Abstract
Deformities of the hands are a fairly common sequel of burn especially in the developing world. This is because of high incidence of burns, limited access to standard treatment and rehabilitation. The best outcome of a burnt hand is when deformities are prevented from developing. A good functional result is possible when due consideration is paid to hands during resuscitation, excisional surgery, reconstructive surgery and physiotherapy. The post-burns deformities of hand develop due direct thermal damage or secondary to intrinsic minus position due to oedema or vascular insufficiency. During the acute phase the concerns are, maintenance circulation minimize oedema prevent unphysiological positioning and wound closure with autogenous tissue as soon as possible. The rehabilitation program during the acute phase starts from day one and goes on till the hand has healed and has regained full range of motion. Full blown hand contractures are challenging to correct and become more difficult as time passes. Long-standing cases often land up with attenuation of extensor apparatus leading to swan neck and boutonniere deformity, muscle shortening and bony ankylosis. The major and most common pitfall after contracture release is relapse. The treatment protocol of contracture is solely directed towards countering this tendency. This article aims to guide a surgeon in obtaining optimal hand function and avoid pit falls at different stages of management of hand burns. The reasons of an unfavourable outcome of a burnt hand are possible lack of optimal care in the acute phase, while planning and performing reconstructive procedure and during aftercare and rehabilitation.
KEY WORDS: PBC hand, complications, deformity
INTRODUCTION
Post-burn deformity of hand is devastating for patients. The functional disability affects daily activities of the patients and renders them professionally incapable. Deformities of the hands are a fairly common sequel of burn especially in the developing world. This is because of high incidence of burns, limited access to standard treatment and rehabilitation. The best outcome of a burnt hand is when deformities are prevented from developing. So the key to make a burnt hand functional is to prevent the need of reconstructive procedure later on. So a focused attention on hand burn is warranted from day one of the injury. A good functional result is possible when due consideration is paid to hands during resuscitation, excisional surgery, reconstructive surgery and physiotherapy. A sound knowledge of the pathogenesis of hand deformity is important in managing these cases.
PATHOGENESIS
The post-burns deformities of hand develop due direct thermal damage or secondary to intrinsic minus position due to oedema or vascular insufficiency. In case there is thermal injury to the hands the severity of the deformity will depend upon the depth of burn. It has been reported that normal hand function is achieved in 97% of patients in case the burn is superficial whereas in cases with deep burns only 81% regained normal function.[1] The degree of contracture depends upon the amount of skin loss due to deep burns, which heals by contraction. During the initial phase of the injury the lax dorsal skin allows oedema fluid to accumulate. This puts the hand in functionally negative position of wrist flexion, metacarpophalangeal joint extension, proximal interphalangeal joint flexion and adduction of the thumb. This is the genesis of crippling dorsal contracture with contracted first web and boutonniere deformity of fingers. The hand can suffer vascular insufficiency due to direct thermal damage, electrical contact burn and secondary to compartment syndrome either due thick eschar proximally or oedema under the unyielding palmar skin. Intrinsic damage due to compartment syndrome leads to swan neck deformity and contracted first web space.
This article aims to guide a surgeon in obtaining optimal hand function and avoid pit falls at different stages of management of hand burns. The reasons of an unfavorable outcome of a burnt hand are possible lack of optimal care in the acute phase, while planning and performing reconstructive procedure and during aftercare and rehabilitation.
ACUTE PHASE
Hand burn per se irrespective of the total percentage of burns is categorized as major burn and an indication for admission.[2] Although isolated superficial burns of hand with no possibility of development of deformity can be managed on an outpatient basis while assessing the patient a focused attention must paid to the affected hand. One must note the depth of burn, severity of oedema, attitude of the hand, distal circulation and any associated injury like fracture or soft-tissue injury. One must have a high level of suspicion in suspecting compartment syndrome leading to intrinsic muscle ischemia and distal vascular compromise. Circulation of the hand is best maintained by preventing oedema and preventing occlusion of microcirculation. The former can be achieved by the number of means like cooling of the part in the first 30 min and elevation of hand. Infusion of colloids after first 24 h also reduces oedema. If the oedema is kept to the minimum the unphysiological position is corrected to a large extent and a ball bandage with metacarpophalangeal joint joint in 70° flexion and interphalangeal joint joints in 10-15° of flexion, can tackle the rest. If there is circumferential deep dermal or full thickness burns in the arm, forearm or the hand escharotomy is indicated in case there is distal vascular compromise. The decision is solely based on clinical suspicion and should be done in anticipation rather than when florid signs ischemia set in. The escharotomy incision must start proximally and should extend into normal tissue. If the perfusion does not improve with incisions in the arm and forearm they are extended into the hand and digits.[3] In case there is suspicion of compartment syndrome of the intrinsic muscles it can be confirmed by Finochietto's intrinsic tightness test, in which it is difficult to flex the PIP joint with the MP joint in hyperextension as the contracted interossei prevent flexion of PIP. But in most cases escharotomy is done in anticipation as the small intrinsic muscles are prone to ischemia. All the interosseous compartments, the Guyon's and carpal tunnel are decompressed.[3] After decompression the haemostasis is achieved and the hand is dressed in ample padding and mild compression. The position of the hand is wrist at 30° dorsiflexion, MP joints at 70° flexion and IP joints in extension [Figure 1].
Figure 1.

Splintage of burned hand in functional position
The next approach to the burnt hand is to achieve wound closure with autogenous tissue as soon as possible. Operative intervention is more frequently warranted in cases of dorsal burns than those of the palm.[4] The intervention for wound closure depends upon the depth of burn. Second degree superficial burns heal within 15 days and no intervention is required other than moist antiseptic dressing. Deep dermal burns take longer time to heal and heal by both contraction and epithelialization. The options in these cases are either early excision and grafting or non-operative treatment with antiseptic dressing and aggressive physical therapy. Two prospective randomized control trails have proven that for deep dermal burn both operative and conservative approach can give good functional result.[5] What is more important is to prevent poor hand posture, minimize oedema, splinting and systematic exercise regimen. For full thickness burns, the options are either early excision and grafting or delayed grafting on granulation after spontaneous eschar separation. The result of both the treatment modalities are equally bad.[4,5] But early excision and grafting can reduce the morbidity to a large extent. Again maintenance of hand in functional position and early mobilization with a structured physical therapy are keys to optimal hand function.
If early excision and grafting is chosen as a modality either for deep dermal or full thickness burn, hand must get the priority over other areas. More over intermediate thickness sheet grafts are preferred over thin meshed grafts to minimize contraction. While applying graft maximum skin should be fed by accentuating the defect by positioning the MP joints, in extension in case volar aspects is resurfaced and in flexion in case dorsum is grafted. Darts of grafts should be fed into the web space to prevent webbing and syndactalisation.[6] Efforts should be made to achieve 100% graft take in order to minimize healing time so that mobilization can be started at the earliest. To achieve this meticulous haemostasis, absolute immobilization and optimum asepsis are important.
The rehabilitation program during the acute phase starts from day one and goes on till the hand has healed and has regained full range of motion. During the immediate post-burn phase the focus is to counter the unphysiological posture of comfort and put the hand in functional position and minimize the oedema. Initially when the oedema is more a ball bandage with elevation is enough. Once the oedema subsides a formal splint to keep the hand in functional position can be used. Mobilization is started once the oedema subsides the patient is stable and cooperative. Adequate pain relief is mandatory. Initially all the joints are passively moved once a day and gradually active movement is encouraged. In cases where the wounds are allowed to heal spontaneously the rehabilitation regimen include passive stretching of healing skin, maintenance of the full range of motion and preservation of motor skills. This promotes functional independence and strengthens the muscles. When early excision and grafting is done the mobilization starts soon after the graft takes but instead of passive stretching active finger movement is encouraged. This prevents the graft from shearing. Later when the graft consolidates the same regimen can be followed.[7]
POST-BURN HAND DEFORMITY
In cases where the hand burn is not treated as described in the previous section the patient presents with non-functional hand with inadequate skin cover with fixed contracture either intrinsic minus or flexed position. Such deformities are challenging to correct and become more difficult as time passes. Long-standing cases often land up with attenuation of extensor apparatus leading to swan neck and boutonniere deformity, muscle shortening and bony ankylosis [Figure 2]. Hence they should be corrected at the earliest. Even if the patient cannot be operated the existing joint movement must be maintained, stretching should be done where possible to counter muscle shortening and further damage to the extensors is prevented by corrective splints.[8,9]
Figure 2.

Post-burn contracture hand with secondary swan neck deformity
The first step in addressing this problematic deformity is a structured and meticulous assessment. A stepwise assessment of each deformity, degree of loss of function and tissue deficit must be recorded. Photographic records, radiographs and Doppler vascular studies are also done when indicated. Ultimately the deformities and losses are enumerated and correlated to anatomic structures and reconstructive plan is conceived. It is important to determine whether the contracture is solely due to post-burn scar or has bony ankylosis and muscle shortening contributing to it. This aspect has lot of bearing on the prognosis and the treatment modality. Along with this the patient is psychologically evaluated to grasp the expectation of the patient and to evaluate his or her compliance to physiotherapy.[10] It is very important to make the patient realistic about the possible outcome of the reconstructive procedure and at the same convince him or her the importance of post-operative physiotherapy. The ultimate goal is to restore the patient to his or her pre-burn vocation and life-style. So, it is important to understand and integrate the professional requirement of patient in the reconstructive plan.
The severity of hand contracture has been graded into four grades by McCauley and given in Table 1.[11] The grading system is useful as it integrates anatomical deformity with functional deficit. This gives a very objective way of evaluation of hand contracture and is useful in predicting the prognosis after surgery. The major and most common pitfall after contracture release is relapse.[12] The treatment protocol of contracture is solely directed towards countering this tendency [Figures 3 and 4]. Although there are many who believe that waiting for scar maturation is not warranted but a general consensus is that the release of contracture should be performed after scar maturation because by then the contractile forces in the scar have subsided.[13,14] The waiting period can be utilized for exercise, stretching of scar and serial splinting.[15] This regimen not only improves the outcome of a subsequent surgery but also obviates operation in 8-15% of cases.[16] There are situations where an early release may be indicated. In cases where waiting may lead to the development of secondary deformities like boutonniere or swan neck deformity or in cases where the contracture scar is unstable and repeatedly breaks down. Early release in the former situation averts further attenuation of extensor apparatus and prevents the development of these deformities. In the latter case instead of an incision release it is wise to excise the whole unstable and immature contracting scar, as it will minimize the relapse to a large extent.
Table 1.
McCauley's classification of burn scar contracture in hand
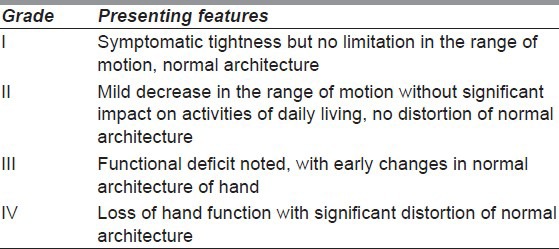
Figure 3.

Relapse of flexion contracture after grafting
Figure 4.

Relapse of extension contracture after grafting
Often these patients have multiple contractures and defects in the body. It is important to operate more than one contracture in one sitting. This approach minimizes anesthetic requirement, reduce the overall cost of treatment and shorten the rehabilitation time.[17] Another thumb rule is to release the proximal contracture first and then proceed distally i.e., the axilla then elbow and then hand.
The goal of contracture release is to achieve a complete release without damaging any vital structure. The incision should be made opposite the joint line from one lateral line to the other.[18] Generally it coincides with the point of maximal tension of the contracting band. Hence the incision is made while keeping the scar maximally stretched. It is convenient to press down the cutting edge of the knife instead of cutting. This way only the tough contracting tissue under tension gets cut and underlying normal soft tissue is safeguarded. The incision is deepened till the full thickness of the scar is divided and healthy tissue is reached. After complete release, the ends of the incision line are fishtailed and the straight line of the edges of the defect is broken by multiple darts. In most cases incision release suffices but excision of scar may be indicated if the scar is depigmented, grossly hypertrophic or unstable with frequent break down.[18,19] These indications are frequent in cases of dorsal contracture. Excision of scar may also be done in cases of dorsal contracture in order to resurface the whole aesthetic unit. Whenever excision of scar is contemplated availability of adequate donor site must be ensure beforehand. The release procedure should be done after infiltration with 1:200,000 adrenaline solutions and under tourniquet control. This gives a bloodless field and ensures that no vital structures are damaged. After release the tourniquet should be deflated and accurate haemostasis must be achieved. If proper haemostasis is not achieved there will hematoma under the graft or flap, which can compromise the graft take and flap survival.
Many a times complete release may not be possible on the table. Such a situation is encountered in cases of severe and longstanding contractures with significant shortening muscle and neurovascular bundle. Forcible release of these contractures lead to exposure of neurovascular bundle and the vessel may go into spasm leading to ischemia. It is important to foresee this scenario pre-operatively so that the patient can be counselled and alternative modality of release may be planned. These contractures can be released gradually with distractors or serial splintage.[19,20] The distractor is applied after a preliminary skin release and the contracture is gradually opened [Figures 5 and 6]. The distractor works with Ilizarov principle where the joint capsule, muscle and neurovascular bundle are simultaneously and gradually stretched. But care should be taken in preventing pin tract infection and joint stiffness, as devise stays in place for a long time.[21] After complete release the defect is resurfaced. Some longstanding contractures especially of fingers land up with bony ankylosis. In these cases arthrodesis of the joint in functional position is a sound option but must be told to the patient preoperatively.
Figure 5.

Severe and longstanding dorsal contracture
Figure 6.

Correction severe dorsal contracture by distractor
Resurfacing of the resultant defect after release is done either with graft or flap. While choosing the modality for resurfacing the reconstructive ladder should be followed. The simplest technique, which meets the reconstructive goal, should be chosen. The modalities of cover in order of increasing complexity are skin grafting, local skin flaps and Z-plasties, local muscle flaps, regional faciocutaneous flaps, distant pedicled flaps and then free flaps.[12]
Most of the raw areas after contracture release have a vascular bed and is possible to skin graft them. It is beyond any doubt that resurfacing with full thickness graft gives superior functional and cosmetic result compared to split thickness graft owing to its minimum secondary contraction and better colour match[22,23] [Figures 7 and 8]. However, the application of full thickness graft is more demanding and one need to be very meticulous in haemostasis and immobilisation, hence is more time consuming. Large full thickness grafts can be harvested from groin and supraclavicular area. But in cases of extensive burn with multiple contractures and paucity of donor sites it is pragmatic to use intermediate thickness split thickness graft. A good donor site for split thickness graft is plantar instep area as it is concealed, has minimum secondary contraction and gives good colour match[24,25] [Figures 9 and 10]. Combined grafting with full thickness graft over the joint and split thickness graft in the rest of the areas is also valid option of resurfacing.[12]
Figure 7.

Contracture release and resurfacing with full thickness skin graft
Figure 8.

Contracture release and resurfacing with split thickness skin graft
Figure 9.

Palmar contracture
Figure 10.

Contracture release and resurfacing with plantar split thickness skin graft
Z-plasty is generally reserved for mild linear contracture of fingers and web-space [Figure 11]. Care should be exercised while raising z-flaps, as they are prone to tip necrosis. To avoid this thick flaps should be elevated and the angle should be 90° instead of 60°.[26]
Figure 11.

Z-plasty for first web space
Flap resurfacing after contracture release is indicated, where vital structures like joints, tendons and neurovascular bundle get exposed and where secondary procedures are contemplated at a later date. Number local flaps have been used for finger and hand contractures viz. transposition flap, advancement flaps, digital island flaps, fillet flaps, lateral or dorsolateral flap, dorsal metacarpal flap, cross finger flap, flag flap and adipofascial flaps.[27–29] The regional flap options are distally based radial artery forearm flap and posterior interosseous flaps.[30–32] While exercising the option of flap for resurfacing one needs to be careful not to limit the amount of release to fit the dimension of a preconceived flap. It important to achieve complete release and chose the flap as per the defect. It is wise to avoid bulky flaps [Figure 12] on hand and thin and pliable flaps like radial artery forearm flaps are preferable [Figure 13].
Figure 12.

Dorsal hand contracture released and resurfaced with bulky groin flap serving no purpose
Figure 13.

Dorsal hand contracture released and resurfaced soft and pliable radial forearm flap allowing full flexion
SPECIAL CONSIDERATION FOR PARTICULAR JOINTS
Metacarpo-phalangeal joint
The basic prerequisite of a functional hand is mobile MP joints. The contracture of MP joints can be either flexion contracture or extension contracture. Result of flexion contracture is quite gratifying and the release procedure is simple as flexion is the position of safety for this joint because the collateral ligaments are in a stretched position in flexion. Most flexion contractures are amenable to skin graft resurfacing. But in long standing cases one needs to be cautious as forceful extension of the joint may cause, spasm of the digital artery. In such situation one should settle for a suboptimal release and achieve the rest with distractor or serial splinting.
The dorsal contracture of MP joints is more challenging deformity to correct. This is because in longstanding severe dorsal contractures the collateral ligaments and the joint capsule get contracted and the extensor muscles get shortened. Secondary boutonniere deformity also develop as the reciprocal flexion of the PIP joint leads to attenuation of central slips and volar displacement of the lateral slips of extensor apparatus resulting in extension of distal interphalangeal (DIP) joint. Graham et al. has given a classification of dorsal contracture of MCP joint:[33]
Type I: >30° of flexion with the wrist in maximal flexion.
Type II: <30° of flexion with the wrist in maximal flexion.
Type III: >30° of hyperextension.
This is a prognostic grading and it is reported that only about 50% cases of Type III regain normal function whereas 95% of Type I had functional improvement.[33]
Hence the deformity of dorsal contracture progressively worsens and should be corrected as early as possible even before scar maturation. The decision regarding resurfacing is taken preoperatively by assessing the quality of dorsal skin and the need for capsulotomy. In case resurfacing with graft is contemplated the release incision should be made an inch proximal to the MP joint so that after release the skin migrates distally over the joints.[34] But where flap is planned this precaution is not required. In cases where skin release does not bring about flexion of MP joint one must proceed to do capsulotomy. It should be done with a No. 11 blade, which is passed on either sides of the MP joint, and the collateral ligaments are released. However, only collateral release may not bring about flexion of the joint as the skin and soft-tissue volar to the joint is tight due to the abnormal claw position. Hence the skin needs to be freed from the volar aspect of the joint, which is done by passing a curved scissors volar to the joint. This facilitates volar rotation of the metacarpal head during MP joint flexion.[34] Following complete release the MP joints are K wired at 90° of flexion and resurfacing is done. It is not always necessary to use a flap even a graft can give a gratifying result provided the extensor tendons are not exposed [Figures 14 and 15]. The commonly used flap is groin flap which should be primarily thinned before in-setting [Figures 16 and 17].
Figure 14.

Severe dorsal contracture hand
Figure 15.

Dorsal contracture released and resurfaced with split skin graft
Figure 16.

Severe dorsal contracture hand
Figure 17.

Dorsal contracture released and resurfaced with groin flap
Some dorsal contractures of MP joints are associated with sever muscle shortening and joint subluxation. Such cases are generally seen in neglected cases where the burn was sustained at a very young age. These cases are best managed by distractors, which are applied after a preliminary skin release.[19] Grafting is done in the second stage after full release.
INTERPHALANGEAL JOINTS
Deformity of the IP joints are flexion contractures, boutonniere deformity, swan neck deformity and extension contracture. Flexion contracture can be either a part of palmar contracture or can be due to reciprocal positioning secondary to dorsal contracture of MP joints.
In cases of primary flexion contracture of IP joints while releasing the neurovascular bundles are at risk and one needs to be cautious. In long standing cases trying to forcibly open up the contracture often tears the flexor sheath exposing the tendons and leads to spasm of the digital arteries. Hence while releasing gradual and sustained force should be applied so that the shortened muscles get lengthened. After the release neurovasucular bundles often tent up but it is possible to graft the area with the help of bolus tie-over dressing.[34] It is also possible that the finger may get ischemic in the post-operative period. This could be either due to injury to the neurovascular bundle or constricting effect of the dressing, which gets compounded by oedema. Hence it is important that the dressing should be compressive and not constricting and should leave some room for subsequent oedema. In some cases the tendons may get exposed and need to be resurfaced with flap. The flap of choice is generally cross finger flap but reverse dorsal metacarpal flap and digital artery island flap can also be used.[28,35]
The flexion contracture of IP joints secondary to dorsal contracture of the MP joints with or without boutonniere deformity are very difficult to correct and are best prevented. This is because of damage to the extensor expansion, unphysiological joint position and poor skin over the dorsal aspect of IP joint. The decision to surgically correct the deformity must be taken judiciously. Unlike the MP joints, which remain stable after capsulotomy because of the interosseous muscles, the IP joints become unstable after collateral ligament release. Hence it is better to arthrodes the joints where the release warrants capsulotomy. The IP joints must be arthrodesed to make the fingers opposable to the thumb, which is fundamental for a functional hand. The recommended angles for arthrodesis of PIP are 25-35° for index, 30-40° for middle, 35-45° for the ring and 40-50° for the little finger.[34] It important to assess the overlying dorsal skin before embarking on the procedure. In case the overlying skin is not favourable it is wise to first excise the scar and resurface with a flap. Also the closure after arthrodesis gets tight as the longitudinal incision ultimately opens up as diamond after bone shortening. Hence it is important to raise flaps from either side to facilitate closure.[34] The desired angle of arthrodesis should be marked as closing wedge with the two limbs on each articular surface and apex dorsally. Alternatively one articular surface is excised transversely and the other transected at the desired angle.[34] The fixation is done with K wire, which is retained for 4-6 weeks. Care should be exercised in osteoporotic bones where multiple passes of the K-wire should be avoided.
If the boutonniere deformity cases are detected early with mobile IP joints and healthy overlying skin, a trial of splinting of PIP in extension with active movement of DIP may slide up the volarly dislocated lateral bands and the deformity may get corrected. If this fails it can be surgically corrected by plicating the dislocated lateral bands dorsally and reinserting the central slip.
Extension contracture of the PIP can be either due to hypertrophic dorsal scar or secondary to mallet finger and may lead to swan neck deformity. Such contractures should be dealt with at the earliest before the DIP goes into flexion due to reciprocal positioning and florid swan neck contracture develops. The release should be done by two incisions over the proximal and middle phalanx keeping the skin intact over the PIP joint. The graft should be applied with the PIP in flexion. Extension deformity of PIP can also be part of swan neck deformity secondary to mallet finger deformity of the DIP, which results from attrition of terminal extensor insertion leading to flexion of DIP. These cases should also be dealt with promptly by arthrodesing the DIP at 0-5° before the lateral slips start dislocating volarwards.[34]
FIRST WEB SPACE CONTRACTURE
The contracture of the first web not only affects thumb mobility but the span of the hand. It results either form burn contracture of the web space or due to prolonged positioning of thumb in adducted and extended position leading to shortening adductor polices. Even in long standing skin contracture adductor muscles get contracted. Hence a pre-operative assessment to determine the need for muscle release is important. A simple skin contracture can be addressed by 5 flap Z plasty or dorsal transposition flap.[36] Structures to be released as the severity of the contracture increases are, origin of first dorsal interosseous muscle, origin of adductor pollicis and finally capsule of carpometacarpal joint.[37] These cases need a flap to bridge the defect. The choices are distally based radial artery forearm flap, posterior interosseous artery flap [Figures 18 and 19] and pedicled groin flap[31] [Figure 20]. While in setting the flap it is important to keep the web space open by bridging K wire.
Figure 18.
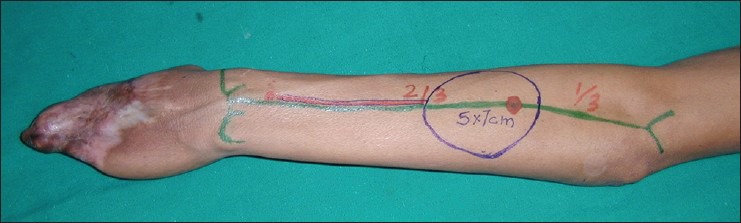
Hand deformity with obliterated 1st web space
Figure 19.

First web space released and resurfaced with distally based posterior interosseous flap
Figure 20.

Web space released and resurfaced with thin groin flap
POST-OPERATIVE PHYSICAL THERAPY
The importance of physical therapy after surgical correction of post-burn hand deformity cannot be overemphasized. This needs dedication of the therapist and compliance of the patient. The hand therapist should be involved in the pre-operative planning session and on the other hand the operating surgeon should supervise the initial days of post-operative physiotherapy.[8] Another aspect of prime importance is analgesia.[38] The pain relief should not only be during the therapy but also throughout the day.[38] The duration of splinting is more in cases where the resurfacing is by skin graft compared to that by flap. Hence it is always important to achieve a complete graft take to reduce the healing time. If the take is good the splint can be removed by 2-3 weeks for therapy and by 6 weeks only night splitage is enough.[37,39] For flexion contractures an out-trigger split which, passively keeps the fingers in extension maintaining the release and allows active flexion is useful.[40] In case a flap has been used including pedicled groin flap the patients is encouraged to start moving the fingers as soon as the pain allows. The patient must be allowed to do activities of daily living as early as possible. This not only gives the patient confidence and a sense of well-being but also strengthens the muscle and improves joint mobility.
CONCLUSION
Burns being a life-threatening and disfiguring injury the initial focus is on saving life and the after that the patient is worried about the aesthetic issues. The hands are often neglected in this scenario. It cannot be overemphasised that the hand therapist should be involved from day one, who not only keeps the hand in proper position but also apprises at a regular interval, both the patient and the doctor, the importance of hand. No other post-burn deformity gets worsened with time as does hand and hence time is key to functional recovery. Therefore while planning the schedule of corrective surgeries the hand must figure higher in the priority list even if patient demand correction of facial and other aesthetic deformities first.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Sheridan RL, Hurley J, Smith MA, Ryan CM, Bondoc CC, Quinby WC, Jr, et al. The acutely burned hand: Management and outcome based on a ten-year experience with 1047 acute hand burns. J Trauma. 1995;38:406–11. doi: 10.1097/00005373-199503000-00022. [DOI] [PubMed] [Google Scholar]
- 2.Appendix B to hospital resources document. Guidelines for service standards and severity classifications in the treatment of burn injury. American Burn Association. Bull Am Coll Surg. 1984;69:24–8. [PubMed] [Google Scholar]
- 3.Sykes PJ. Severe burns of the hand: A practical guide to their management. J Hand Surg Br. 1991;16:6–12. doi: 10.1016/0266-7681(91)90118-8. [DOI] [PubMed] [Google Scholar]
- 4.Robson MC, Smith DJ. Burned hand. In: Jurkiewicz MJ, Krizek TJ, Mathes SJ, Ariaya S, editors. Plastic Surgery: Principles and Practices. St Louis: CV Mosby; 1990. pp. 781–802. [Google Scholar]
- 5.Salisbury RE, Wright P. Evaluation of early excision of dorsal burns of the hand. Plast Reconstr Surg. 1982;69:670–5. doi: 10.1097/00006534-198204000-00017. [DOI] [PubMed] [Google Scholar]
- 6.Krizek TJ, Robson MC, Flagg SV. Management of burn syndactyly. J Trauma. 1974;14:587–93. doi: 10.1097/00005373-197407000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Robson MC, Smith DJ, Jr, VanderZee AJ, Roberts L. Making the burned hand functional. Clin Plast Surg. 1992;19:663–71. [PubMed] [Google Scholar]
- 8.Pandya AN. Principle of treatment of burn contracture. Repair Reconstr. 2001;2:12–3. [Google Scholar]
- 9.Potokar T. Burn injury: Epidemiology and prevention. Repair Reconstr. 2000;1:2–5. [Google Scholar]
- 10.Watson S. Hand burns. Repair Reconstr. 2001;2:2–4. [Google Scholar]
- 11.McCauley RL. Reconstruction of the pediatric burned hand. Hand Clin. 2000;16:249–59. [PubMed] [Google Scholar]
- 12.Kucan JO, Bash D. Reconstruction of the burned foot. Clin Plast Surg. 1992;19:705–19. [PubMed] [Google Scholar]
- 13.Kurtzman LC, Stern PJ. Upper extremity burn contractures. Hand Clin. 1990;6:261–79. [PubMed] [Google Scholar]
- 14.Greenhalgh DG, Gaboury T, Warden GD. The early release of axillary contractures in pediatric patients with burns. J Burn Care Rehabil. 1993;14:39–42. doi: 10.1097/00004630-199301000-00010. [DOI] [PubMed] [Google Scholar]
- 15.Bennett GB, Helm P, Purdue GF, Hunt JL. Serial casting: A method for treating burn contractures. J Burn Care Rehabil. 1989;10:543–5. [PubMed] [Google Scholar]
- 16.Stern PJ, Law EJ, Benedict FE, MacMillan BG. Surgical treatment of elbow contractures in postburn children. Plast Reconstr Surg. 1985;76:441–6. doi: 10.1097/00006534-198509000-00021. [DOI] [PubMed] [Google Scholar]
- 17.Salisbury RE, Bevin AG. Altus of reconstruction of burned hand. Clin Plast Surg. 2000;27:65–9. [PubMed] [Google Scholar]
- 18.Mani MM, Chhatre M. Reconstruction of the burned lower extremity. Clin Plast Surg. 1992;19:693–703. [PubMed] [Google Scholar]
- 19.Gulati S, Joshi BB, Milner SM. Use of Joshi external stabilizing system in postburn contractures of the hand and wrist: A 20-year experience. J Burn Care Rehabil. 2004;25:416–20. doi: 10.1097/01.bcr.0000138297.68047.29. [DOI] [PubMed] [Google Scholar]
- 20.Ilhami K, Safak O, Orhan G. Specifically designed external fixators in treatment of complex postburn hand contractures. Burns. 2003;29:609–12. doi: 10.1016/s0305-4179(03)00082-2. [DOI] [PubMed] [Google Scholar]
- 21.Salafia A, Chauhan G. Use of external fixator in hands. In: Schwarz R, Brandsma W, editors. Surgical Treatment and Rehabilitation in Leprosy. Kathmandu: EKTA Publishers; 2004. pp. 127–32. [Google Scholar]
- 22.Iwuagwu FC, Wilson D, Bailie F. The use of skin grafts in postburn contracture release: A 10-year review. Plast Reconstr Surg. 1999;103:1198–204. doi: 10.1097/00006534-199904040-00015. [DOI] [PubMed] [Google Scholar]
- 23.Pensler JM, Steward R, Lewis SR, Herndon DN. Reconstruction of the burned palm: Full-thickness versus split-thickness skin grafts: Long-term follow-up. Plast Reconstr Surg. 1988;81:46–9. [PubMed] [Google Scholar]
- 24.Bunyan AR, Mathur BS. Medium thickness plantar skin graft for the management of digital and palmar flexion contractures. Burns. 2000;26:575–80. doi: 10.1016/s0305-4179(00)00014-0. [DOI] [PubMed] [Google Scholar]
- 25.Tanabe HY, Aoyagi A, Tai Y, Kiyokawa K, Inoue Y. Reconstruction for palmar skin defects of the digits and hand using plantar dermal grafting. Plast Reconstr Surg. 1998;101:992–8. doi: 10.1097/00006534-199804040-00016. [DOI] [PubMed] [Google Scholar]
- 26.Schwarz RJ. Management of postburn contractures of the upper extremity. J Burn Care Res. 2007;28:212–9. doi: 10.1097/BCR.0B013E318031A172. [DOI] [PubMed] [Google Scholar]
- 27.Strauch B, Vasconez LO, Hall-Findlay EJ, editors. Toronto: Little Brown and Co; 1990. Gabbs Encyclopedia of Flaps. [Google Scholar]
- 28.Ulkür E, Acikel C, Karagoz H, Celikoz B. Treatment of severely contracted fingers with combined use of cross-finger and side finger transposition flaps. Plast Reconstr Surg. 2005;116:1709–14. doi: 10.1097/01.prs.0000185666.62304.19. [DOI] [PubMed] [Google Scholar]
- 29.Peker F, Celebiler O. Y-V advancement with Z-plasty: An effective combined model for the release of post-burn flexion contractures of the fingers. Burns. 2003;29:479–82. doi: 10.1016/s0305-4179(03)00048-2. [DOI] [PubMed] [Google Scholar]
- 30.Cherup LL, Zachary LS, Gottlieb LJ, Petti CA. The radial forearm skin graft-fascial flap. Plast Reconstr Surg. 1990;85:898–902. doi: 10.1097/00006534-199006000-00010. [DOI] [PubMed] [Google Scholar]
- 31.Costa H, Soutar DS. The distally based island posterior interosseous flap. Br J Plast Surg. 1988;41:221–7. doi: 10.1016/0007-1226(88)90104-x. [DOI] [PubMed] [Google Scholar]
- 32.Teo TC, Richard BM. The distally based posterior interosseous fasciocutaneous island flap in reconstruction of the hand in leprosy. Indian J Lepr. 1997;69:93–100. [PubMed] [Google Scholar]
- 33.Graham TJ, Stern PJ, True MS. Classification and treatment of postburn metacarpophalangeal joint extension contractures in children. J Hand Surg Am. 1990;15:450–6. doi: 10.1016/0363-5023(90)90058-y. [DOI] [PubMed] [Google Scholar]
- 34.Sabapathy SR. Hand burns. In: Sarabahi S, Tiwari VK, Goel A, editors. Principle and Practice of Burn Care. Delhi: Jaypee; 2010. pp. 363–82. [Google Scholar]
- 35.Chang LY, Yang JY, Wei FC. Reverse dorsometacarpal flap in digits and web-space reconstruction. Ann Plast Surg. 1994;33:281–9. doi: 10.1097/00000637-199409000-00008. [DOI] [PubMed] [Google Scholar]
- 36.Dmitriyev GI, Petrov SV. Surgery for adduction contracture of the thumb after burn. Acta Chir Plast. 1989;31:236–42. [PubMed] [Google Scholar]
- 37.Stern PJ, Neale HW, Carter W, MacMillan BG. Classification and management of burned thumb contractures in children. Burns Incl Therm Inj. 1985;11:168–74. doi: 10.1016/0305-4179(85)90064-6. [DOI] [PubMed] [Google Scholar]
- 38.Salisbury RE. Reconstruction of the burned hand. Clin Plast Surg. 2000;27:65–9. [PubMed] [Google Scholar]
- 39.Schwarz RJ, Joshi KD. Treatment of postburn contractures. J Nephrol Med Assoc. 2004;43:211–7. [Google Scholar]
- 40.Colditz JC. Therapist's management of stiff hand. In: Mackin EJ, Callahan AD, Skirven TM, Schnider LH, Osterman AL, editors. Rehabilitation of Hand and Upper Extremity. London: Mosby; 2002. pp. 1012–49. [Google Scholar]


