Abstract
Background
Although iliac vein thrombus is uncommon in adolescents, it can present with pelvic inflammatory disease (PID) symptoms.
Case
A 19-year-old sexually active female with Klippel-Trenaunay syndrome (KTS) presented with fever, abdominal and lower extremity pain. Physical findings included cervical motion tenderness and left lower extremity swelling and erythema. The patient was admitted for PID and cellulitis. Despite antimicrobial treatment her pain continued. Neisseriae gonorrhea and Chlamydia trachomatis cultures were negative. Abdominal and pelvic computed tomography scans revealed a left internal iliac vein thrombus. Anticoagulation therapy was initiated; her pain improved. On hospital day 7 she developed pulmonary emboli.
Summary and Conclusion
In sexually active adolescents with known risk factors for thromboembolism such as KTS, symptoms and signs considered characteristic for PID can be present in association with an iliac vein thrombus.
Keywords: Klippel-Trenaunay syndrome, pelvic inflammatory disease, venous thromboembolism
Introduction
Klippel-Trenaunay syndrome (KTS) is an uncommon, congenital angiodysplastic syndrome characterized by vascular nevi, varicose veins, and bony and soft tissue hypertrophy of the affected extremity.1 These patients are at potential risk for hypercoagulability, thrombosis, and pulmonary embolism.2 We describe a case of a sexually active adolescent female with KTS who presented with pelvic inflammatory disease (PID) symptoms. She was ultimately diagnosed with both PID and an iliac vein thrombus.
Case Report
A 19 year old female with KTS with a one day history of abdominal and left lower extremity pain presented to an urban academic pediatric emergency department located in a community with a high prevalence of sexually transmitted infections. She had no recent history of dysuria or vaginal discharge. She was currently sexually active, and reported regularly using condoms. She had one lifetime partner. Past medical history was significant for KTS resulting in lymphedema of the upper thigh with hemangiomas extending to the hip, buttocks, and perineum. She had undergone multiple surgical procedures to debride damaged tissue and graft skin to her leg and foot, as well as embolization and laser ablation of vascular abnormalities to treat skin ulcerations. She had been hospitalized on multiple occasions for cellulitis of her left leg.
On physical examination, her initial temperature was 38.2 °C, heart rate of 102 beats per minute, respiratory rate of 28 breaths per minute. In the emergency department, her temperature increased to 40 °C. Her exam was remarkable for diffuse abdominal tenderness and guarding. Her malformed left lower extremity was found to be erythematous, tender, and swollen. Her genitourinary examination was remarkable for an extensive hemangioma at the perineum; she had both cervical motional tenderness and adnexal tenderness on bimanual exam. Neisseria Gonorrhea (GC) and Chlamydia trachomatis (CT) testing was performed using nucleic acid amplification testing (NAAT). Laboratory findings included a negative HCG, c-reactive protein (CRP) 0.5 mg/dl (reference range, 0-0.5), and a white blood cell count of 6500/cubic mm. Doppler ultrasound of her bilateral low extremities demonstrated no evidence of deep venous thrombosis, but was limited on the left due to pain. A sonogram of the pelvis revealed an enlarged retroverted uterus with minimal fluid in the lower endometrial cavity. Abdominal and pelvic computed tomography scans were also performed on the night of admission; moderate stranding in the pelvis and heterogeneous enhancement of the uterus were reported (Fig. 1). She was given a dose of clindamycin and piperacillin/tazobactam and was admitted with a presumed diagnosis of PID and cellulitis of her lower extremity.
Figure 1.
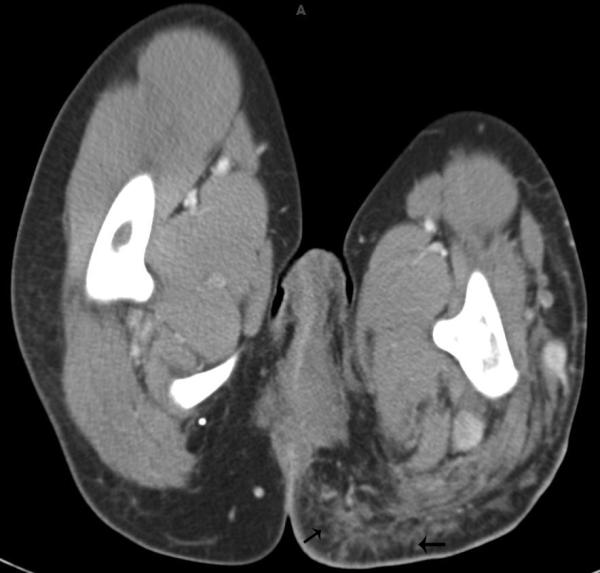
Contrast enhanced CT scan demonstrates stranding in the soft tissues of the pelvis and buttock regions (arrows).
The morning after admission, her pelvic exam was repeated, and the patient still had adnexal and cervical motion tenderness. She received 1 gram of azithromycin, and was started on IV cefoxitin and doxycycline. She continued to receive clindamycin for her presumed cellulitis. Her exam was unchanged and her pain continued despite antibiotic treatment. The NAAT testing for GC and CT was negative. On hospital day 4, her CRP increased to 27 mg/dl. Her initial computed tomography scan was reviewed with a radiologist; a thrombus was identified within the left pelvic veins, including the distal left internal iliac vein (Fig. 2). Investigations for hypercoagulability were performed, and she was treated with low-molecular weight heparin. Her abdominal pain began to improve over the next 3 days. On hospital day 7, the patient had acute shortness of breath and chest pain. Computed tomography pulmonary angiography revealed multiple small peripheral pulmonary emboli (Fig. 3). After temporarily discontinuing heparin, the patient had a vena cava filter placed, and subsequently resumed anticoagulation treatment. She completed a 14 day course of cefoxitin and doxycycline for PID. She also completed a 14 day course of clindamycin for cellulitis. She was discharged home on hospital day 15 on subcutaneous low-molecular weight heparin (1.5mg/kg twice daily).
Figure 2.
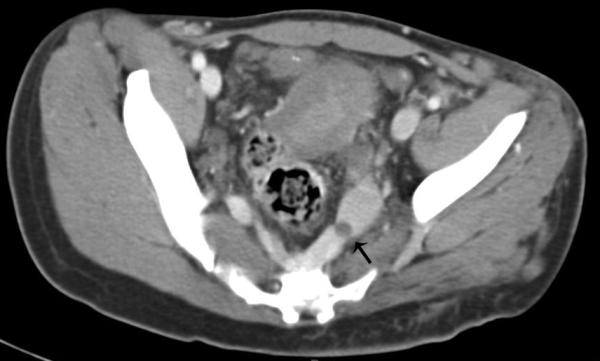
Contrast enhanced CT scan shows left internal iliac vein thrombus (arrow).
Figure 3.
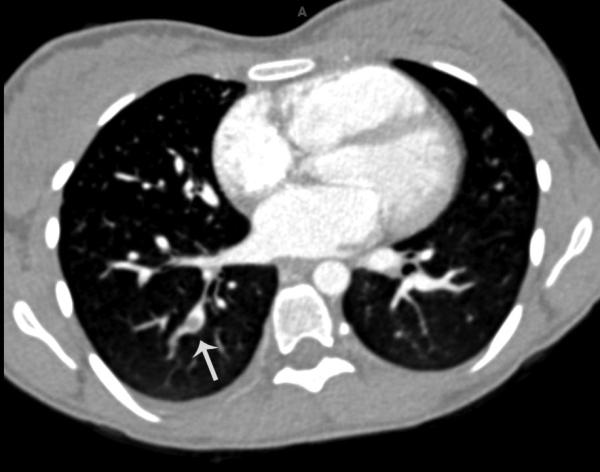
Pulmonary CT angiogram demonstrated multiple small peripheral pulmonary emboli. Note filling defect in right lower pulmonary artery (arrow).
Summary and Conclusion
A sexually active adolescent female who presents with fever, abdominal pain, cervical motion tenderness, and adnexal tenderness needs to have PID excluded due to its deleterious long-term reproductive complications. The differential diagnosis for PID includes such conditions as ectopic pregnancy, ovarian torsion, endometriosis, hemorrhagic ovarian cyst, pelvic vein thrombus, and appendicitis. Our patient had features consistent with both culture-negative PID and an internal iliac (pelvic) vein thrombosis.
In addition to characteristic historical and diagnostic findings of PID, including cervical motion tenderness, adnexal tenderness, and lower abdominal pain,3 her imaging studies were consistent with early PID. Sonographic findings in PID can include an enlarged uterus and free fluid in the cul de sac which were present in this case. Although computed tomography is seen as having a limited role in the radiological evaluation of PID,4 our patient's imaging was notable for pelvic inflammation and edema of the surrounding fat with obscuration of the pelvic fascial planes, i.e. pelvic stranding. Sam et al noted that periovarian stranding and enhancement of the adjacent peritoneum are occasionally seen in PID.5 Because negative GC/CT cervical cultures do not alone exclude infectious etiologies of PID,6 our patient was continued on 14 days of antibiotic therapy to provide additional coverage for other organisms such as gardneralla vaginalis, haemophilus influenza, enteric gram-negative rods, streptococcus agalactiae, ureaplasma urealyticum, and mycoplasma genitalium. Given her history, physical exam, and her radiographic findings, we diagnosed her with PID, despite negative cultures. However, her signs and symptoms may also have been due solely to her leg cellulitis and iliac vein thrombosis. Regardless of her final diagnosis, her PID-like presentation contributed to a delay in recognizing the iliac vein thrombus. This delay in turn likely contributed to the development of pulmonary emboli secondary to her thrombus.
In general, isolated internal iliac vein thrombi are uncommon in adolescents. Bjorgell et al previously described a case of an isolated internal iliac vein thrombosis in a healthy 18 year old female who presented with fever and right lower abdominal pain.7 The authors postulated that the abdominal pain may have been due to phlebitis and retroperitoneal edema from the iliac deep vein thrombosis. In young women, pelvic vein thromboses occur most frequently in the post-partum period, especially after cesarean section.8 Inflammation also increases the risk of venous thrombosis,9 and PID may have contributed to the development of thrombosis in this case.
KTS was first described in 1900 by two French physicians.10 The etiology is unknown. It occurs in approximately 1/30,000 live births.11 The syndrome consists of port wine stain, venous and lymphatic malformations, and soft tissue hypertrophy, primarily involving one lower extremity and the pelvis on that side. Complications include cellulitis, ulceration, and thrombophlebitis of the affected limb. Venous thromboembolism is associated with KTS in up to 8%-22% of affected patients.12 Although the etiology is unclear, Mazoyer et al proposed that the coagulopathy associated with venous malformations including KTS is due to a localized intravascular coagulation within the enlarged, malformed veins.13 Numerous case reports of pulmonary emboli have been reported in both the pediatric and adult literature.2 Huiras et al report that recurrent thromboembolic complications are common in these patients despite anticoagulation.2 Heparin may be superior to warfarin to prevent recurrence.13
Upon discharge, our patient stated her continued desire to be sexually active. Given her history of emboli, systemic estrogen-containing contraceptives were contraindicated, and the patient decided that the initial contraceptive choice should be condoms. She was later started on a long-acting progestin-only hormonal contraceptive because of her ongoing needs for a dual (hormonal and barrier) method.
In conclusion, this case report describes an adolescent with KTS diagnosed with concurrent PID and pelvic thrombus. This case underscores the potential for more than one cause of PID-like symptoms to be present in the same individual. In sexually active patients with known risk factors for thromboembolism such as venous malformations from KTS, one needs to have a high suspicion for iliac vein thrombi even in the presence of PID.
Footnotes
There are no conflicts of interest for any of the authors.
References
- 1.Muluk SC, Ginns LC, Semigran MJ, Kaufman JA, Gertler JP. Klippel-Trenaunay syndrome with multiple pulmonary emboli- an unusual cause of progressive pulmonary dysfunction. J Vasc Surg. 1995;21:686–690. doi: 10.1016/s0741-5214(95)70199-0. [DOI] [PubMed] [Google Scholar]
- 2.Huiras EE, Barnes CJ, Eichenfield LF, Pelech AN, Drolet BA. Pulmonary thromboembolism associated with Klippel-Trenaunay syndrome. Pediatrics. 2005;116:E596–600. doi: 10.1542/peds.2004-1607. [DOI] [PubMed] [Google Scholar]
- 3.Weström L, Joesoef R, Reynolds G, Hagdu A, Thompson SE. Pelvic inflammatory disease and fertility. A cohort study of 1,844 women with laparoscopically verified disease and 657 control women with normal laparoscopic results. Sex Transm Dis. 1992;19:185–92. [PubMed] [Google Scholar]
- 4.Ghiatas AA. The spectrum of pelvic inflammatory disease. Eur Radiol. 2004;14:E184–E192. doi: 10.1007/s00330-003-2043-0. [DOI] [PubMed] [Google Scholar]
- 5.Sam JW, Jacobs JE, Birnbaum BA. Spectrum of CT findings in acute pyogenic pelvic inflammatory disease. Radiographics. 2002;22:1327–1334. doi: 10.1148/rg.226025062. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention Sexually transmitted diseases treatment guidelines 2006. MMWR Morb Mortal Wkly Rep. 2006;55:1–94. [Google Scholar]
- 7.Bjorgell O, Nilsson P, Nilsson A, Loren I, Floren CH, Lindgarde F. Isolated internal iliac vein thrombosis. J Ultrasound Med. 1998;17:671–673. doi: 10.7863/jum.1998.17.10.671. [DOI] [PubMed] [Google Scholar]
- 8.Rodger MA, Avruch LI, Howley HE, Olivier A, Walker MC. Pelvic magnetic resonance venography reveals high rate of pelvic vein thrombosis after cesarean section. AM J Obstet Gynecol. 2006;194:436–437. doi: 10.1016/j.ajog.2005.07.044. [DOI] [PubMed] [Google Scholar]
- 9.Fox EA, Kahn SR. The relationship between inflammation and venous thrombosis: a systematic review of clinical studies. Thromb Haemost. 2005;94:362–365. doi: 10.1160/TH05-04-0266. [DOI] [PubMed] [Google Scholar]
- 10.Klippel M, Trenaunay P. Osteohypertrophic varicose nevus [in French]. Arch Gen Med. 1900;185:641. [Google Scholar]
- 11.Samuel M, Spitz L. Klippel-Trenaunay syndrome: clinical features, complications and management in children. Br J Surg. 1995;82:757–761. doi: 10.1002/bjs.1800820615. [DOI] [PubMed] [Google Scholar]
- 12.Baskerville PA, Ackroyd JS, Thomas ML, Browse NL. The Klippel-Trenaunay syndrome: clinical, radiological and hemodynamic features and management. Br J Surg. 1985;72:232–236. doi: 10.1002/bjs.1800720331. [DOI] [PubMed] [Google Scholar]
- 13.Mazoyer E, Enjolras O, Laurian C, Houdart E, Drouet L. Coagulation abnormalities associated with extensive venous malformations of the limbs: differentiation from Kasabach-Merritt syndrome. Clin Lab Haematol. 2002;24:243–251. doi: 10.1046/j.1365-2257.2002.00447.x. [DOI] [PubMed] [Google Scholar]


