Abstract
Background:
Malaria threatens the life of under-five in rural Nigerian families. Although, factors that influence malaria in under-five are manifold. However, family biosocial factors may contribute to the variability of the clinical picture.
Aim:
To determine proximate family biosocial variable associated with severe malaria among under-five children in a resource-poor setting of a rural hospital in Eastern Nigeria.
Materials and Methods:
A cross-sectional study carried out on the families of under-five managed for malaria. Data extracted included family biosocial variables and diagnosis. An under-five child was defined to have malaria if the mother gave complaints of fever, vomiting, and other symptoms suggestive of malaria, had body temperature exceeding 37.5°C with the asexual forms of Plasmodium falciparum detected on the peripheral blood film. Severe malaria is the malaria that presents with life-threatening features like severe anemia and cerebral malaria.
Results:
The prevalence of severe malaria was 31.8% The family biosocial variables significantly associated with severe malaria were maternal low level of education (P = 0.031), family size >4 (P = 0.044), low social class of the family (P = 0.025), nonliving together of parents (P = 0.011), and poor access to health facilities (P = 0.038). The most significant predictor of severe malaria was nonliving together of parents (P = 0.000, odds ratio = 3.08, confidence interval = 1.64-5.10).
Conclusion:
This study has demonstrated that some family biosocial variables are associated with severe malaria. These families should constitute at risk families that could be targeted for malaria interventional programs.
Keywords: Family variables, hospital, Nigeria, rural, severe malaria, under-five
Introduction
Malaria is a major threat to socioeconomic and demographic development in Africa and accounts for a large proportion of the global burden of infectious diseases especially in sub-Saharan Africa.[1,2] These are the same countries in which large numbers of children still die from treatable and preventable diseases such as malaria and other socioeconomic and demographic ills.[3] Studies have shown that malaria diseases have continued to plague under-five Nigerians in rural[4,5] and urban[6] areas of Imo state, South-eastern Nigeria and constituted the most common cause of emergency medical admissions in Enugu, South-eastern Nigeria,[7] Abuja, capital territory of Nigeria,[8] Ilorin, Western, Nigeria,[9] and in other sub-Saharan African countries such as Uganda.[10]
The clinical manifestations of falciparum malaria in under-five children in Nigeria are characterized by two predominant outcomes: Nonsevere (uncomplicated) or severe (complicated) falciparum malaria.[11] Although, malaria may present initially with benign symptoms if not treated promptly and adequately can lead to life-threatening complications.[12] The common complications of severe malaria among under-five children in Nigeria include severe anemia, cerebral malaria, respiratory distress, and hypoglycemia.[13,14] The prevalence of severe malaria disease has been reported in Enugu, South-eastern Nigeria (18.4%),[7] Ilorin, Western, Nigeria (35.0%),[9] and other sub-Saharan African nations like Uganda (39.4%).[10] Most of the deaths from malaria in under-five Nigerian children are due to severe malaria especially that which presents with severe anemia and cerebral malaria.[5] Similarly, most under-five children dying from malaria do so within 24-72 h of onset of severe symptoms,[5,15] the ease at which malaria is recognized by families of under-five children is, therefore, critical in reducing its severity.[16,17]
The health status of under-five children is influenced by predisposing, promotional, and enabling risk factors and these factors interact to contribute to the morbidity and mortality.[14,18,19] The predisposition factors include family-related factors such as family biosocial characteristics such as parental age, education, and occupation, type of family, size of the family, and poor recognition of symptoms of malaria infection among others. These family biosocial variables have been documented to influence important under-five health indices such as infant and under-five mortality rates.[18,19] The enabling factors include proximity to health facility, availability of funds for direct and indirect cost of care, health insurance and existence of social network.[18,19,20,21]
In rural Nigerian families, three quarters of all child health care takes place at proximal context of the child's home,[16] where mothers generally have the primary responsibility of recognizing a sick under-five child and taking the child to the health facility. Failure of the mothers of under-five children to recognize malaria disease in the under-five child has serious implications for Roll Back Malaria Initiative (RBMI), Millennium Development Goals, and house-hold Integrated Management of Childhood Illnesses (IMCI) as regards malaria disease.[5,22] Family biosocial factors are, therefore, an integral part of family health and are essential for the wellness of under-five child.[22] It is reported that family with favourable biosocial advantages have a greater health awareness,[20,21] culminating in better health practices such as health care seeking for malaria disease especially among the under-five children. It is yet to be ascertained in the study area whether family biosocial variables have any impact on the clinical picture of malaria, since malaria disease constitutes the most common infectious disease among the under-five children in the study area.[4,5,6] Identification of these family biosocial disadvantages and bridging the differences will improve the health status of under-five children as regards severe malaria disease in the resource-poor environment of the study area. The study was prompted by the need to document some of the family factors that might be responsible for the variable presentation of malaria despite effort to reduce the burden of malaria especially its severe manifestation. It is against this background that the authors aimed at determining proximate family biosocial variables associated with severe malaria disease among under-five children in a resource-poor setting of a rural hospital in Eastern Nigeria.
Materials and Methods
Ethical imperatives
Ethical certificate was obtained from the ethics committee of the hospital. Informed verbal consent was also obtained from respondents included in the study.
Study design
This was a hospital-based descriptive cross-sectional study carried out from June 2008 to June 2011.
Study area
Amurie-Omanze is a rural community in Imo State, South-eastern Nigeria. Imo State is endowed with abundant mineral and agricultural resources with supply of professional, skilled, semiskilled, and unskilled manpower. Economic and social activities are low compared with industrial and commercial cities such as Onitsha, Port Harcourt, and Lagos in Nigeria.
The climate of Imo State is essentially tropical with very high temperature within the months of November to March and seasonal rainfall. Two seasons are prominent in the State, namely rainy and dry seasons. The dry season starts in November and lasts until March, while rainy season starts in April and ends in October. The mean monthly temperature of Imo State during the dry season is 34°C, while it is 30°C in rainy season. It has relative humidity of about 60%-80% throughout the year. Its mean annual rainfall is between 2000 and 2500 mm.
Study setting
This study was carried out on a cross section of 220 mothers of under-five children who were managed for malaria at St. Vincent De Paul Hospital, Amurie-Omanze, a rural General Hospital in Isu Local Government Area of Imo State, Eastern Nigeria. The hospital renders 24 h service daily including public holidays to the community and its environs.
Sample size determination
Sample size estimation was determined using the formula[23] for calculating minimum sample size for descriptive studies: N = Z2pq/d2 where N = Minimum sample size, Z = Standard normal deviation usually set at 1.96 which corresponds to 95% confidence interval (CI), P = Proportion of the population estimated to have a particular characteristic. Proportion was taken from previous study in Enugu, South-eastern Nigeria[7] = 18.4% (0.18). q = 1.0 − p = 1.0−0.18 = 0.82, d = degree of accuracy set at 0.05. Hence, N = (1.96)2 × 0.18 × 0.82/(0.05)2 = 226. Therefore, N = 226. However, a total of 220 respondents were used based on the time frame for the study.
Inclusion and exclusion criteria
After clinical evaluation of the under-five patients, those who had presumptive diagnosis of malaria had malaria diagnosis confirmed by thick blood film microscopy using standard Giemsa staining technique.[11] The study population were recruited from among mothers whose under-five children were managed for confirmed malaria at the study center during the study period. Only married women whose husbands were alive were interviewed for family biosocial data. The under-five children who were brought to the hospital by other care givers were excluded from the study. More so, under-five children who needed specialized diagnostic investigations and care were referred out and excluded from the study.
Methods
Detailed enquiries were made about family biosocial characteristics such as parental age, occupation and educational status; and family structure such as type of marital union, family size, and living together of parents.
The social classification of the family[24] was based on three-point classification described in a previous study to suit Nigerian environment. This method considers fathers occupation and mother's educational attainment and places families in upper, middle, and lower social class. The fathers occupation is categorized into three (1, 2, 3), while the mothers educational attainment is categorized into three (0, 1, 2).
Scores Fathers occupation
Professionals, top civil servants, business executives, and politicians.
Middle-level bureaucrats, technicians, skilled artisans, and well-to-do traders.
Unskilled workers and those whose income is at or below the national minimum age.
Scores Mothers level of education
Education up to university level.
Secondary or tertiary below university such as college of education, school of nursing.
No schooling or up to primary level only.
Adding the scores from father's occupation and mother's level of education gives the social class:
Social class I or upper class: Scores of 1 or 2,
Social class 2 or middle class: Scores of 3,
Social class 3 or lower class: Scores of 4 or 5.
Operational definitions
The authors operationally defined a family as made up of a couple and their children. The authors defined under-five patients as a period of childhood from 0 to 59 months.
An under-five child was defined to have malaria if the mother gave complaints of fever, vomiting, and other symptoms suggestive of malaria, had body temperature exceeding 37.5°C with the asexual forms of Plasmodium falciparum detected on the peripheral blood film. The clinical presentation of malaria is categorized into nonsevere and severe malaria disease. A child is defined to have nonsevere malaria when he/she has case definition of malaria without severe malaria features, while severe malaria refers to the malaria that presents with the case definition of malaria in addition to the life-threatening features such as severe anemia and cerebral malaria. Severe malaria anaemia was taken as haemoglobin level of <5.0g/dL, while cerebral malaria refers the presence of altered level of consciousness with or without convulsion.
The educational attainment of the parents was classified into low level of education which was made up of those with no formal and primary education while high level educational attainment refers to those parents with secondary and tertiary education. Accessibility to health facilities is categorized into two: Easy access refers to availability of health services within 30 min walk. This ensures that treatment for malaria is available as near the home as possible. This is one of the major strategies for reducing the burden of malaria disease. Poor access refers to nonavailability of health services within 30 min walk.
Statistical analysis
The results generated were analyzed using software Statistical Package for Social Sciences (SPSS) version 13.0, Microsoft coperation, Inc. Chicago, IL, USA. Categorical variables were described by frequencies and percentages. Bivariate analysis involving chi-square test was used to test for the significance of associations between categorical variables. Furthermore, to identify family biosocial variables independently associated with severe malaria disease, univariate logistic regression analysis was performed at 95% confidence limit. The level of significance was set at P < 0.05.
Results
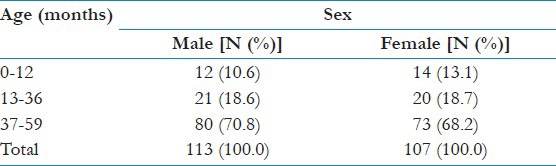
A total of 220 under-five children were studied during the study period. Of the 220 under-five children who were managed for malaria during the study period; 150 (68.2%) had uncomplicated malaria, while 70 (31.8%) had severe malaria disease. The ages of the under-five children ranged from 4 days and 59 months with mean age of 31.0 ± 8.10 months. There were 113 (51.4%) males and 107 (48.6%) females with male to female ratio of 1.1:1.0 [Table 1].
Table 1.
Age and sex distribution of the under-five children
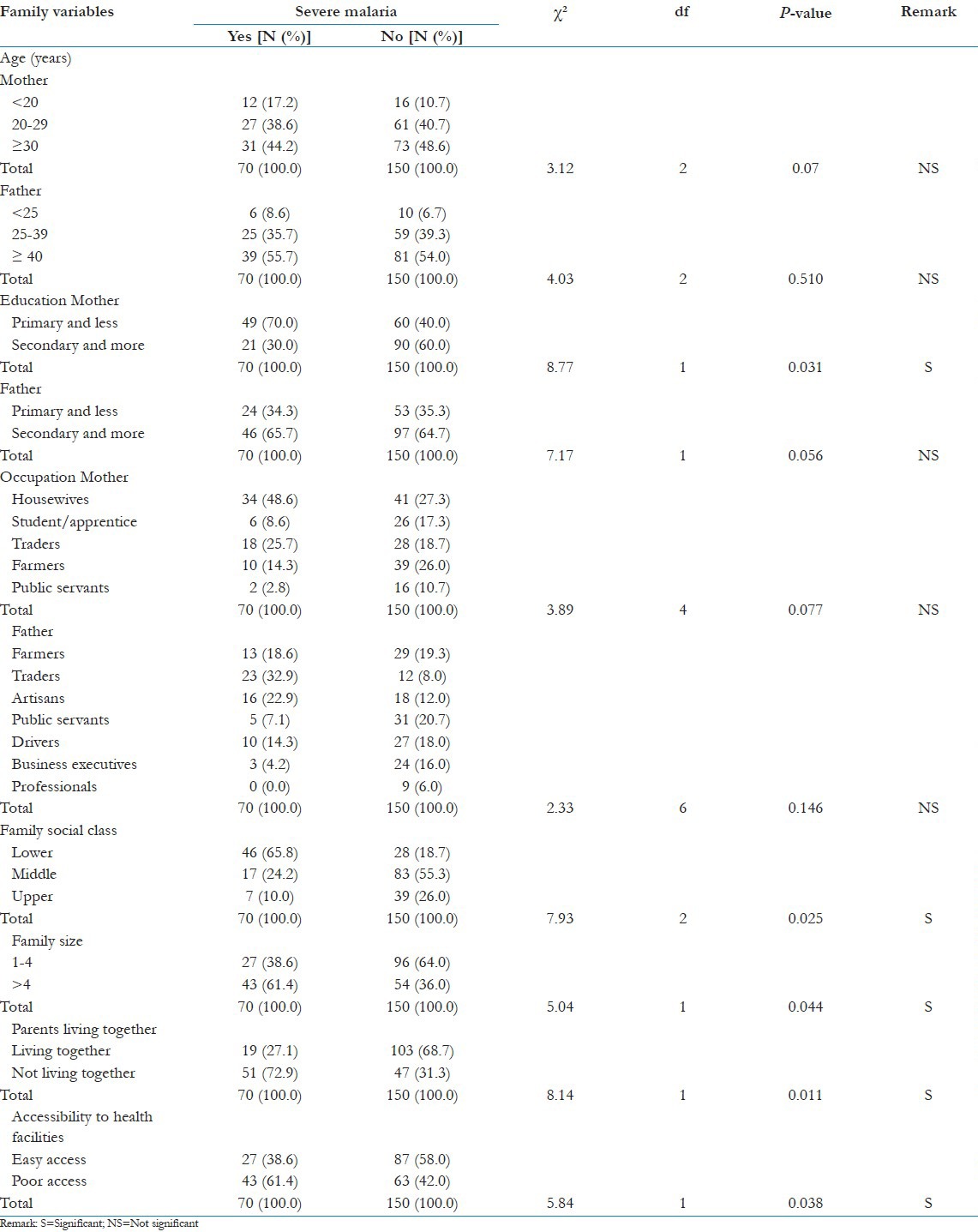
Bivariate analysis of family biosocial variables as related to severe malaria showed that family variables such as maternal low educational level (X2 = 8.77, df = 1, P-value = 0.031); family size of >4 (X2 = 5.04, df = 1, P-value = 0.044), family lower social class (X2 = 7.93, df = 2, P = 0.025), nonliving together of parents (X2 = 8.14, df = 1, P-value = 0.011) and poor access to health facilities (X2 = 5.84, df = 1, P = 0.038) were statistically significant, while other family variables such as parental age, parental occupation, and fathers educational attainment were not statistically significant [Table 2].
Table 2.
Family biosocial variables as related to severe malaria
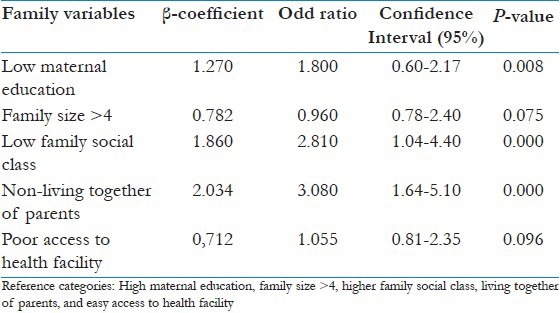
However, on univariate logistic regression of these statistically significant family biosocial variables, nonliving together of parents, lower family social class, and lower maternal educational attainment remained statistically significant with nonliving together of parents being most statistically significant predictor of severe malaria. A significantly higher proportion of under-five children whose parents were not living together had severe disease compared with those living together [odds ratio (OR) = 3.08, CI = 1.64 − 5.10, P-value = 0.000]. The under-five children whose parents were not living together were three times more likely to have severe disease compared with those living together. More so, lower family social class had an OR of 2.81 suggesting that lower family social class was two and half times more likely to have severe disease compared with other family social classes [Table 3].
Table 3.
Predictors of severe malaria disease
Discussion
The prevalence of severe malaria was 31.8%. This prevalence is higher than 18.4% reported in Enugu, South-eastern, Nigeria[7] but lower than 35.0% reported in Ilorin, Western Nigeria,[9] and 39.4% reported in sub-Saharan African country, Uganda.[10] Accordingly, reports from stable and unstable malarial regions of Africa have documented relative frequencies of severe malaria in African children.[25] The outcomes of malaria disease in under-five children have been documented to be influenced by interplay of epidemiological[14,26] and immunological factors.[13] The family biosocial factor is one of the epidemiological factors that influence malaria disease transmission and progression from uncomplicated malaria to severe disease. There is growing evidence that with appropriate key family health practices and household-IMCI as regards malaria disease, its severe presentation can be drastically reduced. Since under-five children cannot take health decisions by themselves, spousal decision making is, therefore, critical in management of malaria disease. The prospects of curtailing the morbidity and mortality from severe malaria among the under-five children, therefore, lie on the epidemiological characteristics of the proximal context of the child's family which constitute a unit of care.[22,27] This study has, therefore, demonstrated that malaria disease is still an issue of serious medical importance in rural Nigeria. Despite the years of formulation and implementation of malaria control intervention programs such as RBMI,[28] the impact of program targets on under-five morbidity and mortality has been below expectation especially in rural Nigerian families.[4,5,6,7,8,9,22,29]
This study observed that under-five children whose mothers had low level of education had severe malaria disease more than those who had high level of education. This could be a reflection of the negative impact of low level of education.on child health especially on decision-making process as regards health seeking behavior for malaria disease.[29] This is compounded by the relatively poor receptivity of awareness of information on malaria control.[4,22] If the under-five children's mothers are aware that malaria could present with life-threatening complications and its consequences then it may be easier to educate and counsel them on the needed malaria intervention measures. Information based on knowledge is power; this knowledge needs to be delivered as part of comprehensive health package during clinical consultation with family of under-five children whose mothers have low level of education. Education of such families on malaria disease should be an integral part of family-oriented intervention approach for malaria disease and improving the functional literacy of mothers of under-five children in this regard is likely to impact positively on severe malaria disease.[30]
The size of the family significantly influenced presentation with severe malaria disease..This finding is in consonance with the finding that large family size does not facilitate good family support such as early decision making especially for malaria disease.[22,27] This could be due to psychosocial demands of parenting in a family with large family size which may lead to division of parental attention and role. More so, large family size is generally characterized by higher rate of family stress and distress as well as more family disruption that militate against adequate child care especially in a milieu of limited and diluted family resources.[17,22,27] In addition, as family size increases, there is increased distance of the under-five children from intimate and appropriate parental care especially the traditional maternal care.
This study has shown that under-five children who presented with severe malaria disease came significantly from family of lower social class. This finding is in agreement with the reports that families at socioeconomic disadvantage have low level of health literacy for good family upkeep.[22,27] More so, lack of financial resources has been shown to constitute a barrier to health care.[31] This could be attributed to lack of family financial resources. This economic circumstance affects the family socioeconomic life and their ability to get health facility care that is not provided for or indeed not sponsored. Imposition of health facility fees and charges, although aimed at improving the financial prowess of the health system, has also contributed to behavior changes such as avoiding health care, seeking traditional and alternative care, and late presentation to health facilities among others. For families in socioeconomic disadvantage, sudden occurrence of under-five child's illness affects family welfare because the cost of health care becomes an added demand on already strained family finances. This family variable has been documented to adversely affect interventional measures for malaria in the study area.[4,5,22] It is, therefore, envisaged that any interventional program aimed at reducing severe malaria disease should, therefore, target these families with lower social class amidst addressing other diverse factors that predispose to malaria disease.
This study has shown that nonliving together of spouse has significant effect on severe malaria disease. Nonliving together of husband and wife has been traditionally assumed to offer poor psychosocial environment for child health. It seems that nonliving together of spouse could have resulted in failure of the mother to take urgent decision on child illness. This could be due to the absence of the husband to persuade the wife to take the sick child to the health facility. The nonliving together of the parents may have negated husband involvement and participation on family health decision making. In addition, nonliving together of parents seems to disrupt mother's psychological wellbeing especially when the under-five child is sick. This finding has buttress the reports that apart from the mothers central and traditional role as a home maker and primary child's care giver, the husband-wife habitation within the household is important for child health.[17,22,27]
This study observed that under-five children whose family lived beyond 30 min walk to a health facility had severe malaria more than those who lived within 30 min radius of a health facility. This could be attributed to poor access to health facilities. This has buttressed the reports that reduction of morbidity and mortality from severe malaria depends largely on easy access and early presentation to health facilities.[5,10,25] Severe malaria has been documented to develop rapidly from uncomplicated malaria disease; therefore, proximity to a health facility is indispensable in early intervention for under-five children with life-threatening malaria disease.[28] As a result of poor access to health facilities, parents may not be willing to take their sick children to the health facilities since they felt that the health facilities were situated at a long distance and they did so only when other alternative remedies had failed and severe complications emanated. This, therefore, makes a strong call to action for government and private multifaceted approach aimed at ensuring that under-five children suffering from malaria disease have easy access to treatment.
The most significant predictor of severe malaria disease was nonliving together of spouse. This association could be explained by the absence of spousal discussion on child's health.[22] Adopting the desired behavior[32] by family of under-five children for malaria disease is a process, not an event. Families receive health education and promotion messages on malaria disease, check if it is acceptable to one's family before decision is implemented. This spousal concurrence and participation are largely absent in families where parents do not live together.[22] Furthermore, since most women especially in rural Nigeria depend on their husband for approval and financial support, nonliving together of the couple delay this support and prolong decision making process for a sick under-five child. In addition, families where husbands and wives do not live together are more unlikely to adhere to health message and information after discussion. More so, it seems that non-living together of husband and wife promotes poor family psychosocial well-being to overcome the problem of early treatment seeking behavior for a sick child.
Study implications
Malaria disease is endemic in the study area and it is commonly overlooked as a mild disease, whereas its devastating effects are enormous. One of the pillars identified that reduces malaria burden in under-five children is early recognition and prompt treatment of malaria disease.
The study of any population characteristics derives information from the families which constitute the most basic units and under-five children constitute special at risk group of the family. However, families of under-five children in biosocial disadvantage may not recognize the threat of severe malaria disease which may rapidly progress to death. Elucidation of the role of family biosocial characteristics in improving the under-five children's health as regard malaria is important for effective under-five health services and attainment of millennium development goal 4 by 2015. This study is, therefore, very valuable as regards malaria disease which constitutes the most common cause of emergency medical admission among the under-five children in the study area.[5] This malaria emergency medical condition predisposes these children to higher risk of disability and mortality. It is envisaged that the unfavorable influence of malaria on under-five morbidity and mortality may change in the future as a result of family biosocial progress and diverse changes.
Study limitations
The limitations of this study are recognized by the authors. First and foremost, the sample for the study was drawn from hospital attendees in the community. Hence, the findings of this study may not be general conclusions regarding the influence of family biosocial variables on severe malaria disease among the under-five children in the study area. Generalization of the results of this study to the entire community and its environs should be done with caution. Furthermore, the report of this study was on the most common presentation of severe malaria (severe anaemia and cerebral malaria) in the study area.[5] The clinical significance of other subtypes of severe malaria syndromes is recognized. Furthermore, the sample size for the study was relatively small, but this was the number of patients seen within the proposed duration of the study.
Conclusion
This study has shown that severe malaria disease may be proximally associated with certain family biosocial variables. Families of under-five children with these biosocial disadvantages should constitute at risk families for malaria disease control interventions. Clinicians attending to under-five children with malaria should be aware of these biosocial characteristics during clinical encounter with these families in the study area. There is also the need to create enabling family environment that recognized malaria as a serious family health problem focusing strongly on family health education, promotion, and risk reduction.
Acknowledgment
The authors are grateful to Rev. Sister Francisca Eya of St. Vincent de Paul Hospital, Amurie-Omanze for permission for the study.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Gallup JL, Sachs JD. The economic burden of malaria. Am J Trop Med Hyg. 2001;64:85–96. doi: 10.4269/ajtmh.2001.64.85. [DOI] [PubMed] [Google Scholar]
- 2.Breman JG, Alilio MS, Mills A. Conquering the intolerable burden of malaria: What's new what's needed: A summary. Am J Trop Med Hyg. 2004;71:1–15. [PubMed] [Google Scholar]
- 3.Sachs J, Malaney P. The economic and social burden of malaria. Nature. 2002;415:680–5. doi: 10.1038/415680a. [DOI] [PubMed] [Google Scholar]
- 4.Iloh GUP, Amadi AN, Nwankwo BO, Ugwu VC. Common under-five morbidity in south-eastern Nigeria: A study of its pattern in a rural mission General Hospital in Imo state. Niger J Med. 2011;22:99–104. [PubMed] [Google Scholar]
- 5.Iloh GUP, Ofoedu JN, Njoku PU, Amadi AN, Godswill-Uko EU. The Magnitude of Under-five Emegencies in a Resource-poor Environment of a Rural Hospital in Eastern Nigeria. Implication for Strenghtening the House-hold and Community-integrated Management of Childhood illnesses. N Am J Med Sci. 2012;4:344–9. doi: 10.4103/1947-2714.99514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nwolisa CE, Erinugha AU, Ofoleta SI. Pattern of morbidity among pre-school children attending the children's outpatient clinic of Federal Medical Centre, Owerri, Nigeria. Niger J Med. 2005;14:378–80. doi: 10.4314/njm.v14i4.37191. [DOI] [PubMed] [Google Scholar]
- 7.Ibeziako SN, Ibekwe RC. Pattern and outcome of admissions in the children's emergency room of the University of Nigeria Teaching Hospital, Enugu. Niger J Paediatr. 2002;29:103–7. [Google Scholar]
- 8.Okechukwu AA, Nwalozie C. Morbidity and mortality pattern of admissions into the emergency paediatric unit of University of Abuja Teaching Hospital, Gwagwalada. Niger J Med. 2011;20:109–13. [PubMed] [Google Scholar]
- 9.Olanrewaju WI, Johnson AW. Pattern and outcome of paediatric malaria admissions in Ilorin. Nig J Paed. 2001;28:87–8. [Google Scholar]
- 10.Idro R, Aloyo J. Manifestations and quality of emergency care and outcome of severe malaria in mulago Hospital, Uganda. Afr Health Sci. 2004;4:50–7. [PMC free article] [PubMed] [Google Scholar]
- 11.Abuja, Nigeria: National Malaria and Vector Control Division, FMOH; 2005. FMOH. National Antimalaria Treatment Policy; pp. 1–66. [Google Scholar]
- 12.Orimadegun AE, Amodu OK, Olumese PE, Omotade OO. Early home treatment of childhood fevers with ineffective antimalarials is deleterious in the outcome of severe malaria. Malar J. 2008;7:143. doi: 10.1186/1475-2875-7-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Anumudu CI, Okafor CM, Ngwumohaike V, Afolabi KA, Nwuba RI, Nwagwu M. Clinical manifestation and immunological response in severe paediatric malaria in Adeoyo hospital, Ibadan. Afr J Med Med Sci. 2004;33:57–63. [PubMed] [Google Scholar]
- 14.Anumudu CI, Okafor CM, Ngwumohaike V, Afolabi KA, Nwuba RI, Nwagwu M. Epidemiological factors that promote the development of severe malaria anaemia in children in Ibadan. Afr Health Sci. 2007;7:80–5. doi: 10.5555/afhs.2007.7.2.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.WHO. The roll back malaria strategy for improving access to treatment through home treatment of malaria. [Last accessed on 2012 Oct 26]. Available from: http://www.WHO/htm/mal/2005.1101 .
- 16.Salako LA, Brieger WR, Afolabi BM, Umeh RE, Agomo PU. Treatment of childhood fevers and other illnesses in three rural Nigerian communities. J Trop Paed. 2001;47:230–8. doi: 10.1093/tropej/47.4.230. [DOI] [PubMed] [Google Scholar]
- 17.Tumwaesigire S, Watson S. Health seeking behaviour by families of children suspected to have malaria in Kabale, Uganda. Afr Health Sci. 2002;2:94–8. [PMC free article] [PubMed] [Google Scholar]
- 18.Obionu CN. Enugu: Ezu Books Ltd; 2007. Primary Health Care for Developing Countries; pp. 231–233. [Google Scholar]
- 19.Lawoyin TO. Risk factors for infant mortality in a rural African community. J R Soc Promot Health. 2000;121:114–8. doi: 10.1177/146642400112100213. [DOI] [PubMed] [Google Scholar]
- 20.Oleribe EO, Alasia DD. Socio-demographic variables and family health: A prospective study of a Katcha in North-central Nigeria. Niger J Med. 2006;15:427–9. doi: 10.4314/njm.v15i4.37262. [DOI] [PubMed] [Google Scholar]
- 21.Nnebue CC, Ifeadike GO, Nworah NG, Duru CB. The effect of socio-demographic status of mothers on the management of febrile illnesses among under-fives that presented in a tertiary hospital in South-east Nigeria: A two-year review. Afr Med J. 2010;1:27–30. [Google Scholar]
- 22.Iloh GU, Amadi AN, Obikwu CE. Family variables influencing the use of insecticide treated nets among under-five children treated for malaria in a rural hospital in South-Eastern Nigeria. Port Harcourt Med J. 2012;6:365–75. [PubMed] [Google Scholar]
- 23.Araoye MO. Research Methodology with Statistics for Health and Social Sciences. 1st edn. Ilorin: Nathadex Publishers; 2004. Sample size determination; pp. 115–121. [Google Scholar]
- 24.Emechebe GO, Emodi IJ, Ikefuna AN, Ilechukwu GC, Igwe WC, Ejiofor OS, et al. Demographic and socio-cultural characteristics of sickle anaemia children with positive hepatitis B surface antigenaemia in a tertiary health facility in Enugu. Niger J Clin Pract. 2010;13:317–20. [PubMed] [Google Scholar]
- 25.World Health Organization. Severe falciparum malaria. Trans Roy Soc Trop Med Hyg. 2000;94:1–45. [PubMed] [Google Scholar]
- 26.Greenwood BM. The epidemiology of malaria. Ann Trop Med Parasitol. 1997;91:763–9. doi: 10.1080/00034989760518. [DOI] [PubMed] [Google Scholar]
- 27.Inem AV, Ayankogbe OO, Obazee M, Ladipo MM, Udonwa NE, Odusote K. Conceptual and contextual paradigm of the family as a unit of care. Niger Med Pract. 2004;45:9–13. [Google Scholar]
- 28.UNICEF. Malaria prevention and treatment. Prescriber. 2000;18:1–16. [Google Scholar]
- 29.Akoqun OB, John KK. Illness-related practices for the management of childhood malaria among the Bwatiye people of north-eastern Nigeria. Malar J. 2005;4:13. doi: 10.1186/1475-2875-4-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Osibogun A, Odeyemi KA, Okoye SO. Female Functional Literacy for Health (FFLH): Experience from the field. Niger Med Pract. 2000;48:110–5. [Google Scholar]
- 31.Scheppers E, van Dongen E, Dekker J, Geertzen J, Dekker J. Potential barriers to the use of health services among ethnic minorities: A review. Fam Pract. 2006;23:325–48. doi: 10.1093/fampra/cmi113. [DOI] [PubMed] [Google Scholar]
- 32.Prochoska JO, Velicer WF. The transtheoritical model of health behaviour change. Am J Health Promot. 1997;12:38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]


