Abstract
Background and Objective: Pneumonia is a common disease with both high morbidity and mortality, the diagnosis of pneumonia remains a clinical challenge. Many studies have been conducted to identify the usefulness of lung ultrasound for the diagnosis of pneumonia, but with inconsistent and inconclusive results. The present study aimed to establish the overall diagnostic accuracy of lung ultrasound in diagnosing pneumonia. Methods: Based on a comprehensive search of the Pubmed, Embase, and the Cochrane database, we identified out-come data from all articles estimating diagnostic accuracy with lung ultrasound for pneumonia. Quality was assessed with the Quality Assessment for Diagnostic Accuracy Studies. Results from different studies were pooled using a bivariate meta-analysis. Summary receiver operating characteristic curve was used to assess the overall performance of lung ultrasound-based assays. Results: Nine studies containing 1080 subjects were included in this meta-analysis. The summary estimates for lung ultrasound in the diagnosis of pneumonia in the studies included were as follows: sensitivity, 0.97 (95% CI: 0.93-0.99); specificity, 0.94 (95% CI: 0.85-0.98); DOR, 507.99 (95% CI: 128.11-2014.34); positive likelihood ratio, 15.62 (95% CI: 6.31-38.68); negative likelihood ratio, 0.03 (95% CI: 0.01-0.08); The area under the summary receiver operating characteristic curve was 0.99 (95% CI: 0.98-1.00). Conclusion: Lung ultrasound is a capable of diagnosing pneumonia with high accuracy and is a promising attractive alternative to chest radiography and thoracic CT scan.
Keywords: Lung ultrasound, pneumonia, diagnosis, meta-analysis
Introduction
Pneumonia is a common and potentially life-threatening disease, which is associated with increasing morbidity, mortality, hospitalization rate and health care costs. In the United States in 2009, more than 54,000 deaths in the United States were attributed to pneumonia [1]. Most deaths from community acquired pneumonia (CAP) occur in elderly patients with multiple comorbid conditions [2]. Pneumonia is also held responsible of the reason for death of children [3]. More than $17 billion were paid for the overall cost of care for patients with CAP annually in the United States [4]. Because of both the clinical and the financial burden of CAP, efficient and cost-effective diagnostic options for pneumonia should be considered. Clinical history and physical examination can’t provide certainty in this diagnosis. The chest X-ray (CXR) is still recommended to be the first imaging step for diagnosing pneumonia, nevertheless, we have limited data on the sensitivity and specificity of the test [5]. Although thoracic CT scan is a diagnostic tool with high sensitivity and specificity, it is not always available in all levels hospital and has limitations of high cost and high radiation dose [6]. For children, the critically ill and the pregnant, CT and CXR are not adequate.
In the last decades, ultrasound has been shown to be highly effective in evaluating a range of pathologic conditions [7]. Lung ultrasound (LUS) is increasingly being used as a valuable bedside method in diagnosing pulmonary diseases, by providing a user-friendly, inexpensive, noninvasive, and reliable examination. The availability of portable equipment also has made chest ultrasonography an interesting and alternative method in intensive care unit and emergency department [8]. LUS takes advantage in some pulmonary conditions. Compared to CXR performed on a supine patient, LUS proves to be more sensitive in detecting pneumothorax [9]. LUS is also more efficient than CXR in pleural effusion diagnosis [10]. In addition, research has shown that modified trans-thoracic LUS is useful in the evaluation of pulmonary alveoli-interstitial involvement of rheumatoid lung disease [11]. To date, several studies have investigated the application of LUS in the diagnosis of pneumonia but with inconsistent results. The aim of this study was to evaluate the overall diagnostic accuracy of chest US for pneumonia.
Method
Data source and search strategy
Two investigators independently performed a systematic electronic search of the Pubmed, Embase and Cochrane database until September 1, 2013 to identify potentially relevant articles on the usefulness of LUS in the diagnosis of pneumonia. The following search terms were used: “Ultrasonography or Ultrasound or Sonography”, “pneumonia”, and “sensitivity or specificity”. We reviewed the bibliographies of all selection articles to identify additional relevant studies.
Selection of studies
Two reviewers independently screened titles and abstracts of all studies for relevance. Disagreements were resolved by a third opinion. The strength of the individual studies was weighed for relevance, based on following items: 1. the clinical domains should include patients with suspected pneumonia; 2. the reference diagnostic standards were clearly described and all patients were diagnosed by using the reference standards; 3. completeness of data (numbers of true-positive, false-positive, true-negative, false negative) were reported, to allow reconstruction of the diagnostic 2 by 2 table; 4. the studies were written in English. A study was excluded if it didn’t meet above mentioned criteria.
Data extraction and quality assessment
The final set of articles was assessed independently by two reviewers. The retrieved data included author, publication year, the number of included specimens (true-positive, false-positive, true-negative, false negative), sensitivity and specificity. The methodological quality of included studies was evaluated using the Quality Assessment for Studies of Diagnostic Accuracy (QUADAS) tool [12]. This is an evidence-based approach to quality assessment intended for use in systematic reviews of diagnostic accuracy studies. A quality index is generated, with a maximum value of 14.
Statistical analysis
We used standard methods recommended for meta-analyses of diagnostic test evaluations [13]. By using a bivariate regression approach, we estimated the pooled sensitivity (SEN) and specificity (SPE), positive and negative likelihood ratios (PLR and NLR, respectively), and constructed summary receiver operating characteristic (SROC) curve to summarize the study results [14]. Based on random-effects models, this bivariate approach accounts for potential between-study heterogeneity and incorporates the possible correlation between the SEN and the SPE.
Heterogeneity was assessed through the test of inconsistency (I2) of the pooled diagnostic odds ratios (DORs) [15]. DOR illustrated the odds of a positive test result in patients with pneumonia compared with patients without pneumonia: (TP/FN)/(FP/TN). It indicated the accuracy of a diagnostic test, corresponding to particular pairings of SEN and SPE [16]. Since publication bias is of concern for meta-analyses of diagnostic studies, the publication bias of included studies was inspected by using Deek’s funnel plot [17]. Posttest probability (PTP) was calculated by using the nomograms of Fagan [18]. All the statistical analysis was analyzed by using software Stata 12.0 (Stata Corporation, College Station, TX, USA).
Results
We evaluated these citations and the bibliographies of the potential studies. Consequently, nine unique publications were available for analysis of the diagnostic accuracy of lung ultrasound in pneumonia [19-27]. The main reasons of excluding studies were as follows: the study was a duplicate between the Pubmed and Embase database, the study was not diagnostic, or the study can’t reconstruct the diagnostic 2 by 2 table.
Study characteristics and quality assessment
The final set of nine studies included 1080 subjects, in which 644 cases were with pneumonia and 436 controls. In all involved studies, most used CXR or CT as a reference standard to diagnose pneumonia. We could find filtration, patch or consolidation on radiography, with pleural effusion or not [28]. Some studies adopted the comprehensive result of CT, clinical course, conventional tests and follow-up outcomes as a diagnostic standard, which was considered to be clinical diagnosis. All of the included studies were prospective. The quality of the 7 studies was generally high, satisfying the majority of the criteria. The study characteristics, along with QUADAS scores, were outlined in Table 1.
Table 1.
Summary data from the nine studies included in the meta-analysis
| Author (Ref) | Country | Design | Year | n | Diagnostic standard | TP | FP | TN | FN | QUADAS score |
|---|---|---|---|---|---|---|---|---|---|---|
| Angelika Reissig [19] | Germany | prospective | 2012 | 356 | CXR/CT | 211 | 3 | 127 | 15 | 13 |
| Americ Testa [20] | Italy | prospective | 2012 | 67 | clinic | 32 | 5 | 28 | 2 | 13 |
| Francesca Cortellaro [21] | Italy | prospective | 2010 | 120 | clinic | 80 | 2 | 37 | 1 | 11 |
| D. Iuri [22] | Italy | prospective | 2008 | 32 | CXR | 20 | 2 | 8 | 2 | 10 |
| Vaishali P. Shah [23] | US | prospective | 2012 | 200 | CXR | 31 | 18 | 146 | 5 | 13 |
| Hadeel M. Seif El Dien [24] | Egypt | prospective | 2013 | 75 | CXR | 64 | 4 | 7 | 0 | 11 |
| Stefano Parlamento [25] | Italy | prospective | 2009 | 49 | CXR/CT | 31 | 0 | 17 | 1 | 10 |
| R. Copetti [26] | Italy | prospective | 2008 | 79 | CXR/CT | 60 | 0 | 0 | 19 | 10 |
| Caiulo VA [27] | Italy | prospective | 2013 | 88 | clinic | 88 | 0 | 1 | 13 | 12 |
CXR: There is filtration, patch or consolidation on chest radiography, with pleural effusion or not. CXR/CT: CT is considered the reference standard when CXR is uncertain for diagnosis or CXR is negative while lung ultrasound is positive. Clinic: Diagnosis of pneumonia is based on comprehensive results of CT, clinical course, conventional tests and follow-up. TP: True positive; FP: False positive; FN: False negative; TN: True negative; QUDUAS: quality assessment for studies of diagnostic accuracy.
Diagnostic accuracy
The overall pooled sensitivity was 0.97 (95% CI: 0.93-0.99), and pooled specificity was 0.94 (95% CI: 0.85-0.98). The PLR was 15.62 (95% CI: 6.31-38.68) (Figure 1), NLR was 0.03 (95% CI: 0.01-0.08) (Figure 1), and the DOR was 507.99 (95% CI: 128.11-2014.34). The SROC curve illustrates the relationship between SEN and SPE, determining the presence of a threshold effect. Based on the bivariate approach which estimates not only the strength but also the shape of the correlation between SEN and SPE, a 95% confidence ellipse and a 95% prediction ellipse were drawn (Figure 2). The area under the SROC curve (AUC) was 0.99 (95% CI: 0.98-1.00), demonstrating the high discriminatory ability of LUS.
Figure 1.
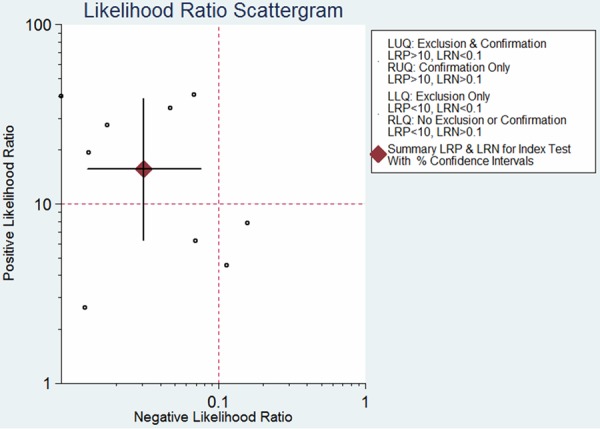
Scattergram of the positive likelihood ratio (PLR) and negative likelihood ratio (NLR).
Figure 2.
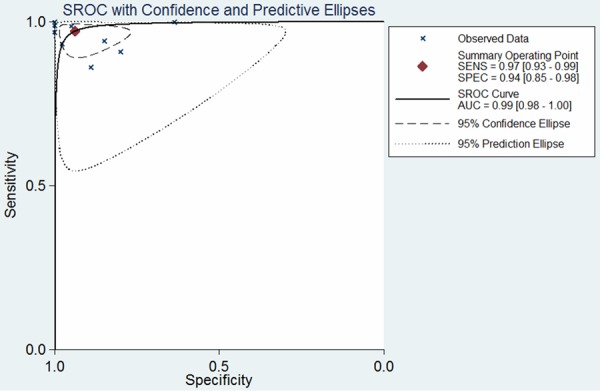
SROC curves from the bivariate model for proven and probable cases.
The I2 for the pooled DOR was 59.3%, and that was 68.6% and 71.9% for SEN and SPE, respectively, showing substantial heterogeneity among studies. Deeks’ funnel plot asymmetry test was used to evaluate the final set of studies for potential publication bias. The slope coefficient was associated with a p value of 0.78, suggesting symmetry in the data and no publication bias (Figure 3). Figure 4 shows the Fagan’s nomogram for likelihood ratios, and the results indicated that LUS for detection of pneumonia increased the post-probability to 80% when the results were positive and reduced the post-probability to 1% when the results were negative.
Figure 3.
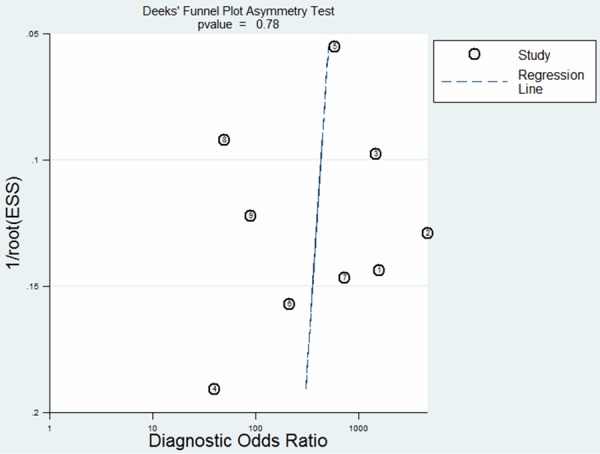
The Deek’s funnel plot for the assessment of potential publication bias.
Figure 4.
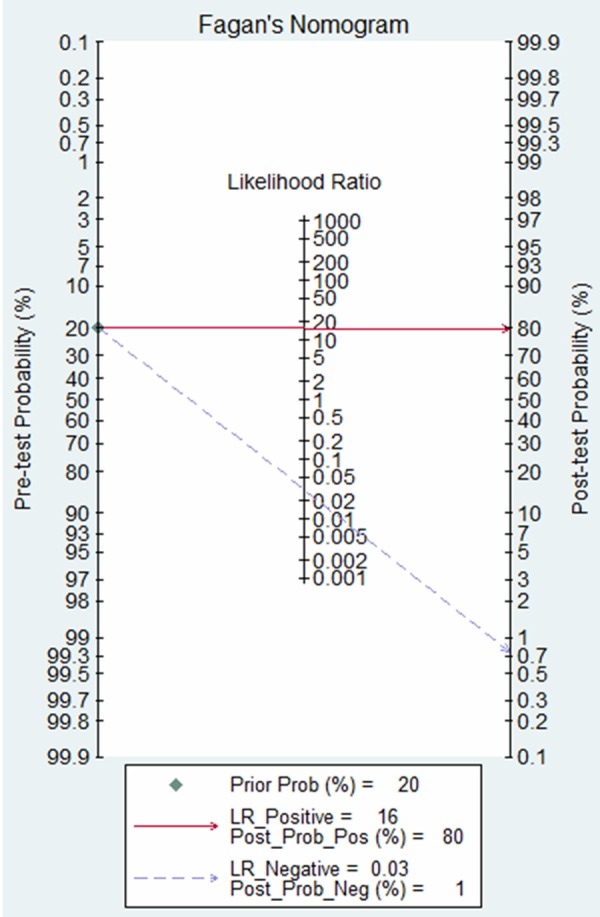
Fagan’s nomogram for calculating posttest probabilities.
Discussion
In recent years, the incidence of pneumonia experiences an upward trend, which causes significant clinical and financial burden all over the world. CXR and thoracic CT are familiar diagnosing tests, but they are irradiating and requiring transportation. LUS has long been used in pulmonary diseases. Pleural effusion, lung consolidation, interstitial syndrome, and pneumothorax are accessible to LUS. It can locate pleural effusion, assisting in thoracentesis for diagnostic or therapeutic purposes. It is also applied in airway management, diagnosis and follow-up of pneumonia, assessment of acute respiratory distress syndrome (ARDS), diagnosis and management of pneumothorax, including assessment of volume and progression [29]. Multiple studies have shown lung ultrasound imaging to be effective in diagnosing pneumonia. In 2002, Beckh S et al paid attention to the diagnostic value of lung ultrasound in pneumonia [30]. Subsequently, extensive diagnostic study had been made. The objective of the present study was to evaluate the diagnostic accuracy of lung ultrasound in pneumonia. In this study, we clarified the diagnostic accuracy of lung ultrasound for pneumonia. To our best knowledge, this is the first meta-analysis to estimate the diagnostic accuracy of lung ultrasound in pneumonia.
The summary results of these nine studies showed that lung ultrasound plays a valuable role in diagnosing pneumonia. We found a summary estimate of 97% for sensitivity and 94% for specificity, and the AUC was 0.99, indicating a high level of overall accuracy. The DOR is a single indicator of test accuracy that combines the data from sensitivity and specificity into a single number [31]. The DOR of a test is the ratio of the odds of positive test results in the patient with disease relative to the odds of positive test results in the patient without disease [32]. The value of a DOR ranges from 0 to infinity, with higher values indicating higher accuracy. In this meta-analysis, we found that the mean DOR was 507.99, indicating a significant high level of overall accuracy. Likelihood ratios are considered to be more clinically meaningful, and we also presented both PLR and NLR as our measures of diagnostic accuracy. The pooled PLR 15.62 suggests that patients with pneumonia have an approximately 16-fold higher chance of being lung ultrasound positive compared with patients without pneumonia. On the other hand, the pooled NLR 0.03 suggests that if the lung ultrasound was negative, the probability that this patient has pneumonia was 3 percent, which is low enough to rule out pneumonia. However, these data should be interpreted in parallel with clinical findings and other tests.
The recent study by Reissig et al [19] is a prospective, multicenter study with very good specificity and sensitivity by highly trained sonographers, which has suggested the use of LUS for diagnosis and close follow-up of community-acquired pneumonia. It is a simple and noninvasive method which avoids the use of ionizing radiation, making it appropriate for children, the pregnant, and young female patients. LUS has bedside availability and feasibility, which facilitates triage and immediate decision making [33]. Additionally, LUS can detect other ancillary findings that are not always obvious on the CXR [34]. It is likely that LUS may be a replacement for chest radiography for CAP [35].
Some limitations should be considered when interpreting the results. Firstly, the sample sizes of several included studies are rather small and they may not have adequate ability to assess the diagnostic accuracy. Secondly, several of the included studies only included neonates and children, who had thinner chest wall, smaller thoracic width and lung mass and smaller volume of lung parenchyma, leading to a higher positive rate [36], which may cause the heterogeneity among included studies. Thirdly, CXR is not included in the guidelines for diagnosing pneumonia, but several of the included studies only used CXR to diagnose pneumonia, which may result in misdiagnosis and cause false negative results. Finally, this meta-analysis is limited to published studies that may miss some of the gray literature. Thus, more clinical studies are needed to further investigate the diagnostic accuracy of US for pneumonia.
Conclusion
In summary, lung ultrasound plays a valuable role in the diagnosis of pneumonia, which is a promising attractive alternative to chest radiography and thoracic CT scan. The results should be interpreted in parallel with clinical findings and the results of conventional tests.
Acknowledgements
This work was supported by grants from the National Natural Science Foundation of China (Grants 81230001 and 31171103 to Fuqiang Wen, 81300032 to Yongchun Shen). The funders had no role in the study design, data collection and analysis, paper preparation, or decision to publish.
References
- 1.Moran GJ, Rothman RE, Volturo GA. Emergency management of community-acquired bacterial pneumonia: what is new since the 2007 Infectious Diseases Society of America/American Thoracic Society guidelines. Am J Emerg Med. 2013;31:602–612. doi: 10.1016/j.ajem.2012.12.002. [DOI] [PubMed] [Google Scholar]
- 2.Ewig S, Birkner N, Strauss R, Schaefer E, Pauletzki J, Bischoff H, Schraeder P, Welte T, Hoeffken G. New perspectives on community-acquired pneumonia in 388406 patients. Results from a nationwide mandatory performance measurement programme in healthcare quality. Thorax. 2009;64:1062–1069. doi: 10.1136/thx.2008.109785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arıca S, Arıca V, Dag H, Kaya A, Hatipoglu S, Fenercioglu A, Karatekin G. Serum zinc levels in children of 0-24 months diagnosed with pneumonia admitted to our clinic. Int J Clin Exp Med. 2011;4:227–233. [PMC free article] [PubMed] [Google Scholar]
- 4.File TM Jr, Marrie TJ. Burden of community-acquired pneumonia in North American adults. Postgrad Med. 2010;122:130–141. doi: 10.3810/pgm.2010.03.2130. [DOI] [PubMed] [Google Scholar]
- 5.Metlay JP, Fine MJ. Testing strategies in the initial management of patients with community-acquired pneumonia. Ann Intern Med. 2003;138:109–118. doi: 10.7326/0003-4819-138-2-200301210-00012. [DOI] [PubMed] [Google Scholar]
- 6.Brenner DJ, Hall EJ. Computed tomography—an increasing source of radiation exposure. N Engl J Med. 2007;357:2277–2284. doi: 10.1056/NEJMra072149. [DOI] [PubMed] [Google Scholar]
- 7.Warhadpande S, Martin D, Bhalla T, Rehman S, Rose M, Guinipero T, Tobias JD. Use of ultrasound to facilitate difficult lumbar puncture in the pediatric oncology population. Int J Clin Exp Med. 2013;6:149–152. [PMC free article] [PubMed] [Google Scholar]
- 8.Gardelli G, Feletti F, Nanni A, Mughetti M, Piraccini A, Zompatori M. Chest ultrasonography in the ICU. Respir Care. 2012;57:773–781. doi: 10.4187/respcare.01743. [DOI] [PubMed] [Google Scholar]
- 9.Kirkpatrick AW, Sirois M, Laupland KB, Liu D, Rowan K, Ball CG, Hameed SM, Brown R, Simons R, Dulchavsky SA, Hamiilton DR, Nicolaou S. Hand-Held thoracic sonography for detection post-traumatic pneumothoraces: the extended focused assessment with sonography for trauma (EFAST) J Trauma. 2004;57:288–295. doi: 10.1097/01.ta.0000133565.88871.e4. [DOI] [PubMed] [Google Scholar]
- 10.Riccabona M. Ultrasound of the chest in children (mediastinum excluded) Eur Radiol. 2008;18:390–399. doi: 10.1007/s00330-007-0754-3. [DOI] [PubMed] [Google Scholar]
- 11.Aghdashi M, Broofeh B, Mohammadi A. Diagnostic performances of high resolution trans-thoracic lung ultrasonography in pulmonary alveoli-interstitial involvement of rheumatoid lung disease. Int J Clin Exp Med. 2013;6:562–566. [PMC free article] [PubMed] [Google Scholar]
- 12.Whiting P, Rutjes AW, Reitsma JB, Bossuyt PM, Kleijnen J. The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol. 2003;3:25. doi: 10.1186/1471-2288-3-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Devillé WL, Buntinx F, Bouter LM, Montori VM, de Vet HC, van der Windt DA, Bezemer PD. Conducting systematic reviews of diagnostic studies: didactic guidelines. BMC Med Res Methodol. 2002;2:9. doi: 10.1186/1471-2288-2-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reistma JB, Glas AS, Rutjes AW, Scholten RJ, Bossuyt PM, Zwinderman AH. Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. J Clin Epidemiol. 2005;58:982–990. doi: 10.1016/j.jclinepi.2005.02.022. [DOI] [PubMed] [Google Scholar]
- 15.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 16.Deeks JJ. Systematic reviews in health care: Systematic reviews of evaluations of diagnostic and screening tests. BMJ. 2001;323:157–162. doi: 10.1136/bmj.323.7305.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Deeks JJ, Macaskill P, Irwig L. The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. J Clin Epidemiol. 2005;58:882–893. doi: 10.1016/j.jclinepi.2005.01.016. [DOI] [PubMed] [Google Scholar]
- 18.Fagan TJ. Letter: Nomogram for Bayes theorem. N Engl J Med. 1975;293:257. doi: 10.1056/NEJM197507312930513. [DOI] [PubMed] [Google Scholar]
- 19.Reissig A, Copetti R, Mathis G, Mempel C, Schuler A, Zechner P, Aliberti S, Neumann R, Kroegel C, Hoyer H. Lung Ultrasound in the Diagnosis and Follow-up of Community-Acquired Pneumonia. Chest. 2012;142:965–972. doi: 10.1378/chest.12-0364. [DOI] [PubMed] [Google Scholar]
- 20.Testa A, Soldati G, Copetti R, Giannuzzi R, Portale G, Gentiloni-Silveri N. Early recognition of the 2009 pandemic influenza A (H1N1) pneumonia by chest ultrasound. Crit Care. 2012;16:R30. doi: 10.1186/cc11201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cortellaro F, Colombo S, Coen D, Duca PG. Lung ultrasound is an accurate diagnostic tool for the diagnosis of pneumonia in the emergency department. Emerg Med J. 2012;29:19–23. doi: 10.1136/emj.2010.101584. [DOI] [PubMed] [Google Scholar]
- 22.Iuri D, De Candia A, Bazzocchi M. Evaluation of the lung in children with suspected pneumonia: usefulness of ultrasonography. Radiol Med. 2009;114:321–330. doi: 10.1007/s11547-008-0336-8. [DOI] [PubMed] [Google Scholar]
- 23.Shah VP, Tunik MG, Tsung JW. Prospective Evaluation of Point-of-Care Ultrasonography for the Diagnosis of Pneumonia in Children and Young Adults. JAMA Pediatr. 2013;167:119–125. doi: 10.1001/2013.jamapediatrics.107. [DOI] [PubMed] [Google Scholar]
- 24.Seif El Dien HM, Abd ElLatif DAK. The value of bedside Lung Ultrasonography in diagnosis of neonatal pneumonia. Egypt J Radiol Nucl Med. 2013;44:339–347. [Google Scholar]
- 25.Parlamento S, Copetti R, Di Bartolomeo S. Evaluation of lung ultrasound for the diagnosis of pneumonia in the ED. Am J Emerg Med. 2009;27:379–384. doi: 10.1016/j.ajem.2008.03.009. [DOI] [PubMed] [Google Scholar]
- 26.Copetti R, Cattarossi L. Ultrasound diagnosis of pneumonia in children. Radiol Med. 2008;113:190–198. doi: 10.1007/s11547-008-0247-8. [DOI] [PubMed] [Google Scholar]
- 27.Caiulo VA, Gargani L, Caiulo S, Fisicaro A, Moramarco F, Latini G, Picano E, Mele G. Lung ultrasound characteristics of community-acquired pneumonia in hospitalized children. Pediatr Pulmonol. 2013;48:280–287. doi: 10.1002/ppul.22585. [DOI] [PubMed] [Google Scholar]
- 28.Woodhead M, Blasi F, Ewig S, Huchon G, Ieven M, Ortqvist A, Schaberg T, Torres A, van der Heijden G, Verheij TJ European Respiratory Society; European Society of Clinical Microbiology and Infectious Diseases. Guidelines for the management of adult lower respiratory tract infections. Eur Respir J. 2005;26:1138–1180. doi: 10.1183/09031936.05.00055705. [DOI] [PubMed] [Google Scholar]
- 29.Lichtenstein DA, Mauriat P. Lung Ultrasound in the Critically Ill Neonate. Curr Pediatr Rev. 2012;8:217–223. doi: 10.2174/157339612802139389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Beckh S, Bolcskei PL, Lessnau KD. Real-time chest ultrasonography: a comprehensive review for the pulmonologist. Chest. 2002;122:1759–1773. doi: 10.1378/chest.122.5.1759. [DOI] [PubMed] [Google Scholar]
- 31.Glas AS, Lijmer JG, Prins MH. The diagnostic odds ratio: a single indicator of test performance. J Clin Epidemiol. 2003;56:1129–1135. doi: 10.1016/s0895-4356(03)00177-x. [DOI] [PubMed] [Google Scholar]
- 32.Westwood ME, Whiting PF, Kleijnen J. How does study quality affect the results of a diagnostic meta-analysis? BMC Med Res Methodol. 2005;5:20. doi: 10.1186/1471-2288-5-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tsung JW, Kessler DO, Shah VP. Prospective application of clinician-performed lung ultrasonography during the 2009 H1N1 influenza A pandemic: distinguishing viral from bacterial pneumonia. Crit Ultrasound J. 2012;4:16. doi: 10.1186/2036-7902-4-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Medford AR, Entwisle JJ. Indications for thoracic ultrasound in chest medicine: an observational study. Postgrad Med J. 2010;86:8–11. doi: 10.1136/pgmj.2009.081455. [DOI] [PubMed] [Google Scholar]
- 35.Medford AR. Chest Ultrasonography as a Replacement for Chest Radiography for Community-Acquired Pneumonia. Chest. 2013;143:877–878. doi: 10.1378/chest.12-2653. [DOI] [PubMed] [Google Scholar]
- 36.Petitti DB. Approaches to heterogeneity in meta-analysis. Stat Med. 2001;20:3625–3633. doi: 10.1002/sim.1091. [DOI] [PubMed] [Google Scholar]


