Abstract
Background:
The annual risk of tuberculosis infection is 1.9% in Himachal Pradesh against a national average of 1%. Revised national tuberculosis control program (RNTCP) in Kangra was introduced in October, 1998. We analyzed the 5-year (2001-2005) RNTCP secondary data from Kangra to evaluate the performance of the program.
Materials and Methods:
We collected data from all the five tuberculosis units the district. We calculated the following indicators-case detection rate, tuberculosis cases by category-new smear positive (or smear negative but seriously ill) defaulters, relapses and failures, extra-pulmonary, and new smear negative cases. We compared the results with Himachal Pradesh and India. We employed the standardized program indicators-sputum positivity, cure, death, failure and default rates.
Results:
Extra pulmonary cases ranged in between 56% and 73%, normal being 15-20%. The highest category-1 varies from 42% to 48%. New smear positive case detection rates (78-90%) and cure rates (88-91%) were the highest as compared to figures of the state and country. Failure rate was maximum in Kangra Tuberculosis Units (TU)-6.5% and the default rate was 7.2% in TU Palampur. The tuberculosis cases have fallen down from 6,462/100, 000 in 1999 to 2,195/100, 000 in 2005 following the introduction of RNTCP in 1999. Age specific (15-55 years) and sex-wise males were more affected than the females (59-64%).
Conclusions:
Continue investment in the program to sustain progress achieved. Investigate the cause of high proportion of extra-pulmonary tuberculosis. Investigate Kangra TU unit with a high default rate.
Keywords: Extra pulmonary tuberculosis, Kangra, revised national tuberculosis control program, tuberculosis unit
Introduction
Tuberculosis is an infectious disease caused by Mycobacterium tuberculosis. In 1865, Villamin succeeded in passing the disease from a cow to a rabbit. In 1892, Robert Koch demonstrated that it was caused by the bacillus, called as Mycobacterium tuberculosis (Koch’ bacillus).[1] The World Health Organization (WHO) has identified 22 high-burden tuberculosis (TB) countries that combined contributes 80% of the global burden of TB. Asia carries the largest number of TB cases worldwide. Globally, estimated cases of infectious TB are 16-20 million, estimated new cases are 4-5 million, and estimated death is three million each year.[2] WHO estimates of 2000 indicates that unless urgent action is taken, more than four million people in India will die of TB in the next decade. India alone accounted for an estimated one quarter (26%) of all TB cases worldwide and China and India combined accounted for 38%.[3] Further studies have shown that TB is a major barrier to economic development, costing approximately Rs.13,000 crores in a year.[4] TB is a worldwide public health problem.[3,5] The number of the persons infected with the TB bacillus is estimated to be 1.7 billion, of which 1.3 billion live in the developing countries.
In India, the overall prevalence of infection is 30%.[6] More than 40% of the adults are infected with TB, and approximately, 1.5 million cases are put on treatment every year. Every smear positive case can infect approximately, 10-15 cases, thereby, increasing the pool of the infected persons. Prevalence of infection in males has increased in 45 years and in females below 35 years. The prevalence of TB is four cases per 1,000 populations. The incidence of infection is 1-2%.[7] Incidence of new cases is one per 1,000 excluding children below 5 years. There is no seasonal variation. Most of the people affected by TB are in the age group of 15-54 years, which is the economically active age group.[8,9] In Himachal Pradesh, TB is quite wide spread among the low socio-economic classes and the slum areas where women are the most sufferers. Himachal has the annualized risk of infection as 1.9% as against that of 1.0% of India,[10] and it occupies the 8th place (3.67%) in the women from the top 10 leading causes of the diseases while in district Kangra, it is numbered on 7th place.[11] TB continues to be a major public health problem for India, Himachal Pradesh and Kangra.
For the control of TB, Revised National TB Control Program was implemented in 12 districts of Himachal Pradesh in phased manner from 1995; first in Hamirpur followed by Kangra, and Mandi in October 1998. Objective of the Revised National Tuberculosis Control Program (RNTCP) programme is to achieve >85% cure rate in all new smear positive pulmonary patients and detect 70% of cases once the >85% cure rate is achieved.[9,12] We analyzed the secondary RNTCP data from Kangra district to review the program performance. The objectives of analysis is to describe TB surveillance data over the period of time in terms of time, place, and person characteristics, identify data quality and issues related to RNTCP, and suggest measures to improve/sustain data quality based upon the findings of above two.
Materials and Methods
Descriptive epidemiology
Study area
District Kangra-Himachal Pradesh, India.
Study period
May 20-31st May, 2006.
Study population
The total population covered under RNTCP in the year 2001 was 13, 38, 536 that was the entire population of district Kangra. The population has been divided in five Tuberculosis Units (TU) and 29 microscopic centers supervised by five senior treatment supervisors (STS), and five Senior Tuberculosis Laboratory supervisor (STLS).
Study design
Analysis of secondary data of TB generated by RNTCP in Kangra district.
Data sources
Records and Reports from the Office of the Chief Medical Officer of Kangra.[13,14]
Operational definition
Sputum positive tuberculosis
We defined a patient as sputum positive when at least two initial sputum smears are positive for acid-fast bacilli (AFB) or one AFB positive smear and one positive culture. Sputum smear examination is a laboratory technique to screen sputum for TB, where AFB are stained red by Ziehl Neelsen method and then identified and counted using microscopy.[15]
OR: TB in a patient with one sputum examination positive for AFB and radiographic abnormalities consistent with active pulmonary TB as determined by the treating Medical Officer,
OR: TB in a patient with one sputum specimen positive for AFB and culture positive for M. tuberculae.
Indicators used for analysis
New smear sputum positive case detection rate
A patient with sputum positive pulmonary TB who has never had treatment for TB or has taken anti-TB drugs for less than four weeks or at least two initial sputum smear positive for AFB or one AFB positive smear and one positive culture.
Case fatality rate
We defined case fatality rate from TB as proportion of deaths due to TB among total number of TB cases during the year.
Cure rate
We defined cure rate as the proportion of patients registered for Directly Observed Treatment Short therapy (DOTS) completed treatment and his two sputum slides have become negative at the end of the treatment. A cure rate is calculated as number of cured cases by total number of new smear sputum positive cases put on treatment by 100.
Failure rate
A patient who was initially smear positive who began treatment and who remained or became smear positive again at 5 months or later during the course of treatment. A failure rate is calculated as number of failure cases by total number of new smear sputum positive cases put on treatment by 100.
Default rate
A default rate is calculated as number of defaulting cases by total number of new smear sputum positive cases put on treatment by 100.
Results
Profile TB cases according to TB treatment category
Category-1 varies from 42% to 48% and is the highest but the category-3 ranges from 34% to 42% [Figure 1]. The extra pulmonary TB (EP TB) cases are higher than 50% [Range being 56-73%, normal being 15-20%, Figure 1]
Figure 1.
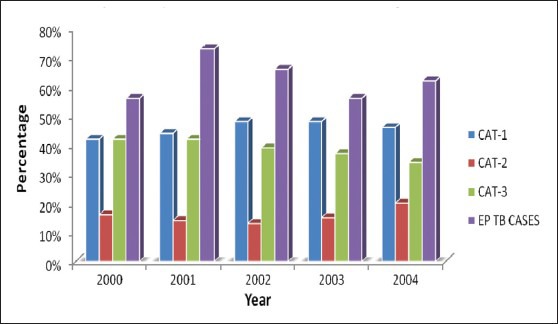
Distribution of tuberculosis cases by treatment category and extra pulmonary cases in district Kangra, Himachal Pradesh
New smear sputum positive case detection rate
Time and place characteristics
The new smear sputum positive (NSP) case detection rate of India was 47% in 2001, 59% in the year 2002, 69% in 2003, 72% in 2004, and 66% in the year 2005, whereas, that of Himachal Pradesh it was 70% in 2001, 65% in 2002, 82% in 2003, 82% in 2004, and 81% in the year 2005. The new smear sputum positive case detection rate had increased in Himachal Pradesh as compared to India during 2001-2005 [Figure 2].
Figure 2.
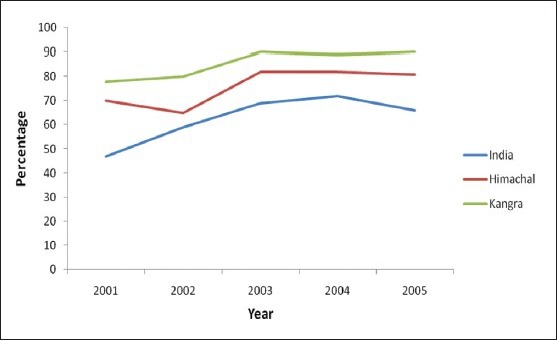
New smear positive case detection rates of India vs. Himachal Pradesh vs. Kangra from 2001 to 2005
Comparison of new smear detection rate of Himachal Pradesh with Kangra
Time and place characteristics
When we compared from 2001 to 2005, new smear positive case detection rates of the state and the district Kangra, we observed Kangra is performing better than the state [Figure 2]. The rates for Kangra are 78% in 2001, 80% in 2002, 90% in 2003, 89% in 2004, and 90% in 2005, respectively.
Cure rate
Time and place characteristics
The cure rate of India was 85% in 2001, 84% in the year 2002, 86% in 2003, 85% in 2004, and it was 85% in the year 2005, whereas of Himachal Pradesh, it was 87% in 2001, 90% in 2002, 88% in 2003, 87% in 2004, and 87% in the 2005. In case of Kangra, the cure rates for the aforesaid period are 91%, 89%, 88%, 90%, and 91%, respectively. The cure rate of Himachal Pradesh was higher as compared to India but Kangra was the highest during 2001-2005 [Figure 3]. When we analyze and compare the inter district cure rates position in Himachal Pradesh, Kangra lies 2nd on the ladder with cure rate of 91%, the other higher up district is Lahaul and Spiti.
Figure 3.
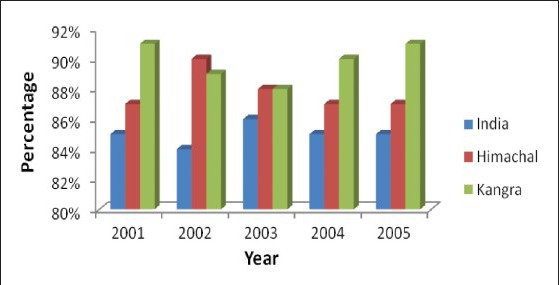
Comparison of Cure rates of India vs. Himachal Pradesh vs. Kangra from 2001 to 2005
The TB cases have fallen down from 6,462/100, 000 in 1999 to 2,195/100,000 in 2005 following the introduction of RNTCP in 1999 in the district [Figure 4]. Sex-wise break up of TB cases in district Kangra for 5 years (2001-2005) in which the proportions of the males varies from 59% to 64%, whereas those of females ranges in between 36% and 41%, indicating that the sex-wise males were more affected than the females [Figure 5]. Age-specific break up of persons’ characteristic suggests from 2001 to 2005 that 15-55 years of the cases are more affected with TB and thereafter, the decline starts.
Figure 4.
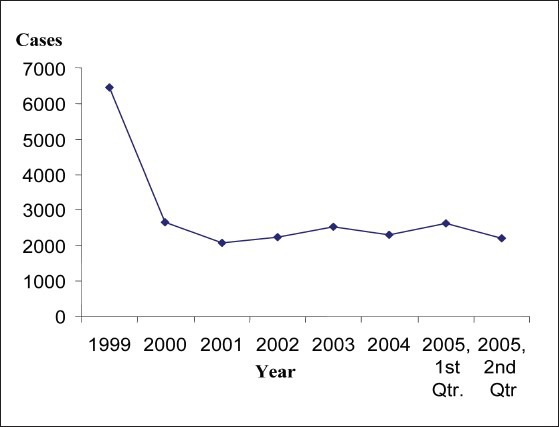
Tuberculosis cases RNTCP in district Kangra
Figure 5.

Sex-wise break up of tuberculosis cases of district Kangra, Himachal Pradesh from 2001 to 2005
Discussion
TB continues to be a major public health problem round the globe, India, Himachal Pradesh and Kangra.[3,5,9,16] Revised National TB Control Program was launched in India in 1993. The laboratory microscopy is the key factor for its operation on the ground for diagnosis and treatment as DOTS strategy. That is why, in Kangra, category-wise high detection rate shows that numbers of the cases in category-1 (CAT 1) are the maximum, followed by category-3 (CAT 3), and the least in category-2 (CAT 2).[16] The incidences of the EP TB cases are quite high as compared to the normal international figure of 15-20%. One of the possible reasons for this may be because of the medical college hospital at Dharamshala and availability of the specialists capable of diagnosing extra pulmonary TB cases at Palampur, district Kangra.
In India, new case detection rate has risen slowly from 59% to 66%, from 2001 to 2005. In Himachal Pradesh, the new sputum positive case detection rate has remained above 75% due to better health facilities and the people faith into the governmental peripheral net work of health care facilities and the literacy rate as high as 77% has caused high awareness of TB in the state. But compared with inter district performance of Kinnour, Chamba district, where the new case detection rate is less than 75%, due to the tribal areas and difficult geographical locations with shortage of medical human resource, Kangra district is the largest population-wise district of Himachal Pradesh (22% of the total population), and it is performing high to the level of the programme targets. The new case detection rate after the introduction of RNTCP in 1999 has gone up from 80% to 84% in 2005, and thereafter, gone down to 62% due to vacancies of the posts of two posts of Medical officer tuberculosis center MO TC.[17] The heavy influx of the tourists in Dharamshala and presence of the local government medical college are the other factors for high case detection rate till now. The government medical college has one of the Designated Microscopic Centers (DMC) in district Kangra. Second factor for high detection rate is its location with Punjab border from where the people from the bordering districts visit the medical college for the expert opinion. Another study by Chennaveerappa et al., at teaching hospital in South India observes the cure rate among new smear positive (NSP) as 84%. The performance of TB control Program at a teaching hospital in 2008 at par with RNTCP norm but the treatment success rate of 83.4% was less than RNTCP norm. This was due to irregular treatment, defaulting and alcoholism.[18]
Analyzing the program indicators to note down the efficacy, comparing from the country figure of 80% to 86% from 2000 onwards for cure rate, Himachal Pradesh has performed better with cure rate indicator ranging from 85% to 90%, from 2001 to 2005. Globally, the treatment success rate has exceeded the 85% target for the first time in 2008 since the target was set in 1991, with a percentage of 87% for patients starting treatment in 2007. Furthermore, treatment success rates were maintained or improved between 2006 and 2007 in all WHO regions with the exception of the European Region which recorded the lowest success rate globally at 67%.[19] Kangra district when we analyze and compare with the state of Himachal Pradesh, we observed that the cure rate indicator has varied from 89% to 91% and second best from Lahaul and Spiti district when inter district comparative analysis was observed. But it has gone to third position as per Himachal Report 2009,[20] trailing by Hamirpur and Lahaul and Spiti district. Kangra has the best literacy rate (80% in males and 82% in females) next to Hamirpur district of the state and second best network of the peripheral medical services. Compared with five TB units TUs Dehra, Dharamshala, Kangra, Nurpur, and Palampur vis-a-vis Kangra, the failure rate of TU Kangra is 6.5% and the default rate in TU Palampur was 7.2%. They may be due to the migratory population taking the temporary treatment while all other indicators of program are above the national norms. We could partially collect the TUs data for 5 years due to corruption of the data file, and hence, the detailed comparative study could not be done. Sex-specific and age-specific person characteristics’ are concerned, females are less affected compared to the males and the age group 15-54 has the maximum burden of the disease. With the introduction of the Revised National TB Program in 1999 at Kangra, the prevalence rate has come down drastically from over 6,000/lac population in 1999 to nearly 2,000 cases/lac in 2005 due to early detection of the cases, qualitative treatment and improved cure rate.
The need for reaching the success rate target is justified by its potential epidemiological impact. Several epidemiological models have shown[5] that achieving the 85% success target coupled with a case detection of at least 70% would cause a decline in the annual TB incidence rate of 5-10% in the absence of co-infection with human immunodeficiency virus (HIV). These theoretical assumptions are further corroborated by empirical findings, particularly in the European context. In fact, the TB incidence has been declining rapidly all over Europe over the past century, but the decline has more than doubled following the introduction of effective treatment.[21]
We failed to comment on different TB related problems like multi-drug resistance, HIV co-existence, as no such data was available from the district health authority. However, strategy to collect data on the said issues will be beneficiary for better management. The study was purely based on the data available with the district health authorities. This did not examine the completeness of the data, functioning of existing surveillance system, operational issues related to RNTCP and quality control mechanism particularly in peripheries. So it may or may not simulate with the actual TB situation in terms of distribution and magnitude of TB-related morbidity and/or mortality as the patients also go to the private sector and resort to the treatments provided by the therapies of the alternative medicines, for which there is no record available and this is certainly, the limitation of the secondary data analysis. The importance of treatment outcome monitoring needs to be further stressed and mechanisms explored to maximize progress towards achievement of the targets. Clinicians, public health experts, and policy makers must be convinced of the importance of a standardized approach to monitoring of treatment including a proper evaluation of its implementation. Only by recognizing the key position that treatment outcome monitoring holds in TB control can progress towards elimination be pursued.[3,22] The results and subsequent discussion enabled us to recommend for better management of TB control programs.
Conclusion
The secondary data analysis shows that the new smear sputum positive case detection rate and cure rate of Kangra district has successfully achieved the target of the program. However, high proportion of EP TB has also been detected on account of the presence of medical specialists in the local medical college. Default rate is higher in TU Palampur due to migratory populations. Health management and information system has been observed to be poorly maintained.
Recommendations
Continue investment in the program to sustain progress achieved including as well as involving the private sector of the district;
Investigate the cause of high proportion of EP TB;
Capacity building at TU level strengthens home visits to the registered cases and counseling, particularly to DOTS defaulters. Emphasis has to be laid on IEC activities so that people are motivated and avail the treatment facility under RNTCP for effective management of TB disease. It has to be targeted for social behavioral change rather than informing the community. The responsibility has to be shared both by health providers and community. Studies may be conducted to investigate (i) the causes of default in the area by the patients. (ii) Knowledge, attitude, and perception status of general population and the contact cases of the patient is an important area of study.
Improve health management and information system.
Acknowledgments
We gratefully acknowledge the cooperation we received in the secondary data analysis of RNTCP program from the Offices of Chief Medical Officer and District Tuberculosis Officer, Kangra at Dharamshala and in five TU of Kangra, Himachal Pradesh. We owe our special thanks for guiding support from National Institute of Epidemiology, Chennai, India.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Dubos R, Dubos J. London: Victor Gollancz; 1953. The White Plague, Tuberculosis, Man and Society. [Google Scholar]
- 2.United Nations Development Programme 2003. Human development Report 2004, Report of Director General WHO. [Last retrieved on 2012 Sept 14]. Available from: http://hdr.undp.org/en/media/hdr04_complete.pdf .
- 3.Global Tuberculosis Control; World Health Organization Report. 2011. [Last retrieved on 2012 Oct 14]. Available from: http://www.who.int/tb/publications/global_report .
- 4.TB India 2007. Status Report Revised National TB Control Programme. [Last retrieved on 2012 Sept 14]. Available from: http://www.tbcindia.nic.in/pdfs/TB%20India%202007.pdf .
- 5.Stockholm: European Centre for Disease Prevention and Control; 2009. [Last retrieved on 2012 Nov 23]. European Centre for Disease Prevention and Control/WHO Regional Office for Europe: Tuberculosis surveillance in Europe 2007. Available from: http://www.ecdc.europa.eu/en/publications/Publications/0904_SUR_Tuberculosis_Surveillance_in_Europe.pdf . [Google Scholar]
- 6.Khatri GR, Frieden TR. Controlling tuberculosis in India. [Last retrieved on 2012 Oct 14];N Engl J Med. 2002 347:1420–5. doi: 10.1056/NEJMsa020098. Available from: http://www.nejm.org/doi/pdf/10.1056/nejmsa020098 . [DOI] [PubMed] [Google Scholar]
- 7.Global Tuberculosis control, Surveillance, Planning and Financing, WHO: Report. 2004. [Last retrieved on 2012 Oct 14]. Available from: http://www.who.int/tb/publications/global_report/2004/contents.pdf .
- 8.Thorson A, Hoa NP, Long NH, Allebeck P, Diwan VK. Do women with tuberculosis have a lower likelihood of getting diagnosed? Prevalence and case detection of sputum smear positive pulmonary TB, a population-based study from Vietnam. J Clin Epidemiol. 2004;57:398–402. doi: 10.1016/j.jclinepi.2002.11.001. [DOI] [PubMed] [Google Scholar]
- 9.Gupta SN, Gupta N. Evaluation of revised national tuberculosis control program, district Kangra, Himachal Pradesh, India, 2007. Lung India. 2011;28:163–8. doi: 10.4103/0970-2113.83970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Himachal Pradesh: Health at Glance, Department of Health and Family Welfare; 2006. [Google Scholar]
- 11.Himachal Pradesh: Health at Glance, Department of Health and Family Welfare; 2005. [Google Scholar]
- 12.TB India 2006, Status report Revised National TB Control Programme. [Last retrieved on 2012 Nov 23]. Available from: http://www.tbcindia.nic.in/pdfs/Annual%20Report%20TB%202006.pdf .
- 13.Kangra at Dharamshala, Himachal Pradesh, India: Office of Chief medical Officer; 2006. [Google Scholar]
- 14.Kangra at Dharamshala, Himachal Pradesh, India: Office of District Tuberculosis Officer; 2006. [Google Scholar]
- 15.TB Manual Hong Kong SAR. 2006. [Last retrieved on 2012 Nov 23]. Available from: http://www.info.gov.hk/tb_chest/doc/Tuberculosis_Manual2006.pdf .
- 16.Gupta SN, Gupta N. Abuja, Nigeria: Africa Region; 2011. Increased extra-pulmonary tuberculosis diagnosed and treated under RNTCP in district Kangra from 2000 to 2004-18th Union conference. [Google Scholar]
- 17.Himachal Pradesh: Health at Glance, Department of Health and Family Welfare; 2011. [Google Scholar]
- 18.Chennaveerappa PK, Siddharam SM. Treatment outcome of tuberculosis patients registered at DOTS centre in a teaching hospital, South India. Int J Biol Med Res. 2011;2:487–9. [Google Scholar]
- 19.Geneva: World Health Organization; 2009. [Last retrieved on 2012 Nov 23]. Global tuberculosis control: A short update to the 2009 report. Available from: http://www.who.int/tb/publications/global_report/2009/update/tbu_9.pdf . [Google Scholar]
- 20.Revised National Tuberculosis Control Programme (RNTCP)-Fact sheet, Himachal Pradesh State, Report-2009, Jun. 2009:17–9. [Google Scholar]
- 21.Smith I. What are the global targets for tuberculosis control, and what is the basis of these targets? In: Frieden T, editor. Toman's Tuberculosis: Case Detection, Treatment, and Monitoring-Questions and Answers. 2nd ed. Geneva: World Health Organization; 2004. [Last retrieved on 2012 Nov 23]. Available from: http://www.tbrieder.org/publications/books_english/toman_2pdf . [Google Scholar]
- 22.Manissero D, Hollo V, Huitric E, Ködmön C, Amato-Gauci A. Analysis of tuberculosis treatment outcomes in the European Union and European Economic Area: Efforts needed towards optimal case management and control. [Last retrieved on 2012 Oct 14];Euro Surveill. 2010 15:19514. Available from: http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=19514 . [PubMed] [Google Scholar]


