Short abstract
Support for dealing with ethical issues in clinical practice should be an integral part of patient care
Clinical practice raises a wide variety of ethical issues that can be difficult for individual doctors to resolve. Some NHS trusts have established clinical ethics committees to provide ethical support. These committees had largely worked alone until a meeting of committee representatives in January 2001 led to the development of the UK Clinical Ethics Network. The principal aims of the network are to promote the development of clinical ethics support in the United Kingdom, to encourage a high level of ethical debate in clinical practice, and to facilitate sharing of best practice between clinical ethics committees (box 1).1 We consider the emergence of clinical ethics support in the context of similar development in other countries.
What is clinical ethics support?
Clinical ethics support can be described as the provision of support and advice to health professionals and patients on ethical issues arising from clinical practice or patient care. The support can take different forms, but in the United Kingdom the most common model is a committee or group sitting within an NHS trust, usually an acute trust. These committees are multidisciplinary and include lay members. Issues are referred to the committee by clinicians and managers, and some committees are now being approached by local general practitioners. Few committees include patients or their families directly in committee discussions.
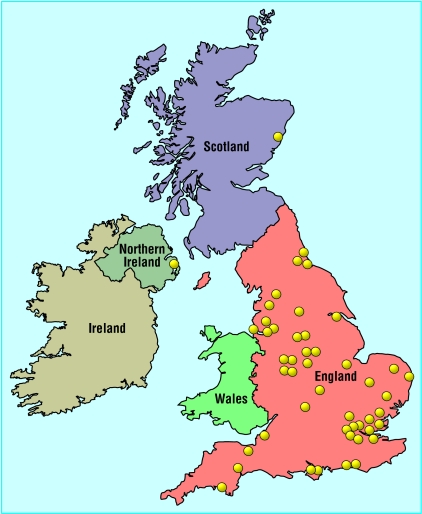
The number of trusts with clinical ethics committees is increasing. In 2001 the Nuffield Trust published a survey of all NHS trusts that identified 20 clinical ethics committees.2 A questionnaire survey conducted by the UK Clinical Ethics Network early in 2003 showed that 60 of the 315 acute NHS trusts had a clinical ethics committee (fig).3 We are unaware of any committees in primary care trusts, although two regional committees cover acute and primary care.
Figure 1.
Distribution of clinical ethics committees in United Kingdom
Box 1: Objectives of UK Clinical Ethics Network
To offer support and advice to developing and established clinical ethics groups
To provide networking facilities including a network newsletter, electronic mailing, and a network website
To facilitate training for members of clinical ethics groups
To support regional initiatives
To organise an annual conference
To produce a database of useful and relevant information for clinical ethics groups
To establish links with clinical ethics groups internationally
Functions of clinical ethics committees
The work of clinical ethics committees falls into three broad areas: providing ethics input into trust policy and guidelines around patient care, facilitating ethics education of health professionals within the trust, and giving advice to clinicians on individual cases (box 2).2 The degree to which the committees engage in each of the functions varies, but there are examples of innovative work in all three areas. For example, some committees are involving patients in developing policies on cardiopulmonary resuscitation, using role play to help clinicians explore ethical dilemmas arising in their work, and developing a system of on-call support for case consultation. As committees become established and recognised, the scope of their work increases and they get more requests for advice from trust staff.
Comparison with other countries
The development of clinical ethics committee in the United Kingdom was largely clinician led. The committees arose because clinicians were identifying difficult issues on which they felt that they needed ethics support and advice.2,4,5 Some countries have had a more top down approach, with committees (often called institutional or hospital ethics committees) forming in response to government recommendation or requirements of regulatory authorities.6 Many hospitals in North America also have ethics consultants, who provide individual support to clinicians, patients, and their families.7,8 Clinical ethics support is less widespread in continental Europe. However, all major hospitals in Norway are now required to have an ethics committee,9 and institutional ethics committees have been a feature of hospitals and nursing homes in the Netherlands for many years.10
Does ethics support make a difference?
It is difficult to evaluate ethics support using a traditional outcomes based model,11 although some US studies have used this approach. A recent study of ethics input in an intensive care unit showed positive outcomes in terms of a reduction in time spent on ventilators among patients who eventually died and in satisfaction of patients' families with the process of care.12
Although measuring specific outcomes of ethics support can be helpful, it ignores other dimensions of ethics support. An equally important aspect is the provision of an explicit and transparent process for engaging with the ethical dimension of clinical decision making. A model of ethics support that facilitates and informs a shared understanding of difficult ethical issues can support and reassure both clinicians and patients, without presupposing that there is an ethically correct outcome. Thus, a principal value of ethics support may lie in its contribution to the process of ethical decision making.
UK Clinical Ethics Network
The UK Clinical Ethics Network is now an important source of information and support for clinical ethics committees and for NHS trusts that are considering providing ethics support for their staff. The network provides a regular newsletter, an annual conference, and educational workshops, and facilitates sharing of information and experience between committees.
Box 2: Issues considered by clinical ethics committees
Withholding or withdrawing treatment
Do not resuscitate orders
Advance directives
Consent
Capacity
Refusal of treatment
Confidentiality
Genetic testing
Assisted reproduction
Issues around intensive care
Issues in emergency medicine
Summary points
About a fifth of NHS acute trusts have clinical ethics committees and their numbers are increasing
The aim of committees is to facilitate ethical decision making by doctors and hospital policy makers
A national clinical ethics network has been formed to facilitate and coordinate high quality ethics support
The network aims to promote good clinical ethics support throughout the United Kingdom
The network has also recently launched a website. The site provides contact details for all clinical ethics committees known to the network, ethical and legal discussion, hypothetical cases, and links to national guidelines on ethical issues (www.ethics-network.org.uk). The aim is to provide relevant information that is easily accessible for members, clinicians, and patients. Since its launch, the website has had an average of 105 hits a week, of which 62% are returning visitors. The most common search terms are consent and refusal of treatment.
Future development
Clinical ethics support is now an established feature of many NHS trusts. It has the potential to become a valuable component of high quality health care, but for this to happen it will require support from trust boards, clinicians, and the medical ethics community. The increasing number of clinical ethics committees, and the increasing workload of established committees, suggests that health professionals in the United Kingdom are becoming more aware of the need to openly engage with the difficult ethical issues arising in their work and that ethics committees are seen as a valuable part of this process.
Contributors and sources: AS is a clinical research fellow in the department of public health and primary care, University of Oxford and a member of Oxford Radcliffe Hospitals NHS Trust clinical ethics committee. She conducted the orginal survey of UK clinical ethics support in 2000. CJ teaches medical law at Kingston University and is a member of St Mary's Hospital clinical ethics committee. She is editor of the network's newsletter and is responsible for the academic content of the website. JG is responsible for technical development of the website and for organising conferences and workshops. TH is professor of medical ethics and has been a member of the Oxford Radcliffe NHS Trust clinical ethics committee since it was first established in 1995.
Funding: The clinical ethics network project is supported by a grant from the Department of Health to the Ethox Foundation.
Competing interests: All authors are closely involved in the development of the UK Clinical Ethics Network.
References
- 1.UK Clinical Ethics Network. About the network. www.ethics-network.org.uk/who.htm (accessed 6 Feb 2004).
- 2.Slowther A, Bunch C, Woolnough B, Hope T. Clinical ethics support in the UK: a review of the current position and likely development. London: Nuffield Trust, 2001.
- 3.UK Clinical Ethics Network. What are clinical ethics committees? www.ethics-network.org.uk/what.htm (accessed 6 Feb 2004).
- 4.Larcher V, Lask B, McCarthy J. Paediatrics at the cutting edge: do we need ethics committees? J Med Ethics 1997;23: 245-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Slowther A, Underwood M. Is there a need for a clinical ethics support service in the UK? J Med Ethics 1998;24: 207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Joint Commission on Accreditation of Healthcare Organizations. Comprehensive accreditation manual for hospitals, the official handbook. Oakbrook Terrace IL: JCAHO, 1996: R1. [PubMed]
- 7.Ehleben CM, Childs BH, Saltzman SL. What is it exactly that you do? A “snapshot” of an ethicist at work. HEC Forum 1998;10(1): 71-4. [DOI] [PubMed] [Google Scholar]
- 8.La Puma J, Toulmin SE. Ethics consultants and ethics committees. Arch Intern Med 1989;149: 1109-12. [PubMed] [Google Scholar]
- 9.Ruyter KW. Ethics committees: the national situation in Norway. In: Lebeer G, Moulin M, eds. Ethical function in hospital ethics committees: Biomed 2 working papers. Brussels: Brussels University Library, 2000: 91-105.
- 10.Van der Kloot Meijburg H. Different profiles for the institutional ethics committees in the Netherlands. HEC Forum 1994;6: 139-57. [DOI] [PubMed] [Google Scholar]
- 11.Fox E, Arnold RM. Evaluating outcomes in ethics consultation research. J Clin Ethics 1996;7: 127-38. [PubMed] [Google Scholar]
- 12.Schneiderman LJ, Gilmer T, Teetzel HD, Duggan DO, Blustein J, Cranford R, et al. Effect of ethics consultations on non-beneficial life-sustaining treatments in the intensive care setting: a randomised controlled trial. JAMA 2003;290: 1166-72. [DOI] [PubMed] [Google Scholar]