Abstract
Aim: To summary the experience for prevention and treatment of recurrent laryngeal nerve (RLN) injury in thyroid surgery. Methods: Clinical features of 623 patients who received thyroid surgery from January 2010 to December 2012 were analyzed retrospectively, and the features of RLN injury and intraoperative as well as postoperative treatments were reviewed. Results: RLN injury occurred in 31 patients (4.98%), in which, unilateral RLN injury occurred in 27 patients and bilateral RLN injuries occurred in 4 patients (temporary injury in 28 patients and permanent injury in 3 patients). 6 patients underwent RLN anastomosis during surgery and exhibited transient hoarseness after surgery. RLN exploration and decompression was given in 1 patient and the patient got normal vocal cord motion 2 months after surgery. 1 patient with bilateral injuries received tracheotomy and CO2 laser resection of arytenoid cartilage and achieved recovery 1 year later. Conclusions: In order to prevent RLN injury, the anatomic variations of RLN should be mastered. Routine exposure of RLN can effectively prevent the injury in patients receiving the second or multiple surgeries. Early interventions for RLN injury include mainly early discovery, early exploration and early anastomosis, and the function of RLN in some patients can recover completely. Subsequent treatments mainly focus on the improvement of the voice, expansion of glottis and melioration of dyspnea.
Keywords: Thyroid surgery, recurrent laryngeal (RLN) injury, prevention, treatment
Introduction
Recurrent laryngeal nerve (RLN) injury is a common severe complication in thyroid surgery [1], and unilateral RLN injury is more common. With the increase of awareness and the improvement of surgical techniques, the incidence of RLN injury has declined (about 0.5%~5% in the foreign reports) [2]. Unilateral RLN injury can cause varying degrees of hoarseness, microaspiration, coughing and other symptoms, seriously affecting patients’ quality of life [3], and bilateral RLN injuries may induce aphonia, dyspnea, and even asphyxia to threaten the life of patients. RLN injury is also one of the important reasons for medical dispute from thyroid surgery [4]. Therefore, it is very important how to prevent and deal with RLN injury during thyroid surgery. In this paper, the relevant clinical data of 623 patients who received thyroid surgery in our department from Jan 2010 to Dec 2012 were retrospectively analyzed, and the causes of RLN injury in thyroid surgery and the prevention experience were summarized. Now the details were reported as follows.
Materials and methods
General data
623 patients (268 males and 355 females [1:1.32]; mean age: 46.5±29.5 years) were treated in Department of General Surgery of our hospital from January 2010 to December 2012, among whom, there were 230 patients with nodular goiter, 128 patients with nodular goiter and thyroid adenoma, 50 patients with thyroid adenoma, 182 patients with thyroid cancer, 29 patients with chronic lymphocytic thyroiditis and 4 patients with granulomatous thyroiditis.
Previous surgery history
34 patients had the history of thyroid surgery, among whom 3 patients had received multiple thyroid surgeries.
Laryngoscopy
All the patients received preoperative fiberoptic laryngoscopy, and laryngoscopy found that the unilateral vocal cord fixation existed in 2 patients with preoperative hoarseness and the normal vocal cord movement was found in the remaining 621 patients (see Figure 1).
Figure 1.
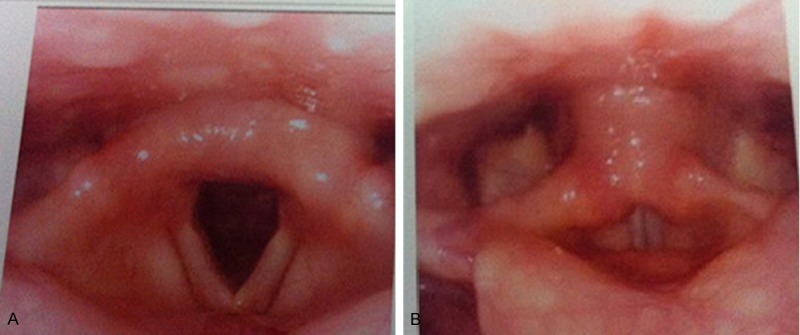
The normal opening and closing of bilateral vocal cords. A. Opening of vocal cords; B. Closing of vocal cords.
Surgical methods
All the patients received surgery under general anesthesia. 5 patients received biopsy of thyroid nodule and 64 patients underwent resection of thyroid tumor, 109 patients underwent unilateral subtotal resection, 189 patients underwent unilateral resection of total thyroid, 43 patients underwent bilateral subtotal resection, 127 patients underwent resection of one side and isthmus and subtotal resection of the other side, 35 patients underwent bilateral thyroid and isthmus resection and 51 patients underwent bilateral and isthmus resection with neck nodal dissection. During surgery, RLN was exposed in 528 patients (see Figure 2), and no RLN was exposed in 95 patients.
Figure 2.
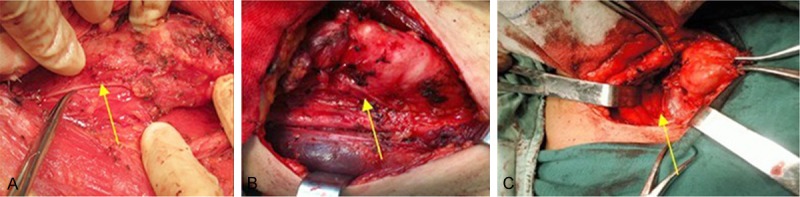
Exposing RLN during the surgery (A-C, arrow: RLN).
Injury criteria
Preoperative routine examination of vocal cords showed that the preoperative vocal cords movements were normal in patients. But postoperative hoarseness was exhibited, and laryngoscopy showed that the vocal cord fixation was caused by RLN injury (see Figure 3). Patients diagnosed with RLN injury whose pronunciation returned to normal and who exhibited normal vocal cord movement by laryngoscopy within six months after surgery were considered to have temporary injury; patients in whom the nerves had been separated during the operation or the vocal cord movement was abnormal after six months from surgery were considered to be permanent injury.
Figure 3.
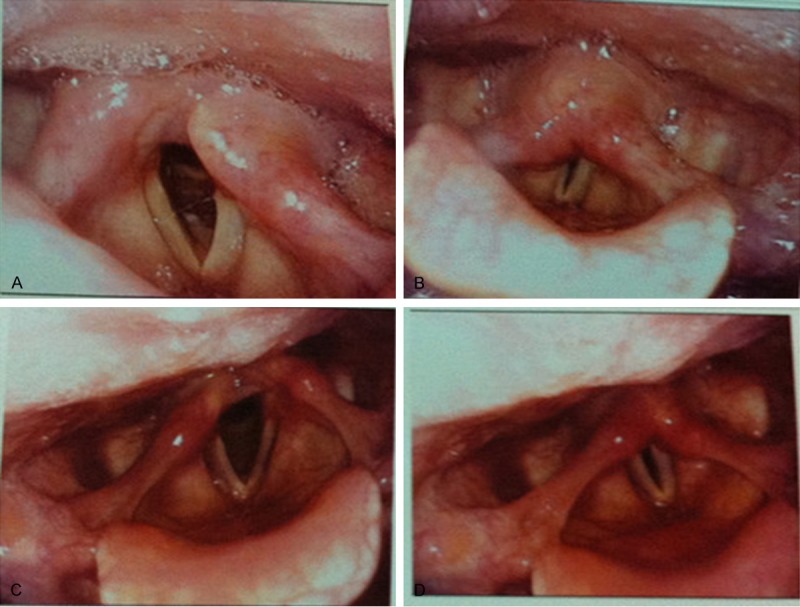
Limited vocal cord movement after RLN injury. A. Good movement of the right vocal cord; B. Fixation and poor closure in the left vocal cord; C. Good movement of the left vocal cord; D. Fixation and poor closure in the right vocal cord.
Results
Incidence of RLN injury
No death occurred during the operation and after the operation. Unilateral RLN injury occurred in 27 patients, bilateral RLN injury occurred in 4 patients, temporary injury occurred in 28 patients, and permanent injury occurred in 3 patients. The incidence of RLN injury in this group was about 4.98%, in which, the unilateral and temporary injury accounted for about 87% and 90%, respectively.
The incidence of RLN injury was about 4.61% (27/586) in the first surgery and 10.81% (4/37) in the second or multiple surgeries. RLN injury occurred in the single, second and multiple surgeries for the different diseases are provided in Table 1.
Table 1.
RLN injury in the surgeries for the different diseases
| Diseases | Second or multiple surgeries | The first surgery | ||
|---|---|---|---|---|
|
| ||||
| RLN injury | Normal RLN | RLN injury | Normal RLN | |
| Nodular goiter | 1 | 19 | 10 | 200 |
| Nodular goiter and adenoma | 1 | 6 | 3 | 118 |
| Thyroid adenoma | 0 | 1 | 0 | 49 |
| Thyroid cancer | 2 | 7 | 12 | 161 |
| Chronic lymphocytic thyroiditis | 0 | 0 | 1 | 28 |
| Granulomatous thyroiditis | 0 | 0 | 1 | 3 |
| Total | 4 | 33 | 27 | 559 |
The incidence of injury in the exposed RLN group and the unexposed RLN group was about 3.79% (20/528) and 11.58% (11/95) during the operation, respectively. In RLN exposed group with a variety of surgical methods, RLN injury occurred in 20 patients; in unexposed RLN group, RLN injury occurred in 11 patients. See Table 2.
Table 2.
RLN injury caused by a variety of surgical methods
| Surgical methods | Exposed RLN group | Unexposed RLN group | ||
|---|---|---|---|---|
|
| ||||
| RLN injury | Normal RLN | RLN injury | Normal RLN | |
| Biopsy of thyroid nodule | 0 | 0 | 0 | 5 |
| Resection of thyroid tumor | 0 | 18 | 2 | 44 |
| Unilateral subtotal resection | 4 | 100 | 1 | 4 |
| Unilateral resection of total thyroid | 7 | 171 | 2 | 9 |
| Bilateral subtotal resection | 1 | 29 | 2 | 11 |
| Resection of one side and isthmus and subtotal resection of the other side | 5 | 115 | 2 | 5 |
| Bilateral thyroid and isthmus resection | 1 | 26 | 2 | 6 |
| Bilateral and isthmus resection with neck nodal dissection | 2 | 49 | 0 | 0 |
| Total | 20 | 508 | 11 | 84 |
Results of postoperative management
Postoperative RLN exploration and decompression were given in 1 patient, and he had vocal cord motion recovery 2 months after surgery. The remaining 27 patients underwent treatment with neurotrophy and glucocorticoids, and the voice and vocal cord movement returned to normal 1-3 months after surgery. 6 patients were found to have unilateral RLN separation during the operation and were given immediately free-tension anastomosis of RLN (Figure 4), and they exhibited transient hoarseness after surgery which recovered within 1-2 months. 1 patient with granulomatous thyroiditis who showed postoperative bilateral RLN injuries had an obvious hypofunction of thyroid, and exhibited hoarseness and dyspnea 1 year after surgery due to lack of regular follow-up visit in clinic and regular medications, so she/he was given tracheotomy and CO2 laser resection of bilateral arytenoid cartilage in stages in otolaryngological department and the regular treatment with the medicines after surgery; and then the trachea was sealed successfully, the dyspnea were relieved significantly; finally the patient had normal status after 1 year.
Figure 4.

RLN anastomosis (arrow: RLN).
Discussions
Incidence of RLN injury
There are reports about the incidence of RLN injury caused by the thyroid surgery [6] (about 0.5%-5% in the foreign reports) [2], and unilateral RLN injury is more common. The incidence of RLN injury in this group was about 4.98% (the unilateral injury and temporary injury accounted for about 87% and 90%, respectively). The incidence of RLN injury (about 10.81%) in the second or multiple surgeries was obviously higher than that (about 4.61%) in the first surgery, which was attributed to unclear anatomical levels, serious adhesion and increased difficulty of operation when the surgery was performed again [5].
The incidence of injury in exposed RLN group and the unexposed RLN group was about 3.79% and 11.58% during the operation, respectively. The results showed that the exposure of RLN can reduce the incidence of RLN injury in thyroid surgery and is an important measure to prevent RLN injury [6,7].
There has been controversy about the routine dissection and exposure of RLN in thyroid surgery [8], and most scholars believe that only thorough exposure of RLN can ensure that the operators can operate correctly under direct vision and the probability of RLN injury can be reduced because there are more anatomic variations for RLN [4,9], while some doctors still insisted that the dissection and dissociation of RLN after identification may increase the risk of RLN injury [10,11]. However, intra-operative neuromonitoring confirmed that the postoperative RLN and electromyographic signal from vagus was not statistically different from those before surgery under exposure of RLN in the entire operation process, and the extension of RLN dissection length during the surgery neither increase the incidence of RLN injury nor reduce the conductivity of the nerve, so it is safe to carefully dissect and expose RLN [7,12]. The author believes that the majority of surgical procedures for thyroid can easily damage RLN, therefore, RLN should be exposed routinely, and routine dissection for exposure of RLN should be performed especially for the patients receiving the second or multiple surgeries.
Causes of RLN injury
Causes of RLN injury are summarized as follows: 1) anatomic variation and transfer: there is insufficient knowledge of normal anatomy and variation of RLN, and the nerves may be clamped or pulled in the dissection and exposure process especially due to the complicated and changeful relationship of the inferior thyroid artery and RLN; 2) hemorrhage during operation: unclear exposure of surgical field was caused, and nerves may be easily damaged at blind clamping and electric coagulation hemostasis; 3) larger lesions in the thyroid: nerves can be moved and infiltrated, and nerve edema can be induced by forcible pulling or clamping at dissociation to cause temporary injury of the nerves; 4) the second or multiple surgeries: the inordinate anatomical structure of thyroid, changes and destruction of the anatomical levels of the adjacent tissues, tissue adhesions, cicatricial contraction and other factors may cause RLN transfer and shift to easily damage the nerves, and the obvious adhesion at trachea and esophageal groove and the incomplete exposure of RLN is more likely to cause the nerve injury especially at the entrance point of RLN into the larynx (inferior horn of thyroid cartilage); 5) the postoperative edema and errhysis on the surgical wound may lead to pressure on the nerves.
Prevention of RLN injury
The key for avoiding and reducing RLN injury should be placed on the prevention, and the prevention methods are as follows: 1) improvement of preoperative examination (because the preoperative detailed examination can assess in advance the difficulty of surgery to predict the likelihood of injury), 2) being familiar with the dissection and variations of RLN (because the key for avoiding the injury of nerves is to correctly indentify and safely dissect RLN during the operation), 3) the use of the operators who have a good basic skills in the surgery (because full exposure and clear surgical field can be ensured, and the electric knifes or electric coagulation should not be used during the operation close to the nerve to achieve thorough hemostasis, thus ensuring that the injury will not occur in the process of separation, clamping, resection and suturing, and also preventing the nerve compression due to post-operation bleeding to induce secondary injury); 4) gently operating by the operators to avoid the forcible traction of the thyroid tissues, and focusing your attention on the site of RLN where the injury can occurred easily; 5) the intraoperative neuromonitoring that can effectively reduce RLN injury [4]; 6) unnecessarily performing dissection of RLN for patients with huge substernal goiter because the retention of thyroid membrane in the back can effectively avoid the injury.
Intraoperative neuromonitoring of RLN (IONM)
Intraoperative neuromonitoring of RLN (i.e. IONM) has brought the following benefits: significantly reducing iatrogenic RLN injury, increasing the scope of surgical safety, improving the identification rate of RLN, accelerating the intraoperative RLN identification and reducing accidental injury [4,13,14], effectively evaluating the anatomic variations (the incidence of extralaryngeal branch and non-recurrent laryngeal nerve was 30% and 0.5%, respectively), defining the relationship of anatomical structure and nerve function, positioning the damage spots of the nerves, assessing the damage mechanisms, helping to timely remove the causes for injury and implementing the remedial measures and reducing the postoperative incidence and severity of complications [15-17]. However, it can not still substitute for the detailed knowledge of neuroanatomy, intraoperative visual identification of RLN and precise surgical technique [18], and the improper use of monitoring equipment for the never can also cause complications, for example, the excessive stimulated current would cause skin burns.
Treatment of RLN injury
Unilateral RLN injury can cause varying degrees of hoarseness, microaspiration, coughing and other symptoms, and bilateral RLN injuries may induce aphonia, dyspnea, and even asphyxia to threaten the life of the patients. The treatment methods include the medicines (neurotrophic medicines, glucocorticoids and vasodilators); ultrashort wave therapy, acupuncture and moxibustion and others; voice training, vocal cord injection and others; reinnervation methods of the unilateral RLN injury (including RLN decompression, end to end anastomosis of RLN, main branch of ansa cervicalis to RLN anastomosis [19], implantation of ansa cervicalis-nerve muscular pedicle [20], etc.).
The reinnervation methods of RLN injury should be selected according to the course of disease, the extent of neurological injury and the types. The laryngeal muscles will exhibit atrophy and fibrosis after denervation. With the prolongation of denervation time, the pathological changes will be more obvious. There is spontaneous regeneration after RLN injury, which can make intrinsic laryngeal muscle obtaining subclinical innervation to slow down the atrophy and fibrosis of laryngeal muscle induced by denervation to some extent [21]; however, the prolonged denervation will cause the sever denervation of the muscle, resulting in atrophy and fibrosis, and even if reinnervation is performed then, the atrophy and fibrosis of the muscle caused by denervation can not be reversed completely, thereby, and the contractility of the muscle can not be fully restored.
In the early treatment of RLN injury, the exploration should be performed as soon as possible, that is, the exploration of RLN at the affected side should be given unhesitatingly during the entire process when RLN injury is suspected during the operation, and one-stage repair should be provided with the different surgical methods according to the conditions of injury, and the suture can be released in case of suture ligation; patients with separated nerve injury should be given immediately end to end anastomosis of RLN. As for the injury found after surgery, if the patient exhibited postoperative good voice which was changed after several days, and RLN was exposed correctly during the entire process, the neurotrophic drugs, hormonal medicines or physiotherapy can be given as the conservative treatment, and the condition can return to normal 3 months after surgery; if the ligation and separation of the nerve is suspected highly, the nerve should be cut decidedly for seeking the affected site and then the neurolysis or anastomosis should be given; patients who are not suitable for RLN decompression can receive end to end anastomosis of RLN, ansa cervicalis to RLN anastomosis, implantation of ansa cervicalis-nerve muscular pedicle, nerve implantation and other nerve reinnervation, most of whom will go back to the normal status.
The late treatment methods of RLN injury include thyroplasty, injection into and near vocal cords and arytenoid adduction, in order to move the vocal cords inward and to improve the voice; and laser arytenoidectomy, cordectomy, vocal cord abduction and fixation in order to expand glottis and improve the dyspnea. 1 patient in this group received tracheotomy and CO2 laser resection of bilateral arytenoid cartilage and restored the normal status 1 year after surgery.
The treatment principles for RLN injury are early interventions mainly including early discovery, early exploration and early anastomosis with a better treatment effect (RLN function can restore fully in some patients, and patients’ quality of life can be improved) and late treatment mainly includes the improvement o voice, expansion of glottis and melioration of dyspnea.
Disclosure of conflict of interest
None declared.
References
- 1.Akin M, Kurukahvecioglu O, Anadol AZ, Yuksel O, Taneri F. Analysis of surgical complications of thyroid diseases: results of a single institution. Bratisl Lek Listy. 2009;110:27–30. [PubMed] [Google Scholar]
- 2.Trésallet C, Chigot JP, Menegaux F. How to prevent recurrent nerve palsy during thyroid surgery? Ann Chir. 2006;131:149–153. doi: 10.1016/j.anchir.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 3.Shaw GY, Pierce E. Malpractice litigation involving iatrogenic surgical vocal fold paralysis: a closed-claims review with recommendations for prevention and management. Ann Otol Rhinol Laryngol. 2009;118:6–12. doi: 10.1177/000348940911800102. [DOI] [PubMed] [Google Scholar]
- 4.Marcus B, Edwards B, Yoo S, Byrne A, Gupta A, Kandrevas J, Bradford C, Chepeha DB, Teknos TN. Recurrent laryngeal nerve monitoring in thyroid and parathyroid surgery: the University of Michigan experience. Laryngoscope. 2003;113:356–361. doi: 10.1097/00005537-200302000-00028. [DOI] [PubMed] [Google Scholar]
- 5.Gibelin H, Sierra M, Mothes D, Ingrand P, Levillain P, Jones C, Hadjadj S, Torremocha F, Marechaud R, Barbier J, Kraimps JL. Risk factors for recurrent nodular goiter after thyroidectomy for benign disease: case-control study of 244 patients. World J Surg. 2004;28:1079–1082. doi: 10.1007/s00268-004-7607-x. [DOI] [PubMed] [Google Scholar]
- 6.Aytac B, Karamercan A. Recurrent laryngeal nerve injury and preservation in thyroidectomy. Saudi Med J. 2005;26:1746–1749. [PubMed] [Google Scholar]
- 7.Chiang FY, Wang LF, Huang YF, Lee KW, Kuo WR. Recurrent laryngeal nerve palsy after thyroidectomy with routine identifi cation of the recurrent laryngeal nerve. Surgery. 2005;137:342–347. doi: 10.1016/j.surg.2004.09.008. [DOI] [PubMed] [Google Scholar]
- 8.Shindo ML, Wu JC, Park EE. Surgical anatomy of the recurrent laryngeal nerve revisited. Otolaryngol Head Neck Surg. 2005;133:514–519. doi: 10.1016/j.otohns.2005.07.010. [DOI] [PubMed] [Google Scholar]
- 9.Yalçin B, Poyrazoglu Y, Ozan H. Relationship Detween Zuckerkandl’s tubercle and the inferior laryngeal nerve including the laryngeal branches. Surg Today. 2007;37:109–113. doi: 10.1007/s00595-006-3346-y. [DOI] [PubMed] [Google Scholar]
- 10.Procacciante F, Picozzi P, Pacifici M, Picconi S, Ruggeri S, Fantini A, Basso N. Palpatorymethod used to identify the recurrent laryngeal nerve during thyroidectomy. World J Surg. 2000;24:571–573. doi: 10.1007/s002689910093. [DOI] [PubMed] [Google Scholar]
- 11.Makay O, Icoz G, Yilmaz M, Akyildiz M, Yetkin E. The recurrent laryngeal nerve and the inferior thyroid artery-anatomical variations during surgery. Langenbecks Arch Surg. 2008;393:681–685. doi: 10.1007/s00423-008-0320-8. [DOI] [PubMed] [Google Scholar]
- 12.Duclos A, Lifante JC, Ducarroz S, Soardo P, Colin C, Peix JL. Influence of intraoperative neuromonitoring on surgeons’technique during thyroidectomy. World J Surg. 2011;35:773–778. doi: 10.1007/s00268-011-0963-4. [DOI] [PubMed] [Google Scholar]
- 13.Tomoda C, Hirokawa Y, Uruno T, Takamura Y, Ito Y, Miya A, Kobayashi K, Matsuzuka F, Kuma K, Miyauchi A. Sensitivity and specificity of intraoperative recurrent laryngeal nerve stimulation test for predicting vocal cord palsy after thyroid surgery. World J Surg. 2006;30:1230–1233. doi: 10.1007/s00268-005-0351-z. [DOI] [PubMed] [Google Scholar]
- 14.Chiang FY, Lee KW, Chen HC. Standardization of intraoperative neuromonitoring of recurrent laryngeal nerve in thyroid operation. World J Surg. 2010;34:223–229. doi: 10.1007/s00268-009-0316-8. [DOI] [PubMed] [Google Scholar]
- 15.Barczyński M, Konturek A, Cichoń S. Randomized clinical trial of visualization versus neuromonitoring of recurrent laryngeal nerves during thyroidectomy. Br J Surg. 2009;96:240–246. doi: 10.1002/bjs.6417. [DOI] [PubMed] [Google Scholar]
- 16.Serpell JW, Yeung MJ, Grodski S. The motor fibers of the recurrent laryngeal nerve are located of the recurrent laryngeal nerve are located in the anterior extralaryngeal branch. Ann Surg. 2009;249:648–652. doi: 10.1097/SLA.0b013e31819ed9a4. [DOI] [PubMed] [Google Scholar]
- 17.Dralle H, Sekulla C, Lorenz K, Brauckhoff M, Machens A German IONM Study Group. Intraoperative monitoring of the recurrent laryngeal nerve in thyroid surgery. World J Surg. 2008;32:1358–1366. doi: 10.1007/s00268-008-9483-2. [DOI] [PubMed] [Google Scholar]
- 18.Agha A, Glockzin G, Ghali N, Iesalnieks I, Schlitt HJ. Surgical Treatment of Substernal Goiter: An Analysis of 59 Patients. Surg Today. 2008;38:505–511. doi: 10.1007/s00595-007-3659-5. [DOI] [PubMed] [Google Scholar]
- 19.Wang W, Chen D, Chen S, Li D, Li M, Xia S, Zheng H. Laryngeal reinnervation using ansa cervicalis for thyroid surgery-related unilateral vocal fold paralysis: a long-term outcome analysis of 237 cases. PLoS One. 2011;6:e19128. doi: 10.1371/journal.pone.0019128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yumoto E, Sanuki T, Toya Y, Kodama N, Kumai Y. Nerve-muscle pedicle flap implantation combined with arytenoids adduction. Arch Otolaryngol Head Neck Surg. 2010;136:965–969. doi: 10.1001/archoto.2010.155. [DOI] [PubMed] [Google Scholar]
- 21.Chen D, Chen S, Wang W, Zhang C, Zheng H. Spontaneous regeneration of recurrent laryngeal nerve following long-term vocal fold paralysis in humans: histologic evidence. Laryngoscope. 2011;121:1035–1039. doi: 10.1002/lary.21739. [DOI] [PubMed] [Google Scholar]


