Abstract
Background
The benefit of myocardial perfusion imaging (MPI) over exercise ECG stress testing alone is unclear in individuals attaining a workload of ≥10 METS. The purpose of this prospective study is to determine mortality and nonfatal cardiac events in patients at either intermediate pretest risk for CAD or patients with known CAD, achieving ≥10 METS regardless of peak exercise heart rate. The authors previously reported a low prevalence of significant ischemia in this patient cohort.
Methods
Baseline characteristics, ECG stress test findings, and perfusion and function results from quantitative gated 99mTc-SPECT MPI were compared by achievement of a maximum age-predicted heart rate ≥85% in 509 consecutive patients who reached ≥10 METS. Events including all-cause and cardiac mortality, non-fatal myocardial infarction (MI), and late revascularization (>4 weeks after MPI) were prospectively collected.
Results
Of the 509 patients achieving ≥10 METS, follow-up for mortality was obtained in 463 (91%). Those lost to follow-up were older and had higher rates of tobacco use. The prevalences of CAD risk factors, prior known CAD, and MPI abnormalities were higher for the 68 patients failing to reach 85% of their target heart rate. The rate of ≥10% left-ventricular (LV) ischemia by MPI remained very low irrespective of attained heart rate (0.6% (3/463)). Six (1.2%) had an LVEF < 40%. Death occurred in 12 (2.6%) patients, one of which was classified as cardiac (0.1%/year). The other 11 deaths were related to cancer. Additionally, there were three nonfatal MIs (0.7 %) and one late revascularization (0.2%). Only one of these patients had any ischemia on MPI. No cardiac event patient had exercise ST depression or ≥5% LV ischemia.
Conclusions
Thus, patients at intermediate risk for CAD or known CAD achieving ≥10 METS have a very low prevalence of ≥10% LV ischemia and very low rates of cardiac mortality, nonfatal MI, and late revascularization, irrespective of heart rate achieved. Cardiac events did not correlate with abnormalities on the index MPI study. These results suggest that patients who attain ≥10 METS during exercise stress have an excellent prognosis over an intermediate term of follow-up, regardless of peak exercise heart rate achieved. The added value of MPI to standard exercise ECG testing in this population is questionable.
Keywords: Radionuclide imaging, exercise stress testing, risk prediction, coronary artery disease, outcomes
INTRODUCTION
Ischemic heart disease leads to a high morbidity and mortality. Exercise electrocardiographic (ECG) stress testing, although having limited sensitivity for coronary artery disease (CAD) detection, can identify those at high risk for cardiac events.1 Despite receiving an appropriate indication for the evaluation of ischemia in most patients at intermediate risk,2 the precise indications for performing myocardial perfusion imaging (MPI) in conjunction with symptom-limited exercise testing over exercise ECG testing alone is unclear. Because exercise MPI is more sensitive than exercise-induced ST depression for detection of ischemia,3 it is often combined at the outset for testing patients at an intermediate pretest likelihood of disease. On the other hand, it has been shown that patients who achieve high exercise heart rates and workloads without ischemic ST depression have an excellent prognosis.4–9
The authors10 recently reported that in more than 470 consecutive patients who achieved 85% or greater of their maximum age-predicted heart rate (MAPHR) and a workload of ≥10 metabolic equivalents (METS) on symptom-limited exercise MPI, the prevalence of significant ischemia comprising 10% or more of the left ventricle (LV) was very low (0.4%). The authors also found that no patient in this cohort who achieved ≥10 METS without ≥1.0 mm of horizontal or downsloping ST depression had significant ischemia on single-photon emission computed tomography (SPECT) imaging. The prevalence of 5% to 9% ischemia of the left ventricle (LV) was also low in such patients (0.7%). Twenty percent of these patients had known CAD, and seventy percent had chest pain as the indication for testing. These data suggested that MPI could be eliminated in patients achieving ≥10 METS on exercise testing without loss of prognostic capability.
The purpose of this report is to assess all-cause and cardiovascular mortality and the incidence of cardiac events during follow-up of these individuals achieving a high exercise workload. The authors hypothesized that these patients achieving a high exercise capacity (≥10 METS) should have very low rates of cardiac mortality and nonfatal myocardial infarction (MI). Patients who achieved ≥10 METS but less than 85% of MAPHR were also followed-up for cardiac events. If the event rate was found to be very low in these patients, as the authors observed for the prevalence of significant ischemia,10 it would lend support to the notion that an imaging agent might not need to be injected for patients achieving ≥10 METS on exercise testing. Elimination of imaging would yield high cost savings since such patients represent about one-third of all patients referred for exercise SPECT MPI over a period of 1 year.10
METHODS
Prospectively collected data from the University of Virginia Nuclear Databank (UVAND) were analyzed in a cohort of consecutive patients who underwent exercise testing and SPECT MPI through the University of Virginia Health System.
Study Cohort
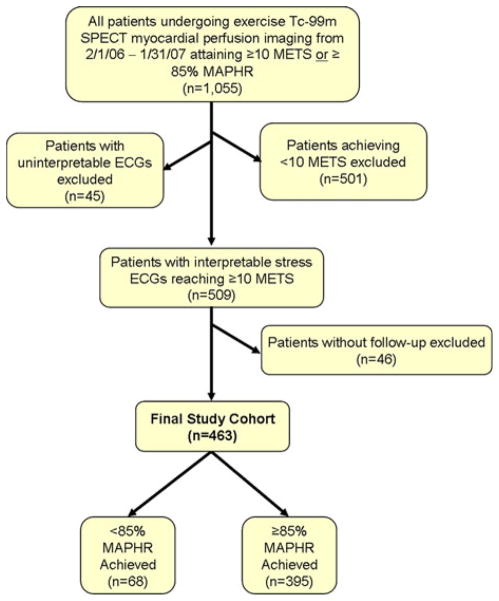
The derivation of the study cohort is provided in Figure 1 and has previously been described.10 There were 1,055 consecutive patients who underwent exercise stress 99mTc SPECT MPI at the University of Virginia Nuclear Cardiology Laboratory between February 2006 and January 2007, of whom 501 achieved <10 METS of workload and were excluded. The authors also excluded 46 patients without follow-up data and 45 patients who had an uninterpretable ECG: 5 with left bundle-branch block; 2 with a paced rhythm; and 38 with resting ST-T abnormalities that precluded analysis. The remaining 463 subjects, who reached ≥10 METS and had diagnostic ECGs and mortality data available, comprised our final study cohort.
Figure 1.
Patient flow diagram showing the derivation of the study cohort.
Clinical Information Collection and Management
Clinical information was collected from patients at the time of exercise testing and was entered into the UVAND, including demographics, comorbidities, and physical examination and baseline ECG findings. Exercise test parameters and SPECT results (volumes, perfusion, and function) were also recorded.9,11 The patients were subdivided by the achievement or failure to reach ≥85% of the MAPHR. Unfortunately, the authors did not have precise characterization of the type of chest pain experienced as part of our entry data in all patients.
Follow-up data, including all-cause and cardiac mortality and nonfatal cardiac events, were obtained by mailing a questionnaire to the 509 subjects reaching ≥10 METS of exercise capacity. Up to three phone calls were placed to questionnaire non-responders and their primary care physicians or cardiologists to collect follow-up data. For all those in whom data could not be obtained, and as a confirmation in those with events who had successful questionnaire/telephone follow-up, a careful chart review was performed by an observer blinded to the stress test results. Questionable data from the chart reviews were analyzed by an additional blinded observer. The Social Security Death Index (SSDI) was utilized to identify all-cause mortality in the 91% in whom social security numbers were available. Patients reaching or failing to reach target heart rate (≥85% of the MAPHR) were compared with respect to prevalence of events.
Protocol and follow-up questionnaire approval and waiver of informed consent were obtained from the University of Virginia Institutional Review Board.
Exercise Testing and SPECT Imaging
The methods utilized by the authors for exercise testing, SPECT imaging, and image interpretation have been well described previously and will be briefly summarized here.10 Symptom-limited exercise treadmill testing was performed according to a Bruce protocol (99% of cases). Exercise workload was defined as the total METS achieved. Ischemic ST depression was defined as ≥1 mm horizontal or down-sloping depression of the ST segment ≥80 ms after the J-point for 3 consecutive beats.
Tc-99m Sestamibi rest-stress, gated SPECT MPI was performed with standard dosages under a 1- or 2-day protocol (for a body mass index ≥ 36). The isotope was injected 1 minute prior to exercise cessation. Images were acquired with a dual-head GE Infinia camera with low-energy, high-resolution collimators using a standard 99mTc energy window and no attenuation correction.
Nuclear Image Interpretation
Experienced nuclear cardiology specialists performed visual and quantitative image analysis of the perfusion images according to a 17-segment model as previously described.11 Borderline and abnormal studies were reclassified by the consensus opinion of two readers blinded to all other clinical information. Each segment was given a score from 0 to 4, with 0 representing normal perfusion and 1–4 representing mild, moderate, severe defects, and absent tracer uptake, respectively. The semi-quantitative summed stress, rest, and summed difference scores were calculated from these segmental scores with the five apical segments each given 40% weighting so that each unit myocardial volume was equal.10 Systolic and diastolic volumes and body surface area normalized volumes were also calculated.11 The “percent myocardial ischemia,” representing the extent and severity of LV inducible ischemia, was derived by dividing the difference between summed stress and summed rest scores by the maximum possible difference.12,13
Outcomes
The primary outcome for this study was the prevalence of mortality from all-causes. Secondary endpoints included cardiac mortality, nonfatal MI, and late revascularization. Cardiac death was defined as any death with a demonstrable cardiac cause or without a clear non-cardiac cause. Nonfatal MI was designated if a patient presented with a history consistent with an acute coronary syndrome and had a troponin ≥2 times the upper limit of normal, with or without typical ischemic ECG changes. The authors considered any cardiac catheterization or coronary revascularization performed later than 4 weeks after the MPI study to be a new event and not directly related to the results of the stress test.
Statistical Analysis
Continuous variables were described as medians with 25th and 75th percentiles and were compared by t tests with Satterthwaite approximations for unequal variances. Categorical variables were given as numbers of patients with percentages and were compared with Pearson chi-square or Fisher’s exact testing. The Poisson distribution was used to identify the 95% confidence intervals of the event rates.14 The alpha level of significance was 0.05 for all analyses. All statistics were performed using SAS version 9.1.
RESULTS
Follow-Up
Follow-up data on all-cause mortality were obtained in 463 of the 509 patients (91%) with interpretable ECGs who reached ≥10 METS of exercise workload (Figure 1). The cohort without follow-up data available were younger (mean age 45.0 vs 53.7, P < .001) and were more likely to use tobacco (43.5% vs 26.4%, P = .014). Otherwise, the baseline demographics of patients lost to follow-up did not significantly differ from the overall cohort. Data on nonfatal events such as MI and late revascularization were available in 415 of these 509 patients (89.6%). The range of follow-up in the final cohort was 0.4 to 3.3 years (all subjects who did not die had at least 1 year of follow-up). The mean follow-up was 2.2 ± 0.5 (standard deviation) years.
Clinical and Stress Test Characteristics of the Study Population
The clinical characteristics of the study cohort are shown in Table 1. The patients were subdivided into those who achieved both ≥10 METS and ≥85% of their MAPHR (Group 1) and those who achieved ≥10 METS but <85% of MAPHR (Group 2). There was no difference in age or documented hyperlipidemia between the groups. However, all other characteristics measured, most importantly a history of prior CAD, were significantly more prevalent in Group 2 patients. Given the use of beta-blockers in CAD, some of these differences are likely due to the higher use of beta-blockers on the day of the test in Group 2 (13/68, 19.1% vs 22/395, 5.6%, P < .001). The higher prevalence of risk factors for CAD in those failing to reach target heart rate is consistent with findings in prior studies of chronotropic incompetence.15
Table 1.
Clinical characteristics of the study cohort dichotomized by achievement of a diagnostic heart rate (≥85% MAPHR)
| Characteristic | Entire Cohort (n = 463) | Group 1 ≥85% MAPHR (n = 395) | Group 2 <85% MAPHR (n = 68) | P value† |
|---|---|---|---|---|
| Age (median (25th, 75th)) | 53.5 (46.0, 61.0) | 54.0 (46.0, 61.0) | 52.5 (47.0, 64.5) | .636 |
| Male (%) | 71.7 | 69.6 | 82.4 | .032 |
| Hypertension (%) | 46.1 | 41.8 | 70.6 | < .001 |
| Hyperlipidemia (%) | 56.9 | 56.5 | 60.3 | .555 |
| Diabetes mellitus (%) | 12.8 | 10.9 | 23.5 | .004 |
| Tobacco use (%) | 26.4 | 23.0 | 45.6 | < .001 |
| Known CAD (%) | 22.7 | 20.0 | 38.2 | .001 |
| History of MI (%) | 14.5 | 11.9 | 29.4 | < .001 |
| Prior revascularization (%) | 19.3 | 16.5 | 35.3 | < .001 |
CAD, Coronary artery disease; MAPHR, maximum age-predicted heart rate; MI, myocardial infarction.
Values < 0.05 are considered statistically significant.
With regard to presenting symptoms, 400 of the 463 subjects (86.4%) had either symptoms of chest pain or shortness of breath (366 patients), and 105 (22.7%) had known CAD. Chest pain was classified in 111 of the subjects without known CAD, and more than half of these patients had a >45% risk of CAD by the Diamond and Forrester classification.16
Ischemic ST depression and findings on nuclear MPI stratified by achievement of target heart rate are provided in Table 2. There was no difference in the prevalence of exercise ST depression between Group 1 and Group 2 patients. End-diastolic and end-systolic volumes were significantly higher in the Group 2 patients who failed to reach target heart rate. An abnormal end-systolic volume index (≥25) was seen in 23.9% in this group versus 7.4% in the Group 2 patients who achieved ≥85% MAPHR (P < .001). Group 2 patients had 4.3- and 3.9-fold higher prevalences of ischemia and fixed perfusion defects, respectively, compared to Group 1 patients (P < .001 for both). For the entire cohort of 463 patients, 3 had ≥10% LV ischemia, 5 had between 5 and 9% LV ischemia, and 20 had < 5% LV ischemia. The difference in prevalence of ≥10% LV ischemia was not statistically significant between Groups 1 and 2, predominantly based on the very low prevalence of this variable. Group 1 patients had a 3% higher post-stress LV ejection fraction (65% vs 62%) that was statistically significant (P = .003), but most likely clinically not significant (Table 3).
Table 2.
Study cohort myocardial perfusion imaging findings by achievement of a diagnostic heart rate (≥85% MAPHR)
| Characteristic | Entire Cohort (n = 463) | Group 1 ≥85% MAPHR (n = 395) | Group 2 <85% MAPHR (n = 68) | P value† |
|---|---|---|---|---|
| Exercise ST depression (n, (%)) | 46 (10.0) | 42 (10.6) | 4 (5.9) | .226 |
| EDVI (n, (%)) | 47.0 (40.0, 55.0) | 46.0 (39.0, 54.0) | 55.0 (43.0, 66.0) | < .001 |
| ESVI (n, (%)) | 14.0 (10.0, 18.0) | 13.0 (10.0, 18.0) | 18.0 (12.0, 25.0) | .004 |
| Normal perfusion (n, (%)) | 417 (90.1) | 365 (92.4) | 52 (76.5) | < .001 |
| Any defect reversibility (n, (%)) | 28 (6.1) | 16 (4.1) | 12 (17.7) | < .001 |
| Fixed defect (n, (%)) | 37 (8.0) | 22 (5.6) | 15 (22.1) | < .001 |
| ≥10% LV ischemia (n, (%)) | 3 (0.6) | 2 (0.5) | 1 (1.5) | .360 |
| LVEF (median (25th, 75th)) | 65.0 (60.0, 69.0) | 65.0 (61.0, 69.0) | 62.0 (56.0, 67.0) | .003 |
EDVI, End-diastolic volume index; ESVI, end-systolic volume index; LV, left-ventricular; LVEF, left-ventricular ejection fraction; MAPHR, maximum age-predicted heart rate.
Values < 0.05 are considered statistically significant.
Table 3.
Prevalence of outcomes and annualized event rates in the total cohort with interpretable ECGs attaining ≥10 METS of cardiac workload
| Cardiovascular event | Prevalence (n (%)) | Annualized rate (%/year (95% CI)) |
|---|---|---|
| All-cause mortality | 11 (2.4) | 1.1 (0.5, 1.9) |
| Cardiovascular death | 1 (0.2) | 0.1 (0.0, 0.5) |
| Nonfatal MI | 3 (0.7) | 0.3 (0.1, 1.0) |
| Late revascularization | 1 (0.2) | 0.1 (0.0, 0.6) |
CI, confidence interval; ECG, electrocardiogram; METS, metabolic equivalents; MI, myocardial infarction.
Mortality
There were 12 total deaths (2.6%) during follow-up in the entire population of 463 patients referred for MPI with interpretable baseline ECGs who achieved ≥10 METS of exercise workload. The annualized all-cause mortality rate was 1.2%. Of these, 12 (84.6%) were in the group reaching ≥85% of the MAPHR. The 12 deaths included only one that was classified as a cardiac death (0.4%), yielding an annualized cardiac mortality of 0.1%/year. Actually, this death was of unknown causes but was classified as cardiac by protocol. This patient was in the group achieving ≥85% of MAPHR. All the other 11 deaths were documented as related to cancer. Thus, in this population of patients, of which 20% had known CAD, the annual cardiac mortality was very low.
Nonfatal Cardiovascular Events
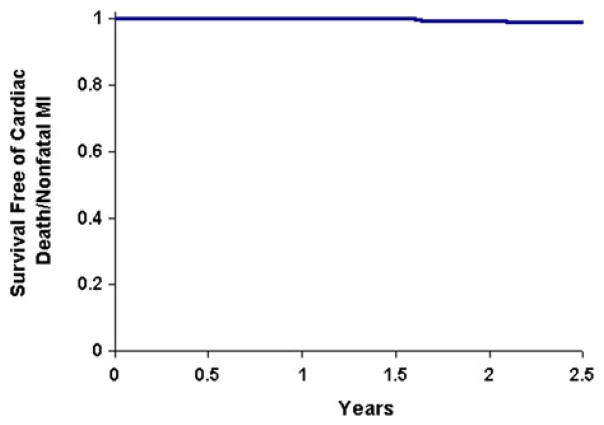
Three patients had a nonfatal MI during the follow-up period (0.7%), all of whom reached ≥85% of their MAPHR. Survival free of cardiovascular death or nonfatal MI is shown in Figure 2. There were 13 patients who had a late cardiac catheterization, all of which were performed >2 months from the original MPI study. Of these, 6 had coronary stenoses of ≥70%. Only one patient undergoing late catheterization had revascularization, which was a balloon angioplasty for instent restenosis. Nine of the 13 patients undergoing late catheterization (69.2%) reached ≥85% MAPHR. The other 4 achieved < 85% MAPHR, including the patient who underwent angioplasty.
Figure 2.
Survival free of cardiac death or nonfatal MI. The percentage of the 463 subjects remaining free of cardiac death or nonfatal MI is displayed over 2.5 years of follow-up.
Exercise ECG and Perfusion Imaging Findings in Patients With Events
We examined the original stress ECG and MPI findings in the patients who had subsequent events. Ischemic ST depression at peak exercise was not seen in any of the patients with cardiac events. No patient who died of any cause or had a cardiac event had significant LV ischemia (≥10% of the LV), and only one patient had any degree of ischemia (< 5%). This patient died from a cancer. It should be pointed out that two patients with ≥10% LV ischemia underwent early revascularization procedures which were not considered events. Thus, no patient who died, had an MI, or underwent late coronary revascularization had ≥5% myocardial ischemia on stress MPI. Moreover, none had ischemic ST depression on the exercise ECG. One of the 3 patients with ≥10% LV ischemia underwent late catheterization without revascularization.
DISCUSSION
This study shows that a consecutive group of patients referred for stress testing with MPI who achieve a workload of ≥10 METS have an excellent prognosis with an annualized cardiac mortality of 0.1% and a combined cardiac death and nonfatal MI rate of 0.4%. Furthermore, the patients with either hard or soft cardiac events were all in the group which achieved their target heart rate. None of the event patients had either >5% or >10% ischemia or were in the subset of patients who manifested exercise-induced ST segment depression. These outcomes are consistent with the very low prevalence of >10% ischemia in this population previously reported.10 The annual cardiac death or nonfatal MI rate is even lower than observed in patients with normal stress perfusion scans.17 These findings are consistent with our earlier publication showing that the prevalence of significant ischemia in patients achieving ≥10 METs was very low, whereas the ischemic burden progressively increased as the workload achieved decreased, even though ≥85% of MAPHR was achieved.
The low cardiac mortality and myocardial infarction rates in this study are consistent with previous reports in the literature.5–8 Morise et al5 reported an all-cause mortality rate of 1.5% over 2.8 years of follow-up in 1,622 male patients who achieved ≥10 METS on exercise testing. None of the patients in that study had known CAD, which is different from our study population in which 20% of patients achieving target heart rate and 38% of those who failed to reach target heart rate had known CAD. Myers et al6 reported that patients achieving a work load of ≥10 METs, even with cardiovascular disease, had a relatively low risk of death during follow-up. Each 1-MET increment in peak treadmill workload was associated with a 14% reduction in cardiac events among young subjects and 18% among those >65 years of age. After adjustment for age, the peak exercise capacity measured in METS was the strongest predictor of the risk of death in patients with or without known cardiovascular disease. Peak workload was a better predictor of mortality than the peak exercise heart rate. Goraya et al,7 reporting on the Olmstead County study, found that peak workload achieved was the only treadmill test-associated variable that was significantly related to all-cause mortality. Consistent with the study of Morise et al,5 in this study, each 1-MET increment in workload achieved was associated with a 14% reduction in cardiac events in younger patients and an 18% reduction in cardiac events in those >65 years of age. Peterson et al8 examined a large cohort of 9,191 patients referred for exercise treadmill testing and found that lower exercise capacity was associated with an increased risk of MI, unstable angina, coronary revascularization, and all-cause mortality compared with high exercise capacity.
Our findings of a good prognosis in patients achieving a high workload of ≥10 METS are consistent with the studies examining the predictive value of the Duke Treadmill Score,9 which has treadmill time as one of the three main components. Patients with a low Duke Treadmill score most often achieve high exercise workload without ST depression or inducible angina. Our study did not examine anginal chest pain on stress testing as a variable since the authors previously showed that the magnitude of inducible ischemia on MPI was similar in patients experiencing or not experiencing chest pain on symptom-limited stress testing.18
Snader et al19 reported that, in a low risk group of patients (none had prior revascularization) undergoing symptom-limited exercise MPI, the presence of thallium-201 perfusion defects was a less powerful predictor of death than functional capacity. In this study, by multivariable analysis, the strongest predictors of all-cause mortality were fair or poor functional capacity and age. Neither cardiac mortality, nonfatal MI nor late revascularization was evaluated in this study. In a study by Bhat et al,20 patients who achieved ≥10 METs even with a positive exercise ECG response had a very low prevalence of exercise echocardiographic abnormalities and a low mortality rate in follow up. This is consistent with the results of the present study, in which few events occurred in those patients with normal or near normal perfusion scans with no ST segment depression.
Kodama et al21 did a Medline search to define the relationship between cardiorespiratory fitness and coronary heart disease events. They found that better cardiovascular fitness was associated with a lower risk of all-cause mortality and coronary heart disease/cardiovascular disease (CHD/CVD) events. A 1-MET higher level of maximum aerobic capacity was associated with 13% and 15% risk reductions in all-cause mortality and CHD/CVD events, respectively. Patients with a maximum workload of 7.9 METS or more had a substantially lower rate of events compared with those attaining < 7.9 METS of exercise capacity.
Implications of the Study for Value of Myocardial Perfusion Imaging
The findings of this study, as well as those from our earlier publication, cast doubt on the value of myocardial perfusion imaging in providing additional prognostic information in patients achieving ≥10 METS on exercise stress testing, whether they reach target heart rate or not. Our earlier study reported that 473 consecutive patients achieving ≥85% of MAPHR and ≥10 METS had only a 0.4% prevalence of ≥10% LV ischemia on quantitative MPI. The prevalence of this amount of inducible ischemia was still only 2.4% in patients not achieving target heart rate but attaining ≥10 METS of workload. The prevalence of any ischemia on MPI was only 4% in patients reaching target heart rate and a high workload of ≥10 METS. When these patients were followed up for events, there was only one death classified as cardiac. What is of importance is that the patients who died, had a nonfatal MI, or underwent late revascularization all had a low risk myocardial perfusion scan and no ischemic ST depression. No patient with 5% or more LV ischemia by SPECT had a subsequent cardiac event. Thus, it appears that MPI did not provide any additional prognostic information in this patient population achieving a high exercise workload of ≥10 METS. This patient population comprised nearly one-third of all patients who underwent exercise stress MPI during the period of study enrollment. Had they not been injected with the imaging agent after achieving ≥10 METs of workload, the cost savings would have been substantial.
Further investigation of a protocol in which radio-nuclide is only injected for those reaching< 10 METS or having ischemic ST-depression would be of interest. Additional issues such as test reimbursement and the order of rest and stress imaging would need to be resolved. Moreover, a small number of patients who developed ST-depression only in the recovery period or other abnormalities would require re-stress.
Most importantly, since the authors did not formally characterize patients by CAD probability, further prospective study should be undertaken to evaluate whether our findings are similar across the range of patients with intermediate to high CAD probability, ranging from typically low-intermediate CAD probability among patients presenting with nonanginal chest pain to high CAD probability among patients presenting with typical angina.
Limitations of the Study
Some limitations of our study require mention. First of all, the authors did not have a complete follow-up in 10% of the patients. It is possible that patients lost to follow-up had a higher event rate than those for whom follow-up data were obtained. However, it should be pointed out that the clinical, electrocardiographic, and radionuclide variables were comparable in those followed-up and those who were lost to follow-up. The authors did not undertake a follow-up study of patients who achieved low exercise workloads, since prior studies have shown that these patients have more inducible ischemia and higher event rates than patients with high exercise capacity. Also, the main purpose of this study was to test the hypothesis that patients achieving an exercise workload of ≥10 METS have a very low prevalence of significant ischemia and a good prognosis. Furthermore, patients who are deemed unable to achieve ≥85% of MAPHR are better risk stratified by pharmacologic stress MPI. Our goal was to investigate the supplemental value of MPI in patients at intermediate pretest likelihood of CAD or with known CAD who then demonstrate good exercise capacity. It is in this subgroup of patients where doubt exists on the additional prognostic value of stress perfusion imaging.
Our study was not powered to determine whether a difference in mortality existed between the group achieving ≥10 METS and ≥85% of MAPHR and the smaller group of patients achieving ≥10 METS but < 85% of MAPHR. The prevalence of ischemia by SPECT was higher in the latter group. However, because the group comprised only 82 patients and the event rate was so low, no conclusion can be made regarding whether this group is at higher risk compared to the group achieving high workloads and a high heart rate. Another limitation is the rather short duration of follow-up. It is possible that more events would have occurred with longer-term follow-up. Nevertheless, the authors can conclude that short-term outcome is excellent for patients achieving ≥10 METS on treadmill testing regardless of SPECT findings. Also, because so few patients had high risk stress SPECT studies, it is unlikely that a substantial number of new events would have emerged, even with a longer follow-up of 3 to 5 years.
CONCLUSIONS
Thus, patients at intermediate risk for CAD or known CAD achieving ≥10 METS have a very low prevalence of ≥10% LV ischemia and very low rates of cardiac mortality, nonfatal MI, and late revascularization, irrespective of heart rate achieved. Cardiac events did not correlate with abnormalities on the index MPI study. These results suggest that patients who attain ≥10 METS during exercise stress have an excellent prognosis over an intermediate term of follow-up, regardless of peak exercise heart rate achieved. The added value of MPI to standard exercise ECG testing in this population is questionable.
Acknowledgments
Dr Bourque is funded by an NIH NRSA Training Grant: T32 EB003841-04.
Footnotes
The authors have indicated that they have no financial conflicts of interest.
References
- 1.Gibbons RJ, Balady GJ, Bricker JT, et al. ACC/AHA 2002 guideline update for exercise testing: Summary article. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines) J Am Coll Cardiol. 2002;40:1531–40. doi: 10.1016/s0735-1097(02)02164-2. [DOI] [PubMed] [Google Scholar]
- 2.Hendel RC, Berman DS, Di Carli MF, et al. ACCF/ASNC/ACR/ AHA/ASE/SCCT/SCMR/SNM 2009 Appropriate Use Criteria for Cardiac Radionuclide Imaging: A Report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the American Society of Nuclear Cardiology, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the Society of Cardiovascular Computed Tomography, the Society for Cardiovascular Magnetic Resonance, and the Society of Nuclear Medicine. J Am Coll Cardiol. 2009;53:2201–29. doi: 10.1016/j.jacc.2009.02.013. [DOI] [PubMed] [Google Scholar]
- 3.Klocke FJ, Baird MG, Lorell BH, et al. ACC/AHA/ASNC guidelines for the clinical use of cardiac radionuclide imaging—executive summary: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASNC Committee to Revise the 1995 Guidelines for the Clinical Use of Cardiac Radionuclide Imaging) J Am Coll Cardiol. 2003;42:1318–33. doi: 10.1016/j.jacc.2003.08.011. [DOI] [PubMed] [Google Scholar]
- 4.Balady GJ, Larson MG, Vasan RS, Leip EP, O’Donnell CJ, Levy D. Usefulness of exercise testing in the prediction of coronary disease risk among asymptomatic persons as a function of the Framingham risk score. Circulation. 2004;110:1920–5. doi: 10.1161/01.CIR.0000143226.40607.71. [DOI] [PubMed] [Google Scholar]
- 5.Morise AP, Jalisi F. Evaluation of pretest and exercise test scores to assess all-cause mortality in unselected patients presenting for exercise testing with symptoms of suspected coronary artery disease. J Am Coll Cardiol. 2003;42:842–50. doi: 10.1016/s0735-1097(03)00837-4. [DOI] [PubMed] [Google Scholar]
- 6.Myers J, Prakash M, Froelicher V, Do D, Partington S, Atwood JE. Exercise capacity and mortality among men referred for exercise testing. N Engl J Med. 2002;346:793–801. doi: 10.1056/NEJMoa011858. [DOI] [PubMed] [Google Scholar]
- 7.Goraya TY, Jacobsen SJ, Pellikka PA, et al. Prognostic value of treadmill exercise testing in elderly persons. Ann Intern Med. 2000;132:862–70. doi: 10.7326/0003-4819-132-11-200006060-00003. [DOI] [PubMed] [Google Scholar]
- 8.Peterson PN, Magid DJ, Ross C, et al. Association of exercise capacity on treadmill with future cardiac events in patients referred for exercise testing. Arch Intern Med. 2008;168:174–9. doi: 10.1001/archinternmed.2007.68. [DOI] [PubMed] [Google Scholar]
- 9.Mark DB, Shaw L, Harrell FE, Jr, et al. Prognostic value of a treadmill exercise score in outpatients with suspected coronary artery disease. N Engl J Med. 1991;325:849–53. doi: 10.1056/NEJM199109193251204. [DOI] [PubMed] [Google Scholar]
- 10.Bourque JM, Holland BH, Watson DD, Beller GA. Achieving an exercise workload of > or = 10 metabolic equivalents predicts a very low risk of inducible ischemia: Does myocardial perfusion imaging have a role? J Am Coll Cardiol. 2009;54:538–45. doi: 10.1016/j.jacc.2009.04.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Watson DD, Smith WH., II The role of quantitation in clinical nuclear cardiology: The University of Virginia approach. J Nucl Cardiol. 2007;14:466–82. doi: 10.1016/j.nuclcard.2007.06.007. [DOI] [PubMed] [Google Scholar]
- 12.Hachamovitch R, Hayes SW, Friedman JD, Cohen I, Berman DS. Comparison of the short-term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation. 2003;107:2900–7. doi: 10.1161/01.CIR.0000072790.23090.41. [DOI] [PubMed] [Google Scholar]
- 13.Hachamovitch R, Rozanski A, Hayes SW, et al. Predicting therapeutic benefit from myocardial revascularization procedures: Are measurements of both resting left ventricular ejection fraction and stress-induced myocardial ischemia necessary? J Nucl Cardiol. 2006;13:768–78. doi: 10.1016/j.nuclcard.2006.08.017. [DOI] [PubMed] [Google Scholar]
- 14.Ulm K. A simple method to calculate the confidence interval of a standardized mortality ratio (SMR) Am J Epidemiol. 1990;131:373–5. doi: 10.1093/oxfordjournals.aje.a115507. [DOI] [PubMed] [Google Scholar]
- 15.Lauer MS, Okin PM, Larson MG, Evans JC, Levy D. Impaired heart rate response to graded exercise. Prognostic implications of chronotropic incompetence in the Framingham Heart Study. Circulation. 1996;93:1520–6. doi: 10.1161/01.cir.93.8.1520. [DOI] [PubMed] [Google Scholar]
- 16.Diamond GA, Forrester JS. Analysis of probability as an aid in the clinical diagnosis of coronary-artery disease. N Engl J Med. 1979;300:1350–8. doi: 10.1056/NEJM197906143002402. [DOI] [PubMed] [Google Scholar]
- 17.Shaw LJ, Iskandrian AE. Prognostic value of gated myocardial perfusion SPECT. J Nucl Cardiol. 2004;11:171–85. doi: 10.1016/j.nuclcard.2003.12.004. [DOI] [PubMed] [Google Scholar]
- 18.Gasperetti CM, Burwell LR, Beller GA. Prevalence of and variables associated with silent myocardial ischemia on exercise thallium-201 stress testing. J Am Coll Cardiol. 1990;16:115–23. doi: 10.1016/0735-1097(90)90467-4. [DOI] [PubMed] [Google Scholar]
- 19.Snader CE, Marwick TH, Pashkow FJ, Harvey SA, Thomas JD, Lauer MS. Importance of estimated functional capacity as a predictor of all-cause mortality among patients referred for exercise thallium single-photon emission computed tomography: Report of 3,400 patients from a single center. J Am Coll Cardiol. 1997;30:641–8. doi: 10.1016/s0735-1097(97)00217-9. [DOI] [PubMed] [Google Scholar]
- 20.Bhat A, Desai A, Amsterdam EA. Usefulness of high functional capacity in patients with exercise-induced ST-depression to predict a negative result on exercise echocardiography and low prognostic risk. Am J Cardiol. 2008;101:1541–3. doi: 10.1016/j.amjcard.2008.01.039. [DOI] [PubMed] [Google Scholar]
- 21.Kodama S, Saito K, Tanaka S, et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: A meta-analysis. JAMA. 2009;301:2024–35. doi: 10.1001/jama.2009.681. [DOI] [PubMed] [Google Scholar]