Abstract
Introduction
Few lung cancer studies have focused on lung cancer survival in underserved populations. We conducted a prospective cohort study among 81,697 racially diverse and medically underserved adults enrolled in the Southern Community Cohort Study throughout an 11-state area of the Southeast from March 2002 to September 2009.
Methods
Using linkages with state cancer registries, we identified 501 incident non-small cell lung cancer cases. We applied Cox proportional hazards models to estimate hazard ratios (HRs) and 95% confidence intervals for subsequent mortality among black and white participants.
Results
The mean observed follow-up time (the time from diagnosis to death or end of follow up) was 1.25 years (range 0-8.3 years) and 75% (N=376) of cases died during follow-up. More blacks were diagnosed at distant stage than whites (57% versus 45%) (p = 0.03). In multivariable analyses adjusted for pack-years of smoking, age, BMI, health insurance, socioeconomic status and disease stage, the lung cancer mortality HR was higher for men vs women (HR = 1.41, 95% CI: 1.09 – 1.81) but similar for blacks vs. whites (HR = 0.99, 95% CI: 0.74 – 1.32).
Conclusions
These findings suggest that although proportionally more blacks present with distant stage disease there is no difference in stage-adjusted lung cancer mortality between blacks and whites of similar low socioeconomic status.
Keywords: lung cancer, race, disparities, survival, socioeconomic status
Introduction
Lung cancer is the leading cause of cancer-related mortality in the U.S. among men and women with an overall 5-year relative survival of only 16%.1-3 According to the American Cancer Society, an estimated 160,340 lung cancer deaths occurred in the United States in 2012, accounting for 28% of all cancer deaths.4 While survival from lung cancer has improved since the early 1990s, racial differences in lung cancer survival persist such that blacks experience poorer 5-year survival for lung cancer compared to whites.1, 3, 5-8 Specifically, recent 5-year relative survival estimates from the Surveillance Epidemiology and End Results (SEER) 18 areas indicates blacks have a 13.0% 5-year relative survival; whereas, whites have a 16.3% 5-year relative survival.3, 9 Moreover, blacks are less likely to present with localized disease 2, 10 and also have a poorer prognosis even when diagnosed with localized disease, which is more successfully treated.2, 11 Advanced stage of disease at diagnosis is the primary factor contributing to the poor prognosis of lung cancer, although other risk factors identified to date include low socioeconomic status, male sex, and incomplete lung resection.12, 13 Populations living in the Southern U.S. experience the highest mortality for lung cancer, especially among men.2, 6
Due to the high burden of lung cancer in underserved populations,14 understanding lung cancer prognosis in these populations is necessary for targeted public health interventions for reducing lung cancer deaths. Moreover the paucity of lung cancer studies conducted among minority and low-income populations emphasizes the need to understand lung cancer survival in these understudied populations. Using data from the Southern Community Cohort Study (SCCS),15, 16 which includes a large proportion of blacks and underserved low-income individuals, we examined whether lung cancer survival differs between socioeconomically similar white and black populations living in the Southern U.S.
Materials and Methods
Study population
The Southern Community Cohort Study (SCCS) is an ongoing prospective cohort study established to examine cancer disparities among a predominantly low-income population. From March 2002 to September 2009, 70,748 racially diverse adults were enrolled into the SCCS at community health centers, institutions providing basic health care and preventative services in medically underserved geographic areas, throughout an 11-state area of the Southeast (Alabama, Arkansas, Florida, Georgia, Kentucky, Louisiana, Mississippi, North Carolina, South Carolina, Tennessee, and Virginia). Additional participants (N=10,949) were enrolled from the same 11-state area into the SCCS by selecting a random sample of adults identified from voter registration, driver’s license records and commercial records. Participants were aged 40-79 years at enrollment and approximately two-thirds self-reported as black/African American. Extensive details of the SCCS study design and participant recruitment are summarized elsewhere.15, 16 Briefly, participants were eligible if they spoke English, were between the ages of 40-79, and were not under treatment for cancer (except for nonmelanoma skin cancer) within the prior 12 months. For this analysis, participants were excluded if they had a prior diagnosis of lung cancer at cohort entry. The SCCS was approved by institutional review boards at Vanderbilt University and Meharry Medical College. Written, informed consent was obtained from all participants.
Baseline characteristics
Epidemiologic data were collected by trained interviewers during in-person computer-assisted personal interviews conducted at the community health centers or by mailed questionnaire from the random sample of the general population. Information was ascertained on demographic characteristics and exposure histories, including race/ethnicity, tobacco smoking history, medical history, and health insurance status. From March 2002 to September 2007, self-reported weight and height were ascertained from the baseline questionnaire administered by trained study interviewers. Participants were provided with the 2000 U.S. Census categories for race/ethnicity and asked to mark all that apply for their race and ethnic background.
Lung cancer case identification and mortality assessment
Incident lung cancer cases (International Classification of Diseases-Oncology, ICD-O-3, codes C340-C349) were identified via linkage with state cancer registries operating in the 11-state study area. Lung cancer stage and cell type were obtained from the state cancer registries. The cohort was followed for all-cause mortality, with the number of survival days defined as the time from date of diagnosis until date of death, loss to follow-up or censoring, by linkage with the National Death Index (NDI) through December 31, 2010 and the Social Security Administration through February 4, 2011. Cause of death was available only for deaths occurring through 2010.
Statistical analysis
Lung cancer patients reporting races other than non-Hispanic white or non-Hispanic black (N=25) were excluded from analyses. Differences in baseline characteristics between blacks and white lung cancer cases were evaluated using the chi-square test and two-sample t-test for categorical or continuous variables, respectively. Kaplan-Meier curves were plotted to visualize survival probabilities and differences in survival between whites and blacks were assessed using the log-rank test. We estimated hazard ratios (HRs) and accompanying 95% confidence intervals for lung cancer mortality using Cox proportional hazard (PH) models, adjusted for demographic and clinical characteristics, to evaluate whether lung cancer survival differed between blacks and whites. Age of the participant at diagnosis was included as a covariate in Cox PH models. The proportional hazards assumption was assessed by including an interaction term between race and time and we found hazards remained constant over time. We estimated odds ratios for the association between education, and health insurance and stage of diagnosis (coded as local versus distant/regional) using multivariable logistic regression models. All analyses were conducted using SAS software, version 9.3 (SAS Institute, Inc.). Statistical tests were two-sided and an alpha of 0.05 was used to assess statistical significance.
Results
We identified 501 incident non-small cell lung cancer (NSCLC) cases (149 non-Hispanic white, 352 non-Hispanic black) occurring among the 81,697 participants during the follow-up period from March 2002 until February 2011. During an average of 1.3 (maximum 8.3) years of follow-up, 376 deaths occurred and 309 (82%) had lung cancer as the primary cause of death. Most cases (88%) were recruited from community health centers. Among the lung cancer cases 66% had an annual household income < $15,000, 42% had less than a high school education, 58% were overweight or obese, 71% were current smokers and 34% reported having no medical insurance at cohort entry, reflecting the overall demographics of the SCCS cohort.15 Approximately half (49%) of the lung cancer cases were diagnosed with distant stage lung cancer, while only 16% of cases were diagnosed at local stage. The most frequent histologic tumor type was adenocarcinoma (39%), followed by squamous cell carcinoma (27%), and non-small cell NOS (27%), and other NSCLC tumors (e.g. large cell) (8%).
No differences were observed between black and white lung cancer cases for household income or smoking status (current/former/never smoker), the primary lung cancer risk factor (Table 1). More blacks smoked menthol cigarettes compared to whites. More whites self-reported a physician diagnosis of emphysema or chronic bronchitis and a first-degree relative with lung cancer. Health insurance status differed between blacks and whites (p = 0.007) with more blacks uninsured (36% versus 30%, respectively) and receiving Medicaid (25% versus 18%, respectively) than whites (Table 1). A greater percentage of blacks were diagnosed with distant stage lung cancer than whites (57% versus 45%, respectively, p = 0.03) (Figure 1). Histologic subtypes of disease did not differ between blacks and whites. The overall mean age at diagnosis for lung cancer cases was 60.0 years (standard deviation 8.9).
Table 1.
Demographic characteristics by race of incident non-small cell lung cancer (NSCLC) cases occurring in the Southern Community Cohort Study, 2002-2011.
| NSCLC Cases N=501 |
||
|---|---|---|
|
| ||
| Black (N=352) | White (N=149) | |
|
|
||
| Characteristic | N (%) | N (%) |
| Sex | ||
| Male | 209 (59.4) | 67 (45.0) |
| Female | 143 (40.6) | 82 (55.0) |
| Vital statusa | ||
| Died | 270 (76.7) | 106 (71.1) |
| Alive | 82 (23.3) | 43 (28.9) |
| Person-years of follow-up | 410.4 | 218.0 |
| Lung cancer stage at diagnosis | ||
| Distant | 181 (56.9) | 60 (45.5) |
| Local | 48 (15.1) | 30 (22.7) |
| Regional | 89 (28.0) | 42 (31.8) |
| Unknown | 51 | |
| Histology | ||
| Adenocarcinoma | 139 (39.5) | 55 (36.9) |
| Non-small cell lung cancer-NOS | 97 (27.6) | 38 (25.5) |
| Squamous | 89 (25.3) | 44 (29.5) |
| Other NSCLC | 27 (7.7) | 12 (8.1) |
| Mean age at enrollment, year (s.d.) | 55.7 (8.8) | 59.7 (8.8) |
| Mean age at diagnosis, year (s.d.) | 59.0 (8.7) | 62.3 (9.0) |
| Mean observed duration of disease among those who diedb, year (s.d.) |
0.74 (0.85) | 0.82 (0.93) |
| Mean observed duration of disease among those alive at last follow-upb, year (s.d.) |
2.57 (1.9) | 3.05 (1.7) |
| Highest education level, years | ||
| < 12 | 161 (45.9) | 51 (34.5) |
| ≥ 12 | 190 (54.1) | 97 (65.5) |
| Unknown | 2 | |
| Household income in last year | ||
| < $15,000 | 232 (66.5) | 94 (63.9) |
| ≥ $15,000 | 117 (33.5) | 53 (36.1) |
| Unknown | 5 | |
| Smoking status at cohort entry | ||
| Current | 253 (72.5) | 102 (68.9) |
| Former | 75 (21.5) | 40 (27.0) |
| Never | 21 (6.0) | 6 (4.1) |
| Smokes (or smoked) menthol cigarettesc | ||
| Yes | 231 (70.6) | 24 (17.1) |
| No | 96 (29.4) | 116 (82.9) |
| Unknown | 7 | |
| Self-reported doctor diagnosis of emphysema or chronic bronchitis |
||
| Yes | 39 (11.1) | 45 (30.2) |
| No | 312 (88.9) | 104 (69.8) |
| Unknown | 1 | |
| First degree relative with lung cancer | ||
| Yes | 26 (9.4) | 28 (23.5) |
| No | 251 (90.6) | 91 (76.5) |
| Unknown | 105 | |
| Body Mass Index (BMI) (kg/m2) | ||
| < 25 | 160 (45.7) | 50 (33.8) |
| 25-29 | 107 (30.6) | 55 (37.2) |
| ≥ 30 | 83 (23.7) | 43 (29.1) |
| Unknown | 3 | |
| Health insurance status | ||
| Uninsured | 126 (36.1) | 44 (29.7) |
| Medicare, age < 65 years | 51 (14.6) | 25 (16.9) |
| Medicare, age ≥ 65 years | 25 (7.2) | 28 (18.9) |
| Medicaid | 88 (25.2) | 27 (18,2) |
| Private | 42 (12.0) | 22 (14.9) |
| Military/Other | 17 (4.9) | 2 (1.4) |
| Unknown | 4 | |
Date of last follow-up February 4, 2011
Date of diagnosis to date of last follow-up (or death).
Among current and former smokers only
Numbers may not add to 100% due to rounding.
NSCLC, non-small cell lung cancer; NOS, not otherwise specified; s.d., standard deviation.
Figure 1.
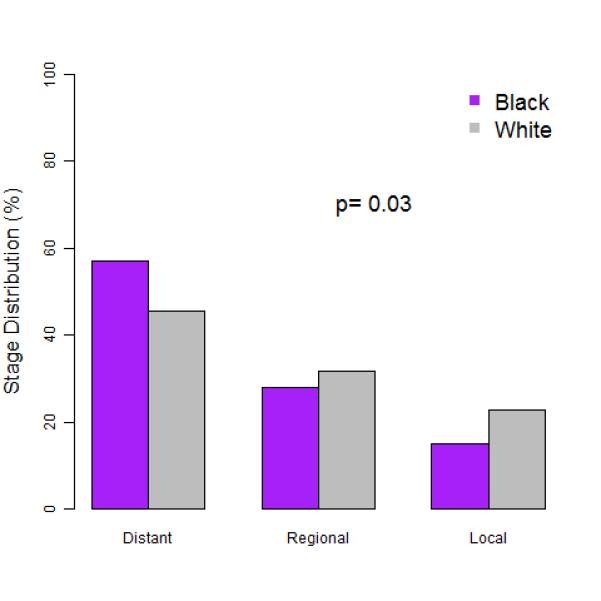
Stage distribution for black and white incident non-small cell lung cancer cases occurring from 2002-2011 in Southern Community Cohort Study participants.
By the end of study follow-up, 75% of identified lung cancer cases were deceased with a median overall survival of 0.73 years. Kaplan-Meier product-limit survival estimates demonstrated blacks had shorter median survival times (0.67 vs. 1.02 years) and poorer overall survival compared to whites (p = 0.06, log-rank test; Figure 2). Figure 3 illustrates the poor survival of black men compared to women and white men (p < 0.0001, log-rank test; Figure 3). Age at diagnosis did not significantly impact survival (data not shown). After adjusting for disease stage, pack-years of smoking, age at diagnosis, sex, education, baseline BMI, health insurance status and study site, blacks and whites had no difference in mortality (HR = 0.99, 95% CI: 0.74-1.32, Table 2). Including an indicator for rural versus urban county of residence did not alter this finding (data not shown). Male lung cancer cases had a statistically significant 41% greater mortality compared to females (HR=1.41, 95% CI: 1.10-1.80, Table 2). As expected, distant stage of disease at diagnosis was strongly associated with mortality, with almost a five-fold increased mortality compared to those diagnosed at localized stage (Table 2). No significant differences in mortality were found according to health insurance classification. Blacks (OR = 0.72, 95% CI: 0.40 – 1.31), males (OR = 0.61, 95% CI: 0.35 – 1.06), and those enrolled at a community health center (OR = 0.55, 95% CI: 0.23 – 1.32) were less likely (although not statistically significant) to have localized stage of disease, after adjusting for pack-years of smoking, education, BMI and age of diagnosis.
Figure 2.
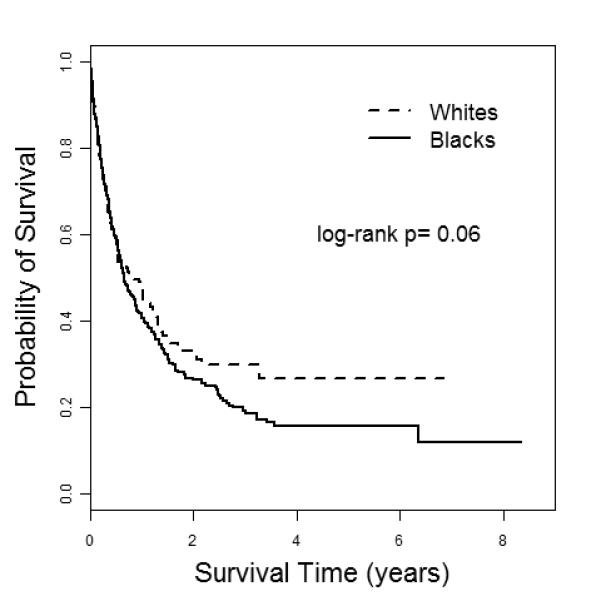
Kaplan-Meier curves for black and white incident non-small cell lung cancer cases occurring from 2002-2011 in Southern Community Cohort Study participants.
Figure 3.
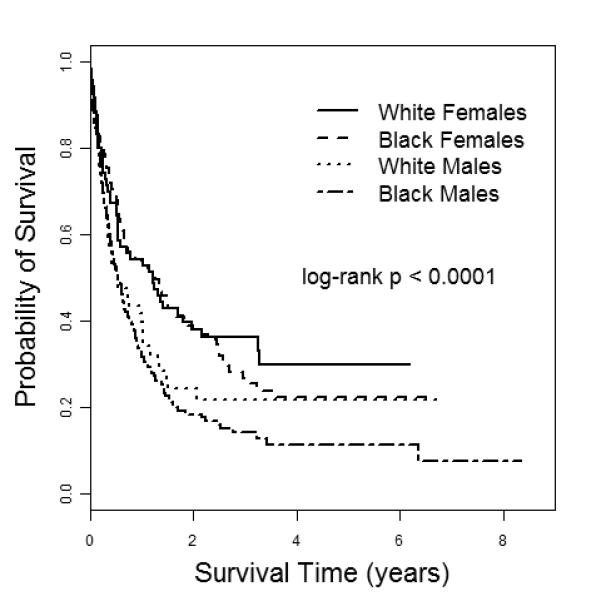
Kaplan-Meier curves for black and white incident non-small cell lung cancer cases, stratified by sex, occurring from 2002-2011 in Southern Community Cohort Study participants.
Table 2.
All-cause mortality among incident NSCLC cases participating in the Southern Community Cohort Study, 2002-2011.
| NSCLC Cases N=424 |
|||
|---|---|---|---|
| Variable | HR | (95% CI) | P |
| Race | |||
| White | 1.0 | Referent | |
| Black | 0.99 | (0.74 – 1.32) | 0.94 |
| Smoking pack-years | 1.005 | (1.00-1.009) | 0.04 |
| Age at diagnosis | 1.00 | (0.98-1.02) | 0.99 |
| Sex | |||
| Female | 1.0 | Referent | |
| Male | 1.41 | (1.09 – 1.81) | < 0.01 |
| Education, years | |||
| < 12 | 1.0 | Referent | |
| ≥ 12 | 1.04 | (0.81 – 1.33) | 0.79 |
| BMI, kg/m2 | |||
| < 25 | 1.0 | Referent | |
| 25-29 | 1.00 | (0.76 – 1.30) | 0.98 |
| ≥ 30 | 0.92 | (0.69 – 1.24) | 0.60 |
| Health insurance status | |||
| No | 1.0 | Referent | |
| Medicare, age < 65 years | 0.92 | (0.65 – 1.32) | 0.66 |
| Medicare, age ≥ 65 years | 0.72 | (0.44 – 1.20) | 0.21 |
| Medicaid | 1.21 | (0.89 – 1.65) | 0.22 |
| Private | 0.74 | (0.49 – 1.12) | 0.15 |
| Military/Other | 1.33 | (0.75 – 2.35) | 0.33 |
| Disease stage | |||
| Localized | 1.0 | Referent | |
| Regional | 2.23 | (1.45 – 3.43) | < 0.01 |
| Distant | 4.99 | (3.33 – 7.48) | < 0.01 |
| Study site | |||
| General population | 1.0 | Referent | |
| CHC | 1.13 | (0.72 – 1.76) | 0.60 |
Cox proportional hazards analysis of lung cancer mortality among SCCS participants.
HR, hazard ratio; CI, confidence interval; NSCLC, non-small cell lung cancer; CHC, community health center.
Discussion
This survival analysis of incident lung cancers nested within a large prospective cohort study of blacks and whites revealed greater crude mortality and shorter median survival for blacks compared to whites but no racial difference in overall mortality between low-income blacks and whites after controlling for stage of diagnosis. We were uniquely positioned to examine lung cancer mortality for both blacks and whites in the Southeastern United States after good control for socioeconomic status, since both blacks and whites in the cohort had generally similar low household income, low education, health insurance and access to basic health services, with minor differences adjusted for in our statistical analyses. Our findings in this population of blacks and whites with similar individual-level socioeconomic status are analogous to lung cancer investigations in other populations with similar access to health care or surgical treatment between blacks and whites12, 17, 18 or investigations stratified by cancer stage.19 Our findings provide evidence to support that when demographic factors, smoking and lung cancer stage are controlled, lung cancer survival between black and white lung cancer patients is similar, even among primarily low-income and medically underserved populations. However, similar to national data,3 we found an increased mortality for males compared to females. This finding deserves further investigation to clarify predictors of local stage when clinical interventions are possible.
Prior research on racial disparities in lung cancer has found blacks are more likely to be diagnosed at advanced stage of lung cancer compared to whites.10 Within the SCCS, we similarly found a greater percentage of blacks were diagnosed at advanced stage of disease compared to whites, despite having similar smoking status, and access to basic health care. Research suggests blacks may tend to hold different beliefs regarding lung cancer treatments compared to whites, including inaccurate beliefs regarding tumor spread when surgically exposed to air7, which may lead to a later stage of presentation. Diagnosis at an early stage of disease is crucial since lung cancers diagnosed at a localized stage have a 52% 5-year relative survival rate; however, only 15% of lung cancers are diagnosed at this early stage,3, 11 consistent with the 16% of localized stage lung cancers identified in our study population.
Contrary to prior investigations by others,13, 20, 21 we did not find that the socioeconomic status, measured using highest education level attained, was associated with localized stage of lung cancer. Lung cancer incidence is higher among poor and low education populations,14 yet few lung cancer studies have been devoted to underserved populations. It is well documented that educational attainment is associated with improved cancer survival such that poorly educated20, 22 and low-income populations experience worse outcomes compared to higher income populations.1, 23 Several studies using census-level data have found inverse associations between socioeconomic status (SES) and lung cancer mortality.13, 21, 24 Using census block group data to construct a socioeconomic status metric, Schwartz and colleagues found that SES predicted lung cancer stage at diagnosis, with individuals living in professional occupation block groups having a reduced mortality compared to individuals living in working poor block groups.13 Similarly, Erhunmwunsee and colleagues found individuals living in census tracts with lower incomes and less education had shorter survival compared to individuals living in regions with higher incomes or greater education level.21 However, these ecologic studies are constrained by the lack of data on important individual-level factors influencing survival and ascribing attributes of a group to an individual can result in inaccurate inferences.25 Using U.S. mortality data and education data from the U.S. Current Population Survey, Albano et al. identified an increased mortality among blacks and whites diagnosed with lung cancer and having less than 12 years of education compared to those with 12 or more years, especially among men.20 However, where health care access has been universal and treatment has been similar, such as among military populations or clinical populations, no racial differences in lung cancer survival between blacks and whites have been observed.12, 17, 18, 26 Thus racial differences in lung cancer survival appear to manifest differently across populations, yet few have examined low-income populations. Our study sheds light on low-income populations and indicates that blacks tend to be diagnosed with lung cancer at later stage and have poorer survival than whites, but when stage and other factors are controlled, racial differences disappear.
Our study is limited by a lack of assessment of treatment received, treatment quality of care, and medically confirmed co-morbidities. Although we do not have systematic treatment information available from clinical records, we were able to adjust for stage and health insurance status as a proxy for treatment. Our findings suggest that if lung cancer treatment differences do exist between blacks and whites in this low-income population, the influence on survival may be minimal. Co-morbidities are important predictors of lung cancer stage, treatment and survival.27, 28 Our limited sample size, especially for whites, limits our statistical power which may have resulted in less precision around our estimated hazard ratios (i.e. wide confidence intervals) and therefore our conclusions regarding statistically significant findings. Future studies are warranted to replicate our findings in larger populations of low-income blacks and whites, stratifying by histology, and incorporating lung cancer treatment and co-morbidities into analyses.
The strengths of our study are the inclusion of blacks and whites of similar low socioeconomic status and incident lung cancer cases nested within a large prospective study. Notably, we obtained individual-level data on smoking and health insurance status that prior studies using SEER cancer registry or census-level data have been unable to measure.10 Furthermore, data were obtained prior to lung cancer diagnosis, thus minimizing the possibility of recall bias. Few studies have focused on medically underserved populations having such low socioeconomic status. Importantly, our findings may be generally applicable to low-income, underserved populations thus filling an important research gap regarding lung cancer outcomes in groups frequently excluded from lung cancer investigations.
In summary, we observed that within an underserved population of blacks and whites of similar socioeconomic status, blacks tend to be diagnosed with lung cancer at later stages of disease and have poorer overall survival, but after control for stage racial differences in mortality are no longer apparent. Regardless of race, the survival was low with 75% of the cases deceased over a mean 1.3 year follow-up period. The poor lung cancer prognosis remains true despite the steady decline in lung cancer incidence, declining smoking rates, increased awareness of the disease in the general population, and the advent of new technologies to detect lung cancers in early stages of the disease. This has prompted the National Cancer Institute to prioritize research aimed at improving early diagnosis of disease29 and underscores the timeliness of the National Lung Screening Trial findings of improved survival associated with computed tomographic screening.30 It remains to be determined whether the observed difference in histologic subtype and stage of presentation of lung cancer between blacks and whites is due to differences in comorbidities, cultural choices between blacks and whites, potential underlying biologic or genetic variations, or combinations of these factors. Importantly, these findings indicate that race per se may not be a predictor of poor survival, even amongst a primarily low-income and medically underserved population. Future efforts should identify opportunities for early diagnosis and treatment, especially for black males who experience a greater mortality from lung cancer.
Acknowledgements
Data on SCCS cancer cases used in this publication were provided by the Alabama Statewide Cancer Registry; Kentucky Cancer Registry, Lexington, KY; Tennessee Department of Health, Office of Cancer Surveillance; Florida Cancer Data System; North Carolina Central Cancer Registry, North Carolina Division of Public Health; Georgia Comprehensive Cancer Registry; Louisiana Tumor Registry; Mississippi Cancer Registry; South Carolina Central Cancer Registry; Virginia Department of Health, Virginia Cancer Registry; Arkansas Department of Health, Cancer Registry, 4815 W. Markham, Little Rock, AR 72205. The Arkansas Central Cancer Registry is fully funded by a grant from National Program of Cancer Registries, Centers for Disease Control and Prevention (CDC). Data on SCCS cancer cases from Mississippi were collected by the Mississippi Cancer Registry which participates in the National Program of Cancer Registries (NPCR) of the Centers for Disease Control and Prevention (CDC). The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of the CDC or the Mississippi Cancer Registry. We thank Dr. Sarah Cohen for her careful statistical review and edits of the manuscript.
Grant Support This article was supported by the NIH/National Cancer Institute (Grant R01 CA092447, and American Recovery and Reinvestment Act supplement 3R01 CA092447-08S1). M.C. Aldrich was supported by a Vanderbilt Clinical & Translational Research Award and a Department of Defense Early Investigator Synergistic Idea Award (W81XWH-12-1-0547). E.L. Grogan was supported by a Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development Service Career Development Award (10-024) and a Department of Defense Early Investigator Synergistic Idea Award (W18XWH-12-1-0544). The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Footnotes
Disclosure of Potential Conflicts of Interest No potential conflicts of interest were disclosed.
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Siegel R, Ward E, Brawley O, et al. Cancer statistics, 2011: The impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA: a cancer journal for clinicians. 2011;61:212–236. doi: 10.3322/caac.20121. [DOI] [PubMed] [Google Scholar]
- 2.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA: a cancer journal for clinicians. 2012;62:10–29. doi: 10.3322/caac.20138. [DOI] [PubMed] [Google Scholar]
- 3.Howlader N, Noone AM, Krapcho M, et al. SEER Cancer Statistics Review, 1975-2009. National Cancer Institute; Bethesda, MD: 2012. Available at http://seer.cancer.gov/csr/1975_2009_pops09/ based on November 2011 SEER data submission, posted to the SEER web site, 2012. [Google Scholar]
- 4.American Cancer Society [Accessed May 18, 2012];Lung Cancer. 2012 Feb 17; Available at http://www.cancer.org/acs/groups/cid/documents/webcontent/003115-pdf.pdf.
- 5.Altekruse SF, Kosary CL, Krapcho M, et al. SEER Cancer Statistics Review, 1975-2007. National Cancer Institute; Bethesda, MD: 2010. Available at http://seer.cancer.gov/csr/1975_2007/ [Google Scholar]
- 6.U.S. Cancer Statistics Working Group [Accessed February 14, 2011];United States Cancer Statistics: 1999–2007 Incidence and Mortality Web-based Report. Available at www.cdc.gov/uscs.
- 7.Berger M, Lund MJ, Brawley OW. Racial disparities in lung cancer. Curr Probl Cancer. 2007;31:202–210. doi: 10.1016/j.currproblcancer.2007.02.002. [DOI] [PubMed] [Google Scholar]
- 8.DeLancey JO, Thun MJ, Jemal A, et al. Recent trends in Black-White disparities in cancer mortality. Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 2008;17:2908–2912. doi: 10.1158/1055-9965.EPI-08-0131. [DOI] [PubMed] [Google Scholar]
- 9.Fast Stats: An interactive tool for access to SEER cancer statistics. Surveillance Research Program. National Cancer Institute; 2012. Available at http://seer.cancer.gov/faststats. [Google Scholar]
- 10.Virnig BA, Baxter NN, Habermann EB, et al. A matter of race: early-versus late-stage cancer diagnosis. Health affairs. 2009;28:160–168. doi: 10.1377/hlthaff.28.1.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American Cancer Society . Cancer Facts & Figures for African Americans 2011-2012. American Cancer Society; Atlanta: 2011. [Google Scholar]
- 12.Mulligan CR, Meram AD, Proctor CD, et al. Unlimited access to care: effect on racial disparity and prognostic factors in lung cancer. Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 2006;15:25–31. doi: 10.1158/1055-9965.EPI-05-0537. [DOI] [PubMed] [Google Scholar]
- 13.Schwartz KL, Crossley-May H, Vigneau FD, et al. Race, socioeconomic status and stage at diagnosis for five common malignancies. Cancer Causes Control. 2003;14:761–766. doi: 10.1023/a:1026321923883. [DOI] [PubMed] [Google Scholar]
- 14.Alberg AJ, Ford JG, Samet JM. Epidemiology of lung cancer: ACCP evidence-based clinical practice guidelines (2nd edition) Chest. 2007;132:29S–55S. doi: 10.1378/chest.07-1347. [DOI] [PubMed] [Google Scholar]
- 15.Signorello LB, Hargreaves MK, Blot WJ. The Southern Community Cohort Study: investigating health disparities. J Health Care Poor Underserved. 2010;21:26–37. doi: 10.1353/hpu.0.0245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Signorello LB, Hargreaves MK, Steinwandel MD, et al. Southern community cohort study: establishing a cohort to investigate health disparities. Journal of the National Medical Association. 2005;97:972–979. [PMC free article] [PubMed] [Google Scholar]
- 17.Bach PB, Cramer LD, Warren JL, et al. Racial differences in the treatment of early-stage lung cancer. N Engl J Med. 1999;341:1198–1205. doi: 10.1056/NEJM199910143411606. [DOI] [PubMed] [Google Scholar]
- 18.Zheng L, Enewold L, Zahm SH, et al. Lung Cancer Survival among Black and White Patients in an Equal Access Health System. Cancer Epidemiol Biomarkers Prev. 2012;21:1841–1847. doi: 10.1158/1055-9965.EPI-12-0560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hardy D, Xia R, Liu CC, et al. Racial disparities and survival for nonsmall-cell lung cancer in a large cohort of black and white elderly patients. Cancer. 2009;115:4807–4818. doi: 10.1002/cncr.24521. [DOI] [PubMed] [Google Scholar]
- 20.Albano JD, Ward E, Jemal A, et al. Cancer mortality in the United States by education level and race. J Natl Cancer Inst. 2007;99:1384–1394. doi: 10.1093/jnci/djm127. [DOI] [PubMed] [Google Scholar]
- 21.Erhunmwunsee L, Joshi MB, Conlon DH, et al. Neighborhood-level socioeconomic determinants impact outcomes in nonsmall cell lung cancer patients in the Southeastern United States. Cancer. 2012;118:5117–23. doi: 10.1002/cncr.26185. [DOI] [PubMed] [Google Scholar]
- 22.Kinsey T, Jemal A, Liff J, et al. Secular trends in mortality from common cancers in the United States by educational attainment, 1993-2001. J Natl Cancer Inst. 2008;100:1003–1012. doi: 10.1093/jnci/djn207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ward E, Halpern M, Schrag N, et al. Association of insurance with cancer care utilization and outcomes. CA: a cancer journal for clinicians. 2008;58:9–31. doi: 10.3322/CA.2007.0011. [DOI] [PubMed] [Google Scholar]
- 24.Singh GK, Williams SD, Siahpush M, et al. Socioeconomic, Rural-Urban, and Racial Inequalities in US Cancer Mortality: Part I-All Cancers and Lung Cancer and Part II-Colorectal, Prostate, Breast, and Cervical Cancers. J Cancer Epidemiol. 2011;2011:107497. doi: 10.1155/2011/107497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Morgenstern H. Uses of ecologic analysis in epidemiologic research. Am J Public Health. 1982;72:1336–1344. doi: 10.2105/ajph.72.12.1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Albain KS, Unger JM, Crowley JJ, et al. Racial disparities in cancer survival among randomized clinical trials patients of the Southwest Oncology Group. J Natl Cancer Inst. 2009;101:984–992. doi: 10.1093/jnci/djp175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tammemagi CM, Neslund-Dudas C, Simoff M, et al. In lung cancer patients, age, race-ethnicity, gender and smoking predict adverse comorbidity, which in turn predicts treatment and survival. J Clin Epidemiol. 2004;57:597–609. doi: 10.1016/j.jclinepi.2003.11.002. [DOI] [PubMed] [Google Scholar]
- 28.Tammemagi CM, Neslund-Dudas C, Simoff M, et al. Smoking and lung cancer survival: the role of comorbidity and treatment. Chest. 2004;125:27–37. doi: 10.1378/chest.125.1.27. [DOI] [PubMed] [Google Scholar]
- 29.National Cancer Institute . The Nation’s Progress in Cancer Research: An Annual Report for 2004. U.S. Department of Health and Human Services, National Institutes of Health; 2004. [Google Scholar]
- 30.Aberle DR, Adams AM, Berg CD, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365:395–409. doi: 10.1056/NEJMoa1102873. [DOI] [PMC free article] [PubMed] [Google Scholar]


