Abstract
Priapism is defined as having prolonged (more than 6 h), and usually painful penile erection that occurs without a sexual desire or arousal. Only a very few priapism cases caused by ziprasidone are reported in the literature. In this case report we aimed to present a prolonged penile erection due to use of ziprasidone.
Keywords: Priapism, Ziprasidon, Side effect, Schizophrenia
INTRODUCTION
Priapism is defined as a prolonged (more than 6 h) and usually painful penile erection that occurs without sexual desire or arousal.1 Of reported drug-induced priapism cases, 50% are associated with the use of typical or atypical antipsychotic drugs2 and may be correlated with the antagonist effects of psychotropic drugs at the adrenergic alpha receptor. Among atypical antipsychotics, clozapine, olanzapine, risperidone, and quetiapine have been found to cause priapism or prolonged erection.3 Priapism is thought to be an idiosyncratic reaction as it is not related to drug dose and may be seen during any stage of treatment.4 Although it is rare, priapism can result in serious side effects, such as erectile dysfunction, that clinicians need to be aware of.5 Very few cases of priapism caused by ziprasidone have been reported in the literature. Here, a case of prolonged penile erection due to use of ziprasidone is presented.
CASE
A 43-year-old male patient was admitted to the emergency department of our hospital due to insomnia, irritability, aggression, self-talk, and complaints of non-compliance with his psychiatric medications over the previous two weeks. During his psychiatric examination, he did not make eye contact, was unwilling to communicate, and exhibited decreased self-care, poor speech content, dysphoric mood, and increased psychomotor activity. His thought content could not be assessed due to his irritability and dissimulative attitude. According to information received from his family and from clinical observations, he suffered persecution, reference, and grandeur delusions. Additionally, it was noted that there had been no use of psychostimulants other than irregular alcohol intake for five years, which had stopped two years previously, and he smoked a pack of cigarettes per day.
The patient had been followed up for nearly 20 years following a diagnosis of chronic schizophrenia, for which he had been hospitalized in a psychiatric institution 17 times. Examination of his past hospital files revealed that he had been prescribed various typical and atypical antipsychotics: haloperidol (20-30 mg/day), sulpiride (800 mg/day), pimozide (4 mg/day), clozapine (600 mg/day), risperidone (6 mg/day), olanzapine (20 mg/day), quetiapine (100-900 mg/day), chlorpromazine (200 mg/day), and amisulpride (800 mg/day). The patient did not describe any involuntary prolonged erections when questioned during his follow-ups or during his former psychiatric hospital admissions. He had been diagnosed with diabetes mellitus type 2 in 2006 and had been receiving antidiabetic treatment since that time.
After his hospitalization, the patient continued to use metformin (2000 mg/day) in conjunction with ziprasidone (40 mg/day) and, as he had gastric ulcers, ranitidine (50 mg/day). The patient's total Positive and Negative Symptom Scale (PANSS) score was 131 (positive: 27; negative: 30; general psychopathology: 72). On the seventh day of treatment, a continuous painful penile erection was observed. The patient felt uncomfortable and stated that this condition had lasted for nearly 8 h and was not associated with sexual stimulation or desire. Following urologic consultation, no medical disorder or trauma that might have caused priapism was found in the patient's history, and laboratory values [complete blood count, biochemical parameters, activated partial thromboplastin time (aPTT), and International Normalized Ratio (INR)] were within the normal range. As it was thought that the antipsychotic medications might be the cause of the prolonged painful penile erection, ziprasidone treatment was discontinued but no emergency urological intervention was undertaken. The antipsychotic treatment regimen of the patient was reorganized and continued with amisulpride (800 mg/day) and quetiapine (600 mg/day). The priapism ameliorated without surgical intervention 8 h after discontinuation of ziprasidone and did not recur during the clinical monitoring of the patient.
DISCUSSION
Priapism is observed in two different patterns: high-flow priapism, in which penile or pelvic trauma leads to a change in arterial flow, and low-flow priapism, a more commonly encountered situation, in which drugs play a major role.1
In the current case, a painful penile erection that lasted nearly 8 h was observed 7 days after the initiation of ziprasidone (80 mg/day without dose adjustment). Ziprasidone is an atypical antipsychotic drug that has a high affinity for adrenergic alpha-1 receptors. Priapism due to use of quetiapine has been reported in the literature6-10 and found to be dose-dependent and possibly idiosyncratic. In the present case, the patient had a history of quetiapine use (900 mg/day) but he reported no history of priapism. Ziprasidone was discontinued after the development of priapism, and quetiapine treatment (600 mg/day) was initiated, owing to the possibilty that the priapism had been caused by ziprasidone. The antagonist effects of antipsychotic drugs on adrenergic alpha-1 receptors are thought to be the cause of drug-induced priapism. Although priapism is encountered in all age groups, it is more often seen in the third and fourth decade of life.
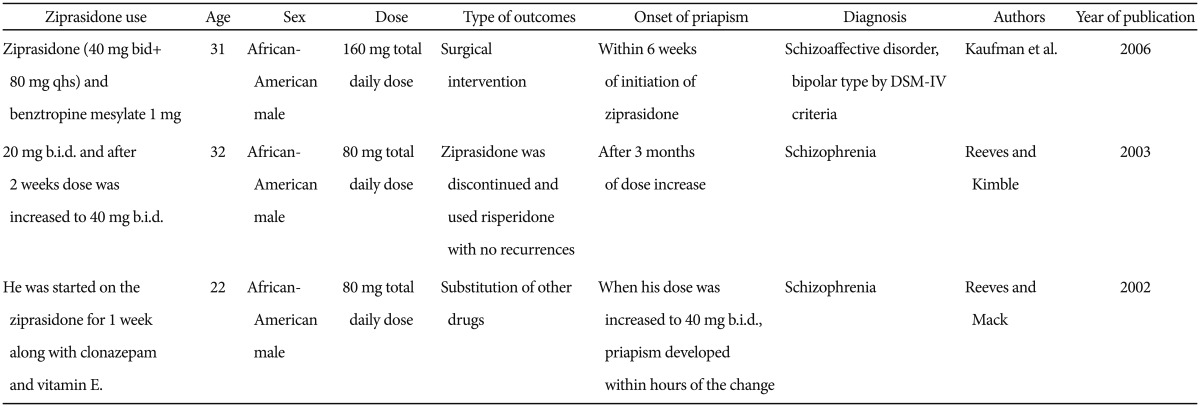
With initiation of antipsychotic treatment, priapism may occur at any stage of treatment and without a change in dose.11 The current patient had been using metformin (2000 mg/day) since 2006 subsequent to a diagnosis of type 2 diabetes. Mago and colleagues12 published a case report describing the use of aripiprazole in conjunction with metformin and atorvastatin and suggested that the presence of comorbid medical disorders can result in drug interactions, which increase the tendency of antipsychotics to induce priapism. Ziprasidone is mainly metabolized via the enzyme CYP3A4, as is quetiapine.13 In vitro studies have shown that ziprasidone can inhibit CYP3A4 and CYP2D6 enzyme action. However, in in vivo studies, its inhibition of CYP3A4 was found to be 9000-fold lower, so it is unlikely to change the metabolism of other drugs acted on by the same enzyme.14 Ranitidine also inhibits CYP3A4 but in vitro and in vivo studies have shown that it has a negligible effect on the metabolism of drugs taken concurrently.15 In addition, it has been observed that metformin taken with other drugs does not have metabolic inhibitory effects.16 Although ziprasidone has the highest affinity for adrenergic alpha-1 receptors among atypical antipsychotic drugs, a literature search reveals only three cases of priapism associated with its use (Table 1).1,17,18
Table 1.
The use of ziprasidon and reported cases of priapism from the literature
In the current patient, the use of multiple drugs that are metabolized by the same enzyme (CYP3A4), albeit with low efficacy, may have led to elevated levels of ziprasidone. This indicates the presence of an indirect drug interaction that increased the susceptibility of the patient to priapism.
In conclusion, priapism may occur at any stage of antipsychotic treatment or following an interaction with pharmacological agents used concurrently with the antipsychotics. The atypical antipsychotic ziprasidone appears to have the potential to induce priapism, not only in the situation of an overdose but also at routine doses when administered with other drugs that may increase its plasma level by inhibiting the metabolism of pharmacological agents.
References
- 1.Kaufman KR, Stern L, Mohebati A, Olsavsky A, Hwang J. Ziprasidone-induced priapism requiring surgical treatment. Eur Psychiatry. 2006;21:48–50. doi: 10.1016/j.eurpsy.2005.07.007. [DOI] [PubMed] [Google Scholar]
- 2.Brichart N, Delavierre D, Peneau M, Ibrahim H, Mallek A. Priapism associated with antipsychotic medications: a series of four patients. Prog Urol. 2008;18:669–673. doi: 10.1016/j.purol.2008.04.010. [DOI] [PubMed] [Google Scholar]
- 3.Kirshner A, Davis RR. Priapism associated with the switch from oral to injectable risperidone. J Clin Psychopharmacol. 2006;26:626–628. doi: 10.1097/01.jcp.0000239792.29449.3c. [DOI] [PubMed] [Google Scholar]
- 4.Sood S, James W, Bailon MJ. Priapism associated with atypical antipsychotic medications: a review. Int Clin Psychopharmacol. 2008;23:9–17. doi: 10.1097/YIC.0b013e3282f1c1ef. [DOI] [PubMed] [Google Scholar]
- 5.Andersohn F, Schmedt N, Weinmann S, Willich SN, Garbe E. Priapism associated with antipsychotics: role of alpha1 adrenoceptor affinity. J Clin Psychopharmacol. 2010;30:68–71. doi: 10.1097/JCP.0b013e3181c8273d. [DOI] [PubMed] [Google Scholar]
- 6.Davol P, Rukstalis D. Priapism associated with routine use of quetiapine: case report and review of the literature. Urology. 2005;66:880. doi: 10.1016/j.urology.2005.03.077. [DOI] [PubMed] [Google Scholar]
- 7.Harrison G, Dilley JW, Loeb L, Nelson K. Priapism and quetiapine in an HIV-positive male. J Clin Psychopharmacol. 2006;26:100–101. doi: 10.1097/01.jcp.0000196115.01001.04. [DOI] [PubMed] [Google Scholar]
- 8.Tsai AC. A case of recurrent priapism in the context of quetiapine use, discontinuation, and rechallenge. J Clin Psychopharmacol. 2011;31:235–236. doi: 10.1097/JCP.0b013e3182112b78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.du Toit RM, Millson RC, Heaton JP, Adams MA. Priapism. Can J Psychiatry. 2004;49:868–869. [PubMed] [Google Scholar]
- 10.Torun F, Yılmaz E, Gümüş E. Priapism due to a single dose of quetiapine: a case report. Turk Psikiyatri Derg. 2011;22:195–199. [PubMed] [Google Scholar]
- 11.Sharma A, Fleisher MH. Risperidone-induced priapism: a case report. Prim Care Companion J Clin Psychiatry. 2009;11:174–175. doi: 10.4088/PCC.08l00666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mago R, Anolik R, Johnson RA, Kunkel EJ. Recurrent priapism associated with use of aripiprazole. J Clin Psychiatry. 2006;67:1471–1472. [PubMed] [Google Scholar]
- 13.Prior TI, Baker GB. Interactions between the cytochrome P450 system and the second-generation antipsychotics. J Psychiatry Neurosci. 2003;28:99–112. [PMC free article] [PubMed] [Google Scholar]
- 14.Prakash C, Kamel A, Cui D, Whalen RD, Miceli JJ, Tweedie D. Identification of the major human liver cytochrome P450 isoform(s) responsible for the formation of the primary metabolites of ziprasidone and prediction of possible drug interactions. Br J Clin Pharmacol. 2000;49(Suppl 1):35S–42S. doi: 10.1046/j.1365-2125.2000.00151.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rendić S. Drug interactions of H2-receptor antagonists involving cytochrome P450 (CYPs) enzymes: from the laboratory to the clinic. Croat Med J. 1999;40:357–367. [PubMed] [Google Scholar]
- 16.Scheen AJ. Drug interactions of clinical importance with antihyperglycaemic agents: an update. Drug Saf. 2005;28:601–631. doi: 10.2165/00002018-200528070-00004. [DOI] [PubMed] [Google Scholar]
- 17.Reeves RR, Kimble R. Prolonged erections associated with ziprasidone treatment: a case report. J Clin Psychiatry. 2003;64:97–98. doi: 10.4088/jcp.v64n0117e. [DOI] [PubMed] [Google Scholar]
- 18.Reeves RR, Mack JE. Priapism associated with two atypical antipsychotic agents. Pharmacotherapy. 2002;22:1070–1073. doi: 10.1592/phco.22.12.1070.33613. [DOI] [PubMed] [Google Scholar]


