Abstract
Bizarre parosteal osteochondromatous proliferation (BPOP; also called Nora’s lesion) is a benign surface osteocartilaginous lesion, which is infrequently reported in world literature. The condition is classically described in the short tubular bones of hands and feet in the second and third decades of life. We present a case report of BPOP of the middle phalanx of middle finger in a 4-year-old girl. The child underwent a wide excision and remained asymptomatic at 2.5 years of follow-up. Our case report highlights the importance of suspecting Nora’s lesion in a child. It also helps in delineating a differential diagnosis and discusses the management principles of this rare osteocartilaginous lesion.
Background
Bizarre parosteal osteochondromatous proliferation (BPOP; also called Nora’s lesion) is a benign surface osteocartilaginous lesion, which is infrequently reported in world literature.1 The condition is classically described in the hands followed by the feet, long bones and the skull.2 The importance of the lesion lies in its clinical and pathological differentiation from malignant lesions particularly osteosarcoma in children and chondrosarcoma in adults. The lesion is described to have a 20–50% local recurrence rate.3 We present a case report of BPOP of the middle phalanx of middle finger in a 4-year-old girl. The importance of the case lies in the fact that most phalangeal lesions in the literature have been described in adults and occurrence of phalangeal BPOP is rare in the paediatric age group.
Case presentation
A 4-year-old girl presented with pain and swelling over the middle finger of the right dominant hand for the last 5 months. The swelling had increased in size over the past 2 months. The pain was mild to moderate in intensity with no particular relieving or exaggerating factors. There was no history of injury or fever. There was no history of any other swellings/lumps in the body. On clinical examination, a 2 cm×3 cm swelling was palpable on the radial aspect of the middle finger. The swelling was arising from the lateral aspect of the middle phalanx and was bony hard in consistency. It was non-tender but the overlying skin was warm on touch with few dilated veins. The movements of the metacarpophalangeal and the proximal and distal interphalangeal joints were preserved. There was no distal neurovascular deficit in the finger. Her general physical and systemic examinations were normal.
Investigations
Radiographs (anteroposterior and lateral views) of the hand revealed an osseous lesion over the lateral border of the middle phalanx. The lesion was calcified with some periosteal reaction. The underlying cortex of the bone appeared slightly irregular; however, there was no definite line of cleavage identified between it and the neighbouring parent bone (figure 1A,B). MRI of the finger was performed and it showed a well-defined rounded nodular lesion lying in relation to the anterolateral aspect of the base of the middle phalanx of the right middle finger. This lesion was around 2 cm in diameter. It exhibited a well-defined contour and had homogenous signal intensity in all sequences. The lesion was of muscle intense pattern on T1-weighted images and moderately hyperintense on T2-weighted images (figure 2). It was seen to be closely related to the volar and lateral aspect of the phalanx, causing some cortical erosion without significant marrow oedema or medullary bone invasion. The lesion was not invading the nearby joints or soft tissues. A clinicoradiological diagnosis of osteochondroma of the middle phalanx of the right middle finger was made.
Figure 1.
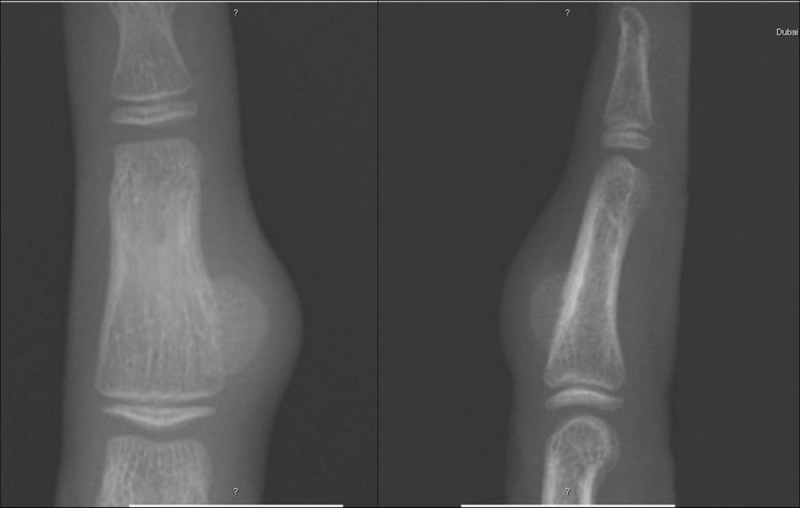
Radiograph of the hand (anteroposterior and lateral views) showing a cortical-based calcified excrescence over the middle phalanx of the middle finger.
Figure 2.
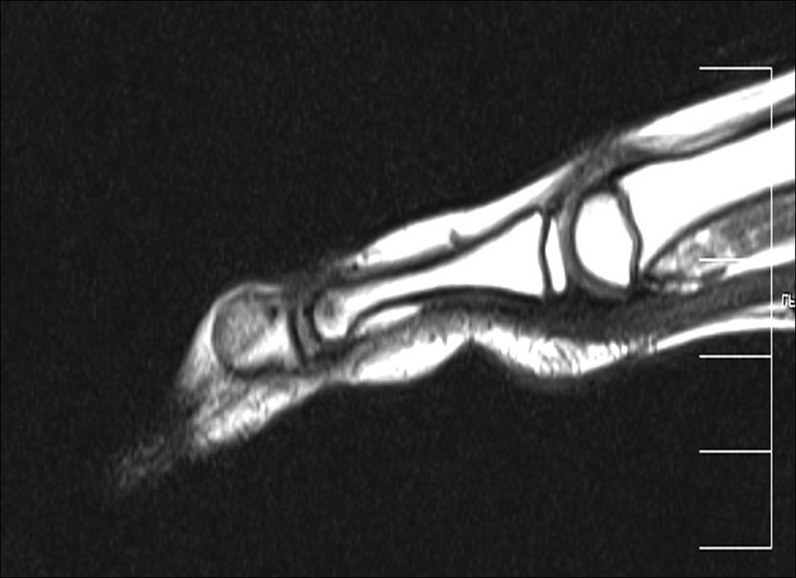
T1-weighted MRI (sagittal) showing a low-signal lesion extending from the middle phalanx. There is normal signal intensity of the cortex and the bone marrow of the underlying bone.
Differential diagnosis
Osteochondoma
BPOP
Turret exostosis
Florid reactive periostitis
Juxtaphyseal osteosarcoma
Treatment
The patient was taken up for excision of the lesion under general anaesthesia. The lesion was accessed through a direct lateral incision over the swelling. The swelling was bluish in colour with no areas of necrosis or degeneration. A wide excision of the lesion was performed. The excised specimen was sent for histopathology.
Outcome and follow-up
Histopathology of the specimen revealed a hypercellular cartilaginous cap with underlying bone trabeculae and intertrabecular fibroblastic proliferation. Higher magnification showed a hypercellular cartilage with groups of enlarged, binucleated and bizarre chondrocytes and areas of calcification in the cartilaginous cap (figure 3A,B). There was no evidence of round cells or spindle cells in the matrix. There was no atypia. A clinicopathological diagnosis of Nora's lesion of bone was made. The finger was immobilised in a below elbow plaster slab for 3 weeks followed by mobilisation. The patient was followed up on a regular basis. She had normal joint movements with no recurrence at the end of 2.5 years of follow-up.
Figure 3.
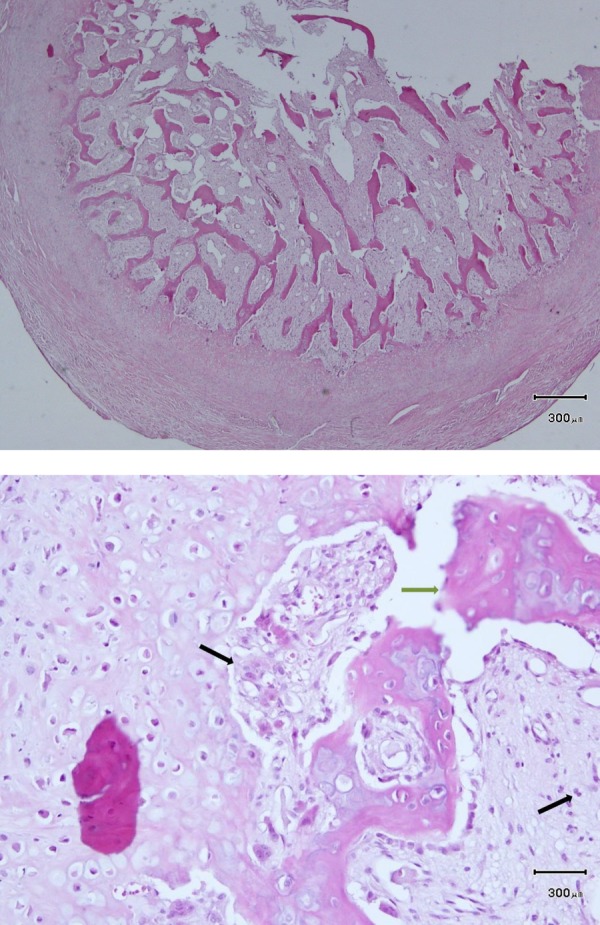
(A) Photomicrographs showing a hypercellular cartilaginous cap with underlying bone trabeculae and intertrabecular fibroblastic proliferation (H&E ×100). (B) A higher magnification photomicrograph showing hypercellular cartilage and areas of calcification in the cartilaginous cap (H&E ×400).
Discussion
BPOP was first described by Nora and colleagues. They reported 35 cases of what they described as ‘peripheral skeletal osteochondromatous tumefactions’, which were histologically and radiologically distinctive.4 It is a benign lesion with atypical microscopic features and a tendency to recur. Histologically, the lesion is characterised by an exophytic outgrowth from the cortical surface that consists of a mixture of bone, cartilage and fibrous tissue.5 Until now, around 200 cases of Nora’s lesion have been described in the literature.
Hands are the commonest site of involvement followed by the feet and skull. The involvement of phalanges is not rare, but lesions have usually been described in the proximal phalanges.2 The clinical presentation of Nora's lesion is variable. The condition typically occurs in the second and third decades of life although cases less than 10 years of age are reported very infrequently.6 In one of the largest series of the condition with 65 patients, the average age was 33.9 years. To the best of our knowledge, the youngest patient reported in the literature was 13 months.7 The condition is characterised by rapid growth and an apparently aggressive behaviour. The symptoms are usually pain and swelling at the affected site. Our patient too had pain with rapid increase in size of the tumour. A history of trauma can be elicited in 20% of cases.8
Horiguchi et al9 believed that BPOP represents a reparative process of periosteal injury. Their analysis revealed that chondrocytes located in the cartilaginous cap expressed chondromedulin-1 whereas those near the osteocartilaginous interface of the lesion expressed vascular endothelial growth factor. This suggests that processes occurring in the cartilaginous cap of BPOP are very similar to enchondral ossification in growth plate. A cytogenetic analysis in five patients of BPOP by Nilsson et al10 revealed a balanced translocation t(1;17) (q32;q21). This was an important aberration in BPOP which determines high recurrence rates in these lesions. Radiologically, the lesion can be confused with Turret exostosis and florid reactive periostitis.2 Histologically, Turret exostosis would have a mature osteocartilaginous cap overlying a transitional area with signs of enchondral ossification and bone tissue trabeculae lined by osteoblasts without atypia whereas florid reactive periostitis would show a picture of proliferating spindle cells with minimal osteocartilaginous growth.11 The rapid onset and progress of Nora's lesion differentiates it from a florid reactive periostitis of the fingers. Yuen et al12 have hypothesised that all the three conditions could be part of a spectrum of reactive bone disorders with florid reactive periostitis representing the initial stage followed by BPOP, finally resulting in Turret exostosis. The radiological differentials also include osteochondroma and juxtaphyseal osteosarcoma. The latter two are very important to differentiate in a paediatric patient like ours. Osteochondroma rarely occurs in the phalanges and has a characteristic continuity of the medullary canal of the lesion with the parent bone.13
The treatment of Nora's lesion is a wide excision although high recurrence rates of 20–50% have been described in most studies.2–4 In a retrospective series of 22 cases of BPOP, Berber et al3 had reported a recurrence rate of 27.3%. Their treatment included excision in 17 patients, supplemented in two cases by curettage, shave excision in three, shark-bite excision in one and in one primary amputation of a toe, owing to the size of the lesion. According to Michelsen et al, although there is a cleavage plane between the lesion and host bone, it is best to excise the pseudocapsule over the lesion, any periosteal tissue beneath the lesion and to decorticate any abnormal-appearing areas in the underlying host bone. This explained the extremely low recurrence rate in a series of 10 patients with Nora's lesion of the hand.14
In summary, BPOP is a rare osteocartilaginous lesion, mainly seen in the adult population. The occurrence in children is extremely rare, and therefore there is a paucity of data on the behaviour of these bizarre lesions in immature skeleton. In view of a varied differential diagnosis and a high rate of local recurrence, an early identification and a wide excision are essential in paediatric Nora's lesions.
Learning points.
Bizarre parosteal osteochondromatous proliferation (Nora's lesion) can occur in children.
The condition needs to be differentiated from florid reactive periostitis, turret exostosis, osteochondroma and juxtaphyseal osteosarcoma.
Behaviour of these lesions in children is not known. Hence, the child has to be kept under surveillance for long term.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Soubeyrand M, De Pinieu G, Biau D, et al. Bizarre parosteal osteochondromatous proliferation (Nora's lesion): two cases. Rev Chir Orthopédique Mot 2007;93:494. [DOI] [PubMed] [Google Scholar]
- 2.Meneses MF, Unni KK, Swee RG. Bizarre parosteal osteochondromatous proliferation of bone (Nora's lesion). Am J Surg Pathol 1993;17:691–7 [DOI] [PubMed] [Google Scholar]
- 3.Berber O, Dawson-Bowling S, Jalgaonkar A, et al. Bizarre parosteal osteochondromatous proliferation of bone clinical management of a series of 22 cases. J Bone Joint Surg Br 2011;93:1118–21 [DOI] [PubMed] [Google Scholar]
- 4.Nora FE, Dahlin DC, Beabout JW. Bizarre parosteal osteochondromatous proliferations of the hands and feet. Am J Surg Pathol 1983;7:245–50 [DOI] [PubMed] [Google Scholar]
- 5.Gruber G, Giessauf C, Leithner A, et al. Bizarre parosteal osteochondromatous proliferation (Nora lesion): a report of 3 cases and a review of the literature. Can J Surg 2008;51:486. [PMC free article] [PubMed] [Google Scholar]
- 6.Kraft D, Hailer NP. [Nora's lesion at the second metacarpal bone of a twelve-year-old female]. Z Für Orthop Ihre Grenzgeb 2006;144:228. [DOI] [PubMed] [Google Scholar]
- 7.Miyajima T, Sakada T, Azuma H. Bizarre parosteal osteochondromatous proliferation in a child's hand. J Hand Surg Br Eur Vol 1997;22:472–3 [Google Scholar]
- 8.Suresh SS. Nora's lesion of the second toe. Indian J Orthop 2010;44:342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Horiguchi H, Sakane M, Matsui M, et al. Bizarre parosteal osteochondromatous proliferation (Nora's lesion) of the foot. Pathol Int 2001;51:816–23 [DOI] [PubMed] [Google Scholar]
- 10.Nilsson M, Domanski HA, Mertens F, et al. Molecular cytogenetic characterization of recurrent translocation breakpoints in bizarre parosteal osteochondromatous proliferation (Nora's lesion). Hum Pathol 2004;35:1063–9 [DOI] [PubMed] [Google Scholar]
- 11.Cañueto J, Santos-Briz Á, Yuste-Chaves M, et al. Exostosis de Turret: osteocondroma adquirido. Actas Dermo-Sifiliográficas 2011;102:474–5 [DOI] [PubMed] [Google Scholar]
- 12.Michael Yuen MB, William Orr MD. Proliferative periosteal processes of phalanges: a unitary hypothesis. Skeletal Radiol 1992;21:301–3 [DOI] [PubMed] [Google Scholar]
- 13.Davies CT. Bizarre parosteal osteochondromatous proliferation in the hand: a case report. J Bone Joint Surg Am 1985;67:648–50 [PubMed] [Google Scholar]
- 14.Michelsen H, Abramovici L, Steiner G, et al. Bizarre parosteal osteochondromatous proliferation (Nora's lesion) in the hand. J Hand Surg 2004;29:520–5 [DOI] [PubMed] [Google Scholar]


