Smoking imposes a huge economic burden on society—currently up to 15% of total healthcare costs in developed countries. Smoking cessation can save years of life, at a very low cost compared with alternative interventions. This chapter reviews some of the economic aspects of smoking cessation.
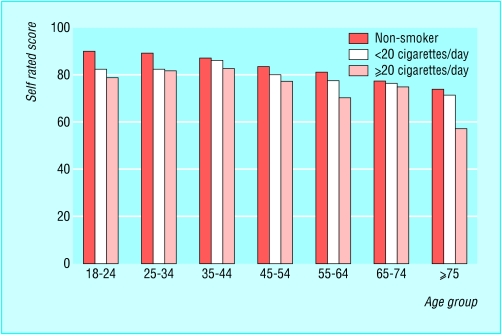
Figure 1.
Self rated health status (100 = best imaginable health state), by age and smoking status. Data from Kind et al. UK population norms for EQ-5D. York: Centre for Health Economics (Discussion paper 172)
Who benefits from cessation?
The most obvious benefits of smoking cessation are improvements in life expectancy and prevention of disease. However, cessation also improves individuals' quality of life as smokers tend to have a lower self reported health status than non-smokers, and this improves after stopping smoking.
Table 1.
Benefits of smoking cessation
| Smokers and their families |
| • Improved quality and quantity of life for those stopping smoking |
| • Improved quality and quantity of life for those living with smokers through a reduction in the harm from passive smoking |
| Society |
| • Lower healthcare expenditure on treatment of smoking induced disease |
| • Less workplace absenteeism due to smoking related disease |
| • Less harm from passive smoking in public places |
| • Reduction in costs related to cleaning up after smokers (cigarette ends, ash, etc and damage from these to floors and furnishings) |
There are also wider economic benefits to individuals and society, arising from reductions in the effects of passive smoking in non-smokers and savings to the health service and the employer. These wider benefits are often omitted from economic evaluations of cessation interventions, which consequently tend to underestimate the true value for money afforded by such programmes.
Economic burden of smoking
Many estimates have been made of the economic cost of smoking in terms of health resources. For the United States they typically range from about 0.6% to 0.85% of gross domestic product. In absolute terms, the US public health service estimates a total cost of $50bn (£29bn; €42bn) a year for the treatment of smoking related diseases, in addition to an annual $47bn in lost earnings and productivity. Estimated total costs in Australia and Canada, as a proportion of their gross domestic product, are 0.4% and 0.56% respectively. In the United Kingdom, the treatment of smoking related disease has been estimated to cost the NHS £1.4bn-£1.5bn a year (about 0.16% of the gross domestic product)—including £127m to treat lung cancer alone.
When expressed as a percentage of gross domestic product, the economic burden of smoking seems to be rising. In reality, however, the burden may not be increasing, but instead, as more diseases are known to be attributable to smoking, the burden attributed to smoking increases. Earlier estimates may simply have underestimated the true cost.
Passive smoking
In the United States, passive smoking has been estimated to be responsible for 19% of total expenditure on childhood respiratory conditions, and maternal smoking has been shown to increase healthcare expenditure by $120 a year for children under age 5 years and $175 for children under age 2 years.
Figure 2.
In Puerto Rico, China (above), and Venezuela, the cost of smoking has been estimated as 0.3%-0.43% of the gross domestic product
In the United Kingdom an estimated £410m a year is spent treating childhood illness related to passive smoking; in adults, passive smoking accounts for at least 1000 deaths in non-smokers, at an estimated cost of about £12.8m a year at 2002 prices.
Passive smoking causes illness and premature loss of life, at all ages from the prenatal period to late adult life
Cost of absenteeism
Absenteeism arising from smoking related disease is also a major cause of lost productivity, a cost incurred by employers. An annual estimated 34 million days are lost in England and Wales through sickness absence resulting from smoking related illness, and in Scotland the cost of this productivity loss is about £400m.
Table 2.
Cost effectiveness estimates for healthcare providers
|
Costs per life year saved (£) |
||
|---|---|---|
| Type of intervention | Undiscounted | Discounted |
| Face to face | ||
| Brief advice |
159 |
248 |
| Brief advice plus self help |
195 |
303 |
| Brief advice plus self help plus NRT |
524 |
815 |
| Brief advice plus self help plus NRT | 658 | 1022 |
| plus specialist cessation service |
||
| Community | ||
| “Quit and win” programme: |
||
| Medium intensity |
634 |
986 |
| “No smoking” day |
26 |
40 |
| Broader community health | 192 | 295 |
| promotion interventions (medium intensity) | ||
NRT = nicotine replacement therapy. Data from Parrott et al, 1998 (see Further Reading box), revised to reflect 2001-2 prices.
Cost effectiveness of cessation programmes
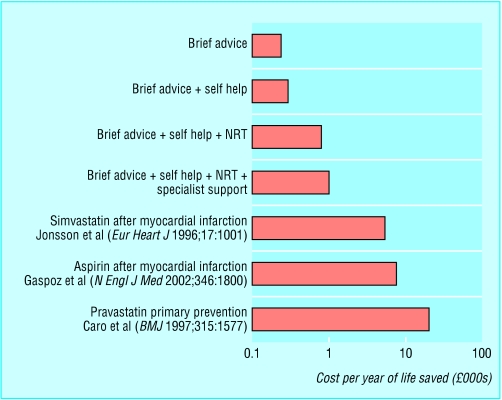
Clear evidence exists that smoking cessation interventions are effective. However, to show value for money, the costs as well as the effectiveness of such programmes have to be examined. The overwhelming evidence is that face to face cessation interventions provide excellent value for money compared with the great majority of other medical interventions.
Several complex factors influence cost effectiveness. For example, although a cessation programme tends to be more effective as its intensity increases, increased intensity is associated with increased costs, therefore increasing both sides of the cost effectiveness ratio. This was illustrated in a study by Parrott et al (1998) of the range of intensities of smoking cessation interventions in the United Kingdom. The researchers examined these interventions using local cost data and life years saved as predicted from the PREVENT simulation model. They looked at four interventions: a basic intervention of three minutes of opportunistic brief advice; brief advice plus self help material; brief advice plus self help material and nicotine replacement products; and brief advice plus self help material, nicotine replacement products, and a recommendation to attend a smoking cessation clinic. The most cost effective intervention was the brief advice alone (cost £159 per life year saved, £248 when discounted at 6%), although the most intensive clinical interventions still represent good value for money at £1002 per life year saved when discounted at 6%.
The cost effectiveness of putting the US Agency for Healthcare Research and Quality's clinical guidelines on smoking cessation into practice has also been estimated, for combined interventions based on smokers' preferences for different types of the five basic recommended interventions. The cost of implementation was estimated at $6.3bn in the first year, as a result of which society would gain 1.7 million new quitters at an average cost of $3779 per quitter, $2587 per life year saved, and $1915 per quality adjusted life year (QALY). In this study the most intensive interventions were calculated to be more cost effective than the briefer therapies.
Care should be taken when extrapolating the results of these evaluations, as cost effectiveness estimates are likely to be time and country specific and highly dependent on the healthcare system in question. In a system of fee for service, as in the United States, monetary rewards may be necessary to encourage provision. On the other hand, if patients who stop smoking place a reduced burden on the primary care budget in future years, the incentives to provide such services may be inherent in the system.
Figure 3.
Cost effectiveness of smoking cessation interventions compared with that of routine strategies for preventing myocardial infarction
Pharmacological interventions
The National Institute for Clinical Excellence (NICE) has recently estimated the cost effectiveness of using nicotine replacement therapy (NRT) or bupropion therapy. These estimates projected life years saved over a shorter period than the PREVENT model and hence produced generally higher figures: £1000-£2400 per life year saved for advice and NRT, £645-£1500 for advice plus bupropion, and £890-£1970 for advice, nicotine replacement, and bupropion. When QALYs are used, the ranges are £741-£1780, £473-£1100, and £660-£1460 respectively. These costs again compare favourably with a range of other healthcare interventions. Bupropion does seem more cost effective than NRT, although the evidence base for the effectiveness of bupropion is much less extensive than for NRT, and results should therefore be treated with caution.
Smoking related fires cause about £151m of damage each year in England and Wales
Discounting is a method of adjusting for the fact that individuals prefer to incur costs in later periods and enjoy benefits in the current period. Applying a discount rate transforms future values into current values, taking this preference into account
The National Institute for Clinical Excellence is part of the NHS in England and Wales; it issues guidance on current “best practice”
The cost effectiveness of bupropion has been investigated in Spain with a decision model (Musin et al, eighth meeting of the Society for Research on Nicotine and Tobacco, Savannah, 2002). The model presents results in an incremental analysis over and above opportunistic advice in primary care. The findings show that if all motivated smokers in Spain were to use the therapy, over a 20 year period 44 235 smoking related deaths would be averted at a saving to the healthcare system of €1.25bn. In the United States, studies have predicted savings of between $8.8m and $14m over 20 years when bupropion is added to an insurance plan. In a UK study, Stapleton et al (1999) used data from a randomised placebo controlled trial of nicotine patches and a survey of resource use to show that if general practitioners were allowed to prescribe transdermal nicotine patches on the NHS for 12 weeks, the cost per life year saved would be £398 for people aged under 35, £345 for those aged 35-44, £432 for those aged 45-54, and £785 for those aged 55-65. Since Stapleton's study was published, NRT has been made available in Britain through NHS prescription. However, studies have tended to exclude potential side effects of bupropion and are again based on a more limited effectiveness database then the evidence for the effectiveness of NRT products.
Table 3.
Comparative costs of other common healthcare treatments (analysis of guidance of the National Institute for Clinical Excellence)
|
Incremental cost (£) |
||
|---|---|---|
| Intervention | Per quality adjusted life year | Per life year gained |
| Zanamivir in managing influenza |
9300-31 500 |
|
| Taxanes for ovarian cancer |
6500-10 000 |
|
| Taxanes for breast cancer |
7000-24 000 |
|
| Implantable cardioverter defibrillators for arrhythmias |
26 000-31 000 |
|
| Glycoprotein IIb/IIIa inhibitors for acute coronary syndromes |
7000-12 000 |
|
| Methylphenidate for attention-deficit/hyperactivity disorder in children |
10 000-15 000 |
|
| Tribavirin and interferon alfa for hepatitis C: | ||
| First six months' treatment |
3000-7000 |
|
| Second six months' treatment |
5000-36 000 |
|
| Laparoscopic surgery for inguinal hernias |
50 000 |
|
| Riluzole for motor neurone disease |
34 000-43 000 |
|
| Orlistat for obesity in adults | 20 000-30 000 | |
Adapted from Raftery (BMJ 2001;323: 1300-3).
The means by which the provision is financed is a crucial determinant of the effectiveness of smoking cessation products. Evidence shows that smokers are more likely to take up smoking cessation interventions if they are provided by their insurance scheme or health service than if they have to pay for them themselves. In the United Kingdom, NHS provision can reduce costs through bulk buying and discounts from pharmaceutical manufacturers. The price for a packet of seven 15 mg Nicorette patches, for example, costs £15.99 through retail outlets, compared with an NHS purchase price of only £9.07, a reduction of about 43%. It is also clear that decreases in the price of NRT products and increases in the price of cigarettes would lead to substantial increases in per capita sales of NRT products.
Table 4.
Key points
| • Savings to the healthcare system, a reduction in the harm caused by passive smoking, and savings to employers are all relevant in evaluations of cessation interventions |
| • The economic cost of smoking in the United States may be as high as 1.15% of gross domestic product in terms of healthcare costs alone |
| • The estimated cost to the NHS is £1.4bn-£1.5bn |
| • Cessation interventions offer excellent value for money when compared with some other healthcare interventions |
| • Some studies have quantified outcomes in life years saved, not allowing for changes in quality of life, thereby underestimating the cost effectiveness of smoking cessation by almost half |
The photograph of the Marlboro advertisement in China is published with permission from Mark Henley/Panos.
Steve Parrott is a research fellow at the Centre for Health Economics and Christine Godfrey is professor at the Department of Health Sciences at the University of York. The ABC of smoking cessation is edited by John Britton, professor of epidemiology at the University of Nottingham in the division of epidemiology and public health at City Hospital, Nottingham. The series will be published as a book in the late spring.
Competing interests: See first article in this series (24 January 2004) for the series editor's competing interests.
References
- • Action on Smoking and Heath. Smoking and disease. Basic facts No 2. London: ASH, 2002. www.ash.org.uk (accessed 15 Dec 2003).
- • Cromwell J, Bartosch WJ, Fiore MC, Hasselblad V, Baker T. Cost-effectiveness of the clinical practice recommendations in the AHCPR guideline for smoking cessation. JAMA 1997;278: 1759-66. [PubMed] [Google Scholar]
- • Nielsen K, Fiore MC. Cost-benefit analysis of sustained-release bupropion, nicotine patch, or both for smoking cessation. Prev Med 2000;30: 209-16. [DOI] [PubMed] [Google Scholar]
- • Parrott S, Godfrey C, Raw M, West R, McNeill, A. Guidance for commissioners on the cost effectiveness of smoking cessation interventions. Thorax 1998;53(suppl 5, part 2): S1-38. [PMC free article] [PubMed] [Google Scholar]
- • Stapleton JA, Lowin A, Russell MAH. Prescription of transdermal nicotine patches for smoking cessation in general practice: evaluation of cost-effectiveness. Lancet 1999;354: 210-5. [DOI] [PubMed] [Google Scholar]