Abstract
Aims
Regular exercise as an effective non-pharmacological antihypertensive therapy is beneficial for prevention and control of hypertension, but the central mechanisms are unclear. In this study, we hypothesized that chronic exercise training (ExT) delays the progression of hypertension and attenuates cardiac hypertrophy by up-regulating anti-inflammatory cytokines, reducing pro-inflammatory cytokines (PICs) and restoring the neurotransmitters balance in the hypothalamic paraventricular nucleus (PVN) in young spontaneously hypertensive rats (SHR). In addition, we also investigated the involvement of nuclear factor-κB (NF-κB) p65 and NAD(P)H oxidase in exercise-induced effects.
Methods and results
Moderate-intensity ExT was administrated to young normotensive Wistar-Kyoto (WKY) and SHR rats for 16 weeks. SHR rats had a significant increase in mean arterial pressure and cardiac hypertrophy. SHR rats also had higher levels of glutamate, norepinephrine (NE), phosphorylated IKKβ, NF-κB p65 activity, NAD(P)H oxidase subunit gp91phox, PICs and the monocyte chemokine protein-1 (MCP-1), and lower levels of gamma-aminobutyric acid (GABA) and interleukin-10 (IL-10) in the PVN. These SHR rats also exhibited higher renal sympathetic nerve activity (RSNA), and higher plasma levels of PICs, and lower plasma IL-10. However, ExT ameliorates all these changes in SHR rats.
Conclusion
These findings suggest that there are the imbalances between excitatory and inhibitory neurotransmitters and between pro- and anti-inflammatory cytokines in the PVN of SHR rats, which at least partly contributing to sympathoexcitation, hypertension and cardiac hypertrophy; chronic exercise training attenuates hypertension and cardiac hypertrophy by restoring the balances between excitatory and inhibitory neurotransmitters and between pro- and anti-inflammatory cytokines in the PVN; NF-κB and oxidative stress in the PVN may be involved in these exercise-induced effects.
Introduction
It is well-known that hypertension is a major risk factor for cardiovascular diseases. Hypertension is a chronic inflammatory state, and cardiac dysfunction and hypertrophy are prevalent in hypertensive patients and animals. A great deal of evidence shows that pro-inflammatory cytokines (PICs) are involved in the hypertensive effect and of prognostic significance [1], [2]. In addition, imbalance neurotransmitters activities in the PVN and excess amount of free radicals are both observed in hypertension and contribute to the progression of hypertension. More importantly, there is an interaction between neurotransmitters and PICs and positive feedback mechanism among PICs, enhanced oxidative stress in the PVN which play a key role in sympathetic regulation of blood pressure [3], [4]. So we hypothesized that the interaction among these factors may be closely associated with the central mechanisms of hypertension.
Exercise training (ExT) has been considered as a non-pharmacological therapeutic strategy substitute for hypertensive patients and recommended by a number of organizations and agencies. A growing body of evidence indicates that ExT helps to improve the quality of life in patients with hypertension [5], [6]. Recent work provides evidences about the anti-hypertensive effect of ExT such as attenuating sympathoexcitation and peripheral levels of PICs and NE [4], [7], [8], but the exact central mechanisms are still unknown.
The present study was undertaken to determine whether ExT delays progression of hypertension and attenuates cardiac hypertrophy in spontaneously hypertensive rats by restoring the balances between the excitatory and inhibitory neurotransmitters and between pro- and anti-inflammatory cytokines in the PVN. Our findings provide further evidence and insight for the role of ExT on hypertension and cardiac hypertrophy.
Materials and Methods
Ethics Statement
All animal experimental procedures in this study were approved by the Animal Care and Use Committees of Xi’an Jiaotong University and were conducted in accordance with the US National Institutes of Health Guide for the Care and Use of Laboratory Animals.
Animals and General Experimental Protocol
The 7 week old male normotensive Wistar-Kyoto (WKY) and spontaneously hypertensive rats (SHR) were used in this study. The WKY and SHR rats were separated into the sedentary group (SHYsed and WKYsed) and the exercise group (SHRex and WKYex) at random [4]. Rats in exercise groups were subjected to moderate-intensity exercise (about 60% of maximal aerobic velocity, 5 days per week, 60 min per day at 18 m/min, 0o inclination) on a motor-driven treadmill continuously for a period of 16 weeks [4].
Measurement of Mean Arterial Pressure
Blood pressure was determined by a tail-cuff occlusion method [9]. Rats were allowed to habituate to this procedure for 3 days prior to each experiment. Blood pressure values were averaged from six consecutive cycles per day obtained from each rat.
Collection of Blood and Tissue Samples
Rats were decapitated under anesthesia, and then trunk blood and tissue samples were collected. The PVN tissue was isolated following Palkovits’s microdissection procedure as previously described [10], [11]. Plasma and tissue samples were stored at −80°C until assayed.
Measurement of PVN Tissue Levels of Glutamate, GABA and NE
PVN tissue levels of NE, glutamate and GABA were measured using high-performance liquid chromatography with electrochemical detection (HPLC-EC) as previously described [10]–[13].
Immunohistochemical Studies
Transverse sections from brains were obtained from the region approximately 1.80 mm from the bregma. Immunohistochemical labeling was performed in floating sections as described previously [11] to identify phosphorylated IKKβ positive neurons and NAD(P)H oxidase subunit gp91phox expression in the PVN. For each animal, the positive neurons within the bilateral borders of the PVN were manually counted in three consecutive sections and an average value was reported.
Quantification of NF-κB p65 Activity in the PVN
The NF-κB/p65 Active ELISA (Active Motif, USA) kit was used to measure the binding activity of free NF-κB p65 in nuclear extracts using a sandwich ELISA method according to the manufacturer’s instructions.
Biochemical Assays
The levels of IL-1β, IL-6 and IL-10 in plasma and the levels of TNF-α, IL-1β, IL-6 in PVN tissues were quantified using commercially available rat ELISA kits (Invitrogen) according to manufacturer’s instructions.
Real-time PCR
Real time PCR amplification reactions were performed to detect the mRNA expression of atrial natriuretic peptide in the left ventricular tissue of the heart, and the mRNA expressions of IL-10 and the MCP-1 in the PVN, as previously described [10], [14]. Data were normalized to GAPDH expression.
Electrophysiological Recording
Renal sympathetic nerve activity (RSNA) was recorded. The general methods for recording and analyzing RSNA have been described previously [15], [16].
Statistical Analysis
All data were analyzed by ANOVA followed by a post-hoc Tukey test. Blood pressure data were analyzed by repeated measures ANOVA. Data were expressed as mean ± SEM. A probability value of P<0.05 was considered to be statistically significant.
Results
Effect of Exercise Training on Mean Arterial Pressure
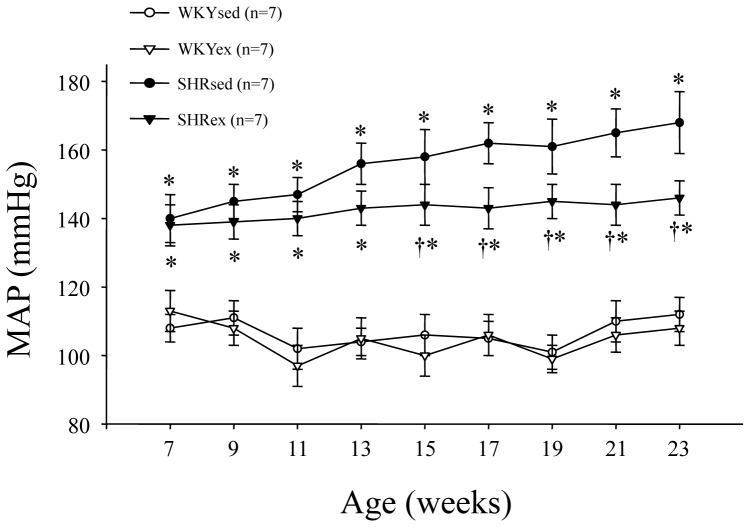
SHR rats had significant higher mean arterial pressure when compared with WKY rats. Exercise training reduced mean arterial pressure in SHR rats from 13 weeks of exercise, indicating the anti-hypertensive effect of exercise training (Figure 1).
Figure 1. Time course of mean arterial pressure (MAP) in WKY and SHR rats.
SHR rats had significant higher MAP when compared with WKY rats. Exercise training reduced MAP in SHR rats from 13 weeks of exercise. *P<0.05 versus control (WKYsed or WKYex); † P<0.05 SHRex versus SHRsed.
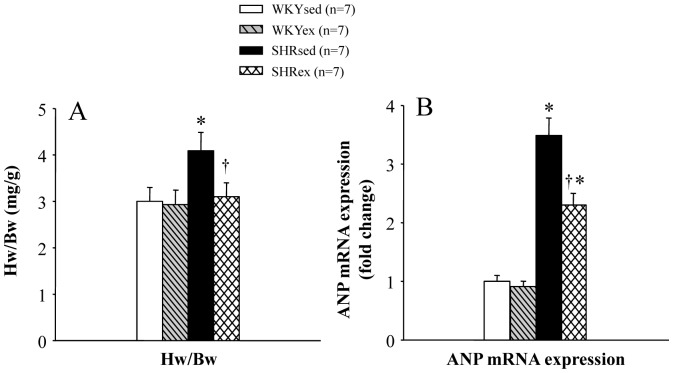
Effect of Exercise Training on Cardiac Hypertrophy
In order to evaluate cardiac hypertrophy, the hearts were harvested and weighed at the end of experiments. The ratio of heart weight/body weight (Hw/Bw) was measured as an indicator of cardiac hypertrophy. SHR rats had increased cardiac hypertrophy, as assessed by the ratio of Hw/Bw (Figure 2A), which was reduced following exercise training. The mRNA expression of a marker of cardiac hypertrophy, atrial natriuretic peptide (ANP), was measured in the left ventricular tissue using real-time PCR. SHR rats had increased mRNA expression of ANP in the left ventricular tissue of the heart, which was decreased by ExT (Figure 2B).
Figure 2. Effect of exercise training on cardiac hypertrophy in WKY and SHR rats.
SHR rats had increased cardiac hypertrophy, as assessed by the ratio of heart weight to body weight (Hw/Bw) (A) and mRNA expression of ANP in the left ventricular tissue of the heart (B), which was reduced following exercise training. *P<0.05 versus control (WKYsed or WKYex); † P<0.05 SHRex versus SHRsed.
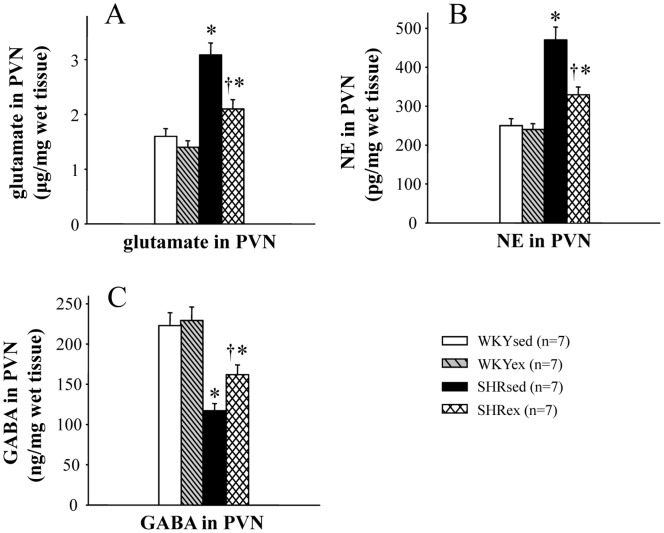
Effect of Exercise Training on the Neurotransmitters in the PVN
SHR rats had higher levels of NE and glutamate, and lower level of GABA in the PVN than WKY rats (Figure 3). Exercise training attenuated the decrease in PVN GABA and the increases in PVN glutamate and NE in SHR rats (Figure 3).
Figure 3. Effect of exercise training on the PVN levels of norepinephrine (NE), glutamate and GABA in WKY and SHR rats.
SHR rats had higher levels of glutamate (A) and NE (B), and lower level of GABA (C) in the PVN. Exercise training attenuated the decrease in PVN GABA and the increases in PVN glutamate and NE in SHR rats. *P<0.05 versus control (WKYsed or WKYex); † P<0.05 SHRex versus SHRsed.
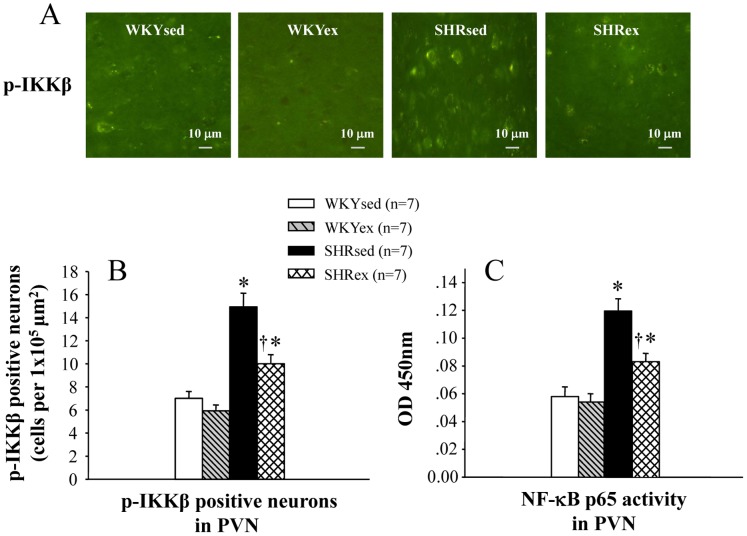
Effect of Exercise Training on NF-κB Activation in the PVN
SHR rats showed increases in NF-κB p65 activity and phosphorylated IKKβ in the PVN. Exercise training attenuated the increases in NF-κB p65 activity and phosphorylated IKKβ in the PVN of SHR rats (Figure 4).
Figure 4. Effects of exercise training on NF-κB p65 activity and the number of p-IKKβ positive neurons in the PVN of WKY and SHR rats.
SHR rats showed increases in NF-κB p65 activity and p-IKKβ in the PVN. Exercise training attenuated the increases in NF-κB p65 activity and p-IKKβ in the PVN of SHR rats. *P<0.05 versus control (WKYsed or WKYex); † P<0.05 SHRex versus SHRsed.
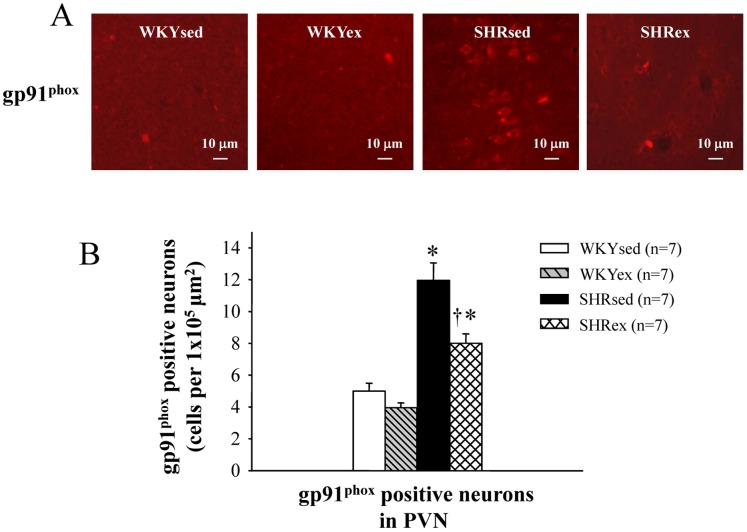
Effect of Exercise Training on the Number of gp91phox Positive Neurons in the PVN
SHR rats had more NAD(P)H oxidase subunit gp91phox expression in the PVN than WKY rats. Exercise training decreased gp91phox expression in the PVN of SHR rats (Figure 5).
Figure 5. Effect of exercise training on the number of gp91phox positive neurons in the PVN of WKY and SHR rats.
SHR rats had more NAD(P)H oxidase subunit gp91phox expression in the PVN than WKY rats. Exercise training decreased gp91phox expression in the PVN in SHR rats. *P<0.05 versus control (WKYsed or WKYex); † P<0.05 SHRex versus SHRsed.
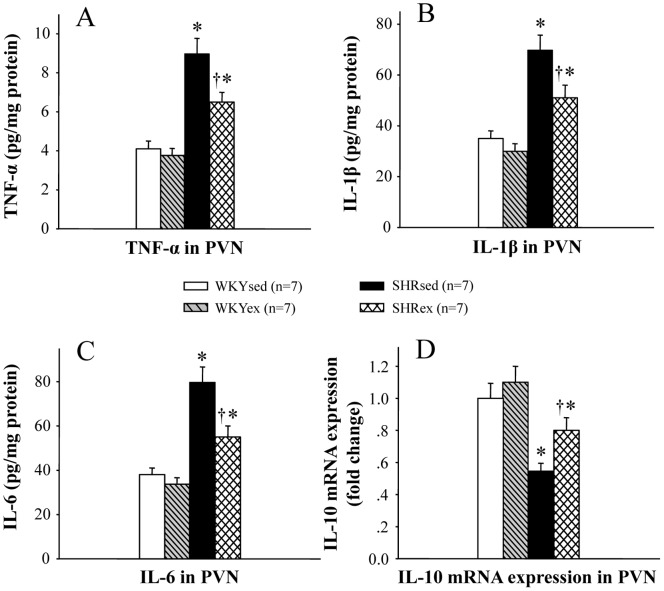
Effect of Exercise Training on PICs in the PVN
In order to determine the effect of exercise training on the production of PICs, chemokines and anti-inflammatory cytokines, the levels of TNF-α, IL-1β, IL-6, IL-10 and the MCP-1 were measured in the PVN (Figure 6 and Figure 7D). PVN levels of TNF-α, IL-1β, IL-6 and the MCP-1 in SHR rats were higher than in WKY rats. Exercise training reduced the PVN levels of TNF-α, IL-1β, IL-6 and the MCP-1 in SHR rats. Exercise training restored the balance between pro- and anti-inflammatory cytokines in the PVN of SHR rats.
Figure 6. Effect of exercise training on the PVN levels of TNF-α, IL-1β, IL-6 and IL-10 in WKY and SHR rats.
PVN levels of TNF-α, IL-1β and IL-6 in SHR rats were higher than in WKY rats, and PVN level of IL-10 in SHR rats was lower than in WKY rats. Exercise training reduced the PVN levels of TNF-α, IL-1β and IL-6 and increased the PVN level of IL-10 in SHR rats. *P<0.05 versus control (WKYsed or WKYex); † P<0.05 SHRex versus SHRsed.
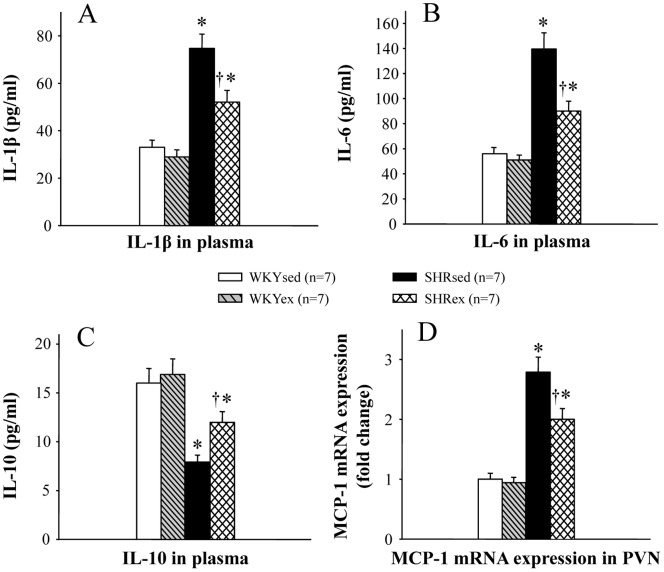
Figure 7. Effect of exercise training on the plasma levels of IL-1β, IL-6 and IL-10 and the PVN level of the chemokine MCP-1 in WKY and SHR rats.
Plasma levels of IL-1β and IL-6 and PVN level of the chemokine MCP-1 in SHR rats were higher than in WKY rats, and plasma level of IL-10 in SHR rats was lower than in WKY rats. Exercise training reduced the plasma levels of IL-1β and IL-6 and PVN level of the chemokine MCP-1, and exercise training increased plasma level of IL-10 in SHR rats. *P<0.05 versus control (WKYsed or WKYex); † P<0.05 SHRex versus SHRsed.
Effect of Exercise Training on Plasma Pro- and Anti-inflammatory Cytokines
Plasma levels of IL-1β and IL-6 in SHR rats were higher than in WKY rats, and plasma level of IL-10 in SHR rats was lower than in WKY rats (Figure 7). ExT reduced the plasma levels of IL-1β and IL-6 and increased plasma level of IL-10 in SHR rats (Figure 7).
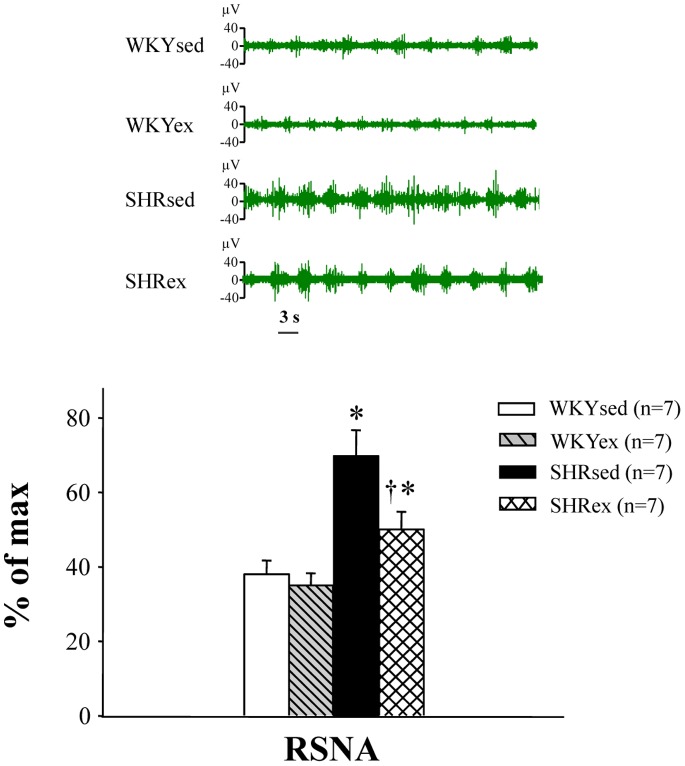
Effect of Exercise Training on RSNA
RSNA was recorded 5 h after rats recovered from anesthesia. RSNA was increased in SHR rats compared with WKY rats. Exercise training decreased RSNA in SHR rats (Figure 8).
Figure 8. Effect of exercise training on renal sympathetic nerve activity (RSNA) in WKY and SHR rats.
RSNA was increased in SHR rats compared with WKY rats. Exercise training decreased RSNA in SHR rats. *P<0.05 versus control (WKYsed or WKYex); † P<0.05 SHRex versus SHRsed.
Discussion
In this study, the role of exercise training on hypertension and cardiac hypertrophy was investigated. The novel findings of the present study are: (1) exercise training may attenuate hypertension-induced cardiac hypertrophy in rats by restoring the balances between the excitatory and inhibitory neurotransmitters and between pro- and anti-inflammatory cytokines in the PVN; (2) NF-κB p65 activity, oxidative stress and PICs in the PVN may be involved in the exercise-induced effects; (3) exercise training also has a beneficial effect by restoring the peripheral cytokine balance between pro- and anti-inflammatory cytokines in hypertension.
Elevated sympathetic outflow is commonly observed in hypertensive disorders and known to result in cardiac dysfunction and hypertrophy [2], [6]. Increasing evidence suggests changes of presympathetic neuronal activity in central nervous system might play a crucial role in blood pressure control, especially in the PVN [3], [16], [17]. The sympathetic outflow from the PVN depends on the balance of excitatory and inhibitory neurotransmitters in sympathetic neurons [18], [19] . Moreover, an imbalance among neurotransmitters caused by an overload of PICs in the PVN has been confirmed [16], [20]. Infusion of pro-inflammatory cytokine production inhibitor into the PVN causes the depression of the sympathetic activity along with the decreases in PVN levels of the excitatory neurotransmitters glutamate and NE as well as the increase in PVN level of inhibitory neurotransmitter GABA [21], [22]. In this study, we observed that SHR rats had exaggerated RSNA, higher PVN levels of glutamate, NE and PICs, and lower PVN level of GABA than WKY rats. These results indicate that the neurotransmitters and PICs in the PVN play important roles in sympathoexcitation and cardiac hypertrophy in hypertension.
Oxidative stress and the subsequent increase in the ROS production in the PVN have been proven to contribute to the progression of hypertension and cardiovascular disease [23]–[25]. In addition, a number of PICs have been identified to have the function of increasing ROS production [4], and the increased ROS in turn activates NF-κB and then results in the further increase in PICs production [26], [27]. Recent studies from our laboratory and others indicate inhibition of PICs production down-regulates NF-κB activity, gp91phox expression and the free radical production in the PVN, and attenuates sympathoexcitation, suggesting the interaction among PICs, ROS, and NF-κB in heart failure [1], [28] . According to these findings, increased PICs in the PVN may be caused by oxidative stress and NF-κB activation.
Exercise training has been recommended as an important nonpharmacological treatment for hypertension [29]–[32]. In the present study, hypertension and cardiac hypertrophy as well as the sympathoexcitation in SHR rats were improved after 16 weeks of moderate ExT. These results were consistent with the findings from Agarwal and others that ExT exerts the anti-hypertensive effect [4], [33]–[35], but the detailed mechanisms of ExT on central nervous system have not been firmly established. Brain PICs and ROS were found to induce the imbalance between excitatory neurotransmitters glutamate and inhibitory neurotransmitters GABA in the PVN [18], [19], [28], [36]. The increased presynaptic glutamate release and over-expression of postsynaptic NMDA receptors have been confirmed to lead to the hyperactivity of the PVN neurons [37], [38]. On the contrary, the inhibitory neurotransmitter GABA in the PVN was obviously down-regulated in hypertensive rats. Chronic ExT not only attenuates PICs, alters the adrenergic and GABAergic system, and reduces oxidative stress, but also improves the anti-inflammatory mechanisms in the PVN and plasma. Therefore, these findings together with previous studies [4], [39]–[41] indicate that chronic exercise training attenuates hypertension and cardiac hypertrophy by restoring the balances between excitatory and inhibitory neurotransmitters and between pro- and anti-inflammatory cytokines in the PVN.
In summary, the results from this study indicates that: (1) hypertensive rats may have an imbalance between excitatory and inhibitory neurotransmitters within the PVN, and an imbalance between pro- and anti-inflammatory cytokines in the PVN, and accompanied by NF-κB p65 activation and oxidative stress in the PVN, and thereby may be responsible for sympathoexcitation, hypertensive response and cardiac hypertrophy; and (2) exercise training attenuates hypertension and cardiac hypertrophy by restoring the balance between the excitatory and inhibitory neurotransmitters and the balance between pro- and anti-inflammatory cytokines, and attenuating NF-κB p65 activity and oxidative stress in the PVN. Our findings provide further evidence and insight for the beneficial effect of exercise training on hypertension and cardiac hypertrophy.
Funding Statement
This study was supported by National Basic Research Program of China (No. 2012CB517805) and National Natural Science Foundation of China (Nos. 31271254, 81170248, 81070199, 31171095, 31171141). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Kang YM, Gao F, Li HH, Cardinale JP, Elks C, et al. (2011) NF-κB in the paraventricular nucleus modulates neurotransmitters and contributes to sympathoexcitation in heart failure. Basic Res Cardiol 106: 1087–1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mariappan N, Soorappan RN, Haque M, Sriramula S, Francis J (2007) TNF-alpha-induced mitochondrial oxidative stress and cardiac dysfunction: restoration by superoxide dismutase mimetic Tempol. Am J Physio Heart Circ Physiol 293: 2726–2737. [DOI] [PubMed] [Google Scholar]
- 3. Nishihara M, Hirooka Y, Matsukawa R, Kishi T, Sunagawa K (2012) Oxidative stress in the rostral ventrolateral medulla modulates excitatory and inhibitory inputs in spontaneously hypertensive rats. J Hypertens 30: 97–106. [DOI] [PubMed] [Google Scholar]
- 4. Agarwal D, Welsch MA, Keller JN, Francis J (2011) Chronic exercise modulates RAS components and improves balance between pro- and anti-inflammatory cytokines in the brain of SHR. Basic Res Cardiol 106: 1069–1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Pescatello LS, Franklin BA, Fagard R, Farquhar WB, Kelley GA, et al. (2004) American College of Sports Medicine Position Stand: Exercise and hypertension. Medicine & Science in Sports & Exercise 36: 533–553. [DOI] [PubMed] [Google Scholar]
- 6. Cornelissen V, Fagard R (2005) Effect of resistance training on resting blood pressure: a meta-analysis of randomized controlled trials. Journal of Hypertension 23: 251–259. [DOI] [PubMed] [Google Scholar]
- 7. Roque FR, Briones AM, García-Redondo AB, Galán M, Martínez-Revelles S, et al. (2013) Aerobic exercise reduces oxidative stress and improves vascular changes of small mesenteric and coronary arteries in hypertension. Br J Pharmacol 168: 686–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Goldberg MJ, Boutcher SH, Boutcher YN (2012) The effect of 4 weeks of aerobic exercise on vascular and baroreflex function of young men with a family history of hypertension. J Hum Hypertens 26: 644–649. [DOI] [PubMed] [Google Scholar]
- 9. Mariappan N, Elks CM, Haque M, Francis J (2012) Interaction of TNF with angiotensin II contributes to mitochondrial oxidative stress and cardiac damage in rats. PLoS One 7: e46568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kang YM, Ma Y, Zheng JP, Elks C, Sriramula S, et al. (2009) Brain nuclear factor-kappa B activation contributes to neurohumoral excitation in angiotensin II-induced hypertension. Cardiovasc Res 82: 503–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. KangYM, He RL, Yang LM, Qin DN, Guggilam A, et al. (2009) Brain tumour necrosis factor-alpha modulates neurotransmitters in hypothalamic paraventricular nucleus in heart failure. Cardiovasc Res 83: 737–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kang YM, Ma Y, Elks C, Zheng JP, Yang ZM, et al. (2008) Cross-talk between cytokines and renin-angiotensin in hypothalamic paraventricular nucleus in heart failure: role of nuclear factor-kappaB. Cardiovasc Res 79: 671–678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Barber M, Kasturi BS, Austin ME, Patel KP, MohanKumar SM (2003) Diabetes-induced neuroendocrine changes in rats: role of brain monoamines, insulin and leptin. Brain Res 964: 128–135. [DOI] [PubMed] [Google Scholar]
- 14. Sriramula S, Cardinale JP, Francis J (2013) Inhibition of TNF in the brain reverses alterations in RAS components and attenuates angiotensin II-induced hypertension. PLoS One 8: e63847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yu XJ, Suo YP, Qi J, Yang Q, Li HH, et al.. (2013) Interaction between AT1 receptor and NF-κB in hypothalamic paraventricular nucleus contributes to oxidative stress and sympathoexcitation by modulating neurotransmitters in heart failure. Cardiovascular Toxicology doi:10.1007/s12012-013-9219-x. [DOI] [PubMed]
- 16. Kang YM, Zhang AQ, Zhao XF, Cardinale JP, Elks C, et al. (2011) Paraventricular nucleus corticotrophin releasing hormone contributes to sympathoexcitation via interaction with neurotransmitters in heart failure. Basic Res Cardiol 106: 473–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Guyenet PG (2006) The sympathetic control of blood pressure. Nat Rev Neurosci 7: 335–346. [DOI] [PubMed] [Google Scholar]
- 18. Kishi T, Hirooka Y, Sakai K, Shigematsu H, Shimokawa H, et al. (2001) Overexpression of eNOS in the RVLM causes hypotension and bradycardia via GABA release. Hypertension 38: 896–901. [PubMed] [Google Scholar]
- 19. Ferguson AV, Latchford KJ (2000) Local circuitry regulates the excitability of rat neurohypophysial neurones. Exp Physiol 85: 153–161. [DOI] [PubMed] [Google Scholar]
- 20. Kang YM, Zhang ZH, Johnson RF, Yu Y, Beltz T, et al. (2006) Novel effect of mineralocorticoid receptor antagonism to reduce proinflammatory cytokines and hypothalamic activation in rats with ischemia-induced heart failure. Circ Res 99: 758–766. [DOI] [PubMed] [Google Scholar]
- 21. Tasker JG, Boudaba C, Schrader LA (1998) Local glutamatergic and GABAergic synaptic circuits and metabotropic glutamate receptors in the hypothalamic paraventricular and supraoptic nuclei. Adv Exp Med Biol 449: 117–121. [DOI] [PubMed] [Google Scholar]
- 22. Chen QH, Haywood JR, Toney GM (2003) Sympathoexcitation by PVN injected bicuculline requires activation of excitatory amino acid receptors. Hypertension 42: 725–731. [DOI] [PubMed] [Google Scholar]
- 23. Lindley TE, Doobay MF, Sharma RV, Davisson RL (2004) Superoxide is involved in the central nervous system activation and sympathoexcitation of myocardial infarction-induced heart failure. Circ Res 94: 402–409. [DOI] [PubMed] [Google Scholar]
- 24. Kishi T, Hirooka Y, Katsuki M, Ogawa K, Shinohara K, et al. (2012) Exercise training causes sympathoinhibition through antioxidant effect in the rostral ventrolateral medulla of hypertensive rats. Clin Exp Hypertens 34: 278–283. [DOI] [PubMed] [Google Scholar]
- 25. Powers SK, Jackson MJ (2008) Exercise-induced oxidative stress: cellular mechanisms and impact on muscle force production. Physiol Rev 88: 1243–7126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Cardinale JP, Sriramula S, Mariappan N, Agarwal D, Francis J (2012) Angiotensin II-induced hypertension is modulated by nuclear factor-κB in the paraventricular nucleus. Hypertension 59: 113–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hirooka Y (2008) Role of reactive oxygen species in brainstem in neural mechanisms of hypertension. Auton. Neurosci 142: 20–24. [DOI] [PubMed] [Google Scholar]
- 28. Shi P, Raizada MK, Sumners C (2010) Brain cytokines as neuromodulators in cardiovascular control. Clin Exp Pharmacol Physiol 37: 52–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hamer M (2006) The anti-hypertensive effects of exercise. Sports Medicine 36: 109–116. [DOI] [PubMed] [Google Scholar]
- 30. Pescatello L, Margauz GA, Blanchard BE, Kerr A, Taylor AL, et al. (2004) Exercise intensity alters postexercise hypotension. Journal of Hypertension 22: 1881–1888. [DOI] [PubMed] [Google Scholar]
- 31. Bertagnolli M, Schenkel PC, Campos C, Mostarda CT, Casarini DE, et al. (2008) Exercise training reduces sympathetic modulation on cardiovascular system and cardiac oxidative stress in spontaneously hypertensive rats. Am J Hypertens 21: 1188–1193. [DOI] [PubMed] [Google Scholar]
- 32.Casillas JM, Gremeaux V, Damak S, Feki A, Pérennou D (2007) Exercise training for patients with cardiovascular disease. Ann Readapt Med Phys 50: 403–18, 386–402. [DOI] [PubMed]
- 33. Wang S, Teschemacher AG, Paton JF, Kasparov S (2006) Mechanism of nitric oxide action on inhibitory GABAergic signaling within the nucleus tractus solitarii. FASEB J 20: 1537–1539. [DOI] [PubMed] [Google Scholar]
- 34. Zheng H, Li YF, Cornish KG, Zucker IH, Patel KP (2005) Exercise training improves endogenous nitric oxide mechanisms within the paraventricular nucleus in rats with heart failure. Am J Physiol Heart Circ Physiol 288: 2332–2341. [DOI] [PubMed] [Google Scholar]
- 35. Li YF, Wang Y, Channon KM, Schultz HD, Zucker IH, et al. (2005) Manipulation of neuronal nitric oxide synthase within the paraventricular nucleus using adenovirus and antisense technology. Methods Mol Med 112: 59–79. [DOI] [PubMed] [Google Scholar]
- 36. Aston JG, Zhu Y, Card JP (2004) Numerous GABAergic afferents to locus ceruleus in the pericerulear dendritic zone: possible interneuronal pool. J Neurosci 24: 2313–2321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Li DP, Chen SR, Pan HL (2002) Nitric oxide inhibits spinally projecting paraventricular neurons through potentiation of presynaptic GABA release. J. Neurophysiol 88: 2664–2674. [DOI] [PubMed] [Google Scholar]
- 38. Lin Y, Matsumura K, Kagiyama S, Fukuhara M, Fujii K, et al. (2005) Chronic administration of olmesartan attenuates the exaggerated pressor response to glutamate in the rostral ventrolateral medulla of SHR. Brain Res 1058: 161–166. [DOI] [PubMed] [Google Scholar]
- 39. Dampney RA, Horiuchi J, Killinger S, Sheriff MJ, Tan PS, et al. (2005) Long-term regulation of arterial blood pressure by hypothalamic nuclei: some critical questions. Clin Exp Pharmacol Physiol 32: 419–425. [DOI] [PubMed] [Google Scholar]
- 40. Michelini LC, Stern JE (2009) Exercise-induced neuronal plasticity in central autonomic networks: role in cardiovascular control. Exp Physiol 94: 947–960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Potts JT (2006) Inhibitory neurotransmission in the nucleus tractus solitarii: implications for baroreflex resetting during exercise. Exp Physiol 91: 59–72. [DOI] [PubMed] [Google Scholar]