Abstract
A 33-year-old woman with no medical history reported an acute onset of left leg and thigh swelling. A review of her medications revealed that she had started oral contraceptives 2 months previously. Ultrasonography and subsequent venography demonstrated extensive ileofemoral clot burden. Thrombolysis and thrombectomy successfully restored venous return with subsequent improvement in the leg swelling and oedema. In this case, we describe a patient presenting with extensive ileofemoral deep vein thrombosis, otherwise known as the May-Thurner syndrome.
Background
May-Thurner syndrome was first described by May and Thurner in 1957.1 It is a clinical condition characterised by abnormal positioning of the right common iliac artery such that it compresses the left common iliac vein, resulting in impeded venous return and a propensity for deep venous thrombosis (DVT). The incidence is about 20% though this is likely an underestimation as patients are often initially asymptomatic.1 2 The condition typically afflicts young-aged to middle-aged women, particularly those in the peri-partum period, or on oral contraceptives like in this patient.3 4 Patients often present with unilateral leg swelling, varicosities, venous stasis changes, along with pain and ulceration. It usually presents in the left leg, though right-sided May-Thurner syndrome has been described.5 6
Case presentation
A 33-year-old previously healthy woman presented to her general practitioner with a 1-day history of worsening left leg swelling associated with pain and tightness. The patient denied a history of recent surgery or trauma, prolonged immobilisation or smoking. She denied any recent insect or animal bites. Her medical history was only significant for gestational diabetes and two prior caesarean sections in her 20s. A review of her medications revealed that she had started oral contraceptives 2 months previously. General inspection revealed a young woman in no apparent distress with stable vital signs. The examination of the leg revealed a diffusely red, painful and grossly swollen left lower extremity with a left calf measurement 7 cm greater than that of the right leg (figure 1). Left-sided popliteal and posterior tibial pulses were slightly diminished in comparison with those of the right leg. She was administered a single dose of subcutaneous (SC) enoxaparin 80 mg in clinic and transferred to the emergency room (ER). Doppler ultrasonography revealed an acute DVT encompassing the left distal external iliac, common femoral, femoral, popliteal, posterior tibial, proximal great saphenous and peroneal veins (figures 2 and 3). Intravenous venography confirmed a large acute DVT extending from the mid left femoral vein throughout the iliac veins (figures 4 and 5). Given the considerable clot burden, we recommended an endovascular intervention. We proceeded to perform pharmacomechanical thrombolysis/thrombectomy and the patient was started on recombinant tissue plasminogen activator (figure 6). Balloon angioplasty was performed and the follow-up venography demonstrated a significant improvement with only minimal residual stenosis and no residual thrombus (figure 7). A stent was not placed at the time because the region of the suspected iliac vein compression showed no residual stenosis.
Figure 1.

Patient on initial presentation, left thigh swelling and erythema.
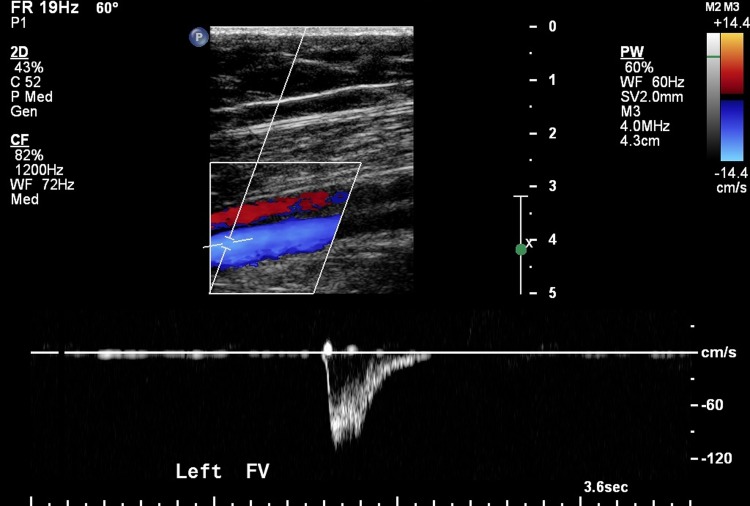
Figure 2.
Ultrasound on presentation demonstrating acute deep venous thrombosis (DVT) of the left external iliac vein.
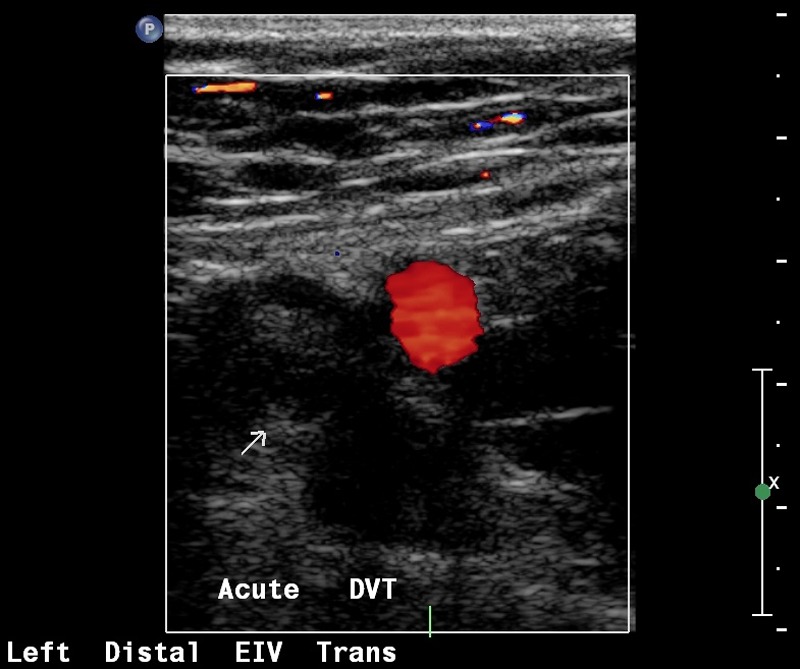
Figure 3.
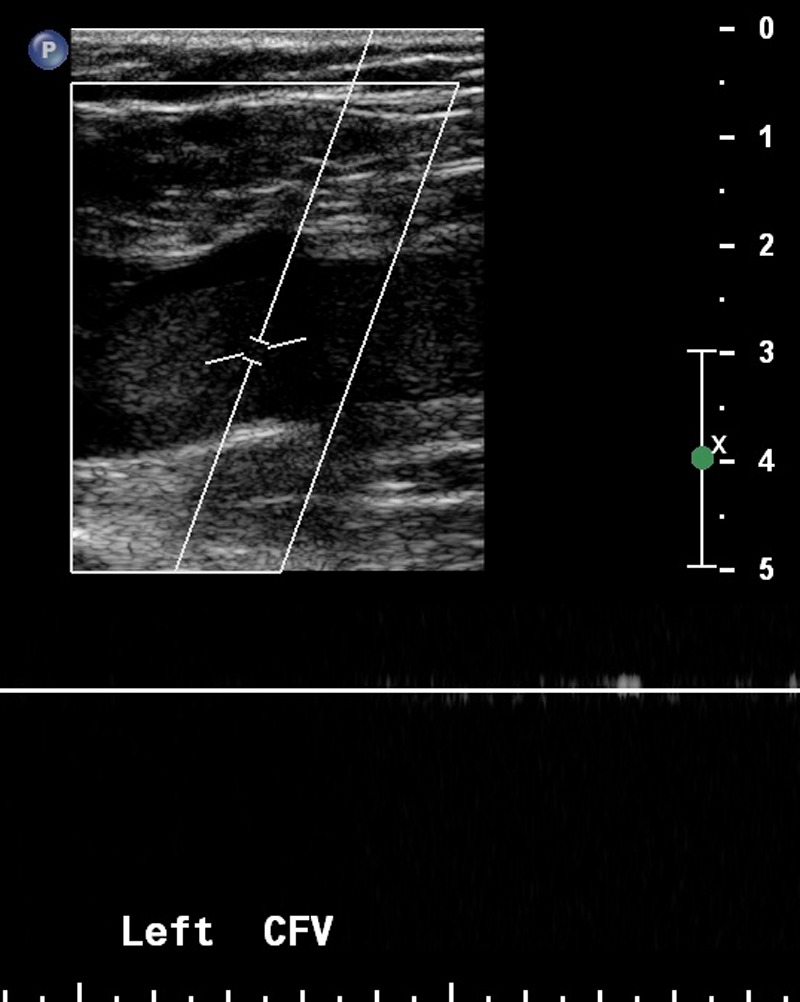
Ultrasound on presentation demonstrating an acute deep venous thrombosis (DVT) of the left common femoral vein.
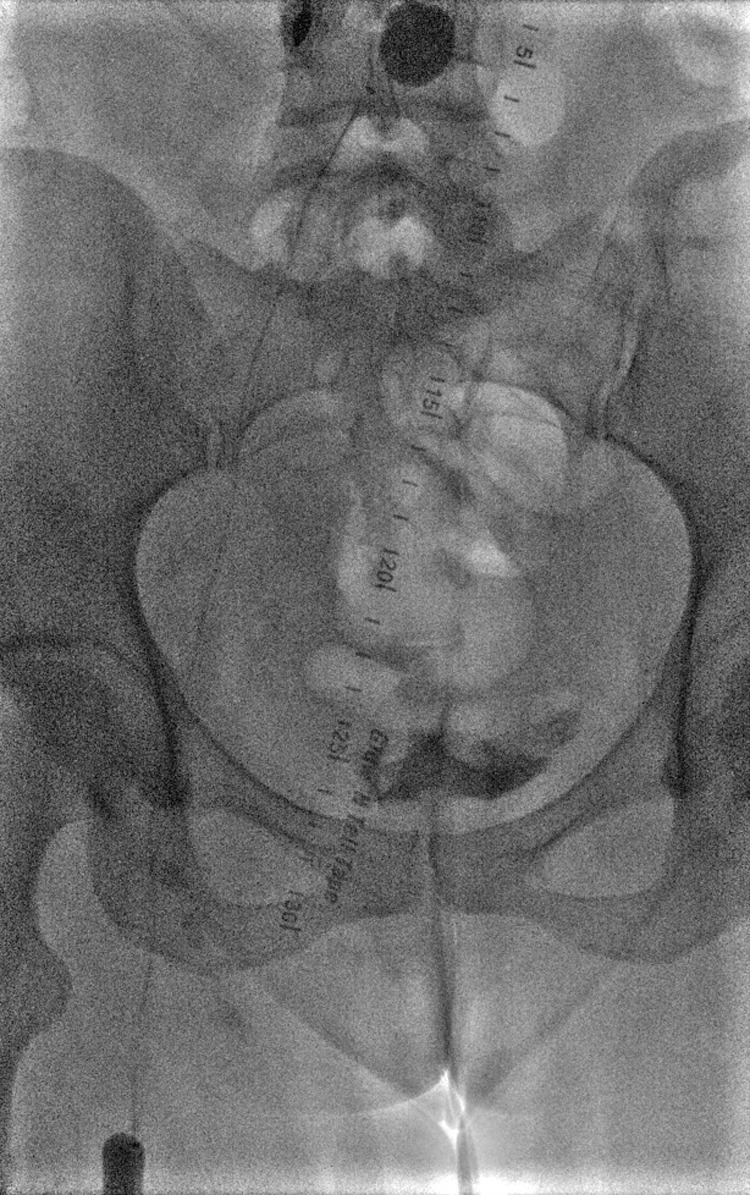
Figure 4.
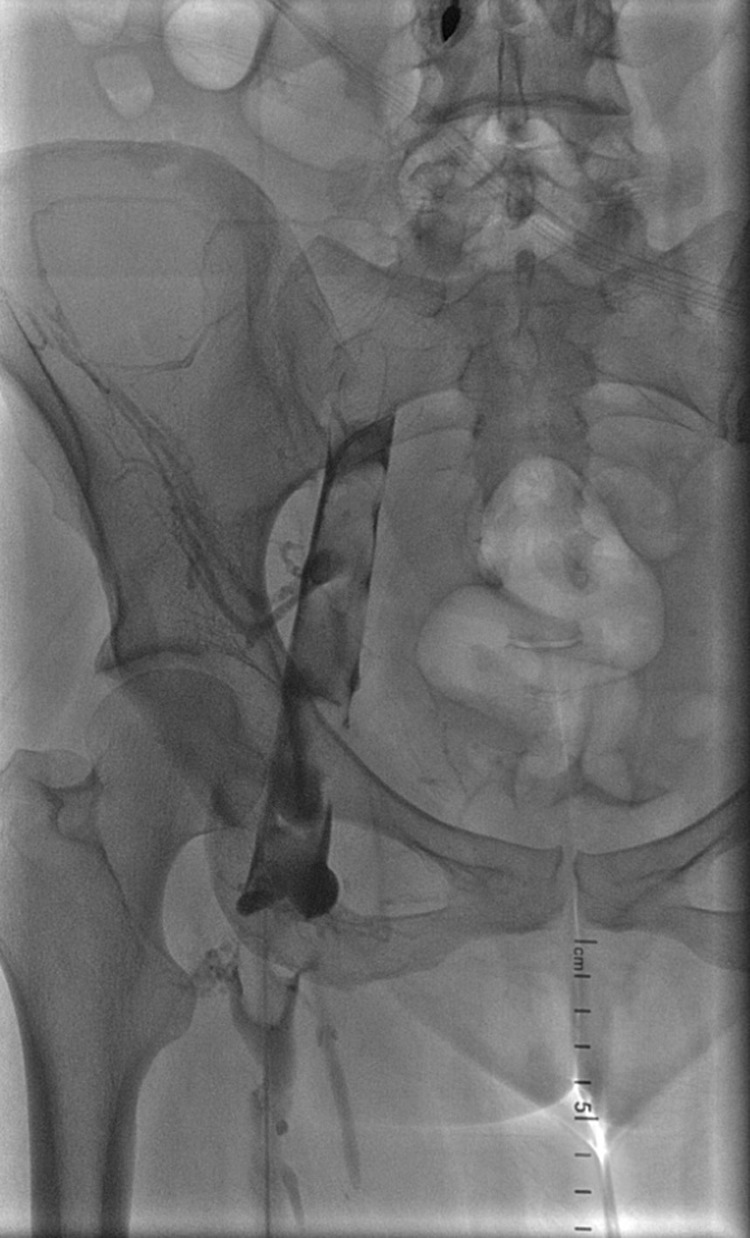
Initial venogram showing intraluminal thrombus of the left common femoral and external iliac vein.
Figure 5.
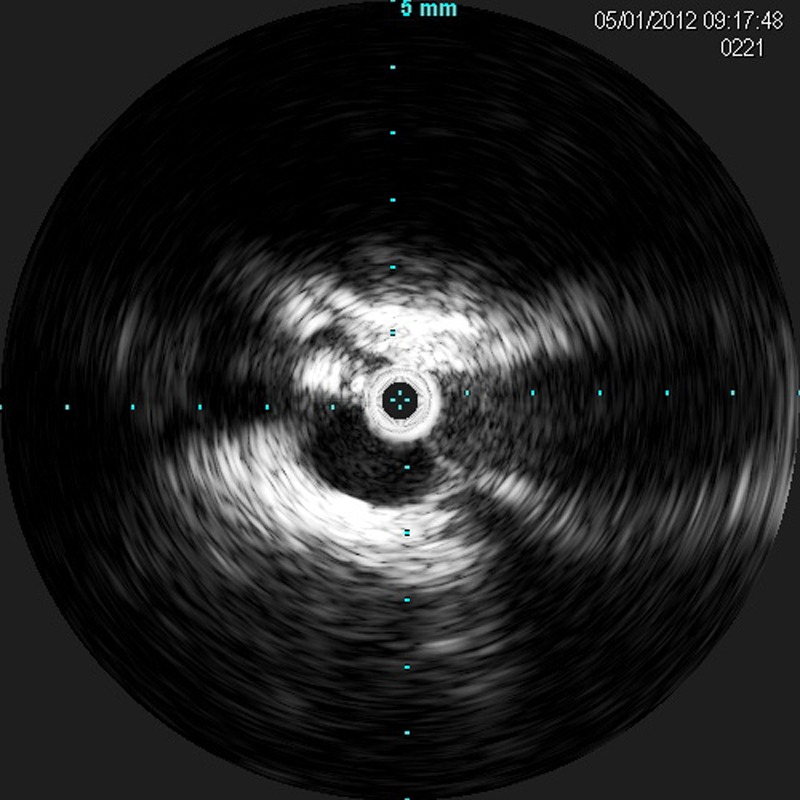
Intravascular ultrasound showing compression of the left common iliac vein by the right common iliac artery.
Figure 6.
Trellis device. Proximal and distal balloons. Tissue plasminogen activator (TPA) in between agitated with a sinusoidal rotating wire.
Figure 7.

Venogram after balloon angioplasty showing a near-complete resolution.
Treatment
Anticoagulation has been the treatment modality for DVT; however alone, it has been proven ineffective for the treatment of ileofemoral DVT in the setting of venous obstruction.7 After completion of the endovascular intervention, the patient was stared on bridging anticoagulation using low-molecular-weight heparin and warfarin. She was prescribed a 6-month course of warfarin and the oral contraceptives discontinued. She was instructed to seek an alternate form of birth control as the oral contraceptive was thought to be the most likely implicating factor.
Outcome and follow-up
The patient was followed up at 1-month, 3-month and 6-month intervals. After 6 months, she underwent a multiplanar, multisequence MRI and MR venography (MRV) of the pelvis. The distal abdominal aorta, common bilateral iliac arteries, distal inferior vena cava, bilateral common iliac and internal and external iliac veins appeared patent without evidence of any dilation or filling defects to suggest thrombi. She was found, however, to have a severely narrowed proximal left common iliac vein, which was also confirmed by angiography (figure 8). This was treated with angioplasty and placement of a stent. Subsequent venogram and venous ultrasonography demonstrated no residual thrombus (figure 9). The patient received warfarin for a total of 6 months. She is currently taking aspirin 325 mg orally daily and uses compression stockings, and is doing well.
Figure 8.
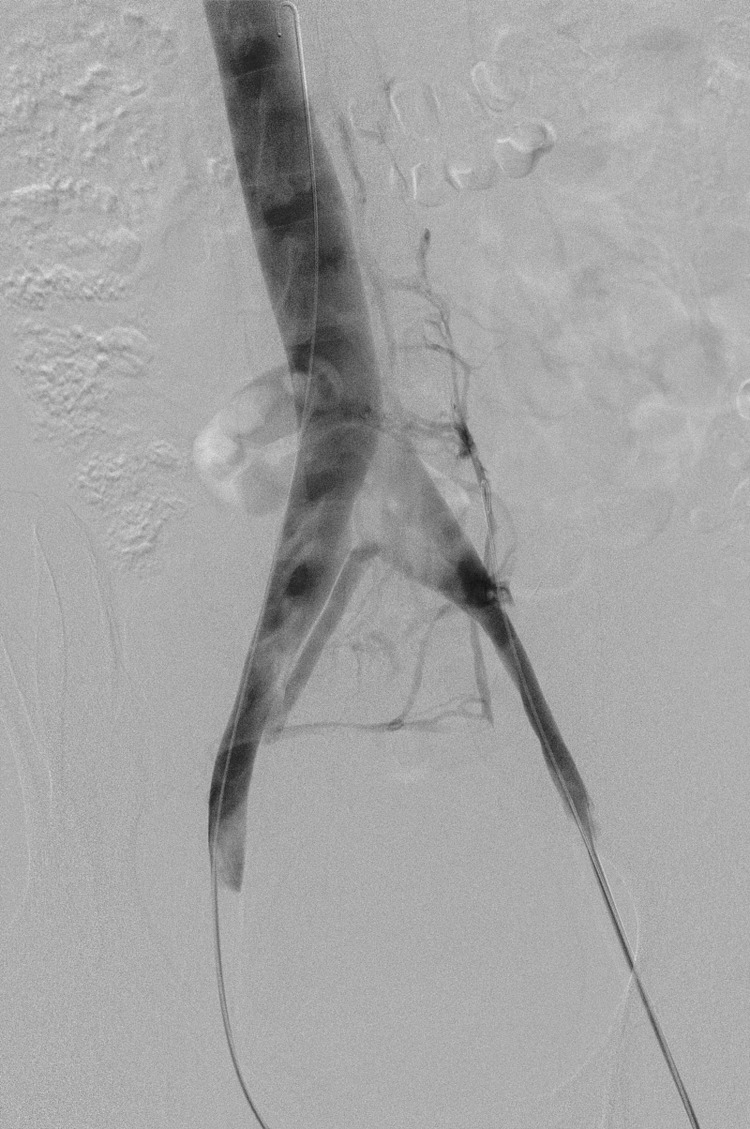
Angiography after 6 months of anticoagulation showing persistent compression with cross-pelvic collaterals.
Figure 9.
Post-treatment ultrasonography (US) showing no residual thrombus in the left femoral vein.
Discussion
The case describes a middle-aged female with May-Thurner syndrome complicated by an extensive left leg DVT temporally associated with the start of the oral contraceptives. This again illustrates the importance of eliciting a detailed medication history. She had required thrombolysis/mechanical thrombectomy along with endovascular angioplasty and stenting. This approach has previously been described in the literature and has been proven to be very efficacious.8–1,1 Catheter-directed thrombolytic therapy for acute extensive ileofemoral DVT was first reported by O'Sullivan et al.1,2 Using thrombectomy, angioplasty and stenting, AbuRahma et al9 demonstrated an 83% rate of 1-year patency.
Learning points.
The study reviews the investigations employed in evaluating the patient presenting with acute lower extremity redness and swelling.
To consider May-Thurner syndrome in the patient presenting with left-sided ileofemoral deep venous thrombosis (DVT).
To recognise the role of thrombolytic and endovascular interventional therapies as well as maintenance anticoagulation therapy in patients with acute extensive ileofemoral DVT.
Footnotes
Contributors: MEA wrote the case. SD and NR took care of the patient. ZA edited the case and performed a literature review.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.May R, Thurner J. The cause of the predominantly sinistral occurrence of thrombosis of the pelvic veins. Angiology 1957;8:419–27 [DOI] [PubMed] [Google Scholar]
- 2.Kibbe M, Ujiki M, Goodwin AL, et al. Iliac vein compression in an asymptomatic patient population. J Vasc Surg 2004;39:937–43 [DOI] [PubMed] [Google Scholar]
- 3.Vandenbroucke JP, Rosing L, Bloekmenkamp KW, et al. Oral contraceptives and the risk of venous thrombosis. N Engl J Med 2001;334:1527–35 [DOI] [PubMed] [Google Scholar]
- 4.Gherman RB, Goodwin T, Leung B, et al. Incidence, clinical characteristics and timing of objectively diagnosed venous thromboembolism during pregnancy. Obstet Gynecol 1999;94:730–4 [DOI] [PubMed] [Google Scholar]
- 5.Fretz V, Binkert CA. Compression of the inferior vena cava by the right iliac artery: a rare variant of May-Thurner syndrome. Cardiovasc Intervent Radiol 2010;33:1060–3 [DOI] [PubMed] [Google Scholar]
- 6.Abboud G, Midulla M, Lions C, et al. “Right-sided” May-Thurner syndrome. Cardiovasc Intervent Radiol 2010;33:1056–9 [DOI] [PubMed] [Google Scholar]
- 7.Krupski WC, Bass A, Dilley RB, et al. Propagation of deep venous thrombosis identified by duplex ultrasonagraphy. J Vasc Surg 1990;12:467–75 [PubMed] [Google Scholar]
- 8.Patel NH, Stookey KR, Ketchman DB, et al. Endovascular management of acute extensive ileofemoral deep venous thrombosis caused by May-Thurner syndrome. JVIR 2000;11:1297–302 [DOI] [PubMed] [Google Scholar]
- 9.AbuRahma AF, Perkins SE, Wulu JT, et al. Ileofemoral deep vein thrombosis: conventional therapy versus lysis and percutaneous transluminal angioplasty and stenting. Ann Surg 2001;233:752–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kwak HS, Han Ym, Lee YS, et al. Stents in common iliac vein obstruction with acute ipsilateral deep venous thrombosis: early and late results. J Vasc Interv Radiol 2005;16:815–22 [DOI] [PubMed] [Google Scholar]
- 11.Wells PS, Hirsh J, Anderson DR, et al. Accuracy of clinical assessment of deep-vein thrombosis. Lancet 1995;345:1326–30 [DOI] [PubMed] [Google Scholar]
- 12. doi: 10.1016/s1051-0443(07)61796-5. O'Sullivan GJ, Semba CP, Bittner CA, et al. Endovascular Management of Iliac Vein Compression (May-Thurner) Syndrome. J Vasc Interv Radiol 2000;11:823–36. [DOI] [PubMed] [Google Scholar]