tool for assessing risk of bias” [36]. Key domains of this risk of bias assessment were sequence generation, allocation concealment, blinding, incomplete outcome data, selective outcome reporting and ‘other issues’. The reviewers independently assessed risk of bias for each study and classified every study as low, high or unclear risk of bias. Final classifications and inclusion in this review were determined by consensus. For a detailed overview of the quality assessment, see Table 1: Characteristic of the included primary studies.
Table 1. Characteristic of the included primary studies.
| Author, Year, Country | Setting & participants (inclusion/exclusion criteria) | Intervention | Control | Outcomes & follow-up | Risk of bias |
| Bair-Merritt et al., 2010 USA (Hawaii) | 643 families Inclusion criteria: English-speaking mother, infant at high risk for child maltreatment born between November 1994 and December 1995, not involved in child protective services. | IG = 373 families The Healthy Start Program (HSP). consisted of home visits by paraprofessionals providing direct services (promote child health, decrease child maltreatment by improving family functioning and reducing malleable risk factors such as IPV) and linked families to community resources. | CG = 270 families The control group participated in the HSP assessment, baseline and follow-up interviews, but did not partake in the HSP program (usual care). | Interviews with the infant's primary caregiver (mostly mothers): baseline interview one week after birth, follow-up interviews at the child's age of 1, 2, 3, 7, 8 & 9 years. Measures included CTS1 at baseline, CTS2 at follow-up for IPV (always past year perpetration and victimisation of physical, psychological and sexual violence). Mental Health Index (anxiety and depressive symptoms), drug and alcohol use. | Low risk |
| Cripe et al., 2010 Peru | 1035 pregnant women attending antenatal care from January to July 2007 in a national referral hospital. Inclusion criteria: positive on AAS, Spanish-speaking, between 18–45 years old. | IG = 110 Empowerment intervention: abuse assessment, wallet-size referral card (listing agencies providing services to abused women) and social worker case management (this encompasses a 30 minutes supportive counselling session with education and advice in the areas of safety by a trained social worker). | CG = 110 Standard care: abuse assessment and wallet-size referral card. | Screening for IPV: modified AAS (physical/sexual past 12 months) Measures pre-intervention eligibility assessment and interviews between 12 & 26 gestational weeks: IPV (CTS2 past year), health-related QOL (SF-36), adaptation of safety behaviours (safety behaviours checklist), use of community resources (community resources assessment). Post-intervention interviews measures: IPV (CTS2 past year), health-related QOL (SF-36), adaptation of safety behaviours (safety behaviours checklist), use of community resources (community resources assessment). | Unclear risk |
| Curry et al., 2006 USA | 1000 women attending antenatal care recruited between 2001–2003 Inclusion criteria: English-speaking, 13–23 weeks pregnant. | IG = 499 (only 130 women were identified as high risk due to a positive score on the AAS and/or PPP stress scale and received NCM) Referral card, offer to see video ‘Faces of abuse’, 24/7 access to the NCM (individualised care plan providing emotional support, basic needs assessment, assessing safety issues, discussing family concerns and providing education) | CG = 501 (101 women were identified as high risk in the CG) Offer to see video ‘Faces of abuse’. Women in the CG who screened positive for abuse, did not receive any other intervention except for a small resource card (except 10 women with high danger assessment scores). | All participants completed 2 research assessments, one prior to 23 weeks (T1 measures included socio-demographics, AAS and PPP) and one between 32 weeks and delivery (T2 measures included AAS and PPP. | Unclear risk |
| Humphreys et al, 2011 USA | 50 women attending antenatal care from June 2006 to December 2007 Inclusion criteria: English-speaking, 18 years or older, <26 weeks pregnant, not first prenatal visit. | IG = 25 A 15-minutes interactive multimedia intervention (video doctor) and counselling. The intervention contained risk reduction messages simulating an ideal discussion with a prenatal health care provider following key principles of motivational interviewing. Messages were tailored to the participant's risk profile and intention to change. Two documents were printed automatically, cueing sheet with suggestions for counselling statements for providers and educational worksheet for participants. The intervention was designed to reduce their risks related to IPV, smoking, alcohol and illicit drugs. | CG = 25 Baseline risk assessment, no interaction with video doctor, usual clinic care. | Before a regularly scheduled prenatal appointment, participants completed a baseline risk assessment (socio-demographics, pregnancy history & status, tobacco, alcohol, drug use & lifetime IPV)+post-visit interview. Follow-up assessment 1 month after baseline+post-visit interview. IP(or someone important to them) V was measured through AAS (physical/sexual violence year before and since pregnancy). Other outcome measures: patient-provider discussion of IPV and perceived helpfulness. | Unclear risk |
| Kiely et al., 2010 USA | 1044 women attending antenatal care from July 2001 to October 2003 Inclusion criteria: self-identified as minority, at least 18 years old, 28 weeks pregnant or less, Washington resident and English-speaking. | Total IG = 521 of which 169 reported IPV Integrated cognitive behavioural intervention delivered immediately before or after routine prenatal care (2 to 8 sessions of +/−35 minutes & up to 2 postpartum booster sessions) targeting cigarette smoking, environmental tobacco smoke exposure, depression and IPV. The intervention for IPV provided information about the types of abuse the cycle of violence, a danger assessment, and preventive options as well as the development of a safety plan and a list of community resources. | Total CG = 523 of which 167 reported IPV Usual prenatal care | Screening for the 4 risk factors cigarette smoking, environmental tobacco smoke exposure, depression and IPV (AAS for physical/sexual IPV previous year) Baseline interview (+/−9 days after screening): socio-demographics, reproductive history behavioural risks and CTS for frequency of physical/sexual coercion (partner to self) Follow-up telephone interviews 22–26 weeks, 34–38 weeks & 8–10 weeks postpartum: physical/sexual IPV (CTS for baseline & follow-up interviews). Data on pregnancy and neonatal outcomes were extracted from the medical records. | Low risk |
| Olds et al, 2004 USA | 735 women attending antenatal care between March 1994 and June 1995 Inclusion criteria: no previous life births, qualified for Medicaid or no private insurance. | IG2(paraprofessional) = 245 & IG3 (nurse) = 235) The trial consists of 3 arms: control group (treatment 1), treatment 2 (paraprofessional) and treatment 3 (nurse). All arms were provided with free developmental screening and referral for children at 6, 12, 15, 21 and 24 months of age. The home visiting program has 3 broad goals, (1) to improve maternal and fetal health during pregnancy; (2) to improve children's health and development; and (3) to enhance mothers' personal development. The visitors helped women accomplish these goals by promoting adaptive behaviors, by helping them improve their relationships with key family members and friends (especially their mothers and boyfriends), and by promoting women's use of needed health and human services. | CG = 255 Treatment 1 (control): free developmental screening and referral for children at 6, 12, 15, 21 and 24 months of age+usual care. | Baseline interview (gestational age 28 & 36 weeks) and follow-up in-home assessments at 6, 12, 15, 21, 24 and 48 months of child's age 48 months (4 years) assessment (this article): Mothers reported: psychologic resources (women's intelligence, mental health and sense of mastery), number & outcomes subsequent pregnancies, socio-demographics, physical IPV last 2 years/past 6 months (CTS), substance use, behavior problems children. Observation mother-child interactions: home environment assessment of early learning. Children were assessed on behavioral adaptation and emotional regulation. | Unclear risk |
| Taft et al., 2011 Australia | 174 women attending antenatal care from January 2006 to December 2007 Inclusion criteria: 16 years or older, pregnant or at least one child 5 years or younger, English- or Vietnamese speaking, disclosed IPV or were psychosocially distressed (no disclosure IPV but symptoms indicative for abuse), no serious mental illness. | IC = 113 The women in the IC received a resource card and up to 12 months support from non-professional mentor mothers providing: non-judgmental support, assistance in developing safety strategies, a trusting relationship, information and assistance in referral to community services. | CG = 61 Women in the CG received a resource card and usual care. | Baseline & 12 month follow-up questionnaires used the following measures: CAS for IPV (emotional/physical/sexual), EPDS for depression, SF-36 for general health & well-being, PSI-SF for parenting stress, MOS-SF for social support. | Unclear risk |
| Tiwari et al., 2005 Hong Kong | 110 women attending antenatal between May 2002 and July 2003. Inclusion criteria: over 18 and less than 30 weeks pregnant and attending first antenatal appointment. | IC = 55 Empowerment intervention, a 30 minutes one-to-one session (at enrolment) including advice in the areas of safety, choice making, problem solving and empathic understanding. A brochure reinforcing the information was given after the session. | CG = 55 Standard care: a wallet size resource card after enrolment. | Screening: AAS (physical/sexual/emotional-psychological male partner abuse last year) Enrolment: CTS, SF-36 & demographics Telephone follow-up interview 6 weeks postpartum: CTS, SF-36 & EPDS. | Low risk |
| Zlotnick et al., 2010 USA | 54 women attending antenatal care Inclusion criteria: attending prenatal care visit, between 18 and 40 years of age, no DSM-IV Axis 1 disorder. | IC = 28 The intervention consisted of four 60 minutes individual sessions over a 4 week period before delivery and 1 booster session within 2 weeks of delivery. The content of these sessions was based on the principles of interpersonal psychotherapy emphasizing social support. Following topics were a.o. covered healthy/abusive relationships, disputes, resolving interpersonal conflicts stress management skills, safety plan, “baby blues,” and postpartum depression, PTSD, substance use, transition to motherhood, self-care and social support networks. | CG = 26 Standard (medical) care, the educational material and a listing of resources for IPV. | Screening: CTS2 (past year physical/psychological/sexual IPV)and demographics Baseline assessment: current affective disorders, PTSD and substance use (SCID-NP). Assessments administered at intake, 5–6 weeks after intake, 2 weeks after delivery, 3 months postpartum): CTS2 (past year or since the last assessment physical/psychological/sexual), LIFE (assess major depressive disorders and PTSD), EPDS (depression level), Davidson trauma scale (PTSD), criterion A from the PTSD module of the SCID-NP (history of trauma). | Unclear risk |
Legend:
AAS = Abuse Assessment Screen.
CAGE = Cut down, Annoyed, Guilty, Eye-opener (alcoholism screening tool).
CAS = Composite Abuse Scale.
CG = Control Group.
CTS = Conflict Tactics Scale.
CTS2 = revised Conflict Tactics Scale.
EPDS = Edinburgh Postnatal Depression Scale.
IG = Intervention Group.
IRR = Incidence Rate Ratio.
LIFE = Longitudinal Interval Follow-up Examination.
MOS-SF = Medical Outcomes Scale - Short Form.
NCM = Nurse Case Management.
MCS = Mental Components Scores (SF36).
PCS = Physical Components Scores (SF36).
PPP = Prenatal Psychosocial Profile.
PSI-SF = Parenting Stress Index – Short Form.
SCID-NP = Structured Clinical Interview for the DSM-IV Axis Disorders – Nonpatient Version.
SF36 = Short Form Health Survey.
SVAWS = Severity of Violence Against Women Scale.
Data extraction
Using a specially designed data extraction form, the two reviewers independently extracted information from the selected papers. Data items compromised country, setting, sample size & participants, sampling methods, measuring tools, description of the intervention and control group(s), outcomes, and follow-up period. Authors were contacted if additional information was required.
Initially, we planned a meta-analysis to quantify and compare the interventions identified. Unfortunately it was not feasible to perform a meta-analysis due to the limited amount of data and the large variation in interventions, outcome measures and measurement time points.
The PRISMA guidelines were used as a framework for this review [37].
Results
Through our electronic database search, we retrieved 412 potentially relevant articles based on keywords and limits set (60 in PubMed, 343 in Web of Science, seven in CINAHL and two in the Cochrane database). Fifteen additional articles were identified through hand search. After title and abstract evaluation, 69 duplicates were removed, leaving 343 to be included in the next step. Thereafter, out of 358 articles (343+15 articles retrieved through hand search) screening resulted in 17 articles deemed eligible for more detailed evaluation. After full text evaluation another eight were excluded because they did not meet the inclusion criteria, leaving nine studies submitted to critical appraisal and included in this systematic review [17],[38]–[45]. Details on setting/participants, intervention/control activities and outcomes are given in Table 1: Characteristic of the included primary studies.
Out of these nine studies, six were conducted in the USA, one in Peru, one in Australia, and one in China. All studies recruited participants through hospital-based antenatal care, with sample sizes ranging from 50 to 1054 women.
Three studies measured the impact of a home visitation program involving paraprofessionals (non-professionals trained to do the home visits and deliver the intervention), mentor mothers (lay mothers trained to do the home visits, provide peer support and mentoring), and/or nurses and followed participants for between one up to nine years.
The six other studies evaluated the effect of some form of supportive counseling, varying from one 30-minute session up to six 60-minutes sessions or 24/7 access to a Nurse Case Manager (NCM). Most (n = 6) of the interventions were specifically designed to target IPV as the main objective, but some (n = 3) were part of a larger, multifaceted intervention in which IPV was one of the targets parallel to e.g. smoking, depression, child health, parenting. All studies compared the intervention to usual or standard care, which, due to ethical considerations, generally implied that patients were provided a referral card or a list of community resources.
Throughout the rest of this paper the term IPV will be used to refer to the combination of physical and sexual and psychological partner violence, unless specified otherwise.
Home visitation programs
Primary outcome
After three years of program implementation Bair-Merritt et al. [41] found that, intervention women reported a lower, albeit statistically marginally non-significant, adjusted rate of IPV victimization [Incidence Rate Ratio (IRR) 0.86, 95% CI, 0.73–1.01] and a significantly lower rate of perpetration (IRR 0.83, 95% CI, 0.72–0.96) than the control group. Intervention women showed significantly lower rates of physical assault victimization (IRR 0.85; 95% CI, 0.71–1.00) and significantly lower perpetration (IRR 0.82, 95% CI, 0.70–0.96). Although rates of overall IPV victimization and perpetration were also lower after 9 years, these results were not statistically significant. In other words, perpetration rates decreased significantly and victimization rates showed a trend towards decrease after three years, but not after nine years.
Olds et al. [44] found on the one hand, no adjusted statistically significant effects of paraprofessional visits on the experience of physical partner violence in the intervention group (IG) versus the control group (CG) (14.2% vs. 13.6%, P = 0.88, OR 1.05, 95% CI not reported) in the six months prior to four year follow-up. On the other hand, nurse-visited women did report (6.9% vs. 13.6%, P = 0.05, OR 0.47, 95% CI not reported) a significant decrease in physical partner violence.
Taft et al. [39] reported evidence of a true difference in mean abuse scores at 12 months follow-up (15.9 vs. 21.8, AdjDiff −8.67, 95% CI, −16.2–−1.15, P = 0.03).
Secondary outcomes
In the study of Olds et al. [44], women visited by paraprofessionals reported a statistically significant greater sense of mastery (101.25 vs. 99.31, P = 0.03) and better mental health (101.21 vs. 99.16, P = 0.03) than control subjects, had fewer subsequent miscarriages (6.6% vs. 12.3%, P = 0.04, OR 0.5, 95% CI not reported), and fewer low birth weight newborns (2.8% vs. 7.7%, P = 0.03, OR 0.34, 95% CI not reported). There were no statistically significant effects of nurse visits on these variables
Taft et al. [39] reported a trend favoring the intervention regarding depression (19/85 vs 14/43; AdjOR 0.42, 95% CI 0.17–1.06), physical wellbeing mean scores (AdjDiff 2.79, 95% CI, 0.40–5.99), and mental wellbeing mean scores (AdjDiff 2.26; 95% CI, 1.48–6) but no observed effect on parenting stress.
Supportive counseling
Primary outcome
The women in the intervention group of Kiely et al. [40] experienced statistically significant fewer recurrent episodes of IPV during pregnancy and postpartum than women receiving usual care (adjOR 0.48, 95% CI, 0.29–0.80). Those with minor IPV were significantly less likely to experience further episodes during pregnancy (first follow-up 22–26 gestational weeks OR 0.48, 95% CI, 0.26–0.86; second follow-up 34–38 gestational weeks OR 0.53, 95% CI, 0.28–0.99) and postpartum (OR 0.56, 95% CI, 0.34–0.93). Those with severe IPV showed significantly reduced episodes only during postpartum (OR 0.39, 95% CI, 0.18–0.82). Women experiencing physical IPV showed a significant reduction in such violence at the first follow-up (OR 0.49, 95% CI, 0.27–0.91) and postpartum (OR 0.47, 95% CI, 0.27–0.82). For sexual IPV the intervention did not significantly reduce episodes of violence at any point in time.
Tiwari et al. [45] reported statistically significant less psychological [Mean Difference (MD) −1.1, 95% CI, −2.2 to −0.04)] (but not sexual) abuse and significantly less minor (MD −1.0, 95% CI, −1.8 to −0.17) (but not severe) physical violence in the intervention group.
Cripe et al. [17] reported no statistically significant differences in the occurrence of IPV between the intervention and control groups after an empowerment counseling session.
Curry et al. [42] did not report any results on IPV, nor were the authors able to provide the IPV data we requested.
Humphreys et al. [43] found no statistically significant differences in prevalence of physical and/or sexual partner violence between the two groups at baseline and did not report partner violence after intervention.
The intervention by Zlotnick et al. [38] did not significantly reduce the likelihood of IPV during pregnancy or up to three months postpartum.
Secondary outcomes
Women in the IG of Kiely et al. [40] had significantly fewer very preterm neonates (1.5% vs. 6.6%, P = 0.03) and an increased mean gestational age (38.2±3.3 vs. 36.9±5.9, P = 0.016).
Tiwari et al. [45] reported significantly higher physical functioning in health related QOL (MD 10, 95% CI, 2.5–1.8) and a significant reduction of role limitation due to physical problems (MD 19, 95% CI, 1.5–37) and emotional problems (MD 28, 95% CI, 9.0–5.0). There was, however, also more bodily pain in this group (MD −1.3, 95% CI, −23–−2.2). Significantly fewer women in the IG reported postnatal depression at follow-up (RR 0.36, 95% CI, 0.15–0.88).
Curry et al. [42] found no statistically significant decrease of total stress scores between the two groups, although total stress scores of both intervention and control women significantly decreased (P<0.001) between follow-up periods.
The intervention by Zlotnick et al. [38] did not significantly reduce the likelihood of a major depressive episode or post traumatic stress disorder (PTSD). They found a trend towards decrease during pregnancy but not during postpartum.
Cripe et al. [17] found a trend towards improved QOL, safety and help seeking behaviors (church and police) in the IG, but no statistically significant differences between the two groups.
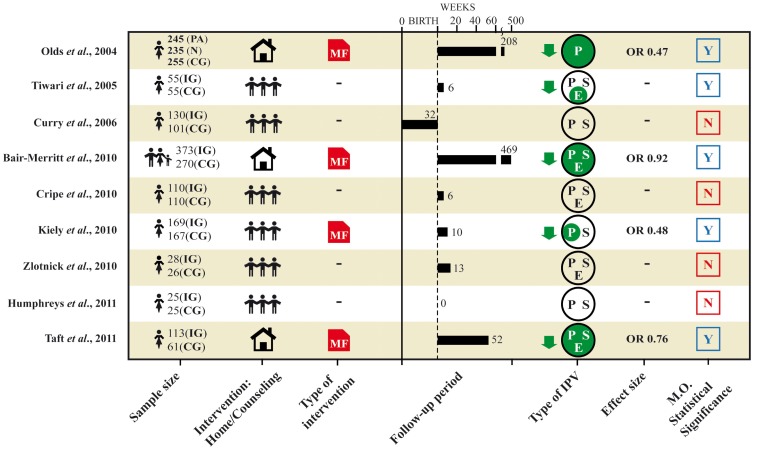
The following figure 2 gives illustrates the correlations between the type of intervention and the impact on the reduction of IPV.
Figure 2. Overview results.
PA = Paraprofessional. N = Nurse. IG = Intervention Group. CG = Control Group. MF = Multifaceted intervention. P = Physical. S = Sexual. E = Emotional. M.O. statistical significance = statistical significant results of measured primary outcome.
Discussion
The results of our systematic review demonstrate that there are few RCTs evaluating interventions for IPV during the perinatal period. Moreover, the overall quality of the nine studies identified is limited and did not produce strong evidence that certain interventions are effective. This finding is also endorsed by Jahanfar et al. [46]. The evidence of IPV interventions outside the context of pregnancy remains similarly insufficient and inconclusive 24,[31],[47]–[49].
Nevertheless, five out of nine studies in our review reported a statistically significant decrease in some form of IPV (odds ratios from 0.47 to 0.92). The most promising results identified by this review are to be found in the home visitation programs and multifaceted counseling-interventions. The three studies [39],[41],[44] on home visitation programs all showed a statistically significant decrease in IPV victimization (and one in perpetration). However, although Olds et al. [44] noted a significant decrease in physical IPV for the nurse-visited women, this was not found for the paraprofessional-visited women. The authors attributed this finding to an increased emphasis among the nurses on partner violence, but it remains unclear if this was really the case. With regard to the secondary outcomes, Olds [44] reported significantly better mental health, fewer subsequent miscarriages and low birth weight newborns in the paraprofessional-visited but not in the nurse-visited women. The different impact of nurses and paraprofessionals raises questions about the mechanisms through which the interventions affected the outcomes.
It is interesting to note that out of six studies evaluating different types of supportive counseling, only two reported a statistically significant effect of the intervention on IPV. First, the high-quality study by Kiely et al. [40] found that their cognitive behavioral intervention significantly reduced recurrent episodes of IPV (except for sexual IPV). Second, Tiwari et al. [45] reported significantly less psychological and minor physical (except for sexual IPV) violence in the intervention group. Sexual partner violence seems to be a form of violence that is difficult to influence. The other four studies [17],[38],[42],[43] did not find a significant difference in IPV between the intervention and control groups. Concerning secondary outcomes, Kiely et al. [40] observed significantly fewer very preterm neonates and an increased mean gestational age in the intervention group. Tiwari et al. [45] reported significantly fewer women with postnatal depression and improved QOL in the intervention group.
None of the studies reported any evidence of a negative or harmful effect of interventions, although only one study [43] mentioned assessing potential harms caused by intervention.
The results should be interpreted with caution and within the light of serious methodological challenges. Researching violence is inherently associated with numerous ethical and safety issues, making it very difficult to produce strong evidence. We identified considerable variation in categorizing certain behavior as IPV, research settings, study populations, sample sizes, content of the intervention, and length of follow-up. Intrinsic to the difficulties associated with the study subject sample sizes are small, there is a considerable loss to follow-up, and it is impossible to blind respondents. Moreover, few studies adjusted their analysis for confounding factors (e.g. childhood abuse), which can create an oversimplified image of reality. However, it should be remembered that lack of statistically significant results does not necessarily imply clinical irrelevance. Some interventions might be effective but not have reached significance level due to methodological and/or ethical challenges.
It is striking that five out of the nine studies reported decreases in IPV after a certain point in time but that these decreases did not significantly differ between intervention and control groups. Apparently, with time (certain) wounds heal. However, other explanations can also be hypothesized.
First, as far as we know, in all the studies reviewed, identifying IPV was not part of routine perinatal care but an additional research-related activity (also known as the Hawthorne-effect) [31],[34]. Asking IPV-related questions to women in the control group, mostly in combination with handing out a referral card could have had a larger impact than assumed. McFarlane et al. [30] found that “simple assessment of abuse and offering referrals has the potential to interrupt and prevent recurrence of IPV”. In other words it is possible that the ‘intervention’ in the control group is more effective than anticipated and therefore no clear difference between the two groups is detected.
Second, it seems reasonable to question the legitimacy of using IPV as a main outcome measure. Given the complexity of intervening factors between identification and IPV reduction (with many not under the control of health care providers), interventions should not necessarily be expected to decrease IPV [35]. Internal changes (mental health, QOL, …) are potentially more informative for evaluating the impact of an intervention for IPV. Significant changes in active or passive experiences of violence may not be observable for some time [5],[47],[48],[50]. At the time of measurement, respondents might simply not acknowledge the violence, or be ready to make changes or accept help. Some counseling interventions (developing safety plans, seeking help, …) might come too early and/or are not adapted to specific needs and therefore prove ineffective [51],[52]. In this review, we identified only one study [43] that included some measure of ‘readiness to change’ which might have contributed to the lack of significant results.
Furthermore, our systematic review yielded only one study [41] reporting both maternal victimization and perpetration behavior, in which there is the striking observation that the rate of perpetration acts in women was twice as high as the victimization acts in both intervention and control groups (at baseline). The intervention seemed to reduce mainly maternal perpetration behavior, but paternal victimization nor perpetration behavior was not directly measured. This finding adds to the debate on gender symmetry in the perpetration of violence and the discussion about over-disclosure by women and under-disclosure by men. Yet, pregnant women's use of violence is virtually ignored by most authors [3]. Moreover, Hellmuth et al. [53] found that IPV perpetration during pregnancy and/or postpartum is associated with negative health outcomes. Therefore, measuring only subjection to violence as a measure of effectiveness of an intervention seems quite insufficient. More attention should be given to outcome measures reflecting the complex process of changing destructive interaction dynamics.
We are aware that this systematic review has several limitations. The choice of databases, inclusion criteria, risk of bias assessment, and interpretation of results all required the individual judgment of the authors. We took various steps to minimize bias at all stages of the review process, but a different review team may not fully agree with our assessment.
Conclusion
This systematic review indicates that strong evidence of effective interventions for IPV during the perinatal period is lacking. Nonetheless, home visitation programs and some multifaceted counseling interventions produced promising results. It is obvious that additional large-scale, high-quality research (with meta-analysis) is essential to tackle the remaining questions and provide further evidence about the effect of certain interventions. Future research should focus on several levels simultaneously (individual, relations, community, and society). Intervening in a single risk factor may be unsuccessful because other risk factors may persist as barriers to the desired change. Readiness to change, help seeking strategies and the complex mutuality of IPV should be taken into account. Serious thought should be given to appropriate outcome measures and to including process indicators in evaluating effectiveness.
Supporting Information
PRISMA checklist.
(PDF)
Acknowledgments
We would like to thank prof. dr. Olivier Degomme for the methodological support, dr Simukai Shamu, Ines Keygnaert, dr. Kristien Michielsen and prof. dr. Kristien Roelens for their useful comments and prof. dr. Michael B. Drennan for the graphic support.
Funding Statement
ASVP received a PhD bursary for her studies from the Research Foundation Flanders (www.fwo.be, grant number 69579). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Daoud N, Urquia ML, O'Campo P, Heaman M, Janssen PA, et al. (2012) Prevalence of abuse and violence before, during, and after pregnancy in a national sample of Canadian women. Am J Public Health 102: 1893–1901 10.2105/AJPH.2012.300843 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Devries KM, Kishor S, Johnson H, Stockl H, Bacchus LJ, et al. (2010) Intimate partner violence during pregnancy: analysis of prevalence data from 19 countries. Reprod Health Matters 18: 158–170 S0968-8080(10)36533-5 [pii]; 10.1016/S0968-8080(10)36533-5 [doi]. [DOI] [PubMed] [Google Scholar]
- 3. Taillieu TL, Brownridge DA (2010) Violence against pregnant women: Prevalence, patterns, risk factors, theories, and directions for future research. Aggression and Violent Behavior 15: 14–35. [Google Scholar]
- 4. Krug EG, Mercy JA, Dahlberg LL, Zwi AB (2002) The world report on violence and health. Lancet 360: 1083–1088. [DOI] [PubMed] [Google Scholar]
- 5. Hegarty KL, Gunn JM, O'Doherty LJ, Taft A, Chondros P, et al. (2010) Women's evaluation of abuse and violence care in general practice: a cluster randomised controlled trial (weave). Bmc Public Health 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Garcia-Moreno C, Heise L, Jansen HAFM, Ellsberg M, Watts C (2005) Public health - Violence against women. Science 310: 1282–1283. [DOI] [PubMed] [Google Scholar]
- 7. Fisher J, de Mello MC, Patel V, Rahman A, Tran T, et al. (2012) Prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: a systematic review. Bulletin of the World Health Organization 90: 139–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kan ML, Feinberg ME (2010) Measurement and Correlates of Intimate Partner Violence Among Expectant First-Time Parents. Violence and Victims 25: 319–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Saltzman LE, Johnson CH, Gilbert BC, Goodwin MM (2003) Physical abuse around the time of pregnancy: an examination of prevalence and risk factors in 16 states. Matern Child Health J 7: 31–43. [DOI] [PubMed] [Google Scholar]
- 10. Jasinski JL (2004) Pregnancy and domestic violence: a review of the literature. Trauma Violence Abuse 5: 47–64 10.1177/1524838003259322 [doi] [DOI] [PubMed] [Google Scholar]
- 11. Charles P, Perreira KM (2007) Intimate partner violence during pregnancy and 1-year post-partum. Journal of Family Violence 22: 609–619. [Google Scholar]
- 12. Martin SL, Harris-Britt A, Li Y, Moracco KE, Kupper LL, et al. (2004) Changes in intimate partner violence during pregnancy. Journal of Family Violence 19: 201–210. [Google Scholar]
- 13. Roelens K, Verstraelen H, Van EK, Temmerman M (2008) Disclosure and health-seeking behaviour following intimate partner violence before and during pregnancy in Flanders, Belgium: a survey surveillance study. Eur J Obstet Gynecol Reprod Biol 137: 37–42 S0301-2115(07)00222-9 [pii]; 10.1016/j.ejogrb.2007.04.013 [doi] [DOI] [PubMed] [Google Scholar]
- 14. Chambliss LR (2008) Intimate partner violence and its implication for pregnancy. Clinical Obstetrics and Gynecology 51: 385–397. [DOI] [PubMed] [Google Scholar]
- 15. Bacchus L, Mezey G, Bewley S (2004) Domestic violence: prevalence in pregnant women and associations with physical and psychological health. European Journal of Obstetrics Gynecology and Reproductive Biology 113: 6–11. [DOI] [PubMed] [Google Scholar]
- 16. Shamu S, Abrahams N, Temmerman M, Musekiwa A, Zarowsky C (2011) A Systematic Review of African Studies on Intimate Partner Violence against Pregnant Women: Prevalence and Risk Factors. Plos One 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cripe SM, Sanchez SE, Sanchez E, Quintanilla BA, Alarcon CH, et al. (2010) Intimate Partner Violence During Pregnancy: A Pilot Intervention Program in Lima, Peru. Journal of Interpersonal Violence 25: 2054–2076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Rose L, Bhandari S, Marcantonio K, Bullock L, Sharps P (2010) Impact of Family and Personal History of Abused Pregnant Women on Their Coping With Current Intimate Partner Violence. International Journal of Qualitative Methods 9: 382–383. [Google Scholar]
- 19. Johnson JK, Haider F, Ellis K, Hay DM, Lindow SW (2003) The prevalence of domestic violence in pregnant women. Bjog-An International Journal of Obstetrics and Gynaecology 110: 272–275. [PubMed] [Google Scholar]
- 20. Taft AJ, Small R, Hegarty KL, Lumley J, Watson LF, et al. (2009) MOSAIC (MOthers' Advocates In the Community): protocol and sample description of a cluster randomised trial of mentor mother support to reduce intimate partner violence among pregnant or recent mothers. Bmc Public Health 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Campbell JC (2001) Abuse during pregnancy: a quintessential threat to maternal and child health - so when do we start to act? Canadian Medical Association Journal 164: 1578–1579. [PMC free article] [PubMed] [Google Scholar]
- 22. Gazmararian JA, Lazorick S, Spitz AM, Ballard TJ, Saltzman LE, et al. (1996) Prevalence of violence against pregnant women. JAMA 275: 1915–1920. [PubMed] [Google Scholar]
- 23. Silverman JG, Decker MR, Reed E, Raj A (2006) Intimate partner violence victimization prior to and during pregnancy among women residing in 26 US states: Associations with maternal and neonatal health. American Journal of Obstetrics and Gynecology 195: 140–148. [DOI] [PubMed] [Google Scholar]
- 24. Bailey BA (2010) Partner violence during pregnancy: prevalence, effects, screening, and management. Int J Womens Health 2: 183–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rodrigues T, Rocha L, Barros H (2008) Physical abuse during pregnancy and preterm delivery. American Journal of Obstetrics and Gynecology 198. [DOI] [PubMed] [Google Scholar]
- 26. Coker AL, Sanderson M, Dong B (2004) Partner violence during pregnancy and risk of adverse pregnancy outcomes. Paediatric and Perinatal Epidemiology 18: 260–269. [DOI] [PubMed] [Google Scholar]
- 27. Mechanic MB, Weaver TL, Resick PA (2008) Mental health consequences of intimate partner abuse: a multidimensional assessment of four different forms of abuse. Violence Against Women 14: 634–654 14/6/634 [pii]; 10.1177/1077801208319283 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Dunn LL, Oths KS (2004) Prenatal predictors of intimate partner abuse. Jognn-Journal of Obstetric Gynecologic and Neonatal Nursing 33: 54–63. [DOI] [PubMed] [Google Scholar]
- 29. Bacchus L, Mezey G, Bewley S (2004) Domestic violence: prevalence in pregnant women and associations with physical and psychological health. European Journal of Obstetrics Gynecology and Reproductive Biology 113: 6–11. [DOI] [PubMed] [Google Scholar]
- 30. McFarlane JM, Groff JY, O'Brien JA, Watson K (2006) Secondary prevention of intimate partner violence - A randomized controlled trial. Nursing Research 55: 52–61. [DOI] [PubMed] [Google Scholar]
- 31. Nelson HD, Bougatsos C, Blazina I (2012) Screening Women for Intimate Partner Violence: A Systematic Review to Update the US Preventive Services Task Force Recommendation. Annals of Internal Medicine 156: 796–+. [DOI] [PubMed] [Google Scholar]
- 32. O'Reilly R, Beale B, Gillies D (2010) Screening and intervention for domestic violence during pregnancy care: a systematic review. Trauma Violence Abuse 11: 190–201 1524838010378298 [pii]; 10.1177/1524838010378298 [doi] [DOI] [PubMed] [Google Scholar]
- 33. Hegarty K, O'Doherty L, Taft A, Chondros P, Brown S, et al. (2013) Screening and counselling in the primary care setting for women who have experienced intimate partner violence (WEAVE): a cluster randomised controlled trial. Lancet 382: 249–258 S0140-6736(13)60052-5 [pii]; 10.1016/S0140-6736(13)60052-5 [doi] [DOI] [PubMed] [Google Scholar]
- 34. Spangaro JM, Zwi AB, Poulos RG, Man WY (2010) Who tells and what happens: disclosure and health service responses to screening for intimate partner violence. Health Soc Care Community 18: 671–680 HSC943 [pii]; 10.1111/j.1365-2524.2010.00943.x [doi] [DOI] [PubMed] [Google Scholar]
- 35. O'Campo P, Kirst M, Tsamis C, Chambers C, Ahmad F (2011) Implementing successful intimate partner violence screening programs in health care settings: Evidence generated from a realist-informed systematic review. Social Science & Medicine 72: 855–866. [DOI] [PubMed] [Google Scholar]
- 36.Higgings JPT ADe (2013) Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S (editors). Cochrane handbook for systematic reviews of interventions version 5.0.1. (updated September 2008).
- 37. Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Journal of Clinical Epidemiology 62: 1006–1012. [DOI] [PubMed] [Google Scholar]
- 38. Zlotnick C, Capezza NM, Parker D (2011) An interpersonally based intervention for low-income pregnant women with intimate partner violence: a pilot study. Archives of Womens Mental Health 14: 55–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Taft AJ, Small R, Hegarty KL, Watson LF, Gold L, et al. (2011) Mothers' AdvocateS In the Community (MOSAIC)-non-professional mentor support to reduce intimate partner violence and depression in mothers: a cluster randomised trial in primary care. Bmc Public Health 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Kiely M, El-Mohandes AAE, El-Khorazaty MN, Gantz MG (2010) An Integrated Intervention to Reduce Intimate Partner Violence in Pregnancy A Randomized Controlled Trial. Obstetrics and Gynecology 115: 273–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Bair-Merritt MH, Jennings JM, Chen RS, Burrell L, McFarlane E, et al. (2010) Reducing Maternal Intimate Partner Violence After the Birth of a Child A Randomized Controlled Trial of the Hawaii Healthy Start Home Visitation Program. Archives of Pediatrics & Adolescent Medicine 164: 16–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Curry MA, Durham L, Bullock L, Bloom T, Davis J (2006) Nurse case management for pregnant women experiencing or at risk for abuse. Jognn-Journal of Obstetric Gynecologic and Neonatal Nursing 35: 181–192. [DOI] [PubMed] [Google Scholar]
- 43. Humphreys J, Tsoh JY, Kohn MA, Gerbert B (2011) Increasing Discussions of Intimate Partner Violence in Prenatal Care Using Video Doctor Plus Provider Cueing: A Randomized, Controlled Trial. Womens Health Issues 21: 136–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Olds DL, Robinson J, Pettitt L, Luckey DW, Holmberg J, et al. (2004) Effects of home visits by paraprofessionals and by nurses: Age 4 follow-up results of a randomized trial. Pediatrics 114: 1560–1568. [DOI] [PubMed] [Google Scholar]
- 45. Tiwari A, Leung WC, Leung TW, Humphreys J, Parker B, et al. (2005) A randomised controlled trial of empowerment training for Chinese abused pregnant women in Hong Kong. Bjog-An International Journal of Obstetrics and Gynaecology 112: 1249–1256. [DOI] [PubMed] [Google Scholar]
- 46. Jahanfar S, Janssen PA, Howard LM, Dowswell T (2013) Interventions for preventing or reducing domestic violence against pregnant women. Cochrane Database of Systematic Reviews [DOI] [PubMed] [Google Scholar]
- 47. Ramsay J, Carter Y, Davidson L, Dunne D, Eldridge S, et al. (2009) Advocacy interventions to reduce or eliminate violence and promote the physical and psychosocial well-being of women who experience intimate partner abuse (Review). Cochrane Database of Systematic Reviews [DOI] [PubMed] [Google Scholar]
- 48. Wathen CN, MacMillan HL (2003) Interventions for violence against women - Scientific review. Jama-Journal of the American Medical Association 289: 589–600. [DOI] [PubMed] [Google Scholar]
- 49. Ludermir AB, Lewis G, Valongueiro SA, de Araujo TVB, Araya R (2010) Violence against women by their intimate partner during pregnancy and postnatal depression: a prospective cohort study. Lancet 376: 903–910. [DOI] [PubMed] [Google Scholar]
- 50. MacMillan HL, Wathen CN, Jamieson E, Boyle MH, Shannon HS, et al. (2009) Screening for Intimate Partner Violence in Health Care Settings A Randomized Trial. Jama-Journal of the American Medical Association 302: 493–501. [DOI] [PubMed] [Google Scholar]
- 51. Zink T, Elder N, Jacobson J, Klostermann B (2004) Medical management of intimate partner violence considering the stages of change: Precontemplation and contemplation. Annals of Family Medicine 2: 231–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Fanslow JL, Robinson EM (2010) Help-Seeking Behaviors and Reasons for Help Seeking Reported by a Representative Sample of Women Victims of Intimate Partner Violence in New Zealand. Journal of Interpersonal Violence 25: 929–951. [DOI] [PubMed] [Google Scholar]
- 53. Hellmuth JC, Gordon KC, Stuart GL, Moore TM (2013) Risk factors for intimate partner violence during pregnancy and postpartum. Archives of Womens Mental Health 16: 19–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA checklist.
(PDF)