Abstract
Background.
Multimorbidity is the co-occurrence of long-term conditions. Obesity is associated with an increased risk of long-term conditions including type 2 diabetes and depression.
Objective.
To quantify the association between body mass index (BMI) category and multimorbidity in a large cohort registered in primary care.
Methods.
The sample comprised primary care electronic health records of adults aged ≥30 years, sampled from the Clinical Practice Research Datalink between 2005 and 2011. Multimorbidity was defined as the co-occurrence of ≥2 of 11 conditions affecting seven organ systems. Age- and sex-standardized prevalence of multimorbidity was estimated by BMI category. Adjusted odds ratios associating BMI with additional morbidity were estimated adjusting for socioeconomic deprivation and smoking.
Results.
The sample comprised 300 006 adults. After excluding participants with BMI never recorded, data were analysed for 223 089 (74%) contributing 1 374 109 person–years. In normal weight men, the standardized prevalence of multimorbidity was 23%, rising to 27% in overweight, 33% in category I obesity, 38% in category II and 44% in category III obesity. In women, the corresponding values were 28%, 34%, 41%, 45% and 51%. In category III obesity, the adjusted odds, relative to normal BMI, were 2.24 (2.13–2.36) for a first condition; 2.63 (2.51–2.76) for a second condition and 3.09 (2.92–3.28) for three or more conditions. In a cross-sectional analysis, 32% of multimorbidity was attributable to overweight and obesity.
Conclusions.
Multiple morbidity is highly associated with increasing BMI category and obesity, highlighting the potential for targeted primary and secondary prevention interventions in primary care.
Keywords. Cardiovascular diseases, comorbidity, diabetes mellitus, family practice, obesity, primary health care.
Introduction
Multimorbidity or the co-occurrence of multiple diseases, is frequent in primary care populations. Estimates for the frequency of multimorbidity depend on the definition used, with no consensus on the conditions that should be included (1). In primary care populations, studies have suggested that up to a quarter of all patients may have two or more coexisting conditions, (2,3) with the prevalence of multimorbidity increasing with age. Multimorbidity is associated with younger age at death, impairments of physical and social functioning (4) and mental health problems (5). Patients with multimorbidity are heavier users of primary care services and may experience lower quality of care (6).
The prevalence of overweight and obesity have been increasing in Europe and North America, although the documentation of body mass index (BMI) and obesity are generally poor in primary care (7,8). Obesity is associated with increased frequency of many long-term conditions that are of importance in primary and secondary care, including type II diabetes, cardiovascular diseases and musculoskeletal problems (9). Despite the well-documented impact of obesity on morbidity and mortality, (9,10) obesity has been seldom considered in the context of multimorbidity (11). The association of obesity with multimorbidity merits evaluation. The aim of the study was to quantify the association between BMI and multimorbidity in a primary care population. An understanding of this association may offer insight into the contribution of obesity to the burden of multimorbidity in primary care and the potential for prevention of multimorbidity.
Methods
Data source
The Clinical Practice Research Datalink (CPRD), formerly known as the General Practice Research Database, is a large database holding the electronic health records of ~7% of UK family practices. The CPRD comprises valid and representative longitudinal data for clinical, referral, test and prescribing records for registered patients (www.cprd.com).
Data selection and definitions
A random sample of men and women aged ≥30 years was selected without replacement for the years 2005–11 with a total of 300 006 patients included. For each participant, the start of the record was defined as the later of the date of registration at the practice or the date on which the practice data began contributing research standard data to CPRD. The end of the record was the earliest of the death date, the end of the patient’s registration at the practice or the last date of data collection from the practice. All patients contributed at least 12 months follow-up to the study. For each participant, person–time was divided into periods of one calendar year from 2005 to 2011, and these periods of person–time then formed the units for analysis. Each year of person–time was allocated into the following BMI categories for analysis: underweight, <18.5kg/m2; normal weight, 18.5–24.9kg/m2; overweight, 25.0–29.9kg/m2; obesity category I, 30.0–34.9kg/m2; obesity category II, 35.0–39.9kg/m2 and obesity category III, >40.0kg/m2. As BMI values were not recorded in every year, we used the methods of last observation carried forwards (LOCF), and next observation carried backwards, to impute BMI values for up to 3 years either side of recorded BMI values. Where more than one BMI value was informative, the nearest in time, or the value carried forward, took precedence. Participants who did not have a BMI record between 2005 and 2011, after imputing missing values, were excluded from the analysis. Missing data values for smoking were imputed using the LOCF method.
Multimorbidity was defined as the presence of two or more concurrent conditions out of 11 conditions, or groups of conditions, affecting seven functional systems of the body. The conditions were coronary heart disease, stroke, asthma, sleep apnoea, type 2 diabetes, all neoplasms, gallbladder, back pain, osteoarthritis, other joint problems and depression. These conditions represented a wide range of common disorders that may be associated with obesity. Risk factors such as hypertension and dyslipidaemia were not included. In the UK, primary care records are coded using READ codes and each condition was defined using a set of READ codes and, where appropriate, evidence of prescribing of relevant drugs such as oral hypoglycaemic drugs for diabetes. Further details on the codes used to identify the conditions are available from the authors.
Statistical analysis
Prevalence was employed as the measure of disease burden because of the long-term nature of the conditions studied. Prevalence estimates were obtained by 10-year age group and sex; age- and sex-standardized values were estimated using the European Standard Population for reference. The population attributable fraction (PAF) was estimated to quantify the contribution of overweight and obesity to the burden of disease in the population (12).
A generalized ordered logistic regression model was used to evaluate the relationship between BMI category and the number of conditions present in each individual. Observations were each individual’s person–time divided into person–years. BMI category was the principal predictor while the outcome was the number of diseases present. The number of conditions was grouped into the categories 0, 1, 2 and 3 or more. Analyses were adjusted for gender, age group, smoking status and socioeconomic deprivation. Initial analyses showed that the more restrictive assumptions of the ordinal logistic model were not met. A generalized ordered logistic model was therefore employed, which allowed the estimated odds ratios to be held constant between contrasts (from zero to one or more conditions, from one or less to two or more and from two or less to three or more conditions) for some variables, and to vary for others as appropriate. An age-squared term was included in the model in the anticipation that the relationship between age and increasing morbidities might be non-linear, and clustering within patients was accounted for. All analyses for this study were conducted using STATA 12.
Results
The initial sample included 300 006 participants. After excluding participants with no BMI data for the years 2005–11, 223 089 (74%) patients remained, contributing 1 374 109 person–years of observation to the analysis. BMI was recorded in year for 49% of person–time after imputation; individuals with missing BMI values comprised 13% of male, and 10% of female person–time; BMI values imputed by carrying values either forward or backward for up to 3 years accounted for the remainder. Men accounted for 634 107 person–years and women, 740 002 person–years; 53% of person–time for men, and 50% of person–time for women, was in age groups over 55 years. Current smoking was reported in 15% of men and 12% of women, with ex-smokers making up 38% and 27% of male and female person–time, respectively. The largest proportion of person–time in men was in the overweight category at 38%, whereas in women it was normal weight at 34%. Fewer than 2% of male and female person–time was in the underweight category. In men, obesity category I accounted for 17% of person–time, obesity category II for 5% and obesity category III for 2%; in women, the figures were 15%, 6% and 4%, respectively.
Table 1 presents data for the distribution of number of conditions present in each participant by BMI category for men and women. The overall prevalence of multimorbidity, defined as two or more morbidities, was 27.1% in men and 33.3% in women. The prevalence of multimorbidity increased with BMI category in both genders. The prevalence of multimorbidity in normal weight men was 23.1%, increasing to 27.2% in overweight, 32.7% in obesity category I, 38.0% in obesity category II and 43.8% in obesity category III. In women, the prevalence of multimorbidity in normal weight patients was 27.6%, rising to 34.2% in overweight, 40.5% in obesity category I, 44.8% in obesity category II and 51.2% in obesity category III. The most prevalent single conditions in males and females were depression, back pain and other joint problems. The prevalence of individual conditions was generally associated with BMI category; women had higher rates of disease than men in several disease categories.
Table 1.
Morbidity by person–year, 2005–11
| Number of conditions | Underweight (4735) | Normal weight (152 869) | Overweight (243 251) | Obese category I (108 223) | Obese category II (31 065) | Obese category III (12 548) | |
|---|---|---|---|---|---|---|---|
| No conditions | Men | 1894 (40.0) | 60 212 (39.4) | 86 477 (35.6) | 33 619 (31.1) | 8809 (28.4) | 3191 (25.4) |
| Women | 5712 (36.6) | 94 032 (37.3) | 63 945 (30.2) | 28 328 (26.0) | 11 296 (23.9) | 5716 (21.2) | |
| One condition | Men | 1498 (31.6) | 49 965 (32.7) | 79 247 (32.6) | 34 687 (32.1) | 9420 (30.3) | 3749 (29.9) |
| Women | 4957 (31.7) | 82 795 (32.8) | 68 177 (32.2) | 33 267 (30.5) | 13 764 (29.1) | 7287 (27.0) | |
| Two conditions | Men | 830 (17.5) | 26 915 (17.6) | 46 991 (19.3) | 22 749 (21.0) | 6918 (22.3) | 2875 (22.9) |
| Women | 3153 (20.2) | 47 643 (18.9) | 46 346 (21.9) | 25 945 (23.8) | 11 490 (24.3) | 6942 (25.7) | |
| Three conditions | Men | 380 (8.0) | 10 986 (7.2) | 20 939 (8.6) | 11 270 (10.4) | 3673 (11.8) | 1492 (11.9) |
| Women | 1296 (8.3) | 20 167 (8.0) | 2248 (10.8) | 13 768 (12.6) | 6829 (14.5) | 4183 (15.5) | |
| Four conditions | Men | 96 (2.0) | 3595 (2.4) | 7161 (2.9) | 4160 (3.8) | 1622 (5.2) | 855 (6.8) |
| Women | 391 (2.5) | 6005 (2.4) | 7826 (3.7) | 5654 (5.2) | 2766 (5.9) | 1998 (7.4) | |
| Five or more conditions | Men | 37 (0.8) | 1196 (0.8) | 2436 (1.0) | 1739 (1.6) | 623 (2.0) | 386 (3.1) |
| Women | 117 (0.7) | 1664 (0.7) | 2359 (1.1) | 2191 (2.0) | 1108 (2.3) | 861 (3.2) |
Figures are frequencies (column percents). Units of analysis are person–years of observation.
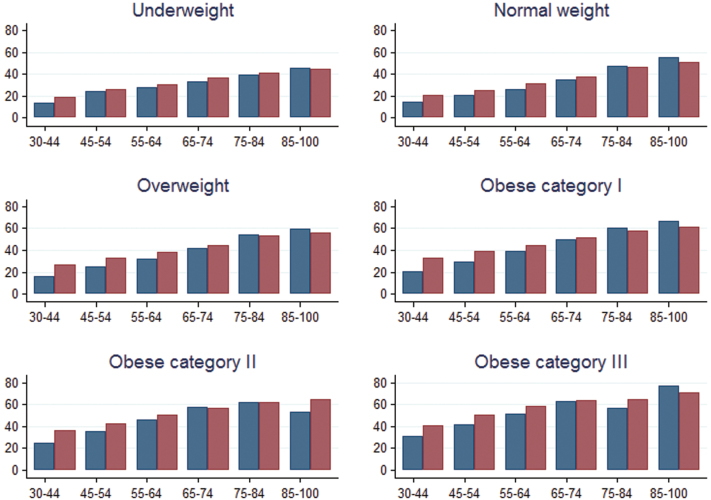
The prevalence of multimorbidity increased with age in each BMI category (Fig. 1). There was a slight decline in the prevalence of multimorbidity in men aged ≥85 with category II obesity and at ages 75–84 with category III obesity. Similar declines were not observed in women. In each age group, the prevalence of multimorbidity increased with BMI category. In underweight women aged 45–54, and men aged 45–64, the prevalence of multimorbidity was higher than that in persons of normal weight of the same age. The PAF for multimorbidity was estimated to be 19% for obesity alone, and 32% for overweight and obesity combined.
Figure 1.
Prevalence (%) of multimorbidity by age group (years) and BMI category in men and women, 2005–11
Table 2 presents the results of the multiple regression analyses. The odds of multimorbidity increased with BMI category. For overweight participants, the odds of one disease, compared with none, were 25% higher than for normal weight patients. In category I obese patients, the relative odds were 54% higher, category II obesity 81% and category III obesity 124% higher. For participants with one condition, the odds of a second or further condition were higher at each level of BMI. For participants with two conditions, the relative odds of developing three or more conditions were 2.34 for participants with category II obesity and 3.09 for participants with category III obesity, when compared with participants with normal body weight. The associations of gender and deprivation with transition to a greater number of morbidities increased in magnitude as the number of conditions increased. Women had relative odds of 1.28, compared with men, for having one or more conditions; this increased to 1.36 for having three or more diseases. Increasing age, socioeconomic deprivation and smoking also showed larger associations with higher numbers of diseases. Smokers had a relative odds of 1.13 compared with non-smokers for having one or more diseases, but former smoking showed the higher relative odds, 1.29 for one or more conditions, rising to 1.35 for three or more conditions.
Table 2.
Impact of BMI category on increasing level of multimorbidity after adjusting for confounding variables
| Increase in conditions | |||
|---|---|---|---|
| Relative odds of one or more (95% CI) | Relative odds of two or more (95% CI) | Relative odds of three or more (95% CI) | |
| Age in decades | 1.25 (1.20–1.31) | 1.45 (1.39–1.52) | 1.77 (1.66–1.89) |
| Age squared | 1.01 (1.00–1.01) | 1.00 (0.99–1.00) | 0.99 (0.98–0.99) |
| Gender | |||
| Male | Ref. | Ref. | Ref. |
| Female | 1.28 (1.25–1.30) | 1.33 (1.31–1.36) | 1.36 (1.33–1.40) |
| BMI | |||
| Underweight | 0.82 (0.78–0.87) | 0.82 (0.78–0.87) | 0.82 (0.78–0.87) |
| Normal weight | Ref. | Ref. | Ref. |
| Overweight | 1.25 (1.22–1.27) | 1.29 (1.26–1.31) | 1.36 (1.32–1.40) |
| Obese category I | 1.54 (1.51–1.58) | 1.65 (1.61–1.69) | 1.83 (1.77–1.90) |
| Obese category II | 1.81 (1.74–1.87) | 2.04 (1.98–2.11) | 2.34 (2.24–2.45) |
| Obese category III | 2.24 (2.13–2.36) | 2.63 (2.51–2.76) | 3.09 (2.92–3.28) |
| Smoking | |||
| Non-smoker | Ref. | Ref. | Ref. |
| Ex-smoker | 1.29 (1.27–1.32) | 1.30 (1.28–1.32) | 1.35 (1.32–1.38) |
| Smoker | 1.13 (1.11–1.16) | 1.13 (1.11–1.16) | 1.13 (1.11–1.16) |
| Missing | 0.36 (0.33–0.39) | 0.25 (0.21–0.29) | 0.16 (0.11–0.22) |
| Deprivation quintile | |||
| Least deprived | Ref. | Ref. | Ref. |
| 2 | 1.01 (0.99–1.04) | 1.03 (1.01–1.06) | 1.07 (1.03–1.11) |
| 3 | 1.05 (1.02–1.08) | 1.09 (1.06–1.12) | 1.14 (1.10–1.19) |
| 4 | 1.13 (1.10–1.16) | 1.19 (1.16–1.23) | 1.25 (1.20–1.30) |
| Most deprived | 1.35 (1.31–1.39) | 1.45 (1.41–1.49) | 1.60 (1.54–1.67) |
CI, confidence interval. Figures are odds ratios adjusted for each of the variables shown.
Discussion
Summary
This study evaluated the association of BMI with the prevalence of 11 conditions in a primary care population. Multimorbidity was found to be strongly associated with obesity. The prevalence of multimorbidity in category I obese patients was almost 50% higher than normal weight, and nearly double for category III obese patients. Women had consistently higher rates of multimorbidity than men. The effect of increasing BMI category on multimorbidity was similar to that of ageing, with obese patients having a prevalence of multimorbidity similar to that of normal weight patients several decades older. In the younger obese patients, aged 30–44 years, over a fifth of males and a third of females had two or more conditions. Using PAF, we estimated that almost a third of multimorbidity could be attributable to overweight and obesity, and a fifth to obesity alone, was a causal relationship to be assumed. This may have important implications for the potential to delay onset of multiple conditions through earlier and more effective management of body weight in primary care.
Strengths and limitations
The study was conducted in a large, population-based cohort and distribution of BMI was broadly comparable to national data (13). Studies using clinical data rely on the quality and completeness of data recorded by clinicians. In these analyses, 51% of BMI values were carried forward or backward by up to 3 years either side of an original record. This might have introduced misclassification with respect to BMI category. The cross-sectional nature of the analysis may have led to the classification of disease to an inappropriate BMI category as investigation of illness-related weight loss or gain was not always possible.
BMI generally increases with age in individuals, and over time in populations, but within-patient variation in BMI in primary care is generally small (7,10). Ethnic differences in disease risks associated with BMI are well established, but the CPRD does not include data on ethnicity. We used a defined set of conditions to measure multimorbidity and the READ codes used to identify relevant conditions were compiled from reference sources. The prevalence of individual conditions were comparable to those reported elsewhere, (14) suggesting that case definitions were appropriate. Odds were used to calculate the PAF, rather than risk, and this might lead to overestimation of the role of obesity on the burden of multimorbidity.
Comparison with existing literature
The definition of multimorbidity varies between studies, tends to be poorly described and no standard taxonomy exists (15). In-keeping with the aim of the paper, and in the absence of other papers investigating multimorbidity in relation to BMI, a set of conditions were selected based on the literature. Currently, researchers include different conditions when defining multimorbidity. We anticipate that this practice will continue, and a consensus on a gold standard or universal definition will be not be reached. Despite variations in definition, the estimated prevalence of overall multimorbidity was comparable to that found in other recent studies conducted in UK primary care, reinforcing our definition as a valid interpretation for the research question. Relationships identified with gender and socioeconomic deprivation were also consistent with current evidence (2,3). We anticipate that the association of BMI category with multimorbidity is likely to hold even if a different definition were to be employed because simple disease counts can be as reflective as standardized measurement tools for the prediction of mortality and health service use in relation to multimorbidity (16). We identified ex-smokers as having higher odds for additional disease, rather than current smokers, in contrast to a cohort study based on a similar set of chronic conditions (17). Possible interpretations of this result might be reverse causation caused by smokers being more likely to give up the habit when their health deteriorates (18), or weight gain after smoking cessation (19).
Implications for research and/or practice
This study is the first to quantify the relationship between excess weight and multiple disease, but will reinforce the experience of many clinicians working with overweight patients. Health professionals working in primary care should be aware of the likelihood and implications of multiple diseases in obese patients, and measurement of BMI plus formal recognition of obesity should be used to identify patients at high risk of multimorbidity in clinical practice. Weight loss can lead to reductions in the incidence of diabetes and remission of symptoms in obese patients (20). Given that both obesity and diabetes are risk factors for the onset of cardiovascular disease, it is possible that weight reduction could also impact on the incidence of other conditions such as stroke or myocardial infarction in these patients (21). BMI recording to identify and monitor obesity should be a priority for primary care clinicians, along with weight management and targeted control of other risk factors such as hypertension and hypercholesterolaemia. Such changes in practice could potentially reduce the onset and burden of multimorbidity and should be a priority for those working in primary health care services.
Declaration
Funding: This research was supported by the National Institute for Health Research Biomedical Research Centre at Guy’s and St Thomas’ NHS Foundation Trust and King’s College London. This study was supported by the UK National Prevention Research Initiative (http://www.npri.org.uk) whose funding partners include the Alzheimer’s Research Trust; Alzheimer’s Society; Biotechnology and Biological Sciences Research Council; British Heart Foundation; Cancer Research UK; Chief Scientist Office, Scottish Government Health Directorate; Department of Health; Diabetes UK; Economic and Social Research Council; Engineering and Physical Sciences Research Council; Health & Social Care Research & Development Office for Northern Ireland; Medical Research Council; The Stroke Association; Welsh Assembly Government and World Cancer Research Fund.
Ethical approval: Ethical approval for the study protocol was granted by the Independent Scientific Advisory Committee (ISAC) of the Medicines and UKHMRA (ISAC Protocol No. 07-054R).
Conflict of interest: The authors of this study have no conflicts of interest to declare.
Acknowledgements
The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
References
- 1. Fortin M, Stewart M, Poitras ME, Almirall J, Maddocks H. A systematic review of prevalence studies on multimorbidity: toward a more uniform methodology. Ann Fam Med 2012; 10: 142–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Salisbury C, Johnson L, Purdy S, Valderas JM, Montgomery AA. Epidemiology and impact of multimorbidity in primary care: a retrospective cohort study. Br J Gen Pract 2011; 61: e12–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet 2012; 380: 37–43 [DOI] [PubMed] [Google Scholar]
- 4. Smith SM, O’Dowd T. Chronic diseases: what happens when they come in multiples? Br J Gen Pract 2007; 57: 268–70 [PMC free article] [PubMed] [Google Scholar]
- 5. Fortin M, Bravo G, Hudon C, Lapointe L, Dubois MF, Almirall J. Psychological distress and multimorbidity in primary care. Ann Fam Med 2006; 4: 417–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Anderson G. Chronic Care: Making the Case for Ongoing Care. Princeton, NJ: Robert Johnson Wood Foundation, 2010. http://www.rwjf.org/content/dam/farm/reports/reports/2010/rwjf54583 [Google Scholar]
- 7. Booth HP, Prevost AT, Gulliford MC. Epidemiology of clinical body mass index recording in an obese population in primary care: a cohort study. J Public Health (Oxf) 2013; 35: 67–74 [DOI] [PubMed] [Google Scholar]
- 8. Waring ME, Roberts MB, Parker DR, Eaton CB. Documentation and management of overweight and obesity in primary care. J Am Board Fam Med 2009; 22: 544–52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Must A, Spadano J, Coakley EH, Field AE, Colditz G, Dietz WH. The disease burden associated with overweight and obesity. JAMA 1999; 282: 1523–9 [DOI] [PubMed] [Google Scholar]
- 10. Prospective Studies Collaboration Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. The Lancet 2009; 373: 1083–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wang F, Xu S, Shen X, Guo X, Shen R. Epidemiology of multimorbidity. Lancet 2012; 380: 1382–3; author reply 1383–4. [DOI] [PubMed] [Google Scholar]
- 12. World Health Organisation Metrics: population attributable fraction (PAF), 2013. [09/01/2013]. http://www.who.int/healthinfo/global_burden_disease/metrics_paf/en/index.html
- 13. Joint Health Surveys Unit Health Survey for England - 2010: Trend tables 2011 [cited 2012. 10/12/2012]. http://www.ic.nhs.uk/statistics-and-data-collections/health-and-lifestyles-related-surveys/health-survey-for-england/health-survey-for-england--2010-trend-tables
- 14. Kress AM, Hartzel MC, Peterson MR. Burden of disease associated with overweight and obesity among U.S. military retirees and their dependents, aged 38-64, 2003. Prev Med 2005; 41: 63–9 [DOI] [PubMed] [Google Scholar]
- 15. France EF, Wyke S, Gunn JM, Mair FS, McLean G, Mercer SW. Multimorbidity in primary care: a systematic review of prospective cohort studies. Br J Gen Pract 2012; 62: e297–307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Huntley AL, Johnson R, Purdy S, Valderas JM, Salisbury C. Measures of multimorbidity and morbidity burden for use in primary care and community settings: a systematic review and guide. Ann Fam Med 2012; 10: 134–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Taylor AW, Price K, Gill TK, et al. Multimorbidity - not just an older person’s issue. Results from an Australian biomedical study. BMC Public Health 2010; 10: 718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Freund KM, D’Agostino RB, Belanger AJ, Kannel WB, Stokes J., 3rd Predictors of smoking cessation: the Framingham Study. Am J Epidemiol 1992; 135: 957–64 [DOI] [PubMed] [Google Scholar]
- 19. Williamson DF, Madans J, Anda RF, Kleinman JC, Giovino GA, Byers T. Smoking cessation and severity of weight gain in a national cohort. N Engl J Med 1991; 324: 739–45 [DOI] [PubMed] [Google Scholar]
- 20. Diabetes Prevention Program Research Group Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002; 346: 393–403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. The Look AHEAD Research Group Long-term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes mellitus: four-year results of the Look AHEAD Trial. Arch Intern Med 2010; 170: 1566–75 [DOI] [PMC free article] [PubMed] [Google Scholar]