Description
A 50-year-old man, a chronic alcoholic with hepatitis C virus positive status, presented with jaundice and right upper quadrant pain for 2 months. He had a history of taking antitubercular drugs for 2 years. General physical examination revealed icterus; systemic examinations were within the normal limits. His bilirubin level was 6.95 mg/dL, alkaline phosphatase 1720 U/L and rest of liver function test parameters were within the normal limits. Ultrasonography examination of the abdomen showed mild splenomegaly and haepatomegaly, gallbladder with biliary sludge, dilated intrahepatic biliary radical (IHBRD) and mural thickening in the pyloric region. Magnetic resonance computerised topography showed dilated IHBRDs, choledocolithiasis, cholelithiasis, mild haepatomegaly and minimal ascites. He was diagnosed with extrahepatic biliary obstruction by multiple stones in the gallbladder and common bile duct, and gastric outlet obstruction. Upper gastrointestinal endoscopy showed normal oesophagus, stomach showed hyperaemia and mucosal oedema at pylorus with food residue. Scope was negotiable to the first part of the duodenum, which also showed food residues, and normal second part of the duodenum. Antral biopsy was taken. On histopathology, biopsy showed intact epithelial lining with focal intestinal metaplasia. The lamina propria showed mild to moderately heavy lymphoplasmacytic cell infiltration with lamina propria fibrosis. No active inflammation or Helicobacter pylori or dysplasia was observed. In addition, there were many intensely haematoxylinophilic spherical organisms in tetrads and octets on gastric mucosa which were positive on Gram staining. These organisms had the morphology of Sarcina1–3 (figure 1A–C). No invasion of gastric mucosa was seen. A diagnosis of chronic gastritis with intestinal metaplasia with the presence of Sarcina was made.
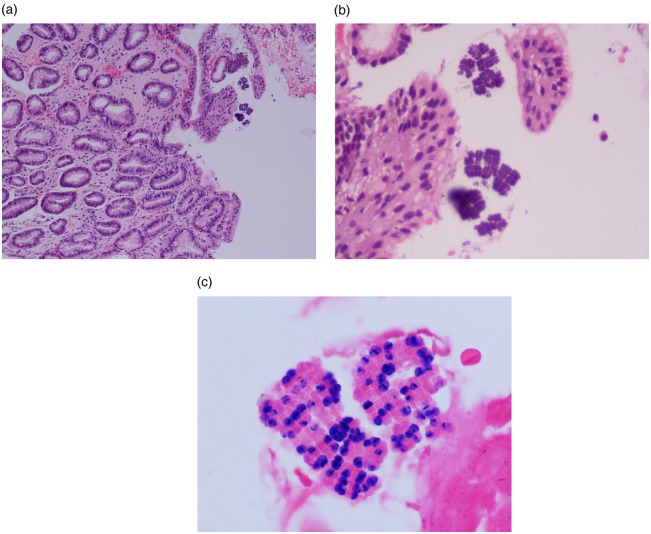
Figure 1.
(A) Low-power photomicrograph of the antral biopsy showing lamina propria inflammation with fibrosis and intact mucosal lining epithelium. There are many intensely haematoxylinophilic spherical organisms overlying the mucosa (H&E, ×250). (B) High microphotograph showing the character of those haematoxylinophilic spherical organisms having characteristic and regular tetrads and octets shapes (H&E, ×500). (C) High microphotograph showing Gram positivity of the organisms (Gram stain, ×1000).
Following the endoscopic report, he was given metronidazole (250 mg) three times daily and ciprofloxacin (250 mg) twice daily for 1 week along with sucralfate. Repeat endoscopy and gastric biopsy after the treatment showed an improvement in the gastritis status and no similar organism could be identified in the biopsy.
Learning points.
The histological features of Sarcina are singular enough that a diagnosis can be made on routine H&E staining.
Infection and colonisation of Sarcina is usually associated with functional gastric outlet obstruction and delayed gastric emptying such as occult malignancy.
The need for antibiotic treatment for Sarcina in a clinically stable patient is unclear. However, a definite endoscopic and histological improvement has been observed by treating the patient.
Footnotes
Contributors: GBL, PS and KV contributed equally in reporting and writing the paper.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Lam-Himlin D, Tsiatis AC, Montgomery E, et al. Sarcina organisms in the gastrointestinal tract: a clinicopathologic and molecular study. Am J Surg Pathol 2011;35:1700–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Canale-Parola E. Biology of the sugar fermenting sarcinae. Bacteriol Rev 1970;34:82–97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Canale-Parola E, Sneath NS, Mair ME, et al. Genus Sarcina. In: Bergey's manual of systematic bacteriology. Philadelphia: Williams & Wilkins, 1986;2:1100–3 [Google Scholar]