Abstract
A 73-year-old man was admitted with symptoms of large bowel obstruction. An emergency CT scan revealed pneumobilia and large bowel obstruction at the level of the rectosigmoid due to a 4×4 cm impacted gallstone. Flexible sigmoidoscopy confirmed the diagnosis but initial attempts to drag the stone into the rectum failed. An endoscopic mechanical lithotripter was employed to repeatedly fracture the gallstone into smaller fragments, which were passed spontaneously the next day. The patient made a complete recovery avoiding the potential dangers of surgery. This case report discusses cholecystoenteric fistula and a novel minimally invasive treatment for large bowel obstruction due to gallstones.
Background
Gallstone ileus is an unusual presentation of small bowel obstruction which is occasionally encountered in clinical practice. However, large bowel obstruction caused by a gallstone migrating through a cholecystocolonic fistula is extremely rare.
When it does occur, it is often associated with high morbidity and mortality because the usual reported treatment is open surgery with enterolithotomy, and the typical patient is elderly with significant comorbidities.
This case is important because it demonstrates that therapeutic endoscopic techniques can be applied to this unusual presentation of large bowel obstruction and provide a successful minimally invasive alternative to surgery.
Case presentation
A 73-year-old man was admitted with a 5-day history of absolute constipation, colicky lower abdominal pain, distension and vomiting. His abdomen was distended, tympanic and slightly tender in the lower quadrants and a digital rectal examination revealed an empty rectum.
There was no preceding change in bowel habit, rectal bleeding or weight loss, nor any family history of colorectal cancer.
Two years prior to presentation he suffered a complicated episode of cholecystitis with a gallbladder empyema, which subsequently perforated and was treated conservatively with antibiotics. A CT scan of his abdomen at that stage demonstrated pneumobilia and suggested a cholecystoenteric fistula; however, no surgical intervention was planned due to a low predicted risk of developing future biliary problems.
Investigations
His white cell count was elevated on admission at 14.4×109/L with a normal haemoglobin and C reactive protein. A plain abdominal radiograph showed dilated loops of small and large bowel consistent with large bowel obstruction and an incompetent ileocaecal valve (figure 1).
Figure 1.
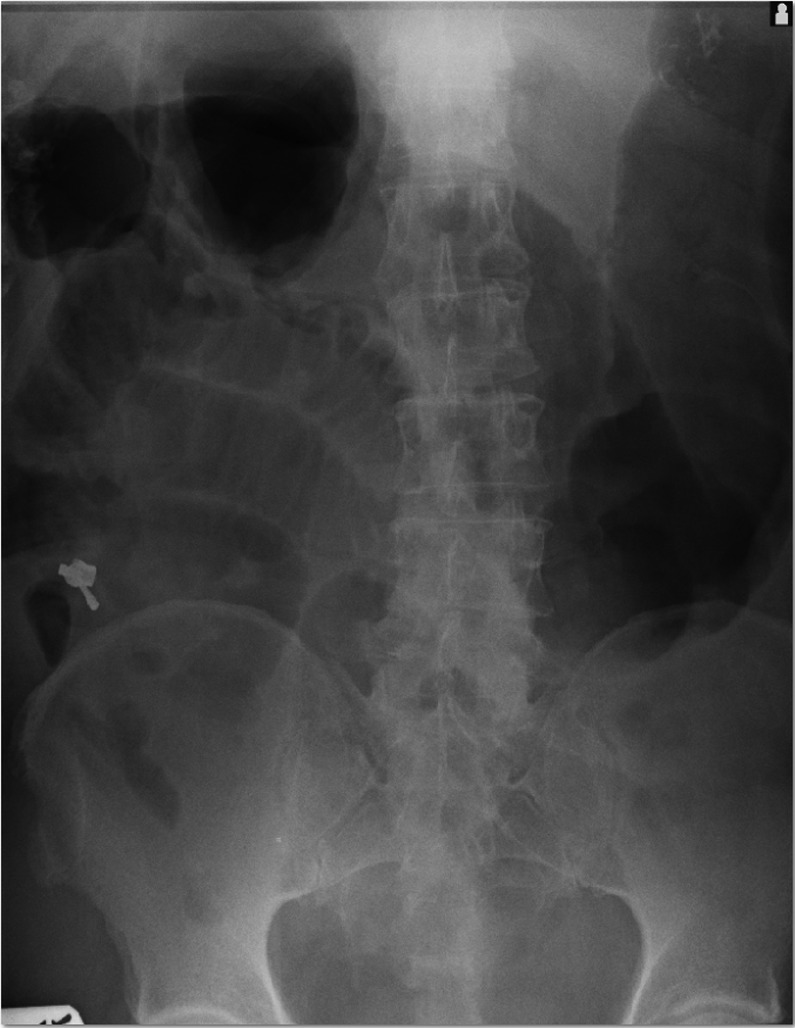
A plain abdominal radiograph showing large bowel obstruction.
A CT scan of his abdomen and pelvis confirmed a mechanical obstruction and demonstrated an obstructing 4×4 cm calculus at the rectosigmoid junction (figures 2 and 3). Several smaller calculi were noted to be lying more proximally within the colon, as well as pneumobilia.
Figure 2.

An axial CT slice demonstrating the obstructing gallstone lying within the pelvis.
Figure 3.
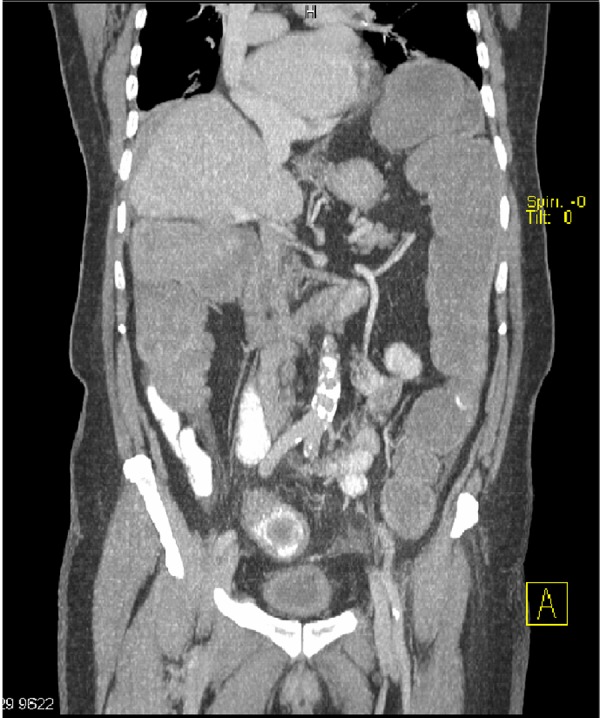
A coronal CT slice demonstrating the obstructing gallstone with more proximal calculi visible.
Treatment
The rectosigmoid junction was easily accessible endoscopically and, given the patient displayed no signs of imminent perforation, it was decided to perform a flexible sigmoidoscopy under sedation in the operating theatre. The diagnosis was visually confirmed and several attempts were made using a Dormia basket, polypectomy snare and retrieval net to manoeuvre the impacted stone distally into the rectum, all of which failed. A mechanical lithotripter was then used to repeatedly crush the stone into smaller fragments (figures 4 and 5). Such force was transmitted through the device that the chassis of the lithotripter bent slightly during the process.
Figure 4.
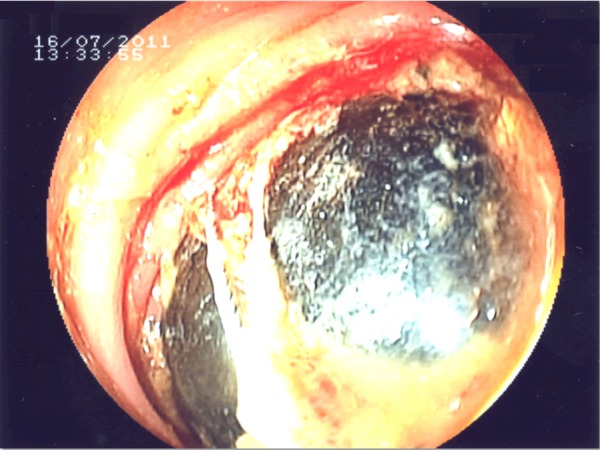
Gallstone encircled by the lithotripter.
Figure 5.
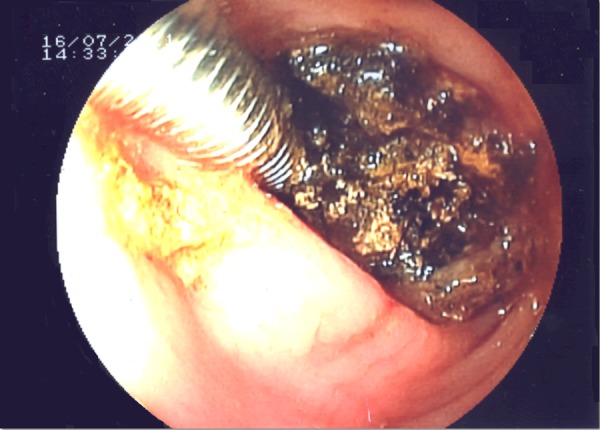
Lithotripter fragmenting the gallstone.
Outcome and follow-up
The episode of obstruction settled spontaneously over the next 24 h and the remaining fragments of the gallstone were passed with only minor discomfort (figure 6). The patient was discharged the following day and reviewed in the clinic 6 weeks later making a complete recovery. On obtaining consent to write this case, the patient has disclosed no further problems in the 2 years since discharge.
Figure 6.

The obstructing gallstone and fragments.
Discussion
Cholecystoenteric fistula is a complication of cholelithiasis resulting from a fistula between the gallbladder and the gastrointestinal tract.1 These fistulas usually occur following an acute inflammatory episode, such as acute cholecystitis, which forms adhesions between the gallbladder and commonly the duodenum, or more rarely the hepatic flexure of the colon or the stomach.2 Other causes include Crohn’s disease, malignancy and trauma. The incidence of cholecystoenteric fistula from autopsy series is reported to be 0.1–0.5%.3
Obstruction of the terminal ileum or ileocaecal valve due to gallstones and a cholecystoduodenal fistula is the most common obstructive presentation; these episodes account for 25% of non-strangulated small bowel obstruction in patients over the age of 65 years.4 Successful colonoscopic retrieval of an impacted gallstone from the ileocaecal valve has been reported in a frail elderly patient.5
Bouveret’s syndrome describes gastric outlet obstruction due to an impacted gallstone in the pylorus in association with a cholecystoduodenal or cholecystogastric fistula. Though extremely rare, a case of endoscopic lithotripsy and successful stone extraction has been reported.6
Cholecystocolonic fistula without obstruction often presents with diarrhoea due to persistent secretion of bile acids into the colon stimulating mucosal release of water and electrolytes. Fat malabsorption may also cause steatorrhoea and vitamin K deficiency and the patient may exhibit a collection of non-specific complications making the condition difficult to diagnose.7
When colonic obstruction does occur due to a cholecystocolonic fistula, the most often reported site of obstruction is the rectosigmoid junction. The majority of cases involve an elderly patient who is often female and a history of preceding biliary disease is likely.
The gold standard for diagnosis is CT which has a sensitivity of 93% and a specificity of 100%; this helps visualise the gallstone and the fistula tract, influencing decision-making in the future management.8
Surgical management consists of simple enterolithotomy, which may be an open or laparoscopic procedure. Synchronous cholecystectomy and fistula repair may be performed or contemplated later as a staged procedure. A review of 1001 gallstone ileus cases showed that the ‘one-stage procedure’ carried a 16.9% mortality compared with 11.7% for a simple enterolithotomy.4
Larger gallstones over 4 cm may not be easily retrieved using simple endoscopic measures such as a Dormia basket or a polypectomy snare. Instead, lithotripsy may be required to break the gallstone into smaller fragments which can then be extracted into the rectum for retrieval. Extracorporeal shockwave lithotripsy and laser lithotripsy have been described to successfully extract an impacted gallstone from the sigmoid colon, although in one case repeated laser treatments were required before complete stone extraction could be achieved.9–11
This is the first reported case to document the use of mechanical lithotripsy to successfully resolve an episode of large bowel obstruction from a gallstone. Although no complications occurred in this patient, rare instances of equipment failure, perforation and bleeding have been reported during mechanical lithotripsy of pancreatic and common bile duct stones.12
We conclude that with a stable patient, in whom bowel perforation is not suspected, little is lost by attempting endoscopy and lithotripsy in the first instance and reserving surgery in case of failure.
Learning points.
Gallstones are common but can present atypically.
Gallstone ileus accounts for 25% of small bowel obstructions over the age of 65 years.
Cholecystocolonic fistula usually presents with diarrhoea.
Large bowel obstruction due to gallstones is extremely rare.
Where bowel perforation is not suspected, consider endoscopy and lithotripsy.
Acknowledgments
The authors would like to thank the CEPOD theatre staff and Ward 109 at University Hospital of North Staffordshire, for the care of the patient.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Athwal TS, Howard N, Belfield J, et al. Large bowel obstruction due to impaction of a gallstone. BMJ Case Rep 2012;2012:pii: bcr1120115100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Osman N, Subar D, Loh MY, et al. Gallstone ileus of the sigmoid colon: an unusual cause of large-bowel obstruction. HPB Surg 2010;2010:153740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hernandez C, Heuman D, Vlahcevid ZR. Pathophysiology of disease associated with deficiency of bile acids. Principles and practice of gastroenterology and hepatology. New York: Elsevier Science Publishing, 1988:384–95 [Google Scholar]
- 4.Reisner RM, Cohen JR. Gallstone ileus: a review of 1001 reported cases. Am Surg 1994;60:441–6 [PubMed] [Google Scholar]
- 5.Murray EL, Collie M, Hamer-Hodges DW. Colonoscopic treatment of gallstone ileus. Endoscopy 2006;38:197. [DOI] [PubMed] [Google Scholar]
- 6.Doycheva I, Limaye A, Suman A, et al. Bouveret's syndrome: case report and review of the literature. Gastroenterol Res Pract 2009;2009:91495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Savvidou S, Goulis J, Gantzarou A, et al. Pneumobilia, chronic diarrhea, vitamin K malabsorption: a pathognomonic triad for cholecystocolonic fistulas. World J Gastroenterol 2009;15:4077–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yu CY, Lin CC, Shyu RY, et al. Value of CT in the diagnosis and management of gallstone ileus. World J Gastroenterol 2005;11:2142–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Meyenberger C, Michel C, Metzger U, et al. Gallstone ileus treated by extracorporeal shock-wave lithotripsy. Gastrointest Endosc 1996;43:508–11 [DOI] [PubMed] [Google Scholar]
- 10.Alkhusheh M, Tonsi AF, Reiss S, et al. Endoscopic laser lithotripsy for gallstone large bowel obstruction. Int J Case Rep Images 2011;2:11–14 [Google Scholar]
- 11.Pracki M, Regula J, Pachlewski J, et al. Sigmoid laser lithotripsy for gallstone ileus. Folia Gastroenterol Hepatol 2006;4:30–2 [Google Scholar]
- 12.Thomas M, Howell DA, Carr-Locke D, et al. Mechanical lithotripsy of pancreatic and biliary stones: complications and available treatment options collected from expert centers. Am J Gastroenterol 2007;102:1896–902 [DOI] [PubMed] [Google Scholar]


