Abstract
Purpose
To determine the age-, gender- and ethnicity-specific prevalence of myopia, hyperopia and astigmatism in Non-Hispanic White (NHW) and Asian preschool children.
Design
Population-based cross-sectional study.
Participants
A population based sample of 1501 NHW children and 1507 Asian children aged 6-72 months from Los Angeles County and Riverside County, California.
Methods
Eligible children underwent an in-home and in-clinic interview and a comprehensive eye examination including cycloplegic auto-refraction from 100 census tracts.
Main outcome measures
The proportion of children with myopia (spherical equivalent (SE) <=−1.00 diopter (D)), hyperopia (SE >=+2.00) D and cylindrical refractive error >=1.50 D in the worse eye. The astigmatism type was defined as with-the-rule (WTR) (+cylinder axis 90° ± 15°) and against-the-rule (ATR) (+ cylinder axis 180° ± 15°); all other orientations were considered oblique (OBL).
Results
The prevalence of myopia, hyperopia and astigmatism in NHW children was 1.20% (95% Confidence Interval (CI) = 0.76-1.89%), 25.65% (95% CI= 23.5-27.9%), and 6.33% (95% CI = 5.21-7.68%), respectively. The prevalence of WTR, ATR and OBL astigmatism in NHW children was 4.33%, 1.00% and 1.00% respectively. Prevalence was lower with older age groups for astigmatism (p=0.0002), but not for myopia or hyperopia (p=0.82 and p=0.31, respectively). In Asian children, the prevalence of myopia, hyperopia and astigmatism was 3.98% (95% CI = 3.11-5.09%), 13.47% (95% CI= 11.8-15.3%) and 8.29% (95% CI=7.01-9.80%), respectively. The prevalence of WTR, ATR and OBL astigmatism was 6.50%, 0.80% and 1.00% respectively. The prevalence of hyperopia was higher in girls than boys (p=0.0002), but no significant differences were found for myopia and astigmatism.
Conclusion
Hyperopia was the most common refractive error in both Asian and NHW children. However, compared to NHW children, myopia was relatively more prevalent, and hyperopia less prevalent, in Asian children. The prevalence of astigmatism was highest in infants, and WTR astigmatism predominated at all ages. Myopia showed relatively stable prevalence across age groups, while hyperopia prevalence decreased after infancy and then increased again in older age groups; however, longitudinal studies are needed to evaluate refractive changes over time in individual children.
The population-based Multi-Ethnic Pediatric Eye Disease Study (MEPEDS) was designed to investigate the prevalence of vision disorders in 6 to 72 month old children from four racial/ethnic groups (African-American, Asian, Hispanic and Non-Hispanic White) in Los Angeles and Riverside Counties, California. An intensive interview and comprehensive eye exam including cycloplegic refraction was performed.
In previous publications we presented the data regarding prevalence of refractive error in African-American and Hispanic children.1,2 This report focuses on the age- and gender-specific prevalence of myopia, hyperopia and astigmatism in Non-Hispanic White (NHW) and Asian children. The prevalence of refractive error is compared to that in African-American and Hispanic children.
Methods
The detail methods are published in an accompanying paper.3,4 Refractive error was determined by cycloplegic refraction performed with the Retinomax Auto-refractor (Right Manufacturing, Virginia Beach, VA) at least 30 minutes after instillation of the last of two drops of 1% cyclopentolate (0.5% if child <=12 months) separated by 5 minutes. Cycloplegic retinoscopy was performed if Retinomax readings with confidence ratings of >=8 were not obtained in both eyes after 3 attempts. Non-cycloplegic retinoscopy was performed if parents did not allow cycloplegic eye drops.
Definitions of Myopia, Hyperopia and Astigmatism
Spherical equivalent (SE) refractive error was calculated as the sphere power plus 1/2 of the cylinder power. Myopia was defined as SE <=−1.00 diopter (D), and hyperopia as SE >=+2.00 D in the worse eye for the primary analysis. We also calculated myopia and hyperopia prevalence for the worse eye using a variety of threshold definitions of myopia and hyperopia, varying by 1.00 D increments. Emmetropia was defined as SE refractive error between −1.00 D and +1.00 D, non-inclusive. The worse eye was defined as the eye with the greater absolute value of SE refractive error. In case of ties (equal absolute values, but one eye myopic and the other hyperopic), the child would be classified both as a myope and as a hyperope. If only one eye had refractive error data, that eye was considered to be the worse eye.
Cylindrical refractive error was expressed as positive correcting cylinder form. Astigmatism was defined using two different threshold levels of cylindrical (cyl) refractive error in the worse eye: >=1.50 diopter (D) and >=3.00 D. Astigmatism type was defined as with-the-rule (WTR) (+ cylinder axis 90° ± 15°) and against-the-r ule (ATR) (+ cylinder axis 180° ± 15°); all other orientations were considered oblique (OBL). The worse eye was defined as the eye with the greater cylindrical refractive error, regardless of axis. When both eyes had equal absolute amounts of cylinder, an eye with OBL astigmatism was considered worse than a fellow eye having WTR or ATR astigmatism. For children with equal absolute amounts of cylinder >=1.50 D in the two eyes having WTR in one eye and ATR in the other, the child was counted among both children with worse eye WTR astigmatism and children with worse eye ATR astigmatism. If only one eye had refractive error data, that eye was considered to be the worse eye.
We used the vector analysis method modified by Thibos5 to decompose the refractive cylinder into J0 (Cartesian) and J45 (Oblique) vector components as follows: J0= −C/2Cos2α, J45=−C/2Sin2α. Where C is cylindrical power and α is the axis in degrees. The J0 vector describes a Jackson cross-cylinder (JCC) with its axes at 90° and 180°. A positive J0 represents with-the-rule astigmatism while a negative J0 represents against-the-rule astigmatism. The J45 vector describes a JCC with its axes at 45°and 135°, representing oblique astigmatism; a J45 value <0 corresponds to a plus cylinder axis <90°.
Statistical Analysis
Prevalence was calculated as the ratio of participants with the particular type of refractive error to the total number of children who successfully completed refraction for at least one eye. Results are presented for 6 age ranges, referred to herein as age groups. Logistic regression was used to compare the prevalence of refractive error between ethnic, gender and age groups. Trends over age were analyzed using logistic regression analysis. All analyses employed SAS 9.2 software (SAS institute, Inc., Cary, NC) with a 0.05 significance level. A locally weighted regression line of estimated prevalence of refractive error by months of age was fitted using MATLAB software (The Mathworks, Inc., Natick, MA).
Results
Study Cohort
9,197 children completed clinical eye examinations out of 11,534 eligible children identified by door to door census of 100 census tracts. NHW children were recruited from Riverside and Glendale and the participation rate was about 82%. Asian children were recruited from Monterey Park and Alhambra and the participation rate was about 87%. The majority of Asian children are Chinese.
Of the children who completed both the in-home interview and clinical examination, 1514 were NHW and 1525 were Asian. 13 NHW and 18 Asian children could not be refracted in either eye, leaving 1501 (99.1%) NHW and 1507 (98.8%) Asian children who were successfully refracted in at least one phakic eye. With the exception of 5 NHW and 6 Asian participants for whom refraction was possible in only one eye, refraction data were available for both eyes of all children. There were no cases with myopia in one eye and hyperopia in the other of equal magnitude of 1.00 D or more.
The demographic characteristics of these participants are shown in Table 1. The proportion of NHW participants who are male was slightly higher than that of female participants (53% vs. 47%, p=0.03). The proportions of male and female Asian participants in Asian were well balanced (51% vs. 49%, p=0.49). There was no significant difference in gender or age range distributions between NHW and Asian children (p=0.31 and p=0.71, respectively).
Table 1. Age and Gender Frequency Distributions of the Non-Hispanic White and Asian Children in the Multi-Ethnic Pediatric Eye Disease Study.
| Non-Hispanic White n (%) |
Asian n (%) |
Total n (%) |
|
|---|---|---|---|
| Age Group | |||
| 6-11 months | 123 (8%) | 133 (9%) | 256 (9%) |
| 12-23 months | 225 (15%) | 239 (16%) | 464 (15%) |
| 24-35 months | 249 (17%) | 256 (17%) | 505 (17%) |
| 36-47 months | 303 (20%) | 272 (18%) | 575 (19%) |
| 48-59 months | 273 (18%) | 287 (19%) | 560 (19%) |
| 60-72 months | 328 (22%) | 320 (21%) | 648 (22%) |
| Total | 1501 | 1507 | 3008 |
| Gender | |||
| Male | 789 (53%) | 767 (51%) | 1556 (52%) |
| Female | 712 (47%) | 740 (49%) | 1452 (48%) |
The parents of 193 NHW participants (12.9%) and 178 Asian participants (11.8%) refused cycloplegic eye drops; these children were examined with non-cycloplegic retinoscopy. Cycloplegic auto-refraction was unsuccessful in one or both eyes of 204 NHW and 298 Asian children who received cycloplegic eye drops; in these cases, cycloplegic retinoscopy was performed and analyzed for both eyes.
Distribution of Refractive Error by Age and Ethnicity
Table 2 (available at http://aaojournal.org) provided mean SE and cylindrical refractive error, in addition to mean J0 and J45 for both eyes stratified by age group. The overall mean SE refractive error for NHW children was 1.33 D (±1.15) for the right eyes and 1.34 D (±1.22) for the left eyes, and that for Asian children was 0.83 D (±1.18) for the right eyes and 0.84 D (±1.18) for the left eyes. The overall mean absolute cylindrical refractive error for NHW was 0.39 D (±0.50) for the right eyes and 0.38 D (±0.49) for the left eyes, and that for Asian was 0.48 D (±0.58) for the right eyes and 0.46 D (±0.58) for the left eyes.
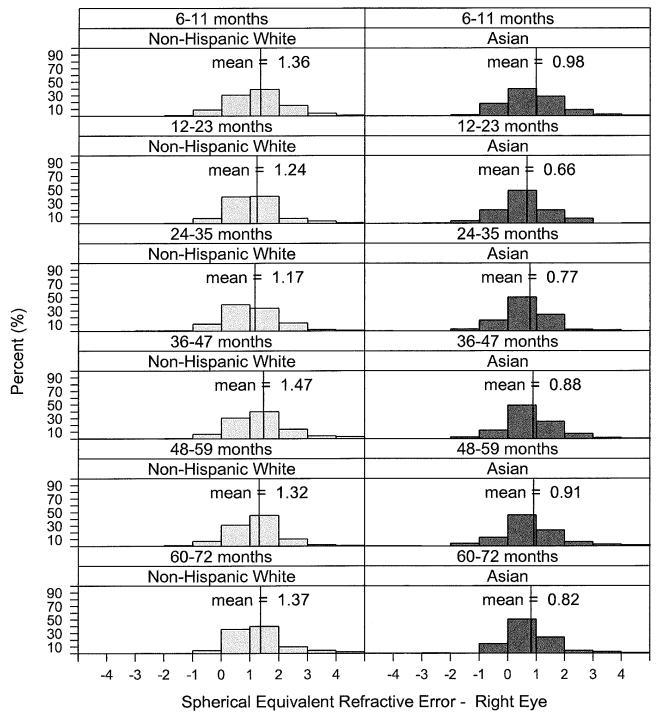
Figure 1 shows the histograms of SE refractive error of the right eye in 1 D intervals for the 6 age groups for both ethnicities. The distributions show peaks around the mean.
Figure 1.
Distribution of SE refractive error of the right eye stratified by level of refractive error, age, and ethnic group in the Multi-Ethnic Pediatric Eye Disease Study (MEPEDS). Horizontal axis shows the SE refractive error in 1 Diopter intervals. SE: Spherical equivalent refractive error
Prevalence of Myopia, Hyperopia and Astigmatism
Table 3 (available at http://aaojournal.org) provided the prevalence of myopia, hyperopia, and emmetropia determined by different threshold values of refractive error for the worse eye, stratified by age group, for NHW and Asian children 6 to 72 months of age. The overall prevalence of myopia (<= −1.00 D) was 1.20% (95% CI = 0.76%-1.89%) for NHW and 3.98% (95% CI = 3.11%-5.09%) for Asian children. The prevalence of myopia among only those children whose refractions were determined by cycloplegic auto-refraction (not including cycloplegic and non-cycloplegic retinoscopy refractions) was 1.27% for NHW and 4.17% for Asian. No difference was seen in the prevalence of myopia between genders in either NHW or Asian children (p=0.79 and p=0.35, respectively). Myopia prevalence was not associated with age in either racial/ethnic group (p=0.82 and p=0.31, respectively). Hyperopia (SE >=+2.00 D) was present in 25.7% (95% CI = 23.5%-27.9%) of NHW children and 13.5% (95% CI = 11.8%-15.3%) of Asian children. The prevalence of hyperopia for only those children who underwent cycloplegic auto-refraction was 28.8% for NHW and 15.8% for Asian.
There was no significant gender difference in the prevalence of hyperopia in NHW children (p= 0.08), however among Asian children, the prevalence of hyperopia was significantly higher in girls (16.2%) than that in boys (10.8%) (p=0.002). Hyperopia was not associated with age in either racial/ethnic group (p=0.31 and p=0.15, respectively).
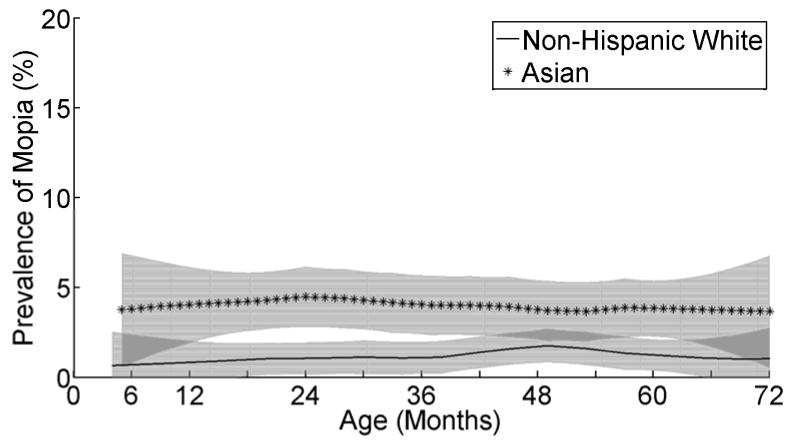
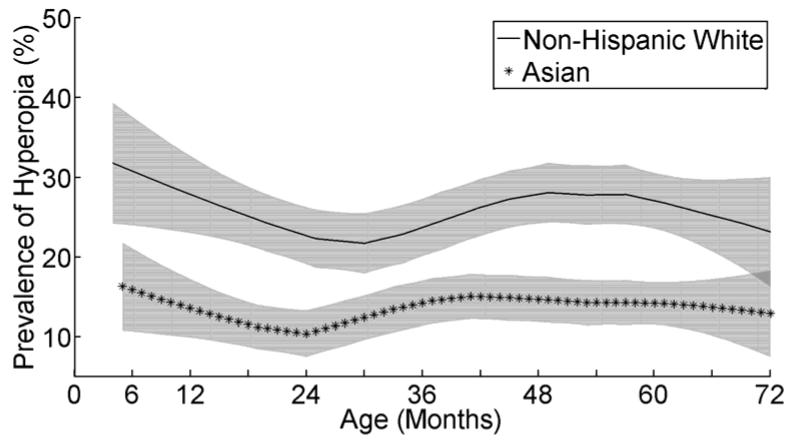
Figures 2 and 3 showed LOWESS plots of the prevalence of myopia (SE <=−1.00 D) and hyperopia (SE >=+2.00 D) by month of age in 6 to 72 month old children. Prevalence of myopia appears relatively stable across the age range with no significant trend. The prevalence of hyperopia, however, is lowest around 30 months of age, peaks in children approximately 52 months of age and then is lower in children up to 72 months of age in NHW children. In Asian children, the prevalence of hyperopia is lowest around 24 months, peaks around 42 months and stays relatively stable thereafter. Based on the variable course of hyperopia in the LOWESS graphs, subgroup trend analysis of hyperopia prevalence with age was performed in NHW and Asian children for different age ranges (Figures 2 and 3). NHW children showed a significant decreasing trend with age in children < 30 months (p=0.04) and a significant increasing trend in children 30 to <52 months (p=0.04). Asian children showed a significant increasing trend in children 24 to <42 months (p=0.01), but no significant trends among children <24 months or >=42 months of age (p= 0.07 and p=0.97, respectively).
Figure 2.
Locally weighted regression lines derived for prevalence of myopia as a function of age in months for Non-Hispanic White and Asian children in the Multi-Ethnic Pediatric Eye Disease Study. Vertical axis shows the estimated prevalence of myopia (SE <=−1.00 D) in the worse eye. Gray shading represent 95% confidence interval of the estimated prevalence. SE: Spherical equivalent refractive error; D: diopters
Figure 3.
Locally weighted regression lines derived for prevalence of hyperopia as a function of age in months for Non-Hispanic White and Asian children in the Multi-Ethnic Pediatric Eye Disease Study. Vertical axis shows the estimated prevalence of hyperopia (SE >=2.00 D) in the worse eye. Gray shading represent 95% confidence interval of the estimated prevalence. SE: Spherical equivalent refractive error; D: diopters
Prevalence of Astigmatism and its subtypes
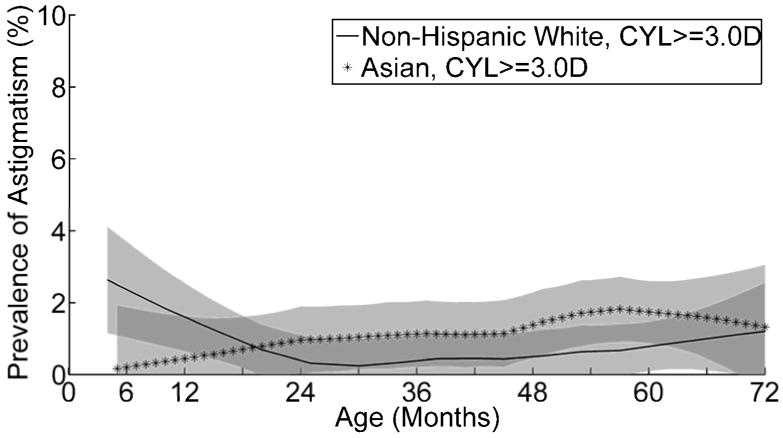
Table 4 and Table 5 (available at http://aaojournal.org) showed astigmatism prevalence in the worse eye stratified by age group, using two different threshold definitions of astigmatism. The overall prevalence of astigmatism >=1.50 D was 6.33% (95% CI = 5.21%-7.68%) in NHW and 8.29% (95% CI = 7.01%-9.80%) in Asian children. Excluding children with cycloplegic and non-cycloplegic retinoscopy refractions, the prevalence of astigmatism among children undergoing cycloplegic auto-refraction was similar to the overall prevalence (6.55% in NHW and 8.44% in Asian). There was no significant gender difference in the prevalence of astigmatism >=1.50 D in either NHW or Asian children. The prevalence of astigmatism >=1.50 D was lower among each subsequent older age category in NHW children (p<0.0001), but not in Asian children (p=0.13). The overall prevalence of astigmatism >=3.00 D was 0.73% (95% CI = 0.41%-1.31%) in NHW and 1.19% (95% CI = 0.76%-1.88%) in Asian. There was no significant gender difference, and no significant trend with age in either NHW or Asian children.
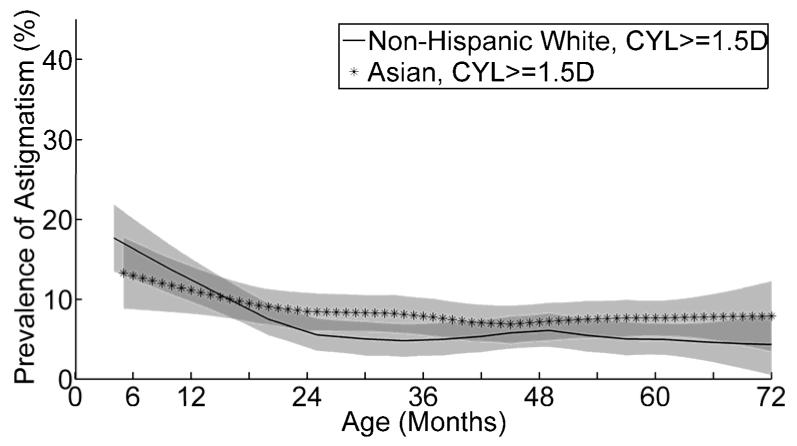
Figures 4 and 5 showed LOWESS plots of the prevalence of astigmatism >=1.50 D and >=3.00 D by month of age in NHW and Asian children. The apparent drop in the prevalence of astigmatism >=1.50 D with increasing age is most pronounced at early ages in both NHW and Asian children. Subgroup trend analysis of the prevalence of astigmatism >=1.50 D with age confirmed this. The prevalence of astigmatism >=1.50 D showed a significant decreasing trend by age in NHW children under 30 months of age (p=0.0003) and in Asian children under 24 months of age (p=0.02). Although the prevalence of astigmatism >=3.00 D appeared to show different trend patterns with age in NHW and Asian children, the numbers of cases in each age group were very small. Nonetheless, the prevalence of astigmatism >=3.00 D did show a significant decreasing trend by age in NHW children under 30 months of age (p=0.04).
Figure 4.
Locally weighted regression lines derived for prevalence of astigmatism as a function of age in months for Non-Hispanic White children in the Multi-Ethnic Pediatric Eye Disease Study. Vertical axis shows the estimated prevalence of astigmatism >=1.50 D in the worse eye (CYL >=1.50 D). Gray shading represent 95% confidence interval of the estimated prevalence. CYL: cylindrical refractive error; D: diopters.
Figure 5.
Locally weighted regression lines derived for prevalence of astigmatism as a function of age in months for Non-Hispanic White children in the Multi-Ethnic Pediatric Eye Disease Study. Vertical axis shows the estimated prevalence of astigmatism >=3.00 D in the worse eye (CYL >=3.00 D). Gray shading represent 95% confidence interval of the estimated prevalence. CYL: cylindrical refractive error; D: diopters.
Table 4 and Table 5 (available at http://aaojournal.org) also presented the prevalence of different subtypes of astigmatism >=1.50 D and >=3.00 D. For astigmatism >=1.50 D, subtype prevalence in NHW children was 4.33%, 1.00%, and 1.00% for WTR, ATR, and OBL astigmatism respectively, and subtype prevalence in Asian children was 6.50%, 0.80%, and 1.00% respectively. WTR was the most common type of astigmatism at all ages for both astigmatism >=1.50 D and astigmatism >=3.00 D.
Comparison with African-American and Hispanic Children
The overall prevalence of myopia >=1.00 D in NHW children (1.20%) was the lowest among the four racial/ethnic groups studied in the MEPEDS. It was statistically significantly lower than the prevalence seen in African-American children (6.6%), Hispanic children (3.7%) or Asian children (3.98%) after adjustment for age and gender (p<0.0001 for all comparisons).1 The overall prevalence of myopia >=1.00 D in Asian children was the second highest among the four racial/ethnic groups. After adjustment for age and gender, it was significantly lower than that in African-American children (p=0.01), but not significantly different from that in Hispanic children (p=0.45).1
The overall prevalence of hyperopia >=2.00 D in Asian children (13.47%) was the lowest among the four racial/ethnic groups. It was statistically significantly lower than the prevalence seen in African-American (20.8%), Hispanic children (26.9%) or NHW (25.65%) after adjustment for age and gender (p<0.0001 for all comparisons). The overall prevalence of hyperopia >=2.00 D in NHW children was the second highest among the four racial/ethnic groups. After adjustment for age and gender, it was significantly higher than that in African-American children (p=0.0003), but not significantly different from that in Hispanic children (p=0.44).1
The prevalence of astigmatism >=1.50 D in NHW children (6.33%) was the lowest among the four racial/ethnic groups. It was significantly lower than that in African-American (12.7%), Hispanic (16.8%) or Asian children (8.29%) after adjustment for age and gender (p<0.0001, p<0.0001, p=0.048 respectively). The prevalence of astigmatism >=1.50 D in Asian was the second lowest among the four racial/ethnic groups. After adjustment for age and gender, it was significantly lower than that in African-American and Hispanic children (p<0.0001 for both comparisons).2 Mean cylindrical power in NHW was significantly lower than all the other three racial/ethnic groups (p<0.05 for all comparisons). Mean cylindrical power in Asian children was the second lowest, and was significantly lower than that in African-American and Hispanic children (p<0.05 for both comparisons).
Discussion
Using the data from this large, population-based multi-ethnic study, we presented prevalence estimates for myopia, hyperopia and astigmatism in NHW and Asian children aged 6 to 72 months old. Mean SE refractive error was hyperopic in NHW in all age groups, and more hyperopic than that in Asian or African-American and Hispanic children in the MEPEDS.1 The Baltimore Pediatric Eye Disease Study (BPEDS), a population-based study paralleling the MEPEDS and examining African-American and NHW children, also reported hyperopic values for mean SE refractive error in NHW children, slightly higher (1.49 D ± 1.23 for right eyes) than in our participant population (1.33 D ±1.15 for right eyes).6 By contrast, mean SE refractive error was <1.0 D in Asian children in all age groups and the overall mean was less hyperopic than in all other racial/ethnic groups studied in the MEPEDS. The Strabismus, Amblyopia and Refractive Error in Singaporean Children (STARS) is a population-based study in southwest Singapore examining Singaporean Chinese children aged 6 to 72 months (sample size n=2639); the STARS also reported relatively emmetropic mean SE refractive error (0.69D ± 1.15 for right eyes).7
In MEPEDS, NHW children had a high prevalence of hyperopia and a low prevalence of myopia compared to other racial/ethnic groups, while the opposite was true for Asians. BPEDS showed very similar prevalence of myopia >=1.00 D in NHW (1.1%), which was also much lower than that in their African-American population. And BPEDS reported an even higher prevalence of hyperopia >=2.00 D in Whites (31.5%), which was likewise significantly higher than that in African-American children (17.4%). Compared to Asian children in our study, STARS reported an even higher prevalence of myopia in their population (5.2%, using a myopia definition of at least −1.00 D). The difference with STARS is largely due to a relatively higher prevalence of myopia in children aged 24 to 35 months in STARS (10.2%), compared to ours (3.91%). The prevalence was very comparable in other age ranges between STARS and MEPEDS. And STARS reported an even lower prevalence of hyperopia in their population (7.5%). In children aged 24 months or older, STARS consistently had a lower prevalence of hyperopia compared to MEPEDS children in all age groups.
This finding also supports earlier non-population-based studies. The classic study of Cook and Glasscock of newborn infants similarly found a lower prevalence of myopia greater than 1D in White children (14.3%) compared to African-American children (23.5%), using atropine cycloplegia.8 The non-population based Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error (CLEERE) study on older school-aged children, reported similar patterns for the prevalence of myopia and hyperopia in NHW and Asians, compared to African-Americans and Hispanics.9
The difference in prevalence of myopia and hyperopia between ethnicities is likely to be multifactorial. Both life style/environmental factors and genetics might contribute. Recently, outdoor activity, time spent outdoors and light intensity have been proposed as factors affecting myopia and hyperopia prevalence.10,11 Furthermore, genetically determined factors (such as eye pigmentation) may theoretically interact with environmental influences (such as outdoor light exposure) to impact refractive development.
Although Asian children in this study had a higher prevalence of myopia than NHW children, it is important to note that even among Asian children, the prevalence of myopia was low in this preschool population, and hyperopia was 3 to 4 times more common than myopia. This contrasts markedly with the high frequency of myopia and low frequency of hyperopia seen in older Asian children. Even in the oldest preschool age-group studied in MEPEDS, and even using a less stringent myopia definition of 0.5 D or more, MEPEDS found a myopia prevalence of only 6.6% in 5 year-old children (Table 3). The Refractive Error Study in Children (RESC) found a similar myopia prevalence (5.7%) for urban Chinese 5 year-olds studied using autorefraction, the prevalence of hyperopia (2D or more) was 17.0%12 By contrast, among 15 year-olds, the myopia prevalence was 78.4%, while the prevalence of hyperopia was <1%.
In the MEPEDS, the prevalence of myopia remained relatively steady throughout the 6 to 72 month age range in both NHW and Asian children. This finding was different from the decreasing prevalence of myopia with increasing age in Hispanic and African-American children, and may be related to the fact that the prevalence of myopia in the youngest age group is considerably lower in NHW and Asian children than in the other two racial/ethnic groups. As shown in previous studies, the rate of emmetropization is greater with larger initial refractive errors.13,14 This study cannot determine whether higher levels of myopia are present in the first 6 months of life in NHW and Asian children, with emmetropization largely completed prior to the youngest ages included in the present study, or whether myopia prevalence is stable from early infancy onward.
Our finding of a relatively low rate of myopia in preschool Asian children that varies little with increasing age reinforces the findings of earlier studies on young Chinese children, such as the study of Chen at al15 showing that most Chinese neonates are hyperopic, and the study of Chan and Edwards,16 which showed that spherical refractive error in Chinese preschool children changes little before the age of 6 years.
In the MEPEDS, the prevalence of hyperopia >=2.00 D decreased from 6 months of age to a low point around 30 months of age in NHW and around 24 months of age in Asian children. This is reminiscent of our findings in Hispanic and African-American children as well as previous reports describing early emmetropization.1,13,17,18 This pattern was similar in all four racial/ethnic groups, although the lowest prevalence of hyperopia occurred at slightly different ages in different racial/ethnic groups.
Myopia and hyperopia were not associated with gender in our Non-Hispanic White children. This is consistent with our previous findings in African-American and Hispanic children.1 Myopia was not associated with gender in Asian children. However, there was a higher prevalence of hyperopia in Asian girls compared to boys. STARS also reported similar myopia prevalence between genders (5.6% for girls and 5.0% for boys), and a higher hyperopia prevalence in girls than in boys (9.4% vs 6.3%).
NHW and Asian preschool children showed less astigmatism than their African-American and Hispanic counterparts and NHW was the lowest. The BPEDS similarly found a lower prevalence of astigmatism >=1.50 D in White children compared to African-Americans, although the prevalence in White children was higher than that in our study (11.4% vs 6.32%).6 In a population-based study of 6 year-old White children in Australia,19,20 the prevalence of astigmatism >=1.50 D was 4.8%, which was similar to the prevalence of astigmatism in our 5 year old NHW children (4.32%). In Asian children, STARS found almost the same prevalence of astigmatism >=1.50 D (8.3%) as that found in our Asian population (8.29%), with a similar distribution of astigmatism subtypes.7
The prevalence of astigmatism showed a decreasing trend with age in younger age ranges in NHW (<30 months) and Asian (<24 months), similar to that seen in African-American and Hispanic children. In all four racial/ethnic groups a stable prevalence level was reached between 24 and 36 months of age. The more prominent early drop in the prevalence of Hispanic children may be a manifestation of higher rates of emmetropization associated with higher baseline refractive errors, a pattern that has been previously observed in other studies.2,13,17,18 Mean absolute cylindrical power also decreased with age in NHW and Asian children, similar to what was reported for the other two racial/ethnic groups (p<0.05 for all).2 Similar decreases in astigmatism prevalence with increasing age were reported in the Baltimore Pediatrics Eye Disease Study.6 Other non-population-based studies, including both cross-sectional21,22 and longitudinal studies23-29 have also reported a decreasing trend with age for astigmatism.
WTR astigmatism was by far the most common form in all age groups in NHW and Asian children, similar to Hispanics and African-Americans. The positive values of mean J0 reflect the dominance of WTR relative to ATR astigmatism, especially in the youngest age group. A similar predominance of WTR astigmatism was seen in the population-based BPEDS6 and STARS7 examining the same age range of preschool children, and also in some non-population based studies in various ethnic groups,13,30 although others have shown a higher prevalence of ATR astigmatism.26,27 Some studies have reported a shift in the predominance of ATR astigmatism in younger children to predominance of WTR in older children,24,25 not observed in this study.
There are limitations to this study that need to be acknowledged. The cross-sectional nature of this study imposes some limitations on our interpretations of the findings. While cross-sectional refractive error distributions in different age groups suggest age-related trends such as emmetropization, only longitudinal data can provide definitive evidence that refractive error distributions change over time in a given group of children. Furthermore, cross-sectional data cannot predict the longitudinal behavior of individuals. Population-based longitudinal studies are required to further elucidate age-related trends in refractive error in individual children. In addition, ethnicity related differences have not been controlled for risk factors other than age and gender in this report. Other factors such as prenatal and postnatal risk factors, environmental exposures such as smoking,31,32 level of outdoor activity and light exposure, and nutrition and other life style differences may play important roles in ethnic group differences.
One additional theoretical limitation of this study is that it is difficult to prove whether differently pigmented eyes (in different ethnic groups) undergo a similar degree of cycloplegia using the cycloplegic regimen of two drops of 1% cyclopentolate (0.5% in children <12 months of age). The RESC also used two drops of 1% cyclopentolate, but required a formal assessment of the adequacy of pupillary dilation and the addition of a third drop of cyclopentolate if needed. We believe for several reasons that our overall study findings are valid despite this methodological difference. First, MEPEDS and RESC findings for myopia prevalence in 5 year-old children are similar for both Asian children (discussed above) and Hispanic children.1,33 African-American children in the MEPEDS did have a higher rate of myopia than African children in the RESC, but they also had a much higher rate of hyperopia than the RESC, which is inconsistent with the hypothesis of inadequate cycloplegia.1,34 Second, we have compared atropine cycloplegia to the MEPEDS cycloplegic regimen in the darkly pigmented eyes of 24 African-American and Hispanic hyperopes (>=2.0 D) in the MEPEDS (Sanchez RN, Choudhury F, Tarczy-Hornoch K, et al. Effect of cyclopentolate versus atropine on cycloplegic refraction: the Multi-Ethnic Pediatric Eye Disease Study. Poster presented at ARVO Annual Meeting, April 27-May 1, 2008; Fort Lauderdale). Although we would expect hyperopes to show the largest effects of inadequate cycloplegia, because of their habitual accommodation, we found that the mean amount of additional hyperopia unmasked with atropine was less than 0.5 D, and in only 1 child did it exceed 0.75 D. In summary, it is conceivable that we might have found slightly lower myopia prevalence and slightly higher hyperopia prevalence in African-American, Hispanic and Asian preschool children had we used the RESC cycloplegic regimen rather than the MEPEDS cycloplegic regimen, but we do not believe the differences would have been substantial.
Strengths of the MEPEDS include large sample size with high participation rate, population-based data, and rigorous examination protocols with excellent quality control. We believe our findings may be generalizable to NHW and Asian children throughout the United States.
In conclusion, this is a unique population-based study using cycloplegic refraction to assess refractive error prevalence in NHW, Asian, African-American and Hispanic children 6-72 months old. Myopia was relatively less prevalent, and hyperopia more prevalent, in NHW as compared to Asian children, although hyperopia was the most common refractive error in both groups. The prevalence of astigmatism was highest in infants, and WTR astigmatism predominated at all ages. Myopia and hyperopia showed relatively stable prevalence across age groups; however, longitudinal studies are needed to evaluate refractive changes over time in individual children.
Supplementary Material
Hyperopia was the most common refractive error in both Non-Hispanic White and Asian children. As compared to Asian children, Non-Hispanic White children have a significant higher prevalence of hyperopia, lower prevalence of myopia and astigmatism.
Acknowledgments
The Multi-Ethnic Pediatric Eye Disease Study investigators would like to thank the following members of the National Eye Institute’s Data Monitoring and Oversight Committee for their substantial contributions through critical review and advice: Jonathan M. Holmes, MD (Chair), Eileen E. Birch, PhD, Karen J. Cruickshanks, PhD, Natalie Kurinij, PhD, Maureen G. Maguire, PhD, Joseph M. Miller, MD, MPH, Graham E. Quinn, MD, and Karla Zadnik, OD, PhD.
Support: Supported by the National Eye Institute, National Institutes of Health, Bethesda, MD (grant nos. EY14472 and EY03040), and an unrestricted grant from the Research to Prevent Blindness, New York, NY. Dr. Varma is a Research to Prevent Blindness Sybil B. Harrington Scholar.
Footnotes
Conflicts of Interest: The authors have no proprietary or commercial interest in any materials discussed in the manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
This article contains online-only material. The following should appear online-only: Table 2-5 and Appendix 1.
References
- 1.Multi-Ethnic Pediatric Eye Disease Study Group Prevalence of myopia and hyperopia in 6- to 72-month-old African American and Hispanic children: the Multi-Ethnic Pediatric Eye Disease Study. Ophthalmology. 2010;117:140–7. doi: 10.1016/j.ophtha.2009.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fozailoff A, Tarczy-Hornoch K, Cotter S, et al. Writing Committee for the MEPEDS Study Group. Prevalence of astigmatism in 6- to 72-month-old African American and Hispanic children: the Multi-Ethnic Pediatric Eye Disease Study. Ophthalmology. 2011;118:284–93. doi: 10.1016/j.ophtha.2010.06.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Varma R, Deneen J, Cotter S, et al. The Multi-Ethnic Pediatric Eye Disease Study Group. The Multi-Ethnic Pediatric Eye Disease Study: design and methods. Ophthalmic Epidemiol. 2006;13:253–62. doi: 10.1080/09286580600719055. [DOI] [PubMed] [Google Scholar]
- 4.The Multi-Ethnic Pediatric Eye Disease Study Group Prevalence of amblyopia or strabismus in Asian and Non-Hispanic White preschool children: Multi-Ethnic Pediatric Eye Disease Study. Ophthalmology. doi: 10.1016/j.ophtha.2013.03.001. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thibos LN, Wheeler W, Horner D. Power vectors: an application of Fourier analysis to the description and statistical analysis of refractive error. Optom Vis Sci. 1997;74:367–75. doi: 10.1097/00006324-199706000-00019. [DOI] [PubMed] [Google Scholar]
- 6.Giordano L, Friedman DS, Repka MX, et al. Prevalence of refractive error among preschool children in an urban population: the Baltimore Pediatric Eye Disease Study. Ophthalmology. 2009;116:739–46. doi: 10.1016/j.ophtha.2008.12.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dirani M, Chan YH, Gazzard G, et al. Prevalence of refractive error in Singaporean Chinese children: the Strabismus, Amblyopia, and Refractive Error in young Singaporean Children (STARS) study. Invest Ophthalmol Vis Sci. 2010;51:1348–55. doi: 10.1167/iovs.09-3587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cook RC, Glasscock RE. Refractive and ocular findings in the newborn. Am J Ophthalmol. 1951;34:1407–13. doi: 10.1016/0002-9394(51)90481-3. [DOI] [PubMed] [Google Scholar]
- 9.Kleinstein RN, Jones LA, Hullett S, et al. Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error Study Group. Refractive error and ethnicity in children. Arch Ophthalmol. 2003;121:1141–7. doi: 10.1001/archopht.121.8.1141. [DOI] [PubMed] [Google Scholar]
- 10.Ashby R, Ohlendorf A, Schaeffel F. The effect of ambient illuminance on the development of deprivation myopia in chicks. Invest Ophthalmol Vis Sci. 2009;50:5348–54. doi: 10.1167/iovs.09-3419. [DOI] [PubMed] [Google Scholar]
- 11.Rose KA, Morgan IG, Ip J, et al. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology. 2008;115:1279–85. doi: 10.1016/j.ophtha.2007.12.019. [DOI] [PubMed] [Google Scholar]
- 12.He M, Zeng J, Liu Y, et al. Refractive error and visual impairment in urban children in southern China. Invest Ophthalmol Vis Sci. 2004;45:793–9. doi: 10.1167/iovs.03-1051. [DOI] [PubMed] [Google Scholar]
- 13.Ehrlich DL, Braddick OJ, Atkinson J, et al. Infant emmetropization: longitudinal changes in refraction components from nine to twenty months of age. Optom Vis Sci. 1997;74:822–43. doi: 10.1097/00006324-199710000-00022. [DOI] [PubMed] [Google Scholar]
- 14.Saunders KJ, Woodhouse JM, Westall CA. Emmetropisation in human infancy: rate of change is related to initial refractive error. Vision Res. 1995;35:1325–8. doi: 10.1016/0042-6989(94)00222-8. [DOI] [PubMed] [Google Scholar]
- 15.Chen J, Xie A, Hou L, et al. Cycloplegic and noncycloplegic refractions of Chinese neonatal infants. Invest Ophthalmol Vis Sci. 2011;52:2456–61. doi: 10.1167/iovs.10-5441. [DOI] [PubMed] [Google Scholar]
- 16.Chan OY, Edwards M. Refractive errors in Hong Kong Chinese pre-school children. Optom Vis Sci. 1993;70:501–5. doi: 10.1097/00006324-199306000-00009. [DOI] [PubMed] [Google Scholar]
- 17.Pennie FC, Wood IC, Olsen C, et al. A longitudinal study of the biometric and refractive changes in full-term infants during the first year of life. Vision Res. 2001;41:2799–810. doi: 10.1016/s0042-6989(01)00169-9. [DOI] [PubMed] [Google Scholar]
- 18.Mutti DO, Mitchell GL, Jones LA, et al. Axial growth and changes in lenticular and corneal power during emmetropization in infants. Invest Ophthalmol Vis Sci. 2005;46:3074–80. doi: 10.1167/iovs.04-1040. [DOI] [PubMed] [Google Scholar]
- 19.Ip JM, Kifley A, Rose KA, Mitchell P. Refractive findings in children with astigmatic parents: the Sydney Myopia Study. Am J Ophthalmol. 2007;144:304–6. doi: 10.1016/j.ajo.2007.03.054. [DOI] [PubMed] [Google Scholar]
- 20.Ojaimi E, Rose KA, Smith W, et al. Methods for a population-based study of myopia and other eye conditions in school children: the Sydney Myopia Study. Ophthalmic Epidemiol. 2005;12:59–69. doi: 10.1080/09286580490921296. [DOI] [PubMed] [Google Scholar]
- 21.Fulton AB, Dobson V, Salem D, et al. Cycloplegic refractions in infants and young children. Am J Ophthalmol. 1980;90:239–47. doi: 10.1016/s0002-9394(14)74861-5. [DOI] [PubMed] [Google Scholar]
- 22.Mayer DL, Hansen RM, Moore BD, et al. Cycloplegic refractions in healthy children aged 1 through 48 months. Arch Ophthalmol. 2001;119:1625–8. doi: 10.1001/archopht.119.11.1625. [DOI] [PubMed] [Google Scholar]
- 23.Atkinson J, Braddick O, French J. Infant astigmatism: its disappearance with age. Vision Res. 1980;20:891–3. doi: 10.1016/0042-6989(80)90070-x. [DOI] [PubMed] [Google Scholar]
- 24.Dobson V, Fulton AB, Sebris SL. Cycloplegic refractions of infants and young children: the axis of astigmatism. Invest Ophthalmol Vis Sci. 1984;25:83–7. [PubMed] [Google Scholar]
- 25.Gwiazda J, Scheiman M, Mohindra I, Held R. Astigmatism in children: changes in axis and amount from birth to six years. Invest Ophthalmol Vis Sci. 1984;25:88–92. [PubMed] [Google Scholar]
- 26.Howland HC, Sayles N. Photorefractive measurements of astigmatism in infants and young children. Invest Ophthalmol Vis Sci. 1984;25:93–102. [PubMed] [Google Scholar]
- 27.Abrahamsson M, Fabian G, Sjostrand J. Changes in astigmatism between the ages of 1 and 4 years: a longitudinal study. Br J Ophthalmol. 1988;72:145–9. doi: 10.1136/bjo.72.2.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gwiazda J, Grice K, Held R, et al. Astigmatism and the development of myopia in children. Vision Res. 2000;40:1019–26. doi: 10.1016/s0042-6989(99)00237-0. [DOI] [PubMed] [Google Scholar]
- 29.Mutti DO, Mitchell GL, Jones LA, et al. Refractive astigmatism and the toricity of ocular components in human infants. Optom Vis Sci. 2004;81:753–61. doi: 10.1097/00006324-200410000-00007. [DOI] [PubMed] [Google Scholar]
- 30.Fan DS, Rao SK, Cheung EY, et al. Astigmatism in Chinese preschool children: prevalence, change, and effect on refractive development. Br J Ophthalmol. 2004;88:938–41. doi: 10.1136/bjo.2003.030338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McKean-Cowdin R, Varma R, Cotter SA, et al. Joint Writing Committee for the Multi-Ethnic Pediatric Eye Disease Study and the Baltimore Pediatric Eye Disease Study Groups Risk factors for astigmatism in preschool children: the Multi-Ethnic Pediatric Eye Disease and Baltimore Pediatric Eye Disease studies. Ophthalmology. 2011;118:1974–81. doi: 10.1016/j.ophtha.2011.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Borchert MS, Varma R, Cotter SA, et al. Joint Writing Committee for the Multi-Ethnic Pediatric Eye Disease Study and the Baltimore Pediatric Eye Disease Study Groups Risk factors for hyperopia and myopia in preschool children: the Multi-Ethnic Pediatric Eye Disease and Baltimore Pediatric Eye Disease studies. Ophthalmology. 2011;118:1966–73. doi: 10.1016/j.ophtha.2011.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Maul E, Barroso S, Munoz SR, et al. Refractive error study in children: results from La Florida, Chile. Am J Ophthalmol. 2000;129:445–54. doi: 10.1016/s0002-9394(99)00454-7. [DOI] [PubMed] [Google Scholar]
- 34.Naidoo KS, Raghunandan A, Mashige KP, et al. Refractive error and visual impairment in African children in South Africa. Invest Ophthalmol Vis Sci. 2003;44:3764–70. doi: 10.1167/iovs.03-0283. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.