Abstract
We compared the infectivity and growth rates of 12 strains of Orientia tsutsugamushi in a cell culture system. ECV304 cells were infected with O. tsutsugamushi strains for 4 hr, and the culture was maintained for 72 hr. Immunofluorescence (IF) staining was performed at 4, 24, 48, and 72 hr after inoculation (hpi), and IF-positive foci were enumerated. The AFSC-4 strain, which is known to be insensitive to doxycycline, showed higher numbers of IF-positive foci than the other 11 strains at 4, 24, 48, and 72 hpi, which may explain its apparent insensitivity to antibiotics.
Keywords: Orientia tsutsugamushi, Scrub typhus, Virulence, Drug resistance
Orientia tsutsugamushi is a fastidious, intracellular, gramnegative bacterium that causes scrub typhus followed by a chronic latent infection [1]. Various antibiotics such as chloramphenicol, tetracyclines, macrolides, and rifampin have shown efficacious clinical outcomes [2]. In 1996, delayed clinical improvement was reported in patients who were infected by doxycycline-insensitive O. tsutsugamushi strains in Chiang Rai, Thailand [3]. After treatment with antibiotics, mice infected with these strains showed higher mortality rates than those infected with the Karp strain, an antibiotic-susceptible strain [3, 4]. In vitro resistance to doxycycline has also been observed [3, 5]. However, there has been no investigation into the mechanism responsible for the delayed defervescence in scrub typhus.
We previously performed several experiments to characterize the antibiotic susceptibility of O. tsutsugamushi strains. During these experiments, the bacterial counts in cultures of the AFSC-4 strain, a doxycycline-insensitive strain [5], were higher than those in cultures of the Boryong strain, an antibiotic-susceptible strain, regardless of whether these cultures contained antibiotics. We hypothesized that if the AFSC-4 strain was capable of growing more rapidly than other strains, a higher amount of bacteria would be present at the time of antibiotic susceptibility testing. Thus, the rapidly growing strain would appear to be resistant to antibiotics, even when the antibiotic susceptibilities of these strains might not be different from one another. To verify this hypothesis, we compared the infectivity and growth rates of various O. tsutsugamushi strains.
Twelve strains of O. tsutsugamushi were evaluated in this study: 6 strains were laboratory-adapted strains and the other 6 were clinical isolates. The AFSC-4 strain was kindly provided by Dr. Daniel Strickman, Naval Medical Research Institute, Bethesda, MD, USA. Other laboratory-adapted strains were Boryong, Gilliam (ATCC VR-312), Karp (ATCC VR-150), Kato (Niigata strain), and Kuroki. The 6 clinical isolates were passaged 4-6 times in ECV304 cells after isolation from patients and stored at -70℃ until use. Sequence analysis of the gene encoding the 56-kDa type-specific antigen of O. tsutsugamushi identified these isolates as the following genotypes: Boryong (Kuroki clade), Neimeng-65 (Gilliam clade), Yonchon (Japanese Gilliam clade), Je-cheon (Karp-related clade), and Young-worl (Saitama clade) [6].
Stock solutions of each O. tsutsugamushi strain were inoculated onto monolayers of ECV304 cells seeded in culture flasks (75 cm2). When the infected ECV304 cells showed maximum cytopathic effects, the degree of infection of ECV304 cells as assessed by immunofluorescence (IF) staining was found to be approximately equal in each experiment. The cells were disrupted with glass beads and centrifuged at 350 × g for 5 min. To avoid the death of ECV304 cells by overgrowth of O. tsutsugamushi within 72 hr, the resultant supernatant was divided equally into 40 aliquots, of which 4 aliquots were used. The amount of each inoculum was one-tenth the amount that is usually used in antibiotic susceptibility tests in our laboratory. Each aliquot was inoculated onto monolayers of ECV304 cells grown in shell vials and incubated for 4 hr. At the end of the initial incubation period, the inocula were replaced with fresh medium and the cultures were maintained for 72 hr. Immunofluorescence staining was performed at 4, 24, 48, and 72 hr post-inoculation (hpi) with O. tsutsugamushi.
ECV304 cells infected with each strain of O. tsutsugamushi on a cover slip of the shell vial were fixed with acetone. The infected cells were then stained with mouse polyclonal antibodies in phosphate-buffered saline (PBS) for 30 min at 37℃, washed briefly with PBS Tween-20 (PBST), treated with fluorescein isothiocyanate-conjugated goat anti-mouse immunoglobulin G (Jackson ImmunoResearch, West Grove, PA, USA.) for 30 min in a moist chamber, and finally washed 3 times with PBST. To clearly define O. tsutsugamushi, the host cells were counter-stained with 0.003% Evans blue in PBS. After the slides had been washed, they were placed in mounting medium (Vector Laboratories, Burlingame, CA, USA) and examined at 400 × magnification under a fluorescence microscope (Zeiss, Germany) with a confocal laser scanning system (Bio-Rad, Hercules, CA, USA). The IF-positive foci per field were enumerated.
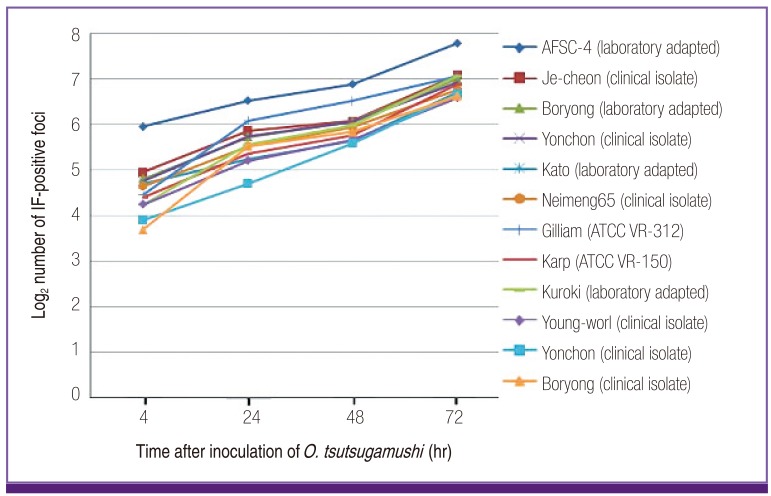
Although the ECV304 cells were inoculated with approximately equal amounts of each O. tsutsugamushi strain, quantification of the bacterial number in each culture at 4 hpi revealed differences among the strains or isolates (Fig. 1). Interestingly, the bacterial count in a culture of the AFSC-4 strain was 2-5 times higher than that in cultures of other strains or isolates at 4 hpi. Additionally, the numbers of the AFSC-4 strain from 4 to 72 hpi were also larger than those of the other strains tested, but with the degree of difference decreasing over time. No consistent differences in the infectivity and growth rates were observed between laboratory-adapted strains and clinical isolates of the same genotype.
Figure 1.
Infectivity and growth rates of Orientia tsutsugamushi strains in ECV304 cells.
The number of immunofluorescence (IF)-positive foci observed in ECV304 cells was quantified at 4, 24, 48, and 72 hr after inoculation (hpi) as an indication of the number of O. tsutsugamushi bacteria present. The amount of bacteria present at 4 hpi represents the infectivity of each O. tsutsugamushi strain or isolate. The increments of IF-positive numbers from 4 to 72 hpi represent the growth rate of each strain or isolate. The AFSC-4 strain demonstrates higher infectivity and larger bacterial numbers than the other 11 strains throughout the experiment.
The present study revealed that the AFSC-4 strain of O. tsutsugamushi had more IF-positive foci than the other strains at 4, 24, 48, and 72 hpi. The bacterial count present at 4 hpi represents the number of O. tsutsugamushi successfully infecting ECV304 cells; and, therefore, is indicative of both its stability during detachment and the degree of infection of the ECV304 cells. The numbers of IF-positive foci at 24, 48, and 72 hpi represent the degree of multiplication. Therefore, the AFSC-4 strain showed either higher infectivity or stability and slower growth than the other 11 O. tsutsugamushi strains. Because the growth rate of O. tsutsugamushi decreases as the bacterium enters the stationary phase of growth from the exponential phase, it is not clear whether the slow growth of the AFSC-4 strain is an intrinsic property.
The present findings were also observed in a previous study [5], wherein the researchers used 3 indices to represent the number of O. tsutsugamushi organisms: the extent of infection, the percentage of maximally infected cells, and the intensity of infection. The first index, the extent of infection (expressed as a percentage of infected cells), was 84% in Karp versus 95% in AFSC-4 strain-infected cultures that did not contain antibiotics. The percentage of maximally infected cells was 60% in the Karp and 68% in AFSC-4 strain-infected cultures containing no antibiotics. The last index, the intensity of infection (measured by calculating the number of O. tsutsugamushi per infected cell), did not reveal any difference between the 2 strains; however, this index was calculated from the former 2 indices and rounding off values of > 50 to 51 during calculation may have influenced the result. In another study investigating antibiotic susceptibility in a cell culture system [4], 2 additional strains-C1 and C27-demonstrated higher infectivity (46% and 43%, respectively) than the Karp strain (39%) in cultures containing no antibiotics. In contrast to these strains, the C3 strain had a lower level of infection (24%) than the Karp strain. These 2 studies revealed that most doxycycline-insensitive strains (with the exception of the C3 strain) were consistently present in larger numbers. Owing to differences in the study design such as cell type, inoculum size, observation period, and staining methods used, the magnitude of the differences in the previous studies are not as prominent as those observed in our study. Considering that we usually observed about 1.2-1.3 times larger numbers of bacteria in AFSC-4 strain-infected cells than that in Boryong strain-infected cells, the reduced inoculum size markedly influenced our present results. In a study comparing the antibiotic susceptibility of the AFSC-4 and Boryong strains, only slight differences in infectivity (63.8% and 63.5%, respectively) were observed [7]; however, infectivity was measured by a flow cytometric assay that might be not sensitive enough to detect small differences [8]. Nevertheless, the results of the present study are in line with those of a previous study performed by Groves and Kelly [9], which suggested that the rapid growth of O. tsutsugamushi strains might be the most important factor in determining pathogenicity.
The present study supports our previous report in which no doxycycline-insensitive strains were found among 37 O. tsutsugamushi isolates in Korea [10]. The strains tested in the present study included clinical isolates of Boryong, Yonchon, Je-cheon, Young-worl, and Neimeng-65 genotypes, which represent the most prevalent genotypes in Korea, with the notable exception of the Kawasaki genotype [11]. None of these strains had higher infectivity or more rapid growth in the present study, suggesting that doxycycline resistance by this mechanism was not present in Korea. Furthermore, if the delayed defervescence in scrub typhus is due to the density of O. tsutsugamushi rather its resistance to antibiotics, a delayed clinical response would be expected with other antibiotics such as azithromycin or rifampin. In actuality, a report by Watt et al [4] revealed that the C3 strain, and particularly C27, resulted in higher mortality rates in mice than the Karp strain when infections were treated with azithromycin. Although azithromycin has been considered efficacious even against infection by doxycycline-insensitive strains, these data suggest that the resistant strains are also azithromycin-insensitive. In addition, a clinical trial evaluating rifampin and doxycycline for the treatment of scrub typhus in Thailand showed that the fever clearance time was 52 hr in doxycycline- and 27.5 hr in rifampin-treated groups [12], compared to 19 hr and 17 hr, respectively, in Korea [13]. Although different study designs and regions might result in some variation in these results, fever clearance times in Thailand were prolonged in both the rifampin- and the doxycycline-treated groups. Taken together, these findings suggest that strains prevalent in northern Thailand are insensitive to rifampin and azithromycin, or alternatively, are only apparently resistant owing to factors independent of their antibiotic susceptibility, such as high infectivity.
Only 1 strain of doxycycline-insensitive O. tsutsugamushi was tested in the present investigation. Therefore, while this study provides an explanation for the apparent in vitro insensitivity to doxycycline, there could be multiple mechanisms responsible for delayed recovery from scrub typhus. Further studies measuring the growth rate of various antibiotic-insensitive strains of O. tsutsugamushi are able to resolve this limitation.
Acknowledgment
This work was supported by an Inha University Research Grant.
Footnotes
No conflicts of interest.
References
- 1.Chung MH, Lee JS, Baek JH, Kim M, Kang JS. Persistence of Orientia tsutsugamushi in humans. J Korean Med Sci. 2012;27:231–235. doi: 10.3346/jkms.2012.27.3.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rajapakse S, Rodrigo C, Fernando SD. Drug treatment of scrub typhus. Trop Doct. 2011;41:1–4. doi: 10.1258/td.2010.100311. [DOI] [PubMed] [Google Scholar]
- 3.Watt G, Chouriyagune C, Ruangweerayud R, Watcharapichat P, Phulsuksombati D, Jongsakul K, Teja-Isavadharm P, Bhodhidatta D, Corcoran KD, Dasch GA, Strickman D. Scrub typhus infections poorly responsive to antibiotics in northern Thailand. Lancet. 1996;348:86–89. doi: 10.1016/s0140-6736(96)02501-9. [DOI] [PubMed] [Google Scholar]
- 4.Watt G, Kantipong P, Jongsakul K, Watcharapichat P, Phulsuksombati D. Azithromycin activities against Orientia tsutsugamushi strains isolated in cases of scrub typhus in Northern Thailand. Antimicrob Agents Chemother. 1999;43:2817–2818. doi: 10.1128/aac.43.11.2817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Strickman D, Sheer T, Salata K, Hershey J, Dasch G, Kelly D, Kuschner R. In vitro effectiveness of azithromycin against doxycycline-resistant and -susceptible strains of Rickettsia tsutsugamushi, etiologic agent of scrub typhus. Antimicrob Agents Chemother. 1995;39:2406–2410. doi: 10.1128/aac.39.11.2406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kelly DJ, Fuerst PA, Ching WM, Richards AL. Scrub typhus: the geographic distribution of phenotypic and genotypic variants of Orientia tsutsugamushi. Clin Infect Dis. 2009;48(Suppl 3):S203–S230. doi: 10.1086/596576. [DOI] [PubMed] [Google Scholar]
- 7.Kim MJ, Kim MK, Kang JS. Improved antibiotic susceptibility test of Orientia tsutsugamushi by flow cytometry using monoclonal antibody. J Korean Med Sci. 2007;22:1–6. doi: 10.3346/jkms.2007.22.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kelly DJ, Salata KF, Strickman D, Hershey JN. Rickettsia tsutsugamushi infection in cell culture: antibiotic susceptibility determined by flow cytometry. Am J Trop Med Hyg. 1995;53:602–606. doi: 10.4269/ajtmh.1995.53.602. [DOI] [PubMed] [Google Scholar]
- 9.Groves MG, Kelly DJ. Characterization of factors determining Rickettsia tsutsugamushi pathogenicity for mice. Infect Immun. 1989;57:1476–1482. doi: 10.1128/iai.57.5.1476-1482.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim ES, Kim MK, Lee HM, Kil SH, Chung MH, Lee JS, Kang JS. Doxycycline resistance in Orientia tsutsugamushi isolated from Korean patients. Infect Chemother. 2008;40:259–265. [Google Scholar]
- 11.Jeong HW, Choi YK, Baek YH, Seong MH. Phylogenetic analysis of the 56-kDa type-specific protein genes of Orientia tsutsugamushi in central Korea. J Korean Med Sci. 2012;27:1315–1319. doi: 10.3346/jkms.2012.27.11.1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Watt G, Kantipong P, Jongsakul K, Watcharapichat P, Phulsuksombati D, Strickman D. Doxycycline and rifampicin for mild scrub-typhus infections in northern Thailand: a randomised trial. Lancet. 2000;356:1057–1061. doi: 10.1016/S0140-6736(00)02728-8. [DOI] [PubMed] [Google Scholar]
- 13.Kim YS. Controlled trial of doxycycline versus rifampin for treatment of mild to moderate scrub typhus. Gwangju: Chosun University; 2010. Master's Thesis. [Google Scholar]