Abstract
BACKGROUND:
According to the precepts of reduced surgical trauma and better cosmesis, an intermediate laparoscopic appendectomy technique between the conventional three-trocar procedure and Laparoendoscopic Single Site Surgery (LESS) was performed, based on literature review and experience of the surgical team.
PATIENTS AND METHODS:
Patients with early stage acute appendicitis and a favourable anatomical presentation were selected. The procedure was performed with two ports: A 10 mm trocar at the umbilicus site for laparoscope and a 5 mm one just above the pubic bone for grasper. The appendix was secured by external wire traction through a right iliac fossa puncture with 14-gauge intravenous catheter.
RESULTS:
From August 2009 to December 2012, we performed 42 cases; two required conversion to a conventional laparoscopic technique. There were no complications in the remaining, no wound infections and a mean operation time of 64.5 minutes.
CONCLUSION:
The use of two-port laparoscopic appendectomy can act as a LESS intermediate step procedure, without loss of instrumental triangulation and maintenance of appropriate counter-traction. This technique can be used as an alternative to the three-port laparoscopic procedure in patients with initial presentation of appendicitis and a favourable anatomical position.
Keywords: Appendix fixation, laparoscopic appendectomy, LESS, minimally invasive surgery
INTRODUCTION
Despite the current refinement of laparoscopy, there is still interest in the reduction of surgical trauma and aesthetic quality by reducing the number and size of incisions for portals. This effort was made in the group of procedures known as Laparoendoscopic Single Site Surgery[1,2] (LESS), including the use of Single-Port Laparoscopy[3,4] and Single-Incision Laparoscopic Surgery (SILS).[5,6] Mini-laparoscopy also appears as an option, using portals positioned conventionally but with reduced diameter.[7] According to these trends, our group established a safe surgical technique that could be offered to patients with acute appendicitis, which was reproducible and economically viable.
PATIENTS AND METHODS
The population consisted of patients evaluated in the emergency department with suspected acute appendicitis. A laparoscopic treatment was initially offered, as well as the possibility of conversion to open surgery. It was also explained that, pathological conditions permitting, the surgery would be initiated with two portals. Informed consent was obtained and all surgeries were recorded and analysed by members of our service. The surgeons participating in this study used to perform conventional laparoscopic appendectomy in their routine surgical practice and the proposed two-port technique was adapted after an 8-hour training box model.
Preparations were made as in the conventional technique. Before entering the operating room, the patient was asked to urinate. The Trendelenburg position was adopted during the procedure with both arms tucked, associated with the operating table angle tilted to the left. The surgeon and his assistant were positioned left to the patient.
The systematised two-port laparoscopic appendectomy technique initiated with diagnostic laparoscopy through the 10-mm umbilical port, with pneumoperitoneum set at 12 mmHg, to confirm the diagnosis or identify another cause of acute abdomen. At this point, the 5-mm port was inserted at the suprapubic area below the pubic hairline, which facilitated the evaluation and mobilisation of the appendix with a grasper. Its (favourable) anatomical position and the absence of generalised peritonitis that would require greater cleaning of the abdominal cavity were evaluated. Had one of these adverse findings been present, appendectomy would have been performed according to the conventional laparoscopic technique and an additional 5-mm, properly triangulated trocar would have been inserted.
The team decided to continue with two ports, and the location of the transparietal puncture with a 14-gauge intravenous catheter was determined. With the grasper traction towards the anterior abdominal wall and external abdominal palpation by the surgeon, the point of greatest exposure of the mesoappendix at the right iliac fossa (or even at the right upper quadrant) was identified.
A simple 2.0 polypropylene loop was protected inside the catheter during the abdominal puncture. Before removing the needle, the loop was introduced into the cavity and secured by the grasper. As in the paracentesis technique, the needle was removed and its infusion line left in place. The loop was passed around the appendix and a sliding knot was fashioned. Because of the monofilament suture used, the knot slides through the 14-gauge infusion line simply by external traction, without the need of a knot pusher. Thus, the appendix is fixed with minimal manipulation [Figure 1].
Figure 1.
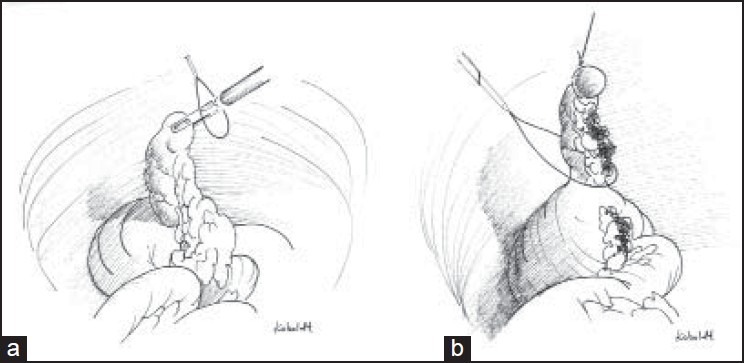
Surgical steps (a) Appendicular transparietal fixation (b) Double ligature at the appendix base using sling knots
The exteriorised suture provides the necessary counter-traction to the surgeon. If the exposure angle required changing during the procedure, the suture would be replaced by a new transparietal puncture. The procedure involved double ligation of the appendix base with 2.0 polypropylene sliding knots and obliteration of the appendicular artery using bipolar electrocautery.[8,9] After appendectomy completion, the surgical specimen was removed inside an endobag inserted through the 10-mm umbilical trocar. This bag was previously held outside with a suture for later extraction through the laparoscope port.
The records of the first cases were analysed to identify improvements that could help establish the technique. Patients were evaluated on the 12th postoperative day for analysis of recovery, port site healing, aesthetic satisfaction and registration of the anatomopathological result.
RESULTS
From August 2009 to December 2012, 42 appendectomies were performed using the two-port technique. In the first attempt, the team had to convert to the conventional technique, placing an additional 5-mm port to control appendicular artery bleeding. In one case, the surgeons had to interrupt the laparoscopic procedure due to haemodynamic instability during pneumoperitoneum creation, then proceeding to open appendectomy. In another patient, the initial diagnostic laparoscopy identified ascending colon appendagitis. In that context, the third port was inserted to remove the inflamed epiploic appendix and perform the incidental appendectomy.
The remaining cases had no complications and were initiated and concluded by using two ports. The mean operative time was 64.5 minutes. Most of the cases were discharged during the first postoperative day and none required antibiotic therapy. The 20th case was conducted in a first trimester pregnant patient who had phlegmonous appendicitis and was discharged on the second postoperative day. The laparoscopic staging of the disease identified initial hyperaemia, oedema and fibrinous exudate in all cases, without any episodes of appendiceal perforation, abscess or diffuse peritonitis.[10] There was no need for re-intervention and all were confirmed to be acute appendicitis by the pathological analysis. Moreover, patients’ aesthetic satisfaction was present with barely visible scars [Figure 2]. The only possible painful site was reported at the umbilical site and no wound infections were detected.
Figure 2.

Aesthetic result in a female patient
DISCUSSION
The described technique can be considered minimally invasive and a transition to LESS procedures, with the advantage of better triangulation and avoiding collisions between laparoscope and instruments. Regarding the mini-laparoscopic surgery, the 5-mm hypogastric port can be replaced with a 3-mm trocar, and a 5-mm laparoscope can be used as well. However, we identified one meta-analysis comparing the “needlescopic” appendectomy against the conventional technique, concluding that there were no differences in postoperative hospitalisation. Although safe and effective, mini-laparoscopy had a higher conversion rate to open appendectomy and longer surgical time.[11]
During the mesoappendix dissection, its position in front of the laparoscope when pulled towards the anterior wall enables the surgeon to simply perform linear movements to cauterise and cut the appendicular artery. The counter-traction of the appendix, the basic difference from the standard procedure and requiring adaptation, was held by the surgeon's left hand tension over the exteriorised suture in the right iliac fossa, as the described “puppet” technique.[12,13] The right hand was used for instrumentation in the 5-mm port during dissection.
Our literature review identified an initial report described as “The Intravenous Catheter at the McBurney's Point” technique,[14] in which an external wire in the right iliac fossa stabilizes the appendix. According to the author, this would be the best way to not traumatise the friable inflamed organ, with less chance of rupture and contamination spread in the peritoneal cavity.
More recently, we have noticed publications interested in the concept of minimally invasive appendectomy. In 2007, Penait L. et al.,[15] published a series of eight patients also treated with two access ports, but with differences in relation to our technique, i.e. trocar sizes, positioning and appendicular fixation (accomplished by a suture in the anterior abdominal wall with a pre-formed endoloop and used as a pulley). In another series,[16] the fixation was done through a transparietal suture in the right iliac fossa, which also transfixes the mesoappendix.
A retrospective study[17] comparing conventional laparoscopic appendectomy (n = 33) versus the SILS technique (n = 40), identified in the latter group shorter surgical time, no conversion to open procedure, and postoperative hospital stay of 1.36 days (vs. 2.36 days). The author noted that with increasing experience, this technique required just one additional port for the laparoscope.
The 14-gauge intravenous catheter puncture did not leave residual scars. In addition, had patients not been advised of the puncture site, many would not have even noticed it. Another description similar to our transparietal appendicular fixation technique[18] also reported the absence of residual scarring created by the puncture needle, which occurs even with incisions for 2 and 3-mm trocars used mini-laparoscopy.
In two recent surgery cases (not added to our series), we tried the surgical technique presented using a single umbilical incision-SILS procedure. Thus, we used two conventional trocars (10 mm and 5 mm) in individualised umbilical aponeurotic insertions. The supra umbilical incision was larger than that used for a single 10-mm trocar accommodation, resulting in a more visible scar. We noted that the difficulty increased due to lower mobility of the instruments, collision, as well as lower triangulation, resulting in increased surgical time (84 and 88 minutes). Even so, the procedures were successful. The patients were also discharged during the first postoperative day. One case developed umbilical seroma, which was managed conservatively.
The adaptation required to migrate from conventional laparoscopic procedures to Single-Port use can be difficult. Consequently, the two-port appendectomy model can be used in training programs to acquire the necessary skills to perform more complex LESS procedures. Much like in basic laparoscopic training, the degree of difficulty offered by appendectomy is of low complexity.[19,20]
As identified in the literature, these studies are mostly case reports or retrospective descriptions and studies with more statistical power are needed for setting guidelines. The completion of the surgical technique can be difficult in cases of unfavourable anatomical presentation (retrocecal) or even in complex cases of abdominal cavity contamination. These situations may lead to an opposing point of view by those who perform the conventional three-port technique. However, the authors suggest that it could be performed in cases of uncomplicated early presentation appendicitis with favourable anatomical position. We do not intend to supplant traditional surgical techniques but to offer options for the arsenal of laparoscopic surgeons.
As future direction, the surgical technique presented in this article motivated our group to conduct research in the development of new technologies at the Federal University of Rio Grande do Sul State (UFRGS, Brazil), entitled “The Development of Two-channel Single Port Model for Minimally Invasive Appendectomy”. We established a partnership with Bhiosupply, a local manufacturer of laparoscopic instruments, and received a governmental grant (SENAI-Brazil).
The single port developed was called Centryport®, which generated an industrial patent. It consists of a reusable device, manufactured in aluminium alloy. Its efficiency and safety were validated through experimental laparoscopic appendectomy using a swine model, reproducing the same technique as described for two-port laparoscopy. The data for this study is currently being compiled and analysed for publication.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Gill IS, Advincula AP, Aron M, Caddedu J, Canes D, Curcillo PG, 2nd, et al. Consensus statement of the consortium for laparoendoscopic single-site surgery. Surg Endosc. 2010;24:762–8. doi: 10.1007/s00464-009-0688-8. [DOI] [PubMed] [Google Scholar]
- 2.Tracy CR, Raman JD, Cadeddu JA, Rane A. Laparoendoscopic single-site surgery in urology: Where have we been and where are we heading? Nat Clin Pract Urol. 2008;5:561–8. doi: 10.1038/ncpuro1215. [DOI] [PubMed] [Google Scholar]
- 3.Galvão M, Almino A, Campos J. Single port laparoscopic access surgery. Tech Gastrointest Endosc. 2009;11:84–93. [Google Scholar]
- 4.Hong TH, You YK, Lee KH. Transumbilical single-port laparoscopic cholecystectomy: Scarless cholecystectomy. Surg Endosc. 2009;23:1393–7. doi: 10.1007/s00464-008-0252-y. [DOI] [PubMed] [Google Scholar]
- 5.Cuesta MA, Berends F, Veenhof AA. The “invisible cholecystectomy”: A transumbilical laparoscopic operation without a scar. Surg Endosc. 2008;22:1211–3. doi: 10.1007/s00464-007-9588-y. [DOI] [PubMed] [Google Scholar]
- 6.Hirano Y, Watanabe T, Uchida T, Yoshida S, Tawaraya K, Kato H, et al. Single-incision laparoscopic cholecystectomy: Single institution experience and literature review. World J Gastroenterol. 2010;16:270–4. doi: 10.3748/wjg.v16.i2.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sajid MS, Khan MA, Ray K, Cheek E, Baig MK. Needlescopic versus laparoscopic cholecystectomy: A meta-analysis. ANZ J Surg. 2009;79:437–42. doi: 10.1111/j.1445-2197.2009.04945.x. [DOI] [PubMed] [Google Scholar]
- 8.Sajid MS, Rimple J, Cheek E, Baig MK. Use of Endo-GIA Versus Endo-loop for securing the appendicular stump in laparoscopic appendicectomy: A systematic review. Surg Laparosc Endosc Percutan Tech. 2009;19:11–5. doi: 10.1097/SLE.0b013e31818a66ab. [DOI] [PubMed] [Google Scholar]
- 9.Ponsky TA, Rothenberg SS. Division of the mesoappendix with electrocautery in children is safe, effective, and cost-efficient. J Laparoendosc Adv Surg Tech A. 2009;19(Suppl 1):S11–3. doi: 10.1089/lap.2008.0101.supp. [DOI] [PubMed] [Google Scholar]
- 10.Gomes CA, Nunes TA. Acute appendicitis laparoscopic classification. Correlation between disease grade and intraoperative variables. Rev Col Bras Cir. 2006;33:289–93. [Google Scholar]
- 11.Sajid MS, Khan MA, Cheek E, Baig MK. Needlescopic versus laparoscopic appendectomy: A systematic review. Can J Surg. 2009;52:129–34. [PMC free article] [PubMed] [Google Scholar]
- 12.Chow A, Purkayasstha S, Aziz O, Paraskeva P. Single-incision laparoscopic surgery for cholecystectomy: An evolving technique. Surg Endosc. 2010;24:709–14. doi: 10.1007/s00464-009-0655-4. [DOI] [PubMed] [Google Scholar]
- 13.Roberts KE. True single-port appendectomy: First experience with the “puppeteer technique”. Surg Endosc. 2009;23:1825–30. doi: 10.1007/s00464-008-0270-9. [DOI] [PubMed] [Google Scholar]
- 14.Yeung GH. The intravenous catheter at the McBurney's point. Surg Laparosc Endosc. 1999;9:45–8. [PubMed] [Google Scholar]
- 15.Panait L, Bell RL, Duffy AJ, Roberts KE. Two-port laparoscopic appendectomy: Minimizing the minimally invasive approach. J Surg Res. 2009;153:167–71. doi: 10.1016/j.jss.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 16.Ateº O, Hakgüder G, Olguner M, Akgür FM. Single-port laparoscopic appendectomy conducted intracorporeally with the aid of a transabdominal sling suture. J Pediatr Surg. 2007;42:1071–4. doi: 10.1016/j.jpedsurg.2007.01.065. [DOI] [PubMed] [Google Scholar]
- 17.Chow A, Purkayastha S, Nehme J, Darzi LA, Paraskeva P. Single incision laparoscopic surgery for appendicectomy: A retrospective comparative analysis. Surg Endosc. 2010;24:2567–74. doi: 10.1007/s00464-010-1004-3. [DOI] [PubMed] [Google Scholar]
- 18.Akgür FM, Olguner M, Hakgüder G, Ateş O. Appendectomy conducted with single port incisionless-intracorporeal conventional equipment-endoscopic surgery. J Pediatr Surg. 2010;45:1061–3. doi: 10.1016/j.jpedsurg.2010.01.025. [DOI] [PubMed] [Google Scholar]
- 19.Perry ZH, Netz U, Mizrahi S, Lantsberg L, Kirshtein B. Laparoscopic appendectomy as an initial step in independent laparoscopic surgery by surgical residents. J Laparoendosc Adv Surg Tech A. 2010;20:447–50. doi: 10.1089/lap.2009.0430. [DOI] [PubMed] [Google Scholar]
- 20.Chiu CC, Wei PL, Wang W, Chen RJ, Chen TC, Lee WJ, et al. Role of appendectomy in laparoscopic training. J Laparoendosc Adv Surg Tech A. 2006;16:113–8. doi: 10.1089/lap.2006.16.113. [DOI] [PubMed] [Google Scholar]


