Abstract
Vascular injuries during laparoscopic cholecystectomy can occur similar to biliary injuries and mostly represented by intraoperative bleeding. Hepatic artery system pseudoaneurysm are rare. It occurs in the early or late postoperative course. Patients present with pallor, signs of haemobillia and altered liver function. We report a case of right posterior sectoral artery pseudoaneurysm detected 2 weeks after laparoscopic cholecystectomy and successfully repaired laparoscopically. We also describe how laparoscopic pringle clamping saved the conversion. The actively bleeding right posterior sectoral artery pseudoaneurysm was diagnosed by CT angiogram. Embolisation, usually the treatment of choice, would have risked liver insufficiency as hepatic artery proper was at risk because the origin the bleeding artery was just after its bifurcation. Isolated right hepatic artery embolisation can also cause hepatic insufficiency. To our knowledge this is the first reported case of laparoscopic repair of post-laparoscopic cholecystectomy bleeding sectoral artery pseudoaneurysm.
Keywords: Laparoscopic repair of aneurysm, pseudoaneurysm, post cholecystectomy vascular injury, right posterior sectoral artery
INTRODUCTION
Vascular injuries during laparoscopic cholecystectomy is less common than biliary injury. Usual presentation is intraoperative bleed, either from the hepatic artery or the portal vein. Hepatic artery system pseudoaneurysm, especially in right posterior sectoral artery, is rare.[1] It can occur early or late. We report successful laparoscopic repair of bleeding pseudoaneurysm of the right posterior sectoral artery, 2 weeks following laparoscopic cholecystectomy.
CASE REPORT
A 29-year-old male underwent laparoscopic cholecystectomy. At operation, Callot's anatomy was normal. Gall bladder was mildly inflamed containing multiple stones. Cystic artery was small and divided with harmonic scalpel in coagulating mode after double sealing. Cystic duct clipped with locking clip and divided.
After 2 weeks, the patient was readmitted to the hospital with complaints of fatigue. He appeared pale, afebrile, with pulse rate of 100 and blood pressure 110/60 and mild guarding over the right upper abdomen. Plain film of the abdomen showed no pathology. Blood investigation showed haemoglobin 8. 6 g/dl (pre operative was 15.6), bilirubin 2.7 mg/dl with indirect bilirubin 1.6, signifying haemolysis, and slight increase in liver enzymes (aspartate aminotransferase 138UI/L; alanine aminotransferase 106 UI/L). Abdominal ultrasound followed by computed tomographic (CT) angiography with vascular reconstruction revealed intraperitoneal blood, mainly in Gallbladder fossa, with active bleed (contrast blush) from right posterior sectoral artery pseudo aneurysm [Figure 1].
Figure 1.
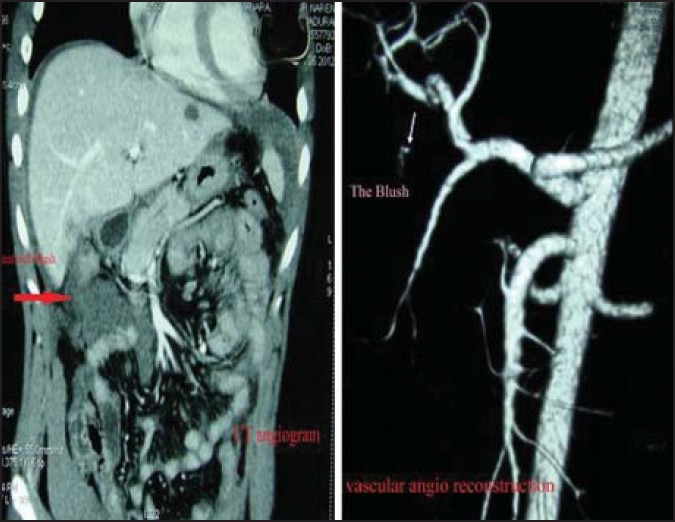
Preopertive imaging
The angiographic embolisation was discussed. As the bleeder originated from right hepatic artery very near the bifurcation of hepatic artery proper, there was a possibility that not only right hepatic artery, but hepatic artery proper also may need to be embolized to control the bleed risking massive liver necrosis. So, operative exploration was decided. After stabilisation, we proceeded with laparoscopy, keeping an open instrument trolley ready for laparotomy.
At laparoscopy, intra-abdominal blood clots were suctioned out and gall bladder fossa adhesions were dissected with suction tip. The pulsating pseudoaneurysm with clot was identified in the right hepatic artery/cystic artery area. While trying to dissect the right hepatic artery, the pseudoaneurysm started to bleed. Combination of pressure, suction, and temporary control with clips failed. While contemplating conversion, we put in an extra port and applied laparoscopic Pringle (vascular) clamp as that would have been the first step after conversion. The bleeding immediately reduced to a trickle. It was now possible to clearly identify the right hepatic artery and the sectoral artery stump and intracorporeally suture ligate the offending artery stump at the base taking some peri-arterial tissue to prevent slipping of the suture [Figure 2]. The controlled environment helped taking precise bites. As per CT, the bleeding point was away from right hepatic duct so risk of biliary injury was minimal. The patient made an uneventful recovery.
Figure 2.
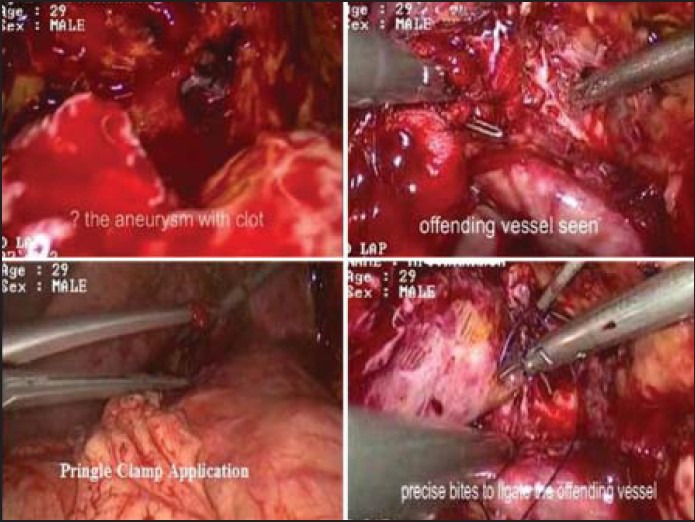
Intraoperative pictures
DISCUSSION
Laparoscopic cholecystectomy has vascular injuries rate of 0.25-0.5%, with major morbidity.[2] Classical triad pain, jaundice and haemobilia is seen in 20-30% of them.[3]
They present with abdominal pain or discomfort, GI bleeding and altered liver function tests. An abdominal mass with bruit may be detected. Rupture into the peritoneal cavity, portal vein or pancreatic pseudo-cyst can also occur.[2] Haemobilia, if present, suggests pseudo-aneurysm. Ultrasound may reveal a hypo-echoic, pulsatile mass within the liver, with bidirectional flow on Doppler. CT arteriogram will demonstrate haemorrhages or pseudo-aneurysm formation, which may be missed on ERCP and angiogram because of the intermittent character of bleeding. Selective celiac and SMA angiography is most reliable. In our case CT angiogram was sufficient. Suggested aetiopathologies are vascular erosion secondary to clip encroachment, direct lesion of the vascular wall during surgery and electric current diffusion through clips placed close to vascular pedicle.[2,4] In our case, the heat from the harmonic used to seal cystic artery may have contributed.
Trans-arterial embolisation is the treatment of choice in the presence of haemorrhage.[5] In our case, due to low origin of the bleeder, there was possibility of embolisation of hepatic artery proper risking massive liver necrosis. Right hepatic artery ligation/embolisation can also cause hepatic insufficiency. Hence operative approach was attempted.
There is no report of successful management of such condition laparoscopically. The magnified laparoscopic view helped precise ligation of the bleeder, avoiding right hepatic artery ligation and hepatic ischaemia.
In conclusion, if angio-embolisation fails or contraindicated, in a stable patient, laparoscopic repair of sectoral artery pseudo aneurysm is feasible. Laparoscopic Pringle's manoeuvre is helpful.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.De Molla Neto OL, Ribeiro MA, Saad WA. Pseudoaneurysm of cystic artery after laparoscopic cholecystectomy. HPB (Oxford) 2006;8:318–9. doi: 10.1080/13651820600869628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roche-Nagle G, MacEneaney, Harte P. Pseudo-aneurysm of the hepatic artery after laparoscopic cholecystectomy: A case report. J Min Access Surg. 2006;2:73–5. doi: 10.4103/0972-9941.26652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Deziel DJ, Millikan KW, Economou SG, Doolas A, Ko ST, Arian MC. Complications of laparoscopic cholecystectomy: A national survey of 4,292 hospitals and an analysis of 77,604 cases. Am J Surg. 1993;165:9–14. doi: 10.1016/s0002-9610(05)80397-6. [DOI] [PubMed] [Google Scholar]
- 4.Rhee JW, Bonnheim DC, Upson J. Cystic artery pseudoaneurysm. N Y State J Med. 1987;87:47. [PubMed] [Google Scholar]
- 5.Saldinger PF, Wang JY, Boyd C, Lang E. Cystic artery stump pseudoaneurysm following laparoscopic cholecystectomy. Surgery. 2002;31:585–6. doi: 10.1067/msy.2002.115353. [DOI] [PubMed] [Google Scholar]


