Abstract
Significant complications still occur after abdominoplasty, the rate varies widely in different series. This variation suggests that there is a lot of scope for improvement. This paper reviews the various complications and also the technical improvements reported in the last 20 years. The root cause of each complication is analysed and preventive steps are suggested based on the literature and the author's own personal series with very low complication rates. Proper case selection, risk stratified prophylaxis of thromboembolism, initial synchronous liposuction, flap elevation at the Scarpa fascia level, discontinuous incremental flap dissection, vascular preservation and obliteration of the sub-flap space by multiple sutures emerge as the strongest preventive factors. It is proposed that most of the complications of abdominoplasty are preventable and that it is possible to greatly enhance the aesthetic and safety profile of this surgery.
KEY WORDS: Abdominoplasty, complications, diastasis recti, haematoma, lipoabdominoplasty, necrosis, seroma, venous thromboembolism, ventral hernia, wound dehiscence
INTRODUCTION
Abdominoplasty is a common aesthetic procedure with a wide appeal;[1,2] however, it has a higher complication rate than other aesthetic procedures.[3] Despite a contemporary history of about 50 years, the basic steps of extensive undermining, skin resections, muscle plication and umbilical transposition have remained unchanged until recently. Although the complication rates have dropped, case series with high complication rates are still reported, striking a note of caution.[4–7] These complications lead to dissatisfaction, prolonged convalescence, unforeseen expenses, physical and psychological suffering and at times litigations. Rarely, they may be dangerous or fatal.[8] Many surgeons accept these complications as inevitable; however, several large series with very low complication rates even in high risk patients have also been published.[9] It is imperative therefore to re-evaluate one's technique critically and take effective steps to make the surgery safer and not accept the status quo.
Two decades long experience in abdominoplasties and an avid interest in reducing complications led the author to innovate and incorporate many published modifications into his technique. The author is convinced that complications in abdominoplasty can be reduced drastically. The present article is aimed at classifying the complications, analysing the root causes wherever possible, reviewing the literature and suggesting ways of minimising or entirely avoiding them.
MATERIALS AND METHODS
A PubMed search supplemented by Google Scholar was done using the keywords abdominoplasty or lipoabdominoplasty and complications, seroma, haematoma, outcome, smoking and obesity. The papers were then vetted for relevance. Reports of freak complications were excluded. A fresh comprehensive classification of possible reported/unreported complications of abdominoplasty was prepared. The list was grouped into logical categories. A root cause analysis of each complication/category was done based on surgical logic, personal experience and the literature, relying more on reviews and larger series. For each problem, preventive steps are suggested and again checked against the literature. These recommendations are further supported by results of the author's carefully maintained data of personal series. The present article is not a systematic review.
RESULTS
There were 445 reports related to this search, which were whittled down to 354 relevant ones; 25 were review articles. The common complications reported were seroma, necrosis, haematoma, infection, wound healing problems and venous thromboembolism (VTE). Less commonly reported complications include chest complications, umbilical loss, nerve symptoms, extensive skin loss, necrotising fasciitis, abdominal compartment syndrome, reflux esophagitis, peritoneal perforation, myocardial infarctions and death. The reported complications are classified in Table 1 and the aesthetic issues further in Table 2.
Table 1.
A classification of abdominoplasty complications based on aetiopathology
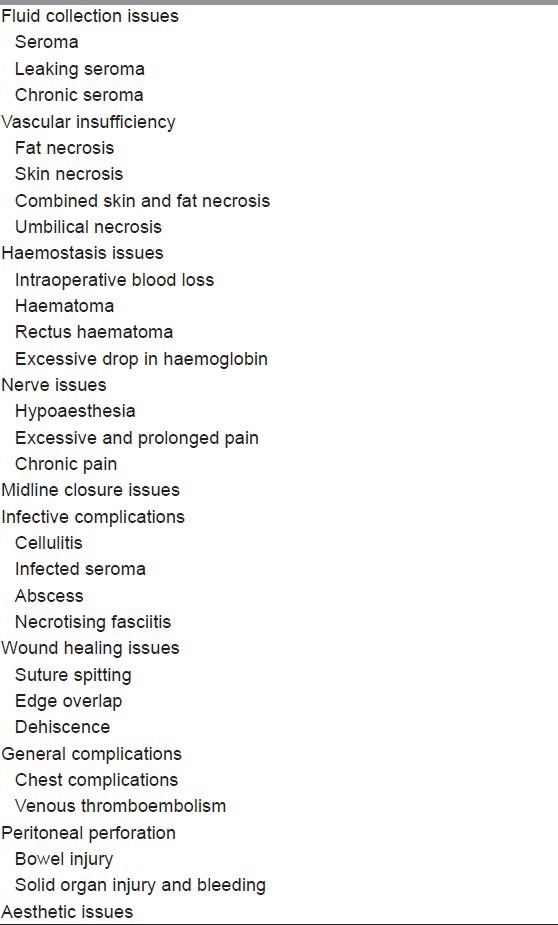
Table 2.
Aesthetic complications of abdominoplasty
DISCUSSION
A complication is any unforeseen event that either adversely affects the outcome of the procedure or delays the recovery or necessitates additional procedures to correct the problem. It may be life-threatening, serious or minor. It may be preventable or may be totally freak and unpreventable. A high variation in the reported complication rates of abdominoplasty suggests that there is scope for improvement and standardisation. The discussion below will take up each complication, analyse its possible root causes and then highlight preventive steps already reported in the literature or based on the author's experience.
Seroma
It is one of the most common complications reported.[10,11] No less than 113 reports discuss seroma as one of the complications. It is defined as a localised collection of serous or haemoserous fluid that is detected clinically or radiologically irrespective of the need for evacuation. The rate varies from 0.1% to 42%.[12] Seromas are distinctly more common in traditional abdominoplasty and distinctly less common in lipoabdominoplasty.[13] The earlier reports suggested that addition of liposuction increased the seroma rates, however in these series, the abdominoplasty was still done with full undermining to the rib cage.[10] The least rates are reported after progressive tension sutures or quilting sutures and when the plane of dissection is kept superficial to the Scarpa's fascia; in many of these series the authors do not even use drains.[14]
In general, seromas form easily when there is lack of adhesion between a flap and the underlying tissues; the risk of seroma is increased by shearing movements. The risk is greatest where either or both of the opposing surfaces is/are a natural gliding surface; as seen after harvest of latissimus dorsi flaps and anterolateral thigh flaps; there is a shiny fascia in both cases (lumbodorsal and fascia lata respectively). In traditional abdominoplasty, the flap is raised just superficial to the external oblique aponeurosis, again a gliding surface. The fat on the aponeurosis is also cut away during flap elevation, thus transecting many lymphatics. It may be proposed that the fat on the undersurface of the abdominoplasty flap does not adhere well to the shiny aponeurosis and this promotes seromas. Evidence for this hypothesis comes from three angles. First, in almost all cases of seromas, drains had been used for an adequate length of time.[10] Hence, drains do not prevent seromas; whether they increase the risk by tissue irritation is unclear. Secondly, keeping the plane of elevation close to the undersurface of Scarpa's fascia and leaving the sub-Scarpa fat undisturbed was associated with lower seroma rates.[15] The subcutaneous fat of the flap probably adheres better to the fat on the aponeurosis. Routine quilting sutures encourage adhesion of the flap to the aponeurosis and improved seroma rates even without drains.[16–18] Finally, flap elevation superficial to Scarpa's fascia has been reported to reduce the drainage output, time to drain removal and seroma rates.[19]
Baroudi and Ferreira proposed routine use of quilting sutures in 1998 based on a 5 year experience with zero seroma rate in 130 patients.[16] There have subsequently been several publications, which repeatedly show that seroma can be eliminated by routine adhesion sutures (variably called Baroudi sutures, progressive tension sutures by Pollock or quilting sutures).[20–22] Directly approximating the flap to the fascia by multiple sutures eliminates dead space, leads to early adhesion, prevents shearing forces between the two layers, enables early mobilisation without fear and also takes away the tension on wound closure. It is the single most important solution to multiple problems of seroma, haematoma, tension and wound healing problems.
The author is a strong proponent of this technique; since 1997, he routinely elevates the flap immediately deep to Scarpa fascia, preserving the fat on external oblique. He uses quilting sutures routinely and has discontinued drains altogether since 2002. There has been no seroma since then in over 200 consecutive primary cases.
Unfortunately, the role of the ‘surgeon-factor’ is rarely given importance in studies of complications, probably because it is not quantifiable. The author strongly believes that gentle tissue handling is an important factor, which can be assured by the following steps. Super-wet infiltration of the tissues with standard tumescent solution, liposuction before flap elevation and the routine and correct use of diathermy renders the dissection almost bloodless.[23] Precise control of the power setting and keeping the cautery tip clean are important to reduce collateral damage. The blend setting is used for clean cutting with minimal bleed; the spray mode is expedient for haemostasis of smaller bleeders, larger ones are securely coagulated or tied. Reducing the load of devitalised tissue in turn leads to less inflammatory exudates, less seroma and may also reduce infection and fat necrosis.
Combining liposuction with abdominoplasty was forbidden or advocated cautiously in the nineties,[24] but now the pendulum has swung to lipoabdominoplasty being the superior alternative.[9,13,25] It is important to note that lipoabdominoplasty is not merely liposuction added to traditional abdominal flap elevation (which will increase complications), but is a highly sophisticated procedure with maximal neurovascular preservation. Principles of blood supply of the abdominal flap laid out in the early days of liposuction assisted abdominoplasty may be reviewed along with modern descriptions of the LABP before adopting this technique.[26,27] Cannula size should not exceed 4 mm diameter.
Chronic seromas have a well-formed pseudocapsule and are best managed by re-excision and obliteration of the cavity by sutures. Autologous fibrin glue has also been used for this.[28]
Haemostasis issues
The incidence of these complications varies in different series, being lowest where vasoconstrictors are used.[29] There is no evidence that infusion of tumescent solution before flap elevation adversely affects tissue viability or compromises the ability to see potential bleeders.[30] It is however important to securely tie or clip the lower rectus sheath perforators. This step eliminates the chance for retraction and rectus sheath haematomas later. Super-wet infusion is a routine step in LABP and the author has used it for 17 years without adverse incident. The haematoma rate is 2% (4 in 200 cases; 1 female hypertensive, 2 male post-bariatric and 1 asthmatic) in his consecutive series. Hypertensives, male sex and post weight-loss surgery (WLS) patients are at higher risk of haematoma.[31,32] Flap elevation using diathermy reduces bleeding and operative time.[23]
Ischaemic complications
I have listed skin necrosis, fat necrosis and combined skin-fat necrosis under ischaemic complications because that is what they are and not a mysterious event after abdominoplasty. All plastic surgeons know that flap necrosis is due to flap ischaemia. In an abdominoplasty, the skin necrosis declares itself by 2nd to 4th day. It is seen as an area of darkness or blood stained blister in the leading edge of the flap. It is often a combined skin-fat necrosis where the skin component is but the tip of the iceberg. This is soon followed by a firm induration in the subcutaneous tissues of the lower abdomen (around the skin ischaemia), indicative of fat necrosis. Often, wound dehiscence or other wound problems follow [Figure 1].
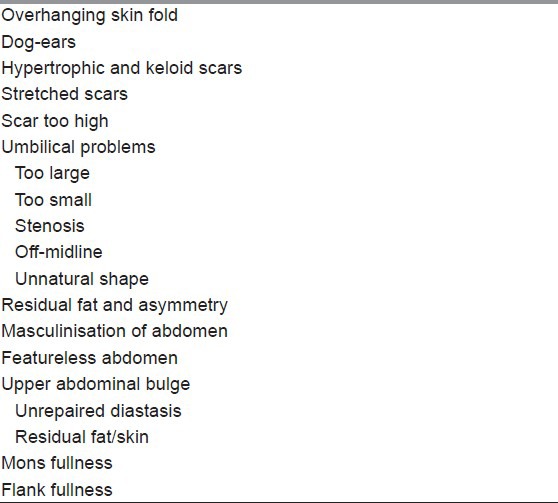
Figure 1.
Ischaemic and wound healing complications. (a) Necrosis of the skin edge with much bigger volume of fat necrosis and seroma, note necrosis of umbilicus as well, (b) Dehiscence of inverted T junction with evident tension in closure and unsatisfactory umbilicoplasty
Flap ischaemia is multifactorial. In traditional abdominoplasty dissection, the flap is undermined all the way until the costal margin; the periumbilical perforators and the smaller vessels arising out of the flat muscles are cut.[26] The flap now relies only on the intercostal perforators at costal margins and the vessels reaching from the lumbar flank. This blood supply has to cross two vascular zones to reach the flap tip. The lower midline is the farthest from blood supply and hence most prone for ischaemia. Tension in skin closure further aggravates ischaemia.
Logical steps to prevent flap ischaemia would be: Minimising the devascularisation to the absolute minimum required for flap mobilisation, using discontinuous dissection and using lipomobilisation more than surgical undermining. Every attempt should be made to preserve the periumbilical perforators especially in the obese abdomens.[33] These perforators of the rectus vascular axis can sustain large transverse rectus abdominis myocutaneous flaps and can feed the entire anterior abdominal wall.[34] Especially in obese abdomens, considerable ‘swing’ of these vascular pedicles can be achieved after liposuction so that the skin slides caudally, still fed by these vessels. Vessels division, when done, should be closer to their origin so as to preserve the superficial anastomoses and choke vessels. Progressive tension sutures are strongly recommended as they distribute the tension over a wide area and relieve tension on the closure line. Adequate hydration of the patient, avoiding very tight compressive garments, maintaining a normal systolic blood pressure and avoiding a cold environment are important as well.
Tobacco consuming habit is assumed to increase risk of flap ischaemia. However, surprisingly, objective data is lacking on the excess risk in smokers. Caution is still needed to encourage smokers to quit for 3 weeks before and after surgery.[35]
Nerve problems
Large areas of hypoaesthesia follow traditional abdominoplasty.[36] With selective undermining, it is possible to maintain nerve connections from the upper rectus sheath and linea semilunaris as well as the perforating branches from the oblique muscles. The nerve fibres accompany the vascular perforators. With this technique, the abdomen remains sensate and this is borne out by the authors’ experience as well.
Rarely, the lateral cutaneous nerve (of thigh) gets caught in a stitch near the anterior superior iliac spine, leading to a vexing pain.[31] This can be avoided by extra care in this area. Femoral neuropathy and prolonged sciatic neuropathy with paralysis have also been reported.[37,38] The sciatic nerve palsy occurred in two patients of simultaneous inner thigh plasty and abdominoplasty and is possibly related to extreme abduction of the hip along with Fowler's position.[37]
Excessive pain and abdominal compartment syndromes
Proper repair of midline divarication can be achieved with anatomical restoration alone, without resorting to unphysiological, aggressive inverting sutures. It is sufficient to take wide bites incorporating the anterior rectus sheath and linea alba (without taking the muscle) at least 1.5 cm away from the medial border and to place the stitches 1-2 cm apart in a continuous loop manner. Most series recommend long absorbing polydiaoxanone type of sutures. The author prefers to reinforce the lower half by additional interrupted sutures of No. 2 ethibond empirically. An attempt must be made to capture the firm tendinous intersections of the rectus muscle through the anterior sheath [Figure 2]. Creating excessive plication is unphysiological and is associated with pain and prolonged convalescence. It forces the diaphragm up by raising the intra-abdominal pressure.[39]
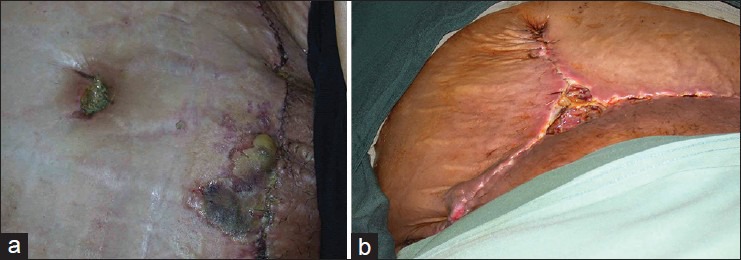
Figure 2.
Schematic diagrams of rectus sheath turn-over and external oblique aponeurosis release techniques. Upper left panel: Cross sections, upper showing diastasis recti and lower showing incisions for rectus sheath turn-over (thin arrow) and external oblique release (thick arrow). Upper right panel: Front view of the same; solid red line depicts rectus sheath turn-over and broken red line the external oblique release. Lower left panel: Cross sections, upper showing rectus sheath turn-over flaps sutured and lower showing the reinforcement of the tendinous intersections. Lower right panel: Frontal view of the same
It is a common practice to onlay a prosthetic mesh in cases of wide diastasis. The author favours just anatomical restoration using specific methods to reduce tension even in wide closures and has been successful in avoiding a mesh. The author recommends an inlay pre-peritoneal mesh if the muscles are very weak. Component separation method has been successful in very large ventral hernia defects.[40,41] The author has modified and simplified this to suit the defects found in abdominoplasties. Two ‘tricks’ may be used [Figure 2]. In the first, medially hinged turn-over flaps of anterior rectus sheath are created from both sides and sutured in the midline to get as narrow a midline as possible without tension. The sutures must incorporate the tendinous intersections of the rectus muscles. At the end of this, the recti muscles come together surprisingly easily and may be approximated with a running suture. A dynamic restoration is thus achieved. The second method uses long bilateral release incisions in the external oblique aponeurosis immediately lateral to the linea semilunaris. This can be done in a closed manner by sliding one jaw of a long metzenbaum type scissors through a small cut in the aponeurosis up and down in an avascular plane and cutting the layer easily. Freed from the lateral pull of the external obliques, the recti come together without tension. Both these incremental methods can be combined and where necessary, the full dissection of the component separation technique can be used as described earlier.[40,41] The lateral abdominal wall is not weakened by this.
Infective issues
Wound infection is a complex topic; it is often multifactorial. Assuming good aseptic technique is followed, the author believes the following steps are important to keep infection rates as low as possible.
Eliminate or rule out co-existing foci of infection elsewhere, especially the umbilicus and genitalia. A routine vaginal culture swab is a good idea
Ensure good skin hygiene with 4% chlorhexidine detergent shower twice prior to the surgery day. Particular attention must be paid to intertriginous areas
Skin preparation with chlorhexidine in alcohol is currently shown to be superior to povidone iodine prep especially for longer surgeries[42]
Meticulous attention to minimise tissue trauma, cautery trauma, drying, tension and dead spaces
Fat necrosis favours late wound infection as it acts as a locus for bacterial multiplication. Measures to prevent flap ischaemia are in order
There is no evidence to support post-operative use of antibiotics. Perioperative single dose prophylactic antibiotic effective against skin flora and coliforms is appropriate.[43]
Necrotising fasciitis is a life threatening, fortunately very rare complication of abdominoplasty.[44] Very quick diagnosis and decisive action in the form of debridement is life-saving. Patient must have access to the surgeon or to a qualified deputy for the first 10 days after an abdominoplasty in case of unexplained sever pain, odour, purulent discharge, redness or fever.
Diabetics have not shown a higher rate of infection after abdominoplasty; however, it is important that they attain the best optimisation of the diabetic status for 2 weeks prior to surgery.[35]
Wound healing issues
Assuming proper surgical wound closure was employed, wound-healing issues should be uncommon. However, several series have reported significantly high rates for wound complications in abdominoplasty especially in post WLS cases.[32,45] Separating isolated wound healing issues from confounding factors of skin tension, ischaemia and undiagnosed fat necrosis is difficult; wound failure is often multifactorial [Figure 3]. However, a robust vascularity of the flap is of over-riding importance for good healing (see ischaemia section above).
Figure 3.

Wound healing complication in a post weight-loss surgery patient who underwent mastopexy and abdominoplasty as a medical tourist. Note dehiscence of breast and abdominal wounds, umbilical malposition, fat necrosis and infection around? Drain sites. Midline scar revision wound is also infected
Ensuring trouble free healing comes down to the basic tenets of tension free closure of wound edges by good technique. Progressive tension sutures eliminate tension on the incision closure. The superior wound edge is always longer than the inferior one, progressive adjustment of this disparity over the entire length of the wound is essential. Proper approximation of Scarpa fascia (present only in the lower flap) to the condensed fat-fascia of the upper flap sets the stage for the next layer. The fat layer is not sutured. Skin may be approximated by deep intradermal monofilament absorbables. Recently, the author has switched to barbed sutures (Quill™, Angiotech Pharmaceuticals, Inc., Vancouver, British Columbia, Canada), which has several advantages, but at a higher cost. A wound closure mesh tape system combined with O-cyanoacrylate paint (Dermabond-Prineo™, Ethibond Inc., Johnson and Johnson) has been shown to give better scars in one prospective study; the author has used this system successfully as well.
Problems like occasional suture sinuses or suture spitting are minor irritants. However, persistent non-healing should prompt a search for underlying fat necrosis, subclinical seromas, edge overlaps or smoldering infection related to deep sutures or prosthetic mesh. Consideration should be given to methicillin-resistant Staphylococcus aureus and atypical mycobacteria.[46,47]
Visceral perforations
Although rare, an undetected bowel perforation can be fatal. Without an index of suspicion, it may be rather late before a bowel perforation is diagnosed; the patient may present to a different facility or doctor with abdominal pain.[48] Bowel perforation is obviously due to a technical error or negligence. Factors that increase the risk are: Co-existing diagnosed or undiagnosed hernia, previous abdominal wall surgeries and visceral obesity with stretched muscles. This last type of patient is not a proper candidate for abdominoplasty anyway. Prevention is by proper case selection, performing the liposuction with the abdomen hyper-extended and taking care during midline plication to avoid bowel impalement. Appropriate investigations must be initiated the case of severe pain or distension to rule out bowel perforation.
General complications
Foremost among these are chest complications and VTE.
Chest complications
Very few studies have addressed the issue of chest complications.[49] Adequate preemptive analgesia by a judicious combination of non-steroidal anti-inflammatory drugs, intravenous titrated patient controlled analgesia, patient education, incentive spirometry and physiotherapy is important to enable the patient to breath well. Perioperative consultation with a chest specialist is recommended in cases of pre-existing respiratory disease.
Recent studies of intra-parietal infusion of local anaesthetics have shown great promise in relieving the pain at the source. Transversus abdominis plane blocks have been shown to offer effective pain relief and reduce the narcotic requirements.[50] The author currently uses continuous infusion of local anaesthetics into the rectus sheath using a special catheter for 24-48 h in cases of extensive muscle plication – this has made a major difference to post-operative pain. Such infusions do not increase infection or seroma rates.[51,52] In simpler cases, a single bolus of 20 ml of 0.25% Bupivacaine is infiltrated inside each rectus sheath.
VTE
VTE is a definite and serious risk factor in abdominoplasty.[53] Risk stratification can be done using Caprini risk assessment model[54] or similar scoring systems in order to decide on appropriate preventive methods. Circumferential abdominoplasty was associated with the highest risk of VTE followed by abdominoplasty combined with an intra-abdominal procedure.[53] Prophylaxes against VTE include graduated compression stockings, intermittent pneumatic compression devices, venous foot pumps and chemoprophylaxis with low molecular weight heparin or low-dose unfractionated heparin.[55] However, the dose should be on the lower range, generally 20 mg of enoxaparin or equivalent daily for a week. The use of direct and indirect factor Xa inhibitors and thrombin inhibitors like Rivaroxaban is contra-indicated as higher bleeding has been reported due to the extensive dissection planes.[56]
Strict adherence to protocol can drastically reduce the risk of VTE as demonstrated in a study of 404 abdominoplasties with 297 high risk and 17 highest risk patients operated over 10 years with only one calf VTE.[57] This can be contrasted with a historical study of abdominoplasty without VTE prophylaxis where the high risk patients with Caprini score >8 had a 11.3% incidence of VTE.[58]
Aesthetic complications
The general satisfaction rate after abdominoplasty is very high.[59] Aesthetic dissatisfaction is commonly voiced by patients, but there are no published studies on this [Table 2]. Avoidance of these complications begins with proper choice of the patient and matching the procedure to the type of abdominoplasty.[24] The abdomen is examined with reference to the flank and contiguous areas of the back. Several important points must be noted: Proportion of parietal and visceral fat, extent of midline divarication, status of the muscles, presence of umbilical hernia or other hernias, extent of upper abdominal skin laxity, native position and orientation of the umbilicus, skeletal features such as the subcostal angle and the vertical distance between costal margin and the upper border of iliac bone. The presence and extent of mons ptosis and bulge must be noted. Patient must be examined in semi-sitting position and a trial approximation of the skin from umbilical level to the lower abdominal crease must be done manually. If this is difficult, it is less likely that the upper abdominal skin will reach the crease incision; hence, the possibility of a lesser resection and separate closure of the umbilical donor hole or a floating umbilicus must be entertained.[60] If tissue laxity is restricted to the lower abdomen, a mini abdominoplasty is suitable.
A patient with a narrow subcostal angle and a long abdomen is more challenging than one with wide angle and closer proximity of the costal margin to pubic bone to realise a “full” abdominoplasty. On the other hand, if the coastal border is close to the upper border of pelvic bone, it is difficult to create a narrow waist and feminine contours, a straighter masculine waist may result especially after removal of the hip rolls – a paradoxical loss of curves. Consideration should also be given to the gluteal contours and simultaneous augmentation by fat graft considered where the area is deficient.
Careful pre-operative marking of the midline, position of the top of the vulval cleft, upper border of the hairy mons triangle and the natural crease line must be done in standing and supine positions. One must ensure that the scar is placed at least 7 cm cranial to the vulval commissure. Over-resection of the hairy mons and cranial traction deformity of the vulva must also be avoided.
The placement of the final scar has to respect the patient's wishes, preferred bikini style and the realities of available redundancy in the upper abdominal skin. However, it must not be too high; although, it makes closure easy. In cases with insufficient skin in the supra-umbilical segment, either a floating umbilicus or a separate closure of the umbilical hole with an additional small transverse scar is preferred to an inverted T; the main scar however must lie inside the bikini markings.
A situation of early commitment to a low incision and excessive resection ending up in a disastrous skin shortage must be avoided at all cost. Vest-over-pants technique and a willingness to close the umbilical donor hole separately if required, can avoid excessive tension at closure.[61] Lateral tilts of the operating table and of the patient on the table must be ruled out before skin resection to avoid an asymmetric umbilicus. When paramedian plication of the abdominal fascia is done, care must be taken to equalise the tension on both sides so as not to displace the umbilicus.
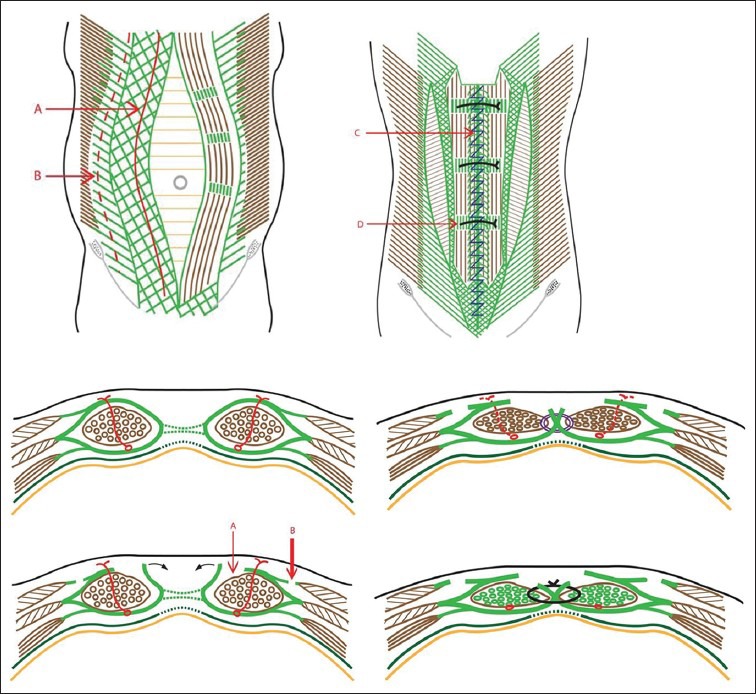
A shapely abdomen is not flat; it has features; gentle bulges and valleys that need to be duplicated during abdominoplasty for achieving a superior result [Figure 4]. Additional liposculpture done at the end can re-create the valleys. Fat grafting of the gluteal and outer gluteal areas is needed to ensure a better waist: hip ratio. Liposuction of the flanks is an important adjunct whether done concurrently or staged. Specific and common issues of discontent are further discussed below.
Figure 4.

Extended scar lipoabdominoplasty and 3D liposculpture. Upper panel front, side and back views before surgery. Lower panel front, oblique and back views 1 month post-operative, a small area of skin overlap has been revised on the right lateral extreme. Note the pleasing features of the abdomen and improvements in waist and back
Dog-ears
The possibility of lateral bulges and dog-ears can be predicted pre-operatively if the patient has a significant degree of hip fat rolls. Preliminary liposuction of these areas in the lateral position eliminates this bulge.[62] Adequate lateral extension of the scar is still needed in patients with skin redundancy on the hip region.[63] Patients usually do not mind an extra-long scar as long as it is flat and well-concealed.
Umbilical problems
A natural looking umbilicus is an inverted truncated cone or an ink-well with a hooding of skin cranially and smooth transition caudally. To simulate this, the following steps are useful.
The new umbilical hole is made 1-2 cm cranial to the surface projection of the umbilical stump. This puts extra traction on the upper abdomen making it flatter and creates a gentle fullness on the lower midline area simulating nature
The extra-long umbilical stalk is ‘telescoped’ by using four-quadrant plicating stitches so that the cicatrix is close to the rectus fascia level
The fat around the new umbilical hole is removed in a shelving manner so that the inner edges have less fat.
A suture from the edge of the neoumbilical hole at 3 and 9’O’ clock position to the rectus sheath inverts the edges inwards
Finally, the skin edges are approximated to the edges of the deep seated umbilicus, always forcing the peripheral skin inwards and centripetally
Circular scar contracture is prevented by breaking up the scar into a wavy pattern.
Upper abdominal fullness
This is due to two reasons: Unrepaired divarication in the upper part and excess residual fat. The former is difficult to correct; so it is important to do a complete plication of the midline muscles (when indicated). The latter can be addressed by secondary liposuction.
Depressed lower midline scar
The skin around the umbilicus is often the thinnest area pre-operatively. This is the skin that comes down to the lower midline leading to a concave deformity. This can be anticipated and prevented by keeping a de-epithelised tongue of tissue projecting from the lower end of the flap and folding this back to double up the thickness of fat here.
Scar problems
Scar hypertrophy and keloid formation are determined by the patient's skin type and surgical technique. Careful pre-operative assessment of skin type and counselling avoids later conflicts. The surgeon can optimise the scar by the following steps: Taking all the tension on the deeper fascia closure, closing the skin accurately with fine suture material (not too close to epidermis), early silicone sheet therapy, fractional ablative laser therapy and early judicious use of intralesional steroids. A stretched scar indicates tension at closure and lack of proper deep closure, a common mistake [Figure 5]. Overhang of upper border is not always preventable but easy to correct under local anaesthetic later. Sometimes a scar revision gives a better chance to start afresh with scar management. The surgeon must actively offer this since most patients are scared of ‘repeat operation’ and fail to anticipate the immense improvement that this simple revision can give.
Figure 5.

Stretched depressed unsightly scar: The net result of poor planning, not performing a deep closure and insufficient separation of umbilicus and scar
Mons fullness
This is an embarrassing outcome if the patient had a fatty mons earlier or gained weight later. It is easily prevented by proper liposuction of this area and incorporating a mons lift during closure. A simultaneous mons lift with upward mobilisation of the lower flap has the added advantage of relieving tension in this crucial area and gives a better aesthesis and comfort to the genital region.
A note on combined surgeries
Patients sometimes request for combining abdominoplasty with other surgeries. Although this topic is outside the scope of this paper, some general observations regarding the potential for complications can be made. Combining Caesarean sections with abdominoplasty is associated with much higher complication rates and aesthetic dissatisfactions and is best avoided.[64] Other gynaecology operations for benign problems may be combined, but with increased possibility for transfusion due to gynaecological indication.[12] The risk of VTE increases when abdominoplasty is combined with intra-abdominal procedures however and chemoprophylaxis and mechanical calf pumps are recommended. The risk is only slightly higher when combined with other aesthetic plastic surgeries, so such combinations are safe. However, circumferential abdominoplasty itself has a high risk of VTE and it may not be prudent to combine it with other surgeries.[53]
CONCLUSION
Several important technical modifications and the concepts of lipoabdominoplasty with selective incremental undermining have been developed over the last 15 years. Careful patient selection, optimisation, risk stratified prophylaxis and meticulous technique using these proven modifications have been shown to reduce the complication rates drastically. Surgeons must be willing to adopt these improvements if these benefits are to percolate to their patients. Accurate record keeping and periodic audit of one's complications must be the responsibility of every surgeon. With so many of the complications ‘solved’ it is no longer justified to do abdominoplasty with high complication rates in any subset of patients. Every complication must lead to introspection and improvement rather than acceptance and dismissal as a ‘known’ complication.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Matarasso A, Swift RW, Rankin M. Abdominoplasty and abdominal contour surgery: A national plastic surgery survey. Plast Reconstr Surg. 2006;117:1797–808. doi: 10.1097/01.prs.0000209918.55752.f3. [DOI] [PubMed] [Google Scholar]
- 2.Momeni A, Heier M, Torio-Padron N, Penna V, Bannasch H, Stark BG. Correlation between complication rate and patient satisfaction in abdominoplasty. Ann Plast Surg. 2009;62:5–6. doi: 10.1097/SAP.0b013e318174f973. [DOI] [PubMed] [Google Scholar]
- 3.Alderman AK, Collins ED, Streu R, Grotting JC, Sulkin AL, Neligan P, et al. Benchmarking outcomes in plastic surgery: National complication rates for abdominoplasty and breast augmentation. Plast Reconstr Surg. 2009;124:2127–33. doi: 10.1097/PRS.0b013e3181bf8378. [DOI] [PubMed] [Google Scholar]
- 4.Brauman D, Capocci J. Liposuction abdominoplasty: An advanced body contouring technique. Plast Reconstr Surg. 2009;124:1685–95. doi: 10.1097/PRS.0b013e3181b98c5d. [DOI] [PubMed] [Google Scholar]
- 5.Beer GM, Wallner H. Prevention of seroma after abdominoplasty. Aesthet Surg J. 2010;30:414–7. doi: 10.1177/1090820X10374116. [DOI] [PubMed] [Google Scholar]
- 6.Zuelzer HB, Ratliff CR, Drake DB. Complications of abdominal contouring surgery in obese patients: Current status. Ann Plast Surg. 2010;64:598–604. doi: 10.1097/SAP.0b013e3181cf9f9e. [DOI] [PubMed] [Google Scholar]
- 7.Stewart KJ, Stewart DA, Coghlan B, Harrison DH, Jones BM, Waterhouse N. Complications of 278 consecutive abdominoplasties. J Plast Reconstr Aesthet Surg. 2006;59:1152–5. doi: 10.1016/j.bjps.2005.12.060. [DOI] [PubMed] [Google Scholar]
- 8.Starling J, 3rd, Thosani MK, Coldiron BM. Determining the safety of office-based surgery: What 10 years of Florida data and 6 years of Alabama data reveal. Dermatol Surg. 2012;38:171–7. doi: 10.1111/j.1524-4725.2011.02206.x. [DOI] [PubMed] [Google Scholar]
- 9.Le Louarn C, Pascal JF. The high-superior-tension technique: Evolution of lipoabdominoplasty. Aesthetic Plast Surg. 2010;34:773–81. doi: 10.1007/s00266-010-9551-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Najera RM, Asheld W, Sayeed SM, Glickman LT. Comparison of seroma formation following abdominoplasty with or without liposuction. Plast Reconstr Surg. 2011;127:417–22. doi: 10.1097/PRS.0b013e3181f95763. [DOI] [PubMed] [Google Scholar]
- 11.Neaman KC, Armstrong SD, Baca ME, Albert M, Vander Woude DL, Renucci JD. Outcomes of traditional cosmetic abdominoplasty in a community setting: A retrospective analysis of 1008 patients. Plast Reconstr Surg. 2013;131:403e–10. doi: 10.1097/PRS.0b013e31827c6fc3. [DOI] [PubMed] [Google Scholar]
- 12.Sinno S, Shah S, Kenton K, Brubaker L, Angelats J, Vandevender D, et al. Assessing the safety and efficacy of combined abdominoplasty and gynecologic surgery. Ann Plast Surg. 2011;67:272–4. doi: 10.1097/SAP.0b013e3181f9b245. [DOI] [PubMed] [Google Scholar]
- 13.Heller JB, Teng E, Knoll BI, Persing J. Outcome analysis of combined lipoabdominoplasty versus conventional abdominoplasty. Plast Reconstr Surg. 2008;121:1821–9. doi: 10.1097/PRS.0b013e31816b1350. [DOI] [PubMed] [Google Scholar]
- 14.Antonetti JW, Antonetti AR. Reducing seroma in outpatient abdominoplasty: Analysis of 516 consecutive cases. Aesthet Surg J. 2010;30:418–25. doi: 10.1177/1090820X10372048. [DOI] [PubMed] [Google Scholar]
- 15.Koller M, Hintringer T. Scarpa fascia or rectus fascia in abdominoplasty flap elevation: A prospective clinical trial. Aesthetic Plast Surg. 2012;36:241–3. doi: 10.1007/s00266-011-9795-8. [DOI] [PubMed] [Google Scholar]
- 16.Baroudi R, Ferreira CA. Seroma: How to avoid it and how to treat it. Aesthet Surg J. 1998;18:439–41. doi: 10.1016/s1090-820x(98)70073-1. [DOI] [PubMed] [Google Scholar]
- 17.Arantes HL, Rosique RG, Rosique MJ, Mélega JM. The use of quilting suture in abdominoplasty does not require aspiratory drainage for prevention of seroma. Aesthetic Plast Surg. 2010;34:102–4. doi: 10.1007/s00266-009-9453-6. [DOI] [PubMed] [Google Scholar]
- 18.Pollock TA, Pollock H. No-drain abdominoplasty with progressive tension sutures. Clin Plast Surg. 2010;37:515–24. doi: 10.1016/j.cps.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 19.Costa-Ferreira A, Rebelo M, Silva A, Vásconez LO, Amarante J. Scarpa fascia preservation during abdominoplasty: Randomized clinical study of efficacy and safety. Plast Reconstr Surg. 2013;131:644–51. doi: 10.1097/PRS.0b013e31827c704b. [DOI] [PubMed] [Google Scholar]
- 20.Pollock TA, Pollock H. Progressive tension sutures in abdominoplasty: A review of 597 consecutive cases. Aesthet Surg J. 2012;32:729–42. doi: 10.1177/1090820X12452294. [DOI] [PubMed] [Google Scholar]
- 21.Andrades P, Prado A, Danilla S, Guerra C, Benitez S, Sepulveda S, et al. Progressive tension sutures in the prevention of postabdominoplasty seroma: A prospective, randomized, double-blind clinical trial. Plast Reconstr Surg. 2007;120:935–46. doi: 10.1097/01.prs.0000253445.76991.de. [DOI] [PubMed] [Google Scholar]
- 22.Roje Z, Roje Z, Karanović N, Utrobicić I. Abdominoplasty complications: A comprehensive approach for the treatment of chronic seroma with pseudobursa. Aesthetic Plast Surg. 2006;30:611–5. doi: 10.1007/s00266-004-0142-1. [DOI] [PubMed] [Google Scholar]
- 23.Araco A, Sorge R, Overton J, Araco F, Gravante G. Postbariatric patients undergoing body-contouring abdominoplasty: Two techniques to raise the flap and their influence on postoperative complications. Ann Plast Surg. 2009;62:613–7. doi: 10.1097/SAP.0b013e3181856d85. [DOI] [PubMed] [Google Scholar]
- 24.Matarasso A. Abdominolipoplasty: A system of classification and treatment for combined abdominoplasty and suction-assisted lipectomy. Aesthetic Plast Surg. 1991;15:111–21. doi: 10.1007/BF02273843. [DOI] [PubMed] [Google Scholar]
- 25.Rangaswamy M. Lipoabdominoplasty: A versatile and safe technique for abdominal contouring. Indian J Plast Surg. 2008;41:S48–55. [PMC free article] [PubMed] [Google Scholar]
- 26.Matarasso A. Liposuction as an adjunct to a full abdominoplasty revisited. Plast Reconstr Surg. 2000;106:1197–202. doi: 10.1097/00006534-200010000-00035. [DOI] [PubMed] [Google Scholar]
- 27.Saldanha OR, Federico R, Daher PF, Malheiros AA, Carneiro PR, Azevedo SF, et al. Lipoabdominoplasty. Plast Reconstr Surg. 2009;124:934–42. doi: 10.1097/PRS.0b013e3181b037e3. [DOI] [PubMed] [Google Scholar]
- 28.di Summa PG, Wettstein R, Erba P, Raffoul W, Kalbermatten DF. Scar asymmetry after abdominoplasty: The unexpected role of seroma. Ann Plast Surg Epub ahead of print. 2012 Nov 8; doi: 10.1097/SAP.0b013e3182503ad9. [DOI] [PubMed] [Google Scholar]
- 29.Hafezi F, Nouhi A. Safe abdominoplasty with extensive liposuctioning. Ann Plast Surg. 2006;57:149–53. doi: 10.1097/01.sap.0000215246.49308.17. [DOI] [PubMed] [Google Scholar]
- 30.Trussler AP, Kurkjian TJ, Hatef DA, Farkas JP, Rohrich RJ. Refinements in abdominoplasty: A critical outcomes analysis over a 20-year period. Plast Reconstr Surg. 2010;126:1063–74. doi: 10.1097/PRS.0b013e3181e60537. [DOI] [PubMed] [Google Scholar]
- 31.van Uchelen JH, Werker PM, Kon M. Complications of abdominoplasty in 86 patients. Plast Reconstr Surg. 2001;107:1869–73. doi: 10.1097/00006534-200106000-00037. [DOI] [PubMed] [Google Scholar]
- 32.Staalesen T, Olsén MF, Elander A. Complications of abdominoplasty after weight loss as a result of bariatric surgery or dieting/postpregnancy. J Plast Surg Hand Surg. 2012;46:416–20. doi: 10.3109/2000656X.2012.717898. [DOI] [PubMed] [Google Scholar]
- 33.Graf R, de Araujo LR, Rippel R, Neto LG, Pace DT, Cruz GA. Lipoabdominoplasty: Liposuction with reduced undermining and traditional abdominal skin flap resection. Aesthetic Plast Surg. 2006;30:1–8. doi: 10.1007/s00266-004-0084-7. [DOI] [PubMed] [Google Scholar]
- 34.Rieger UM, Aschwanden M, Schmid D, Kalbermatten DF, Pierer G, Haug M. Perforator-sparing abdominoplasty technique in the presence of bilateral subcostal scars after gastric bypass. Obes Surg. 2007;17:63–7. doi: 10.1007/s11695-007-9007-4. [DOI] [PubMed] [Google Scholar]
- 35.Karthikesalingam A, Kitcat M, Malata CM. Abdominoplasty in patients with and without pre-existing scars: A retrospective comparison. J Plast Reconstr Aesthet Surg. 2011;64:369–74. doi: 10.1016/j.bjps.2010.05.025. [DOI] [PubMed] [Google Scholar]
- 36.Lapid O, Plakht Y, van der Horst CM. Prospective evaluation of the sensory outcome following abdominoplasty. Ann Plast Surg. 2009;63:597–9. doi: 10.1097/SAP.0b013e318196cc19. [DOI] [PubMed] [Google Scholar]
- 37.Kiermeir D, Banic A, Rösler K, Erni D. Sciatic neuropathy after body contouring surgery in massive weight loss patients. J Plast Reconstr Aesthet Surg. 2010;63:e454–7. doi: 10.1016/j.bjps.2009.07.022. [DOI] [PubMed] [Google Scholar]
- 38.Pechter EA, Smith PB. Transient femoral neuropathy after abdominoplasty. Ann Plast Surg. 2008;61:492–3. doi: 10.1097/SAP.0b013e31816c5cbe. [DOI] [PubMed] [Google Scholar]
- 39.Huang GJ, Bajaj AK, Gupta S, Petersen F, Miles DA. Increased intraabdominal pressure in abdominoplasty: Delineation of risk factors. Plast Reconstr Surg. 2007;119:1319–25. doi: 10.1097/01.prs.0000254529.51696.43. [DOI] [PubMed] [Google Scholar]
- 40.Ramirez OM, Ruas E, Dellon AL. “Components separation” method for closure of abdominal-wall defects: An anatomic and clinical study. Plast Reconstr Surg. 1990;86:519–26. doi: 10.1097/00006534-199009000-00023. [DOI] [PubMed] [Google Scholar]
- 41.DiBello JN, Jr, Moore JH., Jr Sliding myofascial flap of the rectus abdominus muscles for the closure of recurrent ventral hernias. Plast Reconstr Surg. 1996;98:464–9. doi: 10.1097/00006534-199609000-00016. [DOI] [PubMed] [Google Scholar]
- 42.Darouiche RO, Wall MJ, Jr, Itani KM, Otterson MF, Webb AL, Carrick MM, et al. Chlorhexidine-alcohol versus povidone-iodine for surgical-site antisepsis. N Engl J Med. 2010;362:18–26. doi: 10.1056/NEJMoa0810988. [DOI] [PubMed] [Google Scholar]
- 43.Sevin A, Senen D, Sevin K, Erdogan B, Orhan E. Antibiotic use in abdominoplasty: Prospective analysis of 207 cases. J Plast Reconstr Aesthet Surg. 2007;60:379–82. doi: 10.1016/j.bjps.2006.06.025. [DOI] [PubMed] [Google Scholar]
- 44.Araco A, Araco F, Abdullah P, Overton J, Gravante G. Pseudomonas aeruginosa necrotizing infection of the abdominal flap in a post-bariatric patient undergoing body contouring surgery. Obes Surg. 2009;19:812–6. doi: 10.1007/s11695-008-9730-5. [DOI] [PubMed] [Google Scholar]
- 45.Greco JA, 3rd, Castaldo ET, Nanney LB, Wendel JJ, Summitt JB, Kelly KJ, et al. The effect of weight loss surgery and body mass index on wound complications after abdominal contouring operations. Ann Plast Surg. 2008;61:235–42. doi: 10.1097/SAP.0b013e318166d351. [DOI] [PubMed] [Google Scholar]
- 46.Araco A, Zaccheddu R, Araco F, Gravante G. Methicillin-resistant superinfection of the wound after body-contouring abdominal surgery. Aesthetic Plast Surg. 2008;32:681–3. doi: 10.1007/s00266-008-9177-z. [DOI] [PubMed] [Google Scholar]
- 47.Furuya EY, Paez A, Srinivasan A, Cooksey R, Augenbraun M, Baron M, et al. Outbreak of Mycobacterium abscessus wound infections among “lipotourists” from the United States who underwent abdominoplasty in the Dominican Republic. Clin Infect Dis. 2008;46:1181–8. doi: 10.1086/529191. [DOI] [PubMed] [Google Scholar]
- 48.Mallappa M, Rangaswamy M, Badiuddin MF. Small intestinal perforation and peritonitis after liposuction. Aesthetic Plast Surg. 2007;31:589–92. doi: 10.1007/s00266-007-0050-2. [DOI] [PubMed] [Google Scholar]
- 49.Tercan M, Bekerecioglu M, Dikensoy O, Kocoglu H, Atik B, Isik D, et al. Effects of abdominoplasty on respiratory functions: A prospective study. Ann Plast Surg. 2002;49:617–20. doi: 10.1097/00000637-200212000-00011. [DOI] [PubMed] [Google Scholar]
- 50.Araco A, Pooney J, Araco F, Gravante G. Transversus abdominis plane block reduces the analgesic requirements after abdominoplasty with flank liposuction. Ann Plast Surg. 2010;65:385–8. doi: 10.1097/SAP.0b013e3181cc2a24. [DOI] [PubMed] [Google Scholar]
- 51.Smith MM, Hovsepian RV, Markarian MK, Degelia AL, Paul MD, Evans GR, et al. Continuous-infusion local anesthetic pain pump use and seroma formation with abdominal procedures: Is there a correlation? Plast Reconstr Surg. 2008;122:1425–30. doi: 10.1097/PRS.0b013e3181882013. [DOI] [PubMed] [Google Scholar]
- 52.Hovsepian RV, Smith MM, Markarian MK, Sahba K, Paul MD, Evans GR, et al. Infection risk from the use of continuous local-anesthetic infusion pain pumps in aesthetic and reconstructive abdominal procedures. Ann Plast Surg. 2009;62:237–9. doi: 10.1097/SAP.0b013e31817fe4a2. [DOI] [PubMed] [Google Scholar]
- 53.Hatef DA, Trussler AP, Kenkel JM. Procedural risk for venous thromboembolism in abdominal contouring surgery: A systematic review of the literature. Plast Reconstr Surg. 2010;125:352–62. doi: 10.1097/PRS.0b013e3181c2a3b4. [DOI] [PubMed] [Google Scholar]
- 54.Hatef DA, Kenkel JM, Nguyen MQ, Farkas JP, Abtahi F, Rohrich RJ, et al. Thromboembolic risk assessment and the efficacy of enoxaparin prophylaxis in excisional body contouring surgery. Plast Reconstr Surg. 2008;122:269–79. doi: 10.1097/PRS.0b013e3181773d4a. [DOI] [PubMed] [Google Scholar]
- 55.Reish RG, Damjanovic B, Colwell AS. Deep venous thrombosis prophylaxis in body contouring: 105 consecutive patients. Ann Plast Surg. 2012;69:412–4. doi: 10.1097/SAP.0b013e31824a45e0. [DOI] [PubMed] [Google Scholar]
- 56.Dini GM, Ferreira MC, Albuquerque LG, Ferreira LM. How safe is thromboprophylaxis in abdominoplasty? Plast Reconstr Surg. 2012;130:851e–7. doi: 10.1097/PRS.0b013e31826d9fc0. [DOI] [PubMed] [Google Scholar]
- 57.Somogyi RB, Ahmad J, Shih JG, Lista F. Venous thromboembolism in abdominoplasty: A comprehensive approach to lower procedural risk. Aesthet Surg J. 2012;32:322–9. doi: 10.1177/1090820X12438896. [DOI] [PubMed] [Google Scholar]
- 58.Pannucci CJ, Bailey SH, Dreszer G, Wachtman CF, Zumsteg JW, Jaber RM, et al. Validation of the Caprini risk assessment model in plastic and reconstructive surgery patients. J Am Coll Surg. 2011;212:105–12. doi: 10.1016/j.jamcollsurg.2010.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Staalesen T, Elander A, Strandell A, Bergh C. A systematic review of outcomes of abdominoplasty. J Plast Surg Hand Surg. 2012;46:139–44. doi: 10.3109/2000656X.2012.683794. [DOI] [PubMed] [Google Scholar]
- 60.Chin SH, Martin WJ, Matarasso A. Do waistline and umbilical position really change after abdominoplasty? Plast Reconstr Surg. 2010;125:27e–8. doi: 10.1097/PRS.0b013e3181c2a2e9. [DOI] [PubMed] [Google Scholar]
- 61.Bracaglia R, Tambasco D, D’Ettorre M, Gentileschi S. “Inverted-Y”: A modified vest-over-pants abdominoplasty pattern following bariatric surgery. Aesthetic Plast Surg. 2012;36:1179–85. doi: 10.1007/s00266-012-9956-4. [DOI] [PubMed] [Google Scholar]
- 62.Rieger UM, Erba P, Wettstein R, Schumacher R, Schwenzer-Zimmerer K, Haug M, et al. Does abdominoplasty with liposuction of the love handles yield a shorter scar? An analysis with abdominal 3D laser scanning. Ann Plast Surg. 2008;61:359–63. doi: 10.1097/SAP.0b013e31816d824a. [DOI] [PubMed] [Google Scholar]
- 63.Mejia JA, Cárdenas Castellanos YA. Extended abdominoplasty: Applications and a new classification system for abdominoplasty. Aesthetic Plast Surg. 2012;36:278–84. doi: 10.1007/s00266-011-9818-5. [DOI] [PubMed] [Google Scholar]
- 64.Ali A, Essam A. Abdominoplasty combined with cesarean delivery: Evaluation of the practice. Aesthetic Plast Surg. 2011;35:80–6. doi: 10.1007/s00266-010-9563-1. [DOI] [PubMed] [Google Scholar]


