Abstract
Objective: Following the national proclaim of Measles Elimination 2012, plenty of activities for controlling the incidence had practiced in Hangzhou. However, the incidence did not decrease to low degree and remained perform as gap to the elimination target. The present study aimed to describe the epidemiological characteristics of measles, and proposed reasonable method to the target in Hangzhou.
Method: Cases were collected by the National Notifiable Diseases Surveillance System (NNDSS) from 2004 to 2011. The descriptive epidemiology was employed to analyze characteristics of measles.
Results: A total of 4712 confirmed cases were enrolled by the NNDSS with 7.87 per 100,000 people of incidence rate on average from 2004 to 2011. Individuals lived urban districts had higher risk of measles than counties. Infants aged <1 year observed the highest incidence rate with 239.35/100,000, and the age-specific incidence rate declined along with aged-group but reversed at adults. 52.20% of cases were floating cases and the measles vaccination was significantly different from the local cases (χ2=51.65,p <0.001). February to June was the epidemic period for measles incidence with 81.88% of cases reported in cluster.
Conclusion: The descriptive characteristics of measles suggested that factors included infant and adult individual, floating population, and living urban area might be relate to the elimination target. More efforts were need to ensure susceptible population had accepted qualified measles vaccination.
Keywords: measles, measles elimination, immunization strategy, descriptive epidemiology
Introduction
Measles is one of the most devastating infectious diseases for humans and has caused millions of death worldwide each year before introduction of measles vaccine (MV). China as a developing country, the morbidity of measles was 1145.75/ 100,000 before using MV in 1967 y.1 In the past decades, the routine measles immunization recommendations and supplementary immunization activities were proposed to population, which substantial decreased the morbidity and mortality of measles. According to publication, the incidence rate in 2010 reduced to 2.68 per 10, 0000 people, which was the lowest level in the past 20 y.1 Hangzhou as the capital of Zhejiang province located eastern coastline is a developed city of China, started providing MV to population in 1967. In order to improve level of population immunity, besides the first dose MV at 8 mo old, the government provide an additional MV or measles contained vaccine (MCV) to other age groups. The vaccination schedule has also changed with time, two doses of free MCV were proposed as basic vaccination recommendation. Moreover, MCV supplementary immunization has been given at times to children from preschool to senior high school age. However, the measles has not subsided significantly in recent years, and similar as previous data the outbreaks still comes back every 3 to 5 y.2 Meanwhile, with improved economic environment in Hangzhou, floating population from mid or west district of China mainland flocks in each year. Researches described that compared with local population; more defective immunization and less healthcare service demand have been made available to the floating population.3-7 These are probably challenges for Measles Elimination target in the next phase in Hangzhou. The present study aimed to review the measles prevention progress in Hangzhou, to describe the epidemiologic characteristics of measles in the recent years, and proposed reasonable ways to Measles Elimination target finally in Hangzhou.
Results
The incidence rate and proposed measles vaccination schedule from 1967 y in Hangzhou
According to the historical data from 1955 y, the incidence rate of measles reached thousands degree per 100,000 people, especially in 1959 the figure increased to 2543.51/100,000, which could cause 20~50 per 100,000 death each year. When MV injected to susceptible population aged over 8 mo, it obviously decreased to hundreds level later. The 1990s showed a lower incidence compared with other periods, but the rate returned to high degree since 2000 y. A 3 to 5 y interval of measles epidemic could find in the figure (Fig 1). In Hangzhou, the first vaccination of measles vaccine was practiced in 1967 y. People can get infected with measles over 8 mo were recommended to accepted one dose MV or MCV vaccination. To keep on reducing measles case and strengthen immunity level of population, Hangzhou CDC proposed that 7 y old (Primary school age) as the second vaccination time in 1977 to 1979 y. Eight month and 7 y old schedule reconsidered latterly and upgraded to add newly enrolled student at colleges. There have been other modification in the last decade such as the second dose changed to 12 to 23 mo old and 18 to 24 mo and re-proposed 7 y or primary school age vaccination. According to Chinese government’s Measles Elimination proclaim, besides routine vaccination recommendation, supplementary immunization activities covered 8 mo to high school age, ignored individual’s vaccination or infection history was implemented since 2005 y. In all activities, MV or MCV was vaccinated free.
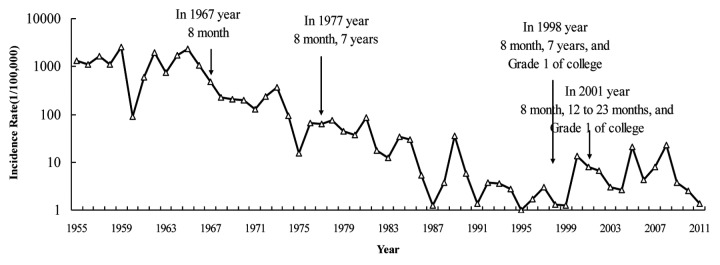
Figure 1. The incidence rate of measles in Hang Zhou from 1955 to 2011.
The general characteristics of measles cases reported by NNDSS from 2004 to 2011 y
From 2004 to 2011 y, a total of 4712 cases were enrolled with 7.87 per 100,000 people of incidence rate on average. The age ranged 12 d to 72 y and median value was 21 y old, male to female ratio was 1.14. Together the number of case in 2005 and 2008, the percentage reached 64.58 nearly twice more than the amount of the other years, more than a half of case as floating population (52.20%). Only 16.51% individuals had measles vaccination according to registration or self-reported. Most of case’s confirmation was through lab testing (94.25%) (Table 1).
Table 1. The general characteristics of measles cases.
| Characteristics | Category | Case (N) | Percentage (%) |
|---|---|---|---|
| Sex | Male | 2513 | 53.33 |
| Female | 2199 | 46.67 | |
| Regional distribution | Urban | 3913 | 83.04 |
| Suburban | 799 | 16.96 | |
| Reported year | 2004 | 171 | 3.63 |
| 2005 | 1337 | 28.37 | |
| 2006 | 317 | 6.73 | |
| 2007 | 586 | 12.44 | |
| 2008 | 1706 | 36.21 | |
| 2009 | 283 | 6.01 | |
| 2010 | 197 | 4.18 | |
| 2011 | 115 | 2.44 | |
| Migrant status* | Local | 2219 | 47.80 |
| Floating | 2423 | 52.20 | |
| Vaccination* | Yes | 767 | 16.51 |
| No | 1958 | 42.15 | |
| Unknown | 1920 | 41.33 | |
| Confirmed method | Lab | 4441 | 94.25 |
| Clinical | 271 | 5.75 |
Note: *Migrant status missed 70 cases, Vaccination missed 67 cases.
The geographical distribution of measles and incidence by epidemiological intensity
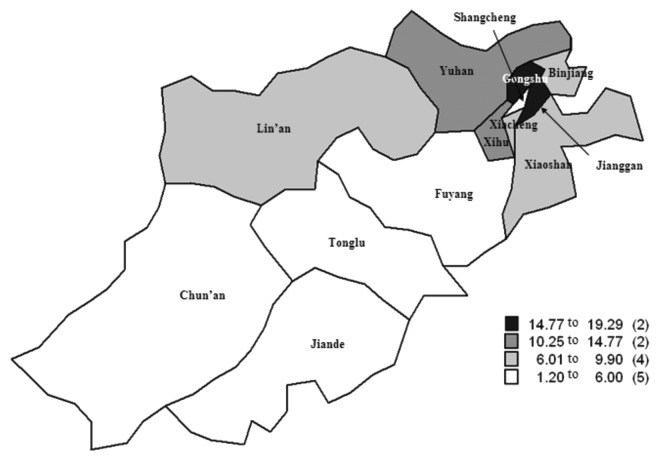
Figure 2 showed that eight urban districts located northeast of Hangzhou with a smaller area compared to five suburban counties. From 2004 to 2011 y, the measles incidence of urban districts was 9.96 per 100,000 people on average, higher than the rate calculated at suburban counties (3.88/100,000). In the urban districts, 19.29 at Jianggan district was the highest rate and 5.28 at Shangcheng district was the lowest rate. Suburban counties ranged 1.20 to 6.01 and the highest and lowest rate belonged to Lin’an and Chun’an. Considering the geographical factor and epidemiological intensity at meanwhile, 4.80 per 100,000 people was observed when the disease was sporadic and significantly increased to 26.98 when the disease was epidemic at urban districts. The incidence range of suburban counties was much gentle as 1.48 to 11.20 (Fig. 3).
Figure 2. The geographical distribution of measles from 2004 to 2011.
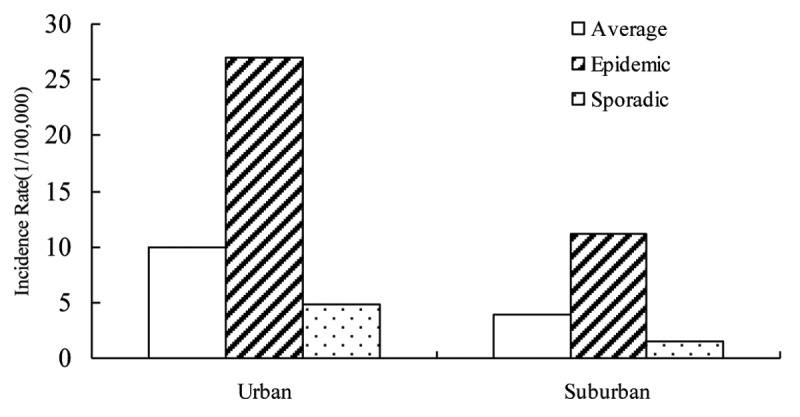
Figure 3. The incidence of measles by geographical distribution and epidemiological intensity.
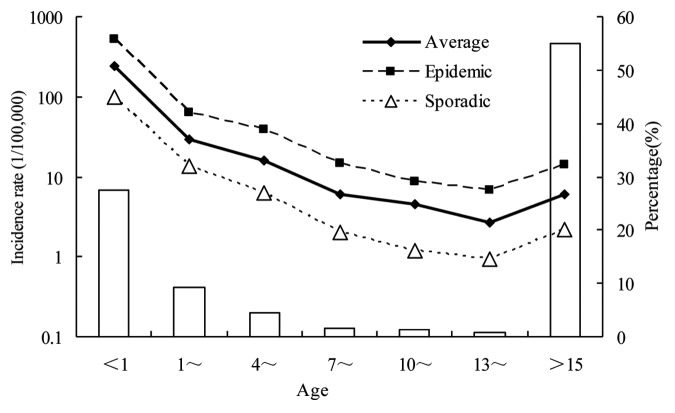
The age-specific incidence rate of measles by epidemiological intensity
As Figure 4 showed, children aged < 1 y had higher risk of measles. The percentage of this group was 27.57% and the age-specific incidence was 239.35/100,000 on average from 2004 to 2011 y. The rate would rise to 530.85 when the disease was epidemic and reduce to 100.97 under sporadic intensity. Thereafter, the incidence decreased obviously with age: the 10~and 13~group maintained a low degree as 4.57 and 2.71. But measles incidence reversed among adult population, 5.93 per 100,000 people was reported among the group aged more than 15 y, contributed 54.97 percent (2598 people) in all the reported cases. If adult cases are grouped by a 5 y space, 78.06 percentage of cases (2028 people) are between 20 and 39 y and 52.51% was female (1065 people) (Fig. 5). A total of 1303 infant cases (age < 1 y) were reported by the system, and cases aged between 5 and 7 mo contributed to 51.50% (Fig. 6).
Figure 4. The age-specific incidence of measles by epidemiological intensity.
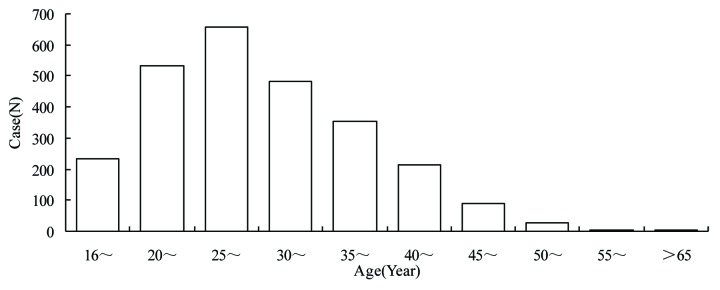
Figure 5. The percentage of adult cases grouped by a 5-y interval.
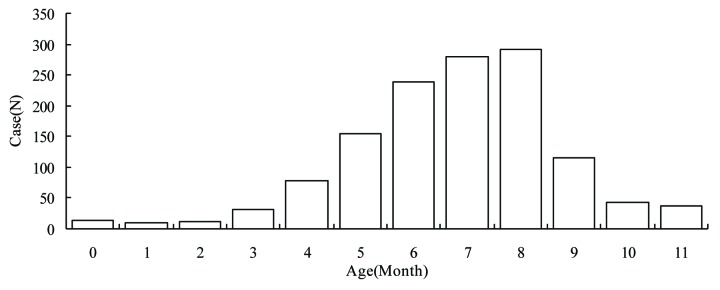
Figure 6. The distribution by month of cases aged less than 1 y.
The measles vaccination information of case grouped by floating status
Divided cases aged less than 1 y into two groups by 8 mo (The initial month to accept MCV). 20.00% had measles vaccination in the cases whose age was reasonable to accept measles vaccine. The vaccinated rate was 21.21% of local cases and 19.00% of floating cases with no significant difference between 2 groups ( ×2 = 2.89, p = 0.09). However, excluded age > 15 y cases to calculated the rate by floating status. 51.83% of local cases had measles vaccination, significantly higher than 30.96% of floating case ( ×2 = 51.65, p < 0.001) (Table 2)
Table 2. The vaccinated information of case by age and migrant status.
| Age (year) | Local case (%) | Floating case (%) | ||||
|---|---|---|---|---|---|---|
| unvaccinated | vaccinated | unknown | unvaccinated | vaccinated | unknown | |
| < 8 mo* | 478 | 322 | ||||
| 8~11 mo | 140(57.38) | 103(42.21) | 1(0.41) | 177(74.06) | 55(23.01) | 7(2.93) |
| 1~ | 26(39.39) | 40(60.61) | 210(57.69) | 102(28.02) | 52(14.29) | |
| 4~ | 4(14.29) | 20(71.43) | 4(14.29) | 64(36.16) | 73(41.24) | 40(22.60) |
| 7~ | 4(23.53) | 13(76.47) | 15(26.79) | 21(37.50) | 20(35.71) | |
| 10~ | 3(10.00) | 27(90.00) | 5(29.41) | 10(58.82) | 2(11.77) | |
| 13~ | 9(37.50) | 9(37.50) | 6(25.00) | 4(25.00) | 8(50.00) | 4(25.00) |
| > 15 | 220(16.65) | 155(11.73) | 946(71.61) | 276(22.72) | 127(10.45) | 812(66.83) |
| Total of age ≥ 8 month |
406(23.47) | 367(21.21) | 957(55.32) | 751(36.04) | 396(19.00) | 937(44.96) |
Note: *Age < 8 mo case was not calculated to total. Missed 70 cases of migrant status and 67 cases of vaccination, a total of 98 cases were excluded in this table. Case age ≥ 8 mo by migrant status ×2 = 2.89, p = 0.09. Case age between 8 mo and 15 y by migrant status ×2 = 51.65,p < 0.001. The level of significance for all analyses designated as p-value less than 0.05.
The time distribution of measles in one year grouped by epidemiological intensity
February to June seemed as a peak for measles incidence in one year, 81.88% cases were reported during this period. By the different epidemiological intensity, the tendency of sporadic intensity was less obvious than epidemic intensity. Percentage of case in February to June was 65.92 for sporadic intensity and 91.05 for epidemic intensity with significant difference ( ×2 = 472.44, p < 0.001) (Fig. 7)
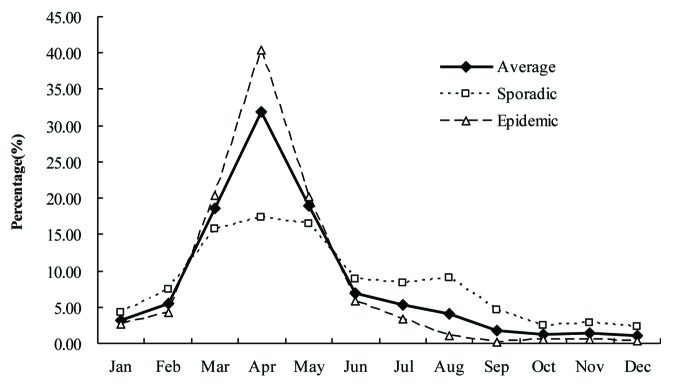
Figure 7. The time-distribution of measles grouped by epidemiological intensity.
Discussion
This study suggested measles still seemed as a public-health problem in Hangzhou. Floating population might be a risk factor for controlling the spread of measles. People lived in urban areas likely to risk higher chance of infecting measles than counties. Infants and adults were the distinguished components for the mortality of measles, and spring to early summer per year was the epidemic seasons of measles.
As a target, the Measles Elimination 2012 was established by the Regional Committee of the World Health Organization (WHO) Western Pacific Region in 2005.8 Following this proposition, Chinese government had drafted the 2006~2012 National Measles Elimination Action Plan in 2006 included effective measles vaccine vaccination policy, dependable measles cases surveillance system and unified cases diagnoses and treatment of disposal process. Through reviewing the historical data, it’s revealed that widespread use of MV or MCV has had a significant impact on measles epidemiology. In Hangzhou, measles incidence sustained a moderately intensity but still short of the recent elimination target . A low incidence in 1990s existed at the decline on measles in the past decades. There are significant differences betweendistribution of measles in 1990s (published in Chinese) with the present data, more cases were reported among infants aged less than 1 y and fewer cases were reported among 1 to 14 y old children from 2004 to 2011. Therefore, infants and adult cases seemed to be the key reason for the reverse of measles incidence according to our speculation. Because both reported and investigated coverage rate of the first dose MCV under 1 y old infant were more than 95%, and similar high rate for the second dose among low aged-group in Hangzhou. Furthermore, supplemental immunization programs (SIPs) were proposed to infant to teenage, accepting an additional dose of MCV, and were executed despite the individuals’ vaccination history. The above could explain the low incidence observed among this population. However, measles incidence still had a typical cycle in the recent years. In 2005 and 2008 y, the rate raised more than 20 per 100,000 people. Some studies related this phenomenon with the accumulation of susceptible population.9-11 Unfortunately, the coverage rate of MCV on whole population could not be estimated in the present study. Abundant studies based on Chinese population only focused the coverage of groups aged under 15 y. Nevertheless, the seroepidemiology could suggest the defect about the immunity of measles among population. There were routine surveillance data from different provinces showed the positive rate of IgG of whole population was not optimistic, especially among adults.12,13
There was no doubt that measles incidence had significantly geographical distribution. In China, northern and western provinces presented high incidence according to national surveillance data.1 In this study, the measles incidence of urban districts almost tripled of counties’, and sharply increased when the intensity of disease became epidemic. This might associate with population density, percentage of floating people, climate, life style, and others social factors. Analysis of American measles during 1980 to 1989, found that counties reporting measles more frequently during the decade had higher median populations, population densities, and percentage of black and Hispanic populations than those counties reporting less frequently.14
Infant had the highest measles incidence in the present study. This phenomenon was mainly because of decline of antibody from mother and timely vaccination. Among infants under 8 mo especially for those who didn’t accept MCV vaccination per recommendation, risk of measles increased along with the birth time. The recommended age for initial vaccination had been changed several times. In the early 1980s, WHO established a policy for measles immunization, recommended the administration of a single dose of measles vaccine at 9 mo of age.15 Meanwhile, some literature had referred to consider 6 mo as the starting vaccination age for children.16-18 In China, the ages for the initial vaccination also had been changed several times. The recent research at Qinghai province concerned about duration of maternally derived antibody against measles, suggested an earlier administration of the first dose of measles vaccination should be considered.19 However, the reality was that practiced an earlier procedure for the first vaccination of measles remained a controversy. In the present study, the incidence of adults was not the high as infant but contributed a dominant percentage of all cases (54.97%). There was no proposed vaccination schedule to protect adults from measles. This population risk to infection of measles might associate with no vaccination, unqualified vaccination, or too long time to protect by antibody. In this group, more than 50% of cases aged 20 to 39 y and 52.51% of cases were female. If mothers did not acquire qualified immunity against measles, infant might in term fail to acquire enough antibodies. In additional, the proportion of adult cases increased obviously along with the controlling of child cases. Previous investigation in Africa had found this change of epidemiological characteristic of measles following the introduction of routine infant immunization programs.20 while the vaccination programs had primarily targeted infants, children or teenagers, those older people who were not vaccinated, unqualified vaccinated or never experienced natural infection remained susceptible to measles. A total of 1278 cases aged 8 mo to 15 y old were reported in this study and 68.00% were floating cases. Basing on ours acknowledge, the amount of floating population in this group was less than local population in Hangzhou. These infants and children might changed living place or migrated from hometown times along with theirs parents, and brought problems to receive an effective vaccination. Furthermore, although SIP activities had executed for times, covered different age group among children, part of floating children also had only one dose vaccination of measles.
April was the time that measles incidence occurred in clusters in the present study. Furthermore, the time distribution had changed along with different epidemiological intensity of disease. February was the starting of traditional season of measles infection. At the same time, people would migrate from hometown after having spring festival in China. Much susceptible individuals moved into, which would enhance the intensity of measles’s spread.
Based on listed epidemiological characteristics of measles above, more strategies to Measles Elimination should be considered while implemented routine immunizations well in Hangzhou. Suggestions were that ensured all children accepting two dose MCV timely, implemented catch-up activities at some specially urban areas where floating population usually stayed in mass, and widely advertised knowledge of harm and prevention about measles among population. The present study had some limitations. Descriptive epidemiology was employed, which could not find significant factors for the epidemic of measles. If the characteristic of floating population and seroepidemiology could add to analysis, it might help to extract reasonable measures for the measles elimination. Ineffective to collect the age-cohort data, induced could not compute the incidence rate of adult groups. Other related factors as policy, hospital infection, education and so on were not included, which could provide other valuable information to Measles Elimination. However, the study showed characteristics of measles in the eastern coastline city in China, infants and adult people were high-risk population for infecting measles, and floating population might generate new challenges for measles elimination.
Materials and Methods
Data source
Hangzhou has a population of approximately 8.5 million people in 2011 y, with a land area of 16,596 km2, divided into 8 urban districts (Shangcheng, Xiacheng, Jianggan, Gongshu, Xihu, Bingjiang, Xiaoshan, Yuhang) and 5 suburban counties (Lin’an, Fuyang, Tonglu, Jiande, Chun’an). Each district and county had set a Center for Disease Prevention and Control (CDC) and several Community Health Centers (CHCs).
The National CDC established the National Notiðable Diseases Surveillance System (NNDSS) in 2004 y, which used to monitor epidemic diseases including measles, Neonatal tetanus, Acute Flaccid Paralysis, and then updated it into higher version for expanding variety of infectious diseases and increasing factors of case investigation like measles in 2008 y. The procedure of measles surveillance as follows: a. Physician working at medical institution was required to report suspected measles case within 24 h to CDC by the NNDSS system online. b. CDC staffs were responsible for case investigation when they receiving the measles reporting information, to gather related information including age, gender, address, vaccination status, and clinical symptoms data such as rash onset, fever, conjunctivitis. CDC staff also need know the likely source of exposure, the site of transmission, the patient’s travel history , the importation status of the disease, any links to other cases, follow up the outcome of disease (complications and death), and collect blood sample or etiology specimens for verification. c. CHCs workers were in charge of disinfection of case’s living or working place, emergence vaccination for susceptible population, health education and so on.
Following is source of figure referred to the present study. The population, history incidence rate (IR) of measles and vaccination schedule was from the annuals of disease surveillance reports of HangZhou CDC each year. Information of reported measles cases from 2004 to 2011 y could download from NNDSS for analyzing.
The criteria of suspect measles and confirmation
About the criterion, suspect case reported by physician was any person with fever and generalized maculopapular rash with cough, coryza, conjunctivitis or any person suspected by a health professional as having measles.
Blood sample or virus isolation for confirmation was tested by CDCs or hospital lab authorized by Hangzhou CDC, and with unified method and reagent. A laboratory confirmation was defined as having tested positive for measles IgM of an individual who had no association with measles vaccination or isolation of the measles virus. A confirmed case of measles included case that is either laboratory confirmed or a case that meets the clinical diagnosis by physician or epidemiologically links to a laboratory-confirmed case.
The definition of factors
Migrant status included local and floating situation, decided by household registration. The local case was one had household registration and usual lived at the place for disease onset, opposite to the floating case means like an imported case for the area of occurring disease. Epidemiological intensity of measles disease included sporadic and epidemic style separated by the incidence rate. In the present study, the incidence of 2005 and 2008 y were set as epidemic intensity and other years recognized as sporadic intensity.
Statistical analysis
Statistical analysis was performed with SPSS version 13.0 (SPSS Inc., Chicago, IL). Employed frequency to describe the characteristics of measles case, used Chi-square to test the significant difference among groups. The level of significance for all analyses designated as p-value less than 0.05.
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
Footnotes
Previously published online: www.landesbioscience.com/journals/vaccines/article/24032
References
- 1.Chao M, Lixin H, Jing M, Yan Z, Lei C, Xiaofeng L, et al. Measles Epidemiological Characteristics and Progress of Measles Elimination in China, 2010. Chinese Journal of Vaccine and Immunization. 2011;17:242–8. [Chinese] [Google Scholar]
- 2.Chiu HH, Lee CY, Chih TW, Lee PI, Chang LY, Lin YJ, et al. Seroepidemiological study of measles after the 1992 nationwide MMR revaccination program in Taiwan. J Med Virol. 1997;51:32–5. doi: 10.1002/(SICI)1096-9071(199701)51:1<32::AID-JMV5>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention (CDC) International Notes Nutritional and Health Status of Displaced Persons, Sudan, 1988-1989. MMWR Weekly. 1989;38:848–50. [PubMed] [Google Scholar]
- 4.Moore PS, Marfin AA, Quenemoen LE, Gessner BD, Ayub YS, Miller DS, et al. Mortality rates in displaced and resident populations of central Somalia during 1992 famine. Lancet. 1993;341:935–8. doi: 10.1016/0140-6736(93)91223-9. [DOI] [PubMed] [Google Scholar]
- 5.Toole MJ, Waldman RJ. An analysis of mortality trends among refugee populations in Somalia, Sudan, and Thailand. Bull World Health Organ. 1988;66(2):237–47. [PMC free article] [PubMed] [Google Scholar]
- 6.Chao M, Huiming L, Zhijie A, Ping Z, Ning W, Wei X, et al. Analysis on Epidemiological Characteristics and Measures of Measles Control in China During 2006-2007. Chinese Journal of Vaccine and Immunization. 2010;14:208–13. [Chinese] [Google Scholar]
- 7.Kouadio IK, Kamigaki T, Oshitani H. Measles outbreaks in displaced populations: a review of transmission, morbidity and mortality associated factors. BMC Int Health Hum Rights. 2010;10:5. doi: 10.1186/1472-698X-10-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization. Fifty-fourth session of the regional committee for the western pacific. Summary record of the fifth meeting. Resolution WPR/RC54.R3. Expanded programme on immunization: measles and hepatitis B. Manila, Philippines: WHO, 2003. http://www.wpro.who.int/rcm/en/archives/rc54/rc_resolutions/wpr_rc54_r03.htm
- 9.Moss WJ, Griffin DE. Measles. Lancet. 2012;379:153–64. doi: 10.1016/S0140-6736(10)62352-5. [DOI] [PubMed] [Google Scholar]
- 10.Fine PE, Clarkson JA. Measles in England and Wales--I: An analysis of factors underlying seasonal patterns. Int J Epidemiol. 1982;11:5–14. doi: 10.1093/ije/11.1.5. [DOI] [PubMed] [Google Scholar]
- 11.Ferrari MJ, Grais RF, Bharti N, Conlan AJK, Bjørnstad ON, Wolfson LJ, et al. The dynamics of measles in sub-Saharan Africa. Nature. 2008;451:679–84. doi: 10.1038/nature06509. [DOI] [PubMed] [Google Scholar]
- 12.Zhu HL, Ji JM, He B, Lin Y, Gao WJ, Fu XF, et al. Investigation on antibody level of measles and influencing factors among adults in Jiangxing, Zhejiang. Chin Prev Me. 2012;13:527–9. [Chinese] [Google Scholar]
- 13.Cheng J, Huo XX, Zhang HC, Zhan FX, Yang BF, Zhan JB. Analysis of immune levels against measles, rubella and mumps in healthy population in Hubei province. Chinese Journal of Health Laboratory Technology. 21:2737–41. [Google Scholar]
- 14.Hersh BS, Markowitz LE, Maes EF, Funkhouser AW, Baughman AL, Sirotkin BI, et al. The geographic distribution of measles in the United States, 1980 through 1989. JAMA. 1992;267:1936–41. doi: 10.1001/jama.1992.03480140062034. [DOI] [PubMed] [Google Scholar]
- 15.Martins CL, Garly ML, Balé C, Rodrigues A, Ravn H, Whittle HC, et al. Protective efficacy of standard Edmonston-Zagreb measles vaccination in infants aged 4.5 months: interim analysis of a randomised clinical trial. BMJ. 2008;337:a661. doi: 10.1136/bmj.a661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gans H, Yasukawa L, Rinki M, DeHovitz R, Forghani B, Beeler J, et al. Immune responses to measles and mumps vaccination of infants at 6, 9, and 12 months. J Infect Dis. 2001;184:817–26. doi: 10.1086/323346. [DOI] [PubMed] [Google Scholar]
- 17.Kumar ML, Johnson CE, Chui LW, Whitwell JK, Staehle B, Nalin D. Immune response to measles vaccine in 6-month-old infants of measles seronegative mothers. Vaccine. 1998;16:2047–51. doi: 10.1016/S0264-410X(98)00083-8. [DOI] [PubMed] [Google Scholar]
- 18.Aaby P, Martins CL, Garly ML, Rodrigues A, Benn CS, Whittle H. The optimal age of measles immunisation in low-income countries: a secondary analysis of the assumptions underlying the current policy. BMJ Open. 2012;2:e000761. doi: 10.1136/bmjopen-2011-000761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang X, Shirayama Y, Zhang Y, Ba W, Ikeda N, Mori R, et al. Duration of maternally derived antibody against measles: a seroepidemiological study of infants aged under 8 months in Qinghai, China. Vaccine. 2012;30:752–7. doi: 10.1016/j.vaccine.2011.11.078. [DOI] [PubMed] [Google Scholar]
- 20.Tumwine JK. Measles in Chimanimani Zimbabwe. East Afr Med J. 1989;66:531–4. [PubMed] [Google Scholar]