Abstract
Objective: To evaluate the patients’ attitudes about the devices, of which they use for long-term respiratory support at home. Method: 200 consecutive patients were questioned about the treatment and devices of respiratory support at home by face to face questionnaire. Their records were taken from the archives of Social Security Agency. Results: 123 (61.5%) of the patients were men and 77 (38.5%) were women. The mean age was 65.8 ± 11.9 (15-92) years. The most frequently prescribed device was oxygen concentrator and BIPAP was the one that follows. The most common indications were hypoxic and hypercapnic respiratory failure due to COPD. The devices were prescribed by the state university hospitals, most commonly. The average daily oxygen usage duration was 16.3 ± 3.1 hours, the average duration was 7.4 ± 3.1 hours, for BIPAP. Twenty one (11.4%) of the patients, who were treated with LTOT, stated that they were taking oxygen less than 15 hours a day. Higher education levels of the patients was correlated with the higher rates of visiting the companies - that they bought the devices- both for information about and control of the devices (p=0.002). The rate of visiting companies/firms was significantly higher in patients, who use BIPAP and respiratory support combined with it (p=0.010). Twenty three (47.9%) of the 48 patients, who notified that their devices were impaired, waited for repairment by the firm, 20 (41.6%) investigated special repair facilities and the rest (10.5%) rented a new device. Conclusion: Effective and continuous technical maintenance support must be provided to the patients, who are treated with long-term respiratory support at home.
Keywords: Oxygen concentrators, noninvasive mechanical ventilation
Introduction
The usage of Long-Term Oxygen Therapy (LTOT) and Non-Invasive Mechanical Ventilation (NIMV) devices at home, for chronic respiratory diseases particularly for chronic obstructive pulmonary disease (COPD), is widespread due to the increase in elderly population. It is proposed that these treatment modalities have brought a large burden to the health care systems. In USA, it was reported that the cost of medical care of approximately 1 million patients treated with LTOT have been reported to exceed $2 billion per year [1,2]. Some studies reported that the addition of NIMV to the oxygen therapy at home for hypercapnic respiratory failure due to COPD, does not increase the cost, when compared with the oxygen treatment alone [3].
The patient’s adaptation and adherence has a special importance in the use of home respiratory support devices.
The primary factors that affect the adaptation of the patients to the LTOT are regular follow-up and communication between physician and patient [4]. Also, a well-organized home-care program increases the adaptation [5]. In this study, the attitudes of patients about their home respiratory support devices and their methods in care of these devices are evaluated, so patients’ adherence to the therapy and the device is indirectly evaluated.
Materials and method
The records of 200 consecutive patients, who were treated by home LTOT and respiratory support therapies, were reached from the Social Security Agency. Between January and May 2010, we interviewed with the patients face to face manner. The interview was performed by the physicians, who carried out the study. During the interview; the patient’s demographic data (age, gender, occupation, educational background), type of respiratory support device that used at home, indication of the prescribed device, the institution that device was prescribed, smoking status, smoking status in the patient’s room were questioned. About the device, if it’s first hand or not, do patients visit the device company regularly or not, whether if its controls are done regularly or not, some parts regularly changed or not, oxygen concentrator components and BIBAP’s maintenance procedure, whether the device got malfunction or not, what kind of attitude taken when the device got malfunction, and what was done for repairment were asked. In addition, by calling the companies that sell the devices, frequently seen device malfunctions, home service availabilities and if the patients were informed about the use of the device were questioned. Frequency and descriptive analysis of data were performed with SPSS 13.0 statistical program. Chi-square test was used in differential analysis of non-parametric data. p<0.05 was accepted as statistical significance.
Results
123 (61.5%) of the patients were men and 77 (38.5%) were women. According to their educational status it was seen that, high school graduates were most frequent with 65 patients (32.5%) and primary school graduates (48 patients, 24.0%) and patients who are illiterate (34 patients, 16.9%) were following. According to the professional distribution, retirees took first place (103 patients, 51.5%) and housewives took the second place (57 patients, 28.5%). Mean age of the patients was 65.8 ± 11.9 (15-92). Women’s mean age was 66.9 ± 13.2, while those of men’s was 65.1 ± 11.0 (p>0.05). 10% (12 patients) were still smoking and 12 patients (6%) reported smokers in their rooms. Device types, indications, information about devices are shown in Table 1.
Table 1.
Device types, indications and device-related attitudes of the patients
| Number of patients | Percentage | |
|---|---|---|
| Type of the device | ||
| Oxygen concentrator | 85 | 42.5 |
| Oxygen concentrator + nebulizer | 31 | 15.5 |
| Oxygen concentrator + bilevel positive airway pressure | 46 | 23.0 |
| Bilevel positive airway pressure + nebulizer | 19 | 9.5 |
| Others (homecare Ventilator + concentrator, oxygen tube + BIPAP, Liquid oxygen, etc) | 19 | 9.5 |
| Indications | ||
| Type 1 respiratory insufficiency (COPD) | 93 | 46.5 |
| Type 2 respiratory insufficiency (COPD) | 54 | 27.0 |
| Type 2 respiratory insufficiency | 27 | 13.5 |
| COPD + OSAS | 13 | 6.5 |
| Others (OSAS, malignancy, etc) | 13 | 6.5 |
| Institution | ||
| State University | 113 | 56.5 |
| Research Hospitals of Ministry of Health | 57 | 28.5 |
| Others (private hospital, etc) | 30 | 15.0 |
| First hand oxygen concentrator | ||
| Yes | 180 | 90.0 |
| No use | 16 | 8.0 |
| No | 4 | 2.0 |
| First hand bilevel positive airway pressure | ||
| No use | 130 | 65.0 |
| Yes | 66 | 33.0 |
| No | 4 | 2.0 |
| Regular visits to firm | ||
| Yes | 81 | 40.5 |
| No | 119 | 59.5 |
| Regular control | ||
| Yes | 184 | 92.0 |
| No | 16 | 8.0 |
| Regular change (some parts) | ||
| Yes | 143 | 71.5 |
| No | 57 | 28.5 |
| Maintenance of oxygen devices | ||
| Water cape, cannula, filter trimonthly | 113 | 56.5 |
| No response/Not know | 76 | 38.0 |
| Others (filter weekly, Cannula monthly, etc) | 11 | 5.5 |
| Maintenance of positive pressure devices | ||
| No use/Not know | 157 | 78.5 |
| Air canal, mask annual | 25 | 12.5 |
| Others (mask, filter weekly) | 18 | 9.5 |
| Malfunction of device | ||
| Yes | 48 | 24.0 |
| No | 152 | 76.0 |
The most commonly prescribed device was the oxygen concentrator and then was BIPAP. The most common indication was hypoxic and hypercapnic respiratory failure due to the COPD. Most commonly, the devices were prescribed by the state university hospitals. A large proportion of patients reported that the oxygen concentrators and BIPAP devices were first hand-held. More than half of the patients were not regularly going to the companies that they bought the devices from. Most of the patients were making check of their devices regularly and making replacements of parts on a regular basis already. Most of the patients answered that, the parts of concentrator, which are water container, cannula and filter, had to be changed every three months. More than one-third (25/70) of those who used BIPAP, reported that hose and mask should change once a year, the less percentage of group (18/70) stated to change mask and filter once a week and the rest stated that they had no information. ¼ of all patients reported that, their devices had malfunction. Patients’ duration of device use was 32.4 ± 30.7 months, BIPAP duration of use was 26.1 ± 19.1 months. The average daily duration of oxygen therapy was 16.3 ± 3.1 hours and for BIPAP it was 7.4 ± 3.1 hours. 21 (11.4%) of the patients treated with LTOT, stated that they received less than 15 hours of oxygen per day. The connection between the educational background of the patients and regular visit to device selling firms was shown on Figure 1. When the patients’ level of education increase, the level of visiting device companies also increase (p=0.002). The relationship between the prescribed device and frequency of visiting the companies is summarized in Figure 2.
Figure 1.
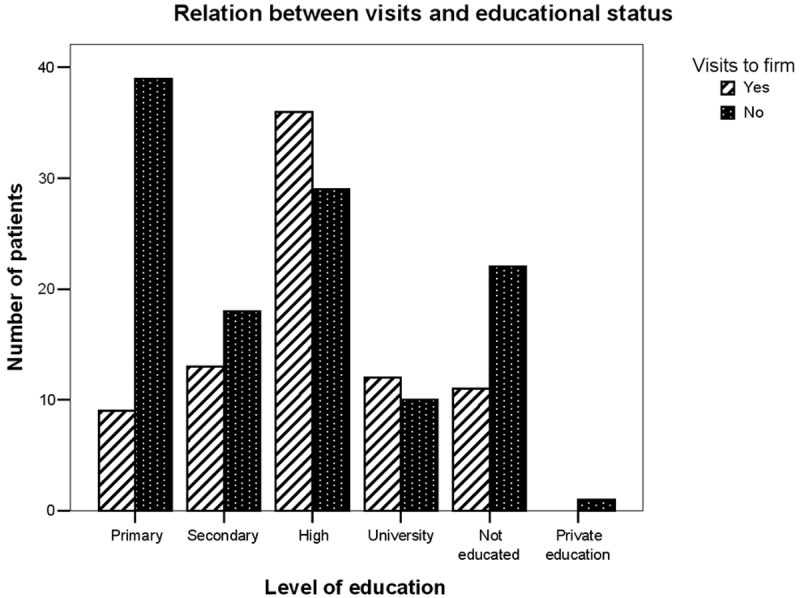
Firm visiting condition according to the educational background.
Figure 2.
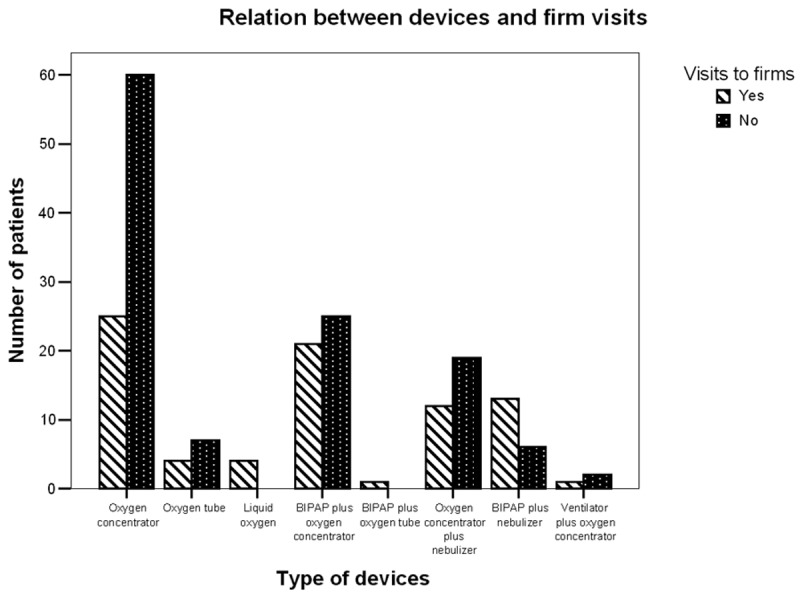
Firm visiting condition according to the device type.
The company visiting rate of BIPAP users was greater. 45.7% (21/46) of patients using oxygen concentrators with BIPAP and 68.4% (13/19) of patients using the nebulizer with BIPAP had visited the company (p=0.010). 48 patients had malfunction in their devices and 23 of them (47.9%) had to wait for repairment. 20 of them (41.6%) investigated special repair facilities and the rest (10.5%) chose to rent a new device. The reason of control of devices and the results were shown in Table 2.
Table 2.
Reasons for maintenance/change of devices
| Maintenance/change | Number of patients | Percent |
|---|---|---|
| No control | 96 | 48.0 |
| The compressor of oxygen concentrator/Filter change | 44 | 22.0 |
| The compressor of oxygen concentrator | 20 | 10.0 |
| Filter change | 11 | 5.5 |
| The compressor of oxygen concentrator/Filter change + damage | 7 | 3.5 |
| BIPAP malfunction | 6 | 3.0 |
| Others (BIPAP calibration, Air tube problem, etc) | 16 | 8.0 |
The most common problem in the maintenance of device was the necessity of changing oxygen compressor and filter. BIPAP-related issues were observed less frequently.
Discussion
Type of respiratory support devices used at home, varies between countries. This difference has been observed especially in the most commonly used oxygen delivery systems. For instance, gaseous oxygen systems (oxygen cylinders) give their place to liquid oxygen and oxygen concentrators because of their heavy weights and the risk of explosion [6]. In some other studies, it is admitted that, because of the noise and power consumption of oxygen concentrators, liquid oxygen systems are preferred [7,8]. In Italy, while liquid gas is the most common preferred system because of increasing the patient’s adherence and provides the ability to move, the gaseous oxygen is only used in temporary situations like fatal patients or exacerbations of acute bronchitis. The oxygen concentrators are prescribed less frequently [9]. It is observed in our study that, the oxygen concentrators were used in almost all the patients and gaseous and liquid oxygen delivery systems aren’t preferred.
In our study, among the institutions that physicians who may prescribe the oxygen treatment working, the university hospitals took the 1st place, research hospitals of the Ministry of Health took the 2nd place. It is observed that; in Denmark, provided to apply the criteria of LTOT, the prescribing right was given to the general practitioner, contrarily in our country, the LTOT decision is given and prescribed by specialists, who are working for advanced research institutions, at most [10]. Although there are more patient admissions to hospitals of Ministry of Health authorized to prescribe the LTOT, it is interesting that more patients are prescribed for LTOT from university hospitals pointing that the approach to LTOT has to be improved in our country.
It is still a problem that LTOT patients may continue smoking which may cause fire and explosion accidents while lighting a cigarette under oxygen inhalation [11]. In a study done in Denmark, it is observed that, among the patients who use LTOT, smoking rates change between 8-41% and it is offered to activate the smoking cessation program by checking routinely carboxyhemoglobin levels of patients while prescribing the device [10]. In our study, 10% of the patients were smokers and 6% of the patients stated that it is smoked in the places they live in. This is also suggesting that, for patients who take LTOT at home, an effective and continuous pulmonary rehabilitation is necessary. In our study, as observed in the other international studies, the most common indication to use LTOT and other respiratory support devices at home is respiratory insufficiency due to COPD and the average duration of oxygen usage was over 15 hours per day, in accordance with the literature. In the previous studies, it is stated that, short daily oxygen usage recommendation by the physician and lack of explanation of the importance of the duration prevents the benefits of LTOT [4,12]. It is observed in a study that, 36% of patients do not take oxygen in optimal duration [13]. In another study done by Kurtar and friends, it was observed that, LTOT was used in rate of 29% effectively. In the same study, the reasons for not using LTOT effectively were found as; lack of the need felt by the patient for LTOT, power consumption and noise of the device, and lack of education about the therapy [14]. In our study, the oxygen use in 11.4% of the patients was less than 15 hours daily.
More than 60% of the patients, who use LTOT, replied about component replacement and cleaning of the equipment. Considering the fact that filter cleaning and changing periods of different device types are variable we accepted that responding patients were conscious in terms of maintenance. Forty three (61%) of 70 patients, who use BIPAP, also responded about the care of the device. In our study, we should have investigated more about the relationship between social and demographic factors and the interest of patients on maintenance of the device they use. There is also a lack of information in our study, if the patients had any help from internet resources about maintenance of their devices. However, a valuable information from our study was, with increasing patient educational level, the rate of company visit for the aim of information or maintenance is also increasing. The company visiting rate of the patients, who use BIPAP and respiratory support combined with it, was also significantly grater. In the technical maintenance programs that applied in some parts of the European countries, technical and paramedical staff serves at home. The task of these teams is to establish the devices at home, in accordance with the requirements of the prescription, and to make correspondence with social security institutions. They can train the patient and their relatives about the use of mask and operation of the device. In case of device failure, they can offer 24 hours of service and technicians and nurses are able to check the compliance with device regularly [15]. In our study, it was responded that, approximately half of the patients waited for the repair for malfunctioning equipment. The remaining group searched for private repair facilities or rented a new device.
Conclusion
The questionnaire answers in our study show that, new studies are needed in which patients receiving long term respiratory support at home may express their expectations from physicians, nurses and device maintenance companies.
References
- 1.Dunne PJ. The demographics and economics of long-term oxygen therapy. Respir Care. 2000;45:223–228. [PubMed] [Google Scholar]
- 2.O'Donohue WJ Jr, Plummer AL. Magnitude of usage and cost of home oxygen therapy in the United States. Chest. 1995;107:301–302. doi: 10.1378/chest.107.2.301. [DOI] [PubMed] [Google Scholar]
- 3.Clini EM, Magni G, Crisafulli E, Viaggi S, Ambrosino N. Home Non-Invasive Mechanical Ventilation and Long-Term Oxygen Therapy in Stable Hypercapnic Chronic Obstructive Pulmonary Disease Patients: Comparison of Costs. Respiration. 2009;77:44–50. doi: 10.1159/000127410. [DOI] [PubMed] [Google Scholar]
- 4.Howard P, Waterhouse JC, Billings CG. Compliance with long-term oxygen therapy by concentrator. Eur Respir J. 1992;5:128–129. [PubMed] [Google Scholar]
- 5.Rizzi M, Grassi M, Pecis M, Andreoli A, Taurino AE, Sergi M, Fanfulla F. A specific home care program improves the survival of patients with chronic obstructive pulmonary disease receiving long term oxygen therapy. Arch Phys Med Rehabil. 2009;90:395–401. doi: 10.1016/j.apmr.2008.08.223. [DOI] [PubMed] [Google Scholar]
- 6.Kampelmacher MJ, van Kestern RG, Alsbach GP, Melissant CF, Wynne HJ, Douze JM, Lammers JW. Characteristics and complaints of patients prescribed longterm oxygen therapy in the Netherlands. Respir Med. 1998;92:70–75. doi: 10.1016/s0954-6111(98)90035-x. [DOI] [PubMed] [Google Scholar]
- 7.Nasiłowski J, Przybyłowski T, Klimiuk J, Leśkow A, Orska K, Chazan R. The effects of frequent nurse visits on patient’s compliance with long-term oxygen therapy (LTOT). A 14-month follow-up. Pneumonol Alergol Pol. 2009;77:363–370. [PubMed] [Google Scholar]
- 8.Katsenos S, Charisis A, Daskalopoulos G, Constantopoulos SH, Vassiliou MP. Long-term oxygen therapy in chronic obstructive pulmonary disease: the use of concentrators and liquid oxygen systems in north-western Greece. Respiration. 2006;73:777–782. doi: 10.1159/000094393. [DOI] [PubMed] [Google Scholar]
- 9.Neri M, Melani AS, Miorelli AM, Zanchetta D, Bertocco E, Cinti C, Canessa PA, Sestini P Educational Study Group of the Italian Association of Hospital Pulmonologists (AIPO) Long-term oxygen therapy in chronic respiratory failure: a Multicenter Italian Study on Oxygen Therapy Adherence (MISOTA) Respir Med. 2006;100:795–806. doi: 10.1016/j.rmed.2005.09.018. [DOI] [PubMed] [Google Scholar]
- 10.Ringbaek TJ, Lange P, Viskum K. Geographic Variation in Long-term Oxygen Therapy in Denmark: Factors Related to Adherence to Guidelines for Long-term Oxygen Therapy. Chest. 2001;119:1711–1716. doi: 10.1378/chest.119.6.1711. [DOI] [PubMed] [Google Scholar]
- 11.West GA, Primeau P. Non-medical hazards of long-term oxygen therapy. Respir Care. 1983;28:906–912. [PubMed] [Google Scholar]
- 12.Granados A, Escarrabill J, Borras JM, Rodriguez-Roisin R. The importance of process variables analysis in assessment of long-term oxygen therapy by concentrator. Respir Med. 1997;91:89–93. doi: 10.1016/s0954-6111(97)90073-1. [DOI] [PubMed] [Google Scholar]
- 13.Walshaw MJ, Lim R, Evans CC, Hind CR. Factors influencing compliance in patients using oxygen concentrators for long-term home oxygen therapy. Respir Med. 1990;84:331–333. doi: 10.1016/s0954-6111(08)80062-5. [DOI] [PubMed] [Google Scholar]
- 14.Kurtar NP, Uçan ES, Şahbaz S, Ellidokuz H, Çımrın AH, Kurtar E, İtil O, Akkoçlu A. Uzun Süreli Oksijen Tedavisinin Etkinliği ve Hasta Uyumu. Türk Toraks Dergisi. 2007;8:163–169. [Google Scholar]
- 15.Leger P, Laier-Groeneveld G. Infrastructure, funding and follow-up in a programme of noninvasive ventilation. Eur Respir J. 2002;20:1573–78. doi: 10.1183/09031936.02.00405802. [DOI] [PubMed] [Google Scholar]


