Abstract
Background:
Facial plastic surgeons may primarily focus on esthetic improvement of the nasal shape in patients seeking rhinoplasty (RP). However, medical conditions inside the nasal cavity should not be neglected because they may lead to unresolved sinonasal problems and, hence, dissatisfaction after esthetic RP. This observational study investigated the prevalence of sinonasal symptoms and endonasal pathology in patients requesting esthetic RP.
Methods:
Patients seeking RP (n = 269) were given a questionnaire evaluating nasal obstruction and sinonasal symptoms using visual analog scales and the 22-item Sino-Nasal Outcome Test. In addition, patients underwent nasal endoscopy to evaluate anatomic and/or mucosal disease and skin-prick testing in case of clinical suspicion of allergy. Two control groups consisted of patients with an otological or general ear/nose/throat problem (n = 65) and patients who planned for endoscopic sinus surgery (ESS; n = 90).
Results:
The general appraisal of nasal breathing on a scale from 0–10 in patients seeking RP was as low as 4.3 ± 3.1. Structural pathology was found in 62% of RP patients, with septal deviation being the most frequent problem encountered (54%), followed by internal nasal valve dysfunction (14%). Mucosal disease was present in 28% of RP patients. The mean SNOT-22 score of RP patients (31.8 ± 23.3) was significantly higher than the control group (11.6 ± 7.9; p < 0.001), but lower than the ESS patients (48.5 ± 22.0; p < 0.001).
Conclusion:
The prevalence of endonasal structural or mucosal pathology in patients seeking RP is high and should not be overlooked at the time of planning surgery.
Keywords: ESS, esthetic, facial, functional, mucosal disease, nasal breathing, nasal valve, revision, rhinoplasty, sinonasal
Facial plastic surgeons may be focused primarily on esthetic improvement of the nose in patients seeking esthetic rhinoplasty (RP), because the patients and relatives will appraise the change in nasal shape. However, associated medical conditions inside the nasal cavity should not be neglected at the time of planning RP because any neglect of concomitant endonasal mucosal or anatomic pathology may be associated with dissatisfaction after RP.1–3 Indeed, breathing difficulties or nasal blockage turned out to be the second most frequent reason for seeking revision RP after nasal tip asymmetry.1 Similarly, others have reported on two-thirds of revision RP patients suffering from a variable degree of nasal obstruction most commonly caused by residual septal deviation and nasal valve problems from either valve collapse or adhesions.1–4 Patients undergoing reduction RP are particularly at risk for postoperative nasal breathing problems as it significantly reduces the minimal cross-sectional area of the nose.5
Functional nasal pathology can be divided into mucosal and structural or anatomic pathology. In general, mucosal disease is medically treated, whereas structural problems require surgical treatment. Most of the latter can be addressed during RP without interfering with nasal esthetics.6,7 The negative influence of functional nasal pathology on patients' quality of life and on satisfaction after RP has already been established,1–3,8–13 emphasizing the importance of a thorough preoperative evaluation of the nose in every patient seeking esthetic RP.
So far, prevalence of functional sinonasal symptoms and structural and/or mucosal endonasal pathology has not been studied in patients seeking esthetic RP in a tertiary academic referral center for RP. Therefore, we evaluate the presence of functional pathology in patients seeking esthetic RP based on full clinical rhinologic examination and using questionnaires given to patients before surgery.
MATERIALS AND METHODS
Patient Recruitment
The study was conducted at the Department of Otorhinolaryngology of the University Hospitals Leuven, a tertiary referral center for RP and nasal pathology. All patients ≥16 years of age seeking RP for altering the nasal shape between February 2009 and October 2010 were asked to participate in this study.
A first control group was selected out of patients of ≥16 years of age, consulting for an otological or general ear/nose/throat–related problem. To prevent any selection bias, no exclusion was made based on upper respiratory tract disease or treatment, except for subjects with a current or recent (<2 weeks before their visit) common cold. A second control group consisted of patients ≥16 years of age who planned for endoscopic sinus surgery (ESS) because of mucosal disease refractory to medical treatment.
Because of the fact that the questionnaires were in Dutch, only patients with good knowledge of Dutch were included.
The study was approved by the Local Committee of Medical Ethics of the University Hospitals of Leuven.
Evaluation of Sinonasal Symptoms
All patients and control subjects were asked to express a general appraisal of nasal breathing capacity on a scale of 0 (total blockage) to 10 (free nasal breathing). In addition, RP patients and patients who planned for ESS were asked to evaluate their nasal breathing on both sides in three specific situations, i.e., in rest, during physical activity, and at sleep (0 representing total blockage and 10 representing free nasal breathing). The nasal breathing score was obtained by adding up the six items to a total score of 60.
Patients and subjects in both control groups also filled in the 22-item Sino-Nasal Outcome Test-22 (SNOT-22), a validated disease-specific quality-of-life questionnaire for rhinosinusitis,12 in which patients have to score a total of 22 sinonasal symptoms on a scale of 0 (no problem) to 5 (very severe problem).
Evaluation of Structural and/or Mucosal Pathology
Nasal examination including nasal endoscopy was performed in all individuals requesting RP and in patients who planned for sinus surgery. Endonasal pathology was divided into structural or anatomic abnormality and inflammatory nasal or sinus disease. Structural causes were subdivided in nasal septum deviation, nasal septum perforation, inferior turbinate hypertrophy, external and internal nasal valve narrowing, and adhesions in the nasal cavity. Alar insufficiency being a reason for external valve dysfunction was defined as a medial movement of the lateral crura during inspiration in association with a positive Cottle maneuver. Inner nasal valve dysfunction with a narrow nasal vault was diagnosed by anterior rhinoscopy and confirmed by a positive cotton ball test.
Sinonasal inflammatory disease was arbitrarily divided in rhinitis, acute rhinosinusitis, and chronic rhinosinusitis with or without nasal polyps. Rhinitis comprised a heterogeneous group of nasal disorders characterized by one or more of the following symptoms: sneezing, nasal itching, rhinorrhea, and nasal congestion.14 Rhinosinusitis (including nasal polyps) was defined according to its definition in the “European Position Paper on Rhinosinusitis and Nasal Polyps 2012”: inflammation of the nose and the paranasal sinuses, characterized by two or more symptoms, one of which should be either nasal blockage/obstruction/congestion or nasal discharge, ± facial pain/pressure, ± reduction or loss of smell; and either endoscopic signs of polyps and/or mucopurulent discharge and/or edema/mucosal obstruction, and/or CT changes.15 Acute rhinosinusitis was defined as symptoms that persisted for <12 weeks and with symptom-free intervals if the problem was recurrent. Chronic rhinosinusitis was defined as symptoms that persisted for >12 weeks.15
When allergic rhinitis/rhinosinusitis was suspected in a patient without previous investigations for underlying sensitization, standard skin-prick tests were performed with house-dust mite, timothy grass, smooth meadow grass, orchard grass, nettle, plantago, oxeye daisy, mugwort, alder, birch, hazel, horse, cat, dog, rabbit, Alternaria, Aspergillus, and Cladosporium (HAL Allergy, Leiden, the Netherlands).
Statistical Methodology
All analyses were performed using Microsoft Excel (for MAC version 12.2.0, Katholieke Universiteit Leuven, Flanders, Belgium). Comparisons between the RP population and the control groups were made by ANOVA test. Data are expressed as means ± SEM. A difference was considered to be significant when p < 0.05.
RESULTS
Patients' Characteristics
Two hundred sixty-nine Dutch-speaking patients with esthetic nasal concerns, 90 patients who planned for ESS and 65 control subjects, were included in the study. Demographic characteristics and details of rhinologic history of RP population and control groups are summarized in Table 1.
Table 1.
Demographic characteristics and details on rhinologic history of patients requesting RP, patients who planned for ESS, and control subjects
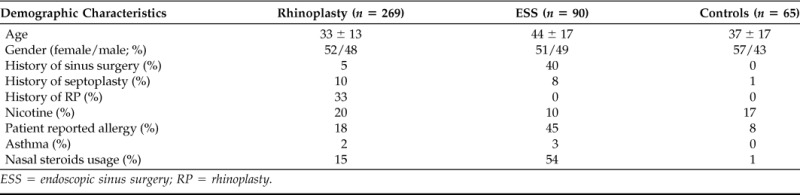
ESS = endoscopic sinus surgery; RP = rhinoplasty.
Nasal Breathing Problems in Patients Seeking Esthetic RP and in Control Groups
The mean general appraisal of nasal breathing by the patient on a visual analog scale ranging from 0 (total blockage) to 10 (free nasal breathing) was 4.3 ± 3.1 in the RP population (n = 267), 4.1 ± 2.4 in patients who planned for ESS (n = 90), and 8.0 ± 1.6 in the control group (n = 65). There was a significant difference in general evaluation of nasal breathing between RP patients and control subjects (p < 0.001) but no significant difference between patients requesting RP and patients who planned for sinus surgery (p = 0.29; Fig. 1). Only 22% of RP patients scored their general nasal breathing as ≥7, representing good and satisfactory nasal breathing.
Figure 1.
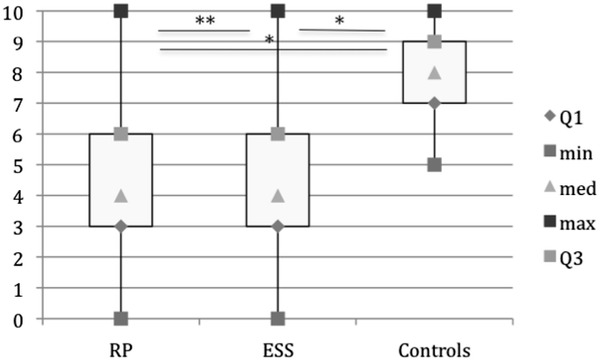
General evaluation of nasal breathing on a visual analog scale from 0 (total blockage) to 10 (free nasal breathing) in patients requesting rhinoplasty (RP; n = 262), in patients who planned for endoscopic sinus surgery (ESS; n = 90), and in control subjects (n = 65). There is a significant difference in general evaluation of nasal breathing between RP patients and control subjects (*p < 0.001) but no significant difference between patients requesting RP and patients who planned for sinus surgery (**p = 0.29).
Using the self-made nasal breathing score, the mean nasal breathing score in patients requesting RP was 28.5 (ranging from 0 to 60, with SEM of 14, and maximal score of 60) and in patients who planned for ESS the score was 25.3 ± 13.2.
In the overall RP population 229 of 269 (85%) patients and in patients requesting revision RP 77 of 88 (88%) patients expressed the desire for improvement of their nasal breathing.
Nasal Structural Pathology in Patients Seeking Esthetic RP and in Patients Who Planned for ESS
In 167 patients seeking esthetic RP at least one structural cause for sinonasal pathology was identified during clinical examination (62%). The most frequent problem encountered was septal deviation, found in 145 patients (54%), followed by internal nasal valve dysfunction in 38 patients (14%), inferior turbinate hypertrophy in 30 patients (11%), and external nasal valve dysfunction in 21 patients (8%). In patients requesting revision RP (n = 88) residual septum deviation was found in 41 patients (46%), followed by internal nasal valve dysfunction in 15 patients (17%) and external nasal valve dysfunction in 11 patients (12%; Table 2).
Table 2.
Sinonasal pathology in patients requesting RP, in patients requesting revision RP, and in patients who planned for ESS
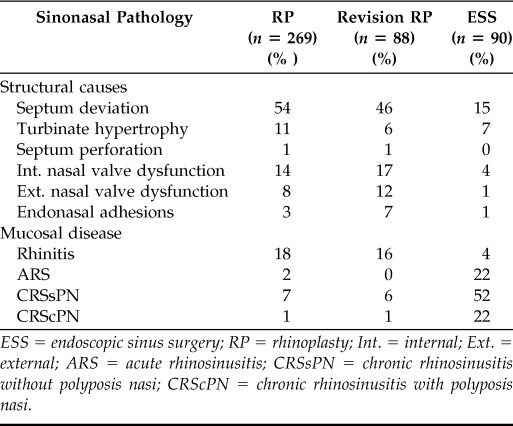
ESS = endoscopic sinus surgery; RP = rhinoplasty; Int. = internal; Ext. = external; ARS = acute rhinosinusitis; CRSsPN = chronic rhinosinusitis without polyposis nasi; CRScPN = chronic rhinosinusitis with polyposis nasi.
In patients who planned for ESS (n = 90), structural pathology was found in 20 patients (22%). The most frequent problem encountered was septal deviation, found in 14 patients (15%), followed by turbinate hypertrophy in 6 patients (7%).
Mucosal Disease in Patients Seeking Esthetic RP and Patients Who Planned for ESS
Mucosal disease was present in 75 of 269 RP patients (28%), with rhinitis diagnosed in 48 patients (18%), recurrent acute rhinosinusitis in 6 patients (2%), and chronic rhinosinusitis with or without nasal polyps in 21 patients (8%). Skin-prick tests were performed in 44 patients and were positive in 36 patients (13% of RP patients; Table 2).
In patients who planned for ESS (n = 90), 67 patients presented with chronic rhinosinusitis (with or without nasal polyps; 74%), 20 patients with recurrent acute rhinosinusitis (22%), and 4 patients with rhinitis (4%; Table 2).
SNOT-22 Scores in Patients Seeking Esthetic RP and in Control Groups
In patients requesting RP, the mean SNOT-22 score was higher than in control patients but lower than in those patients who planned for ESS: 31.8 ± 23.3 (n = 251) in RP patients, 48.5 ± 22.0 (n = 90) in patients who planned for ESS, and 11.6 ± 7.9 (n = 65) in control subjects. There was a significant difference in the mean SNOT-22 score between all three groups (p < 0.001; Fig. 2).
Figure 2.
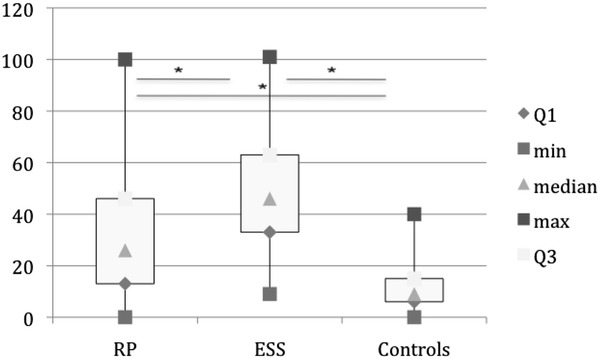
Twenty-two-item Sino-Nasal Outcome Test (SNOT-22) score in patients requesting rhinoplasty (RP; n = 251), in patients who planned for endoscopic sinus surgery (ESS; n = 90), and in control subjects (n = 65). There is a significant difference in the mean SNOT-22 score between all three groups (*p < 0.001).
DISCUSSION
This large-scale observational study highlights the high prevalence of functional sinonasal symptoms and pathology in patients seeking esthetical RP. The overall nasal breathing in our population was evaluated as poor and 85% of patients expressed the desire for improvement of their nasal breathing. The high prevalence of functional burdens in our population is probably partly caused by a referral bias because our center is a tertiary referral center for RP and general rhinology. However, these data reinforce the need for the RP surgeon to be familiar with the different etiology of functional nasal burdens and with its medical and surgical treatment.
Clinical examination of our RP patients revealed in 62% at least one structural abnormality that interferes with the normal nasal breathing, whereas in patients who planned for ESS, this percentage was only 22%. The most frequently encountered structural problems in the overall RP population were nasal septal deviation (in 54% of patients), followed by internal nasal valve dysfunction (14%), inferior turbinate hypertrophy (11%), and external nasal valve dysfunction (8%). In patients seeking revision RP, 88% of patients expressed the desire for improvement of their nasal breathing. Residual nasal septal deviation (46%) and nasal valve insufficiency (29%) were the most frequently occurring structural problems in this subgroup of patients. This is in accordance with previous research, where authors reported neglected anatomic problems inside the nose becoming the source of nasal symptoms after surgery leading to postoperative dissatisfaction and revision RP.1,5,13
Mucosal disease was present in 28% of RP patients; in 36 patients (13% of RP patients) sensitization to commonly inhaled allergens was diagnosed. The negative influence of nasal mucosal disease on quality of life has been extensively documented.8–12,14–16 On the other hand, the condition may frequently be trivialized and/or unrecognized.15,16 Because most of these patients benefit from medical treatment, proper diagnosis and, when indicated, initiation of medical therapy should be implemented in the preoperative assessment of every patient undergoing esthetic nasal operation.
The high prevalence of sinonasal burdens in our population is reflected by the reduced disease-specific quality of life, as measured with the SNOT-22. The mean SNOT-22 score in our population was 31.8 ± 23.3, comparable to the SNOT-22 score found in patients with allergic and nonallergic asthma.17 The mean SNOT-22 score was significantly higher than the mean SNOT-22 score in control subjects (11.6 ± 7.9) but lower than in patients who planned for sinus surgery (48.5 ± 22.0).
We can conclude that the prevalence of functional sinonasal symptoms and pathology in patients seeking esthetic RP is high and therefore should not be overlooked at the time of planning surgery. The RP surgeon should be familiar with the different etiology of functional nasal burdens and with its medical and surgical treatment.
Footnotes
The authors have no conflicts of interest to declare pertaining to this article
REFERENCES
- 1. Yu K, Kim A, Pearlman SJ. Functional and aesthetic concerns of patients seeking revision rhinoplasty. Arch Facial Plast Surg 12:291–297, 2010. [DOI] [PubMed] [Google Scholar]
- 2. Foda HM. Rhinoplasty for the multiply revised nose. Am J Otolaryngol 26:28–34, 2005. [DOI] [PubMed] [Google Scholar]
- 3. Thomson C, Mendelsohn M. Reducing the incidence of revision rhinoplasty. J Otolaryngol 36:130–134, 2007. [DOI] [PubMed] [Google Scholar]
- 4. Hellings PW, Nolst Trenité GJ. Long-term patient satisfaction after revision rhinoplasty. Laryngoscope 117:985–989, 2007. [DOI] [PubMed] [Google Scholar]
- 5. Grymer LF. Reduction rhinoplasty and nasal patency: Change in the cross-sectional area of the nose evaluated by acoustic rhinometry. Laryngoscope 105:429–431, 1995. [DOI] [PubMed] [Google Scholar]
- 6. Rhee JS, Poetker DM, Smith TL, et al. Nasal valve surgery improves disease-specific quality of life. Laryngoscope 115:437–440, 2005. [DOI] [PubMed] [Google Scholar]
- 7. Becker DG, Ransom E, Guy C, Bloom J. Surgical treatment of nasal obstruction in rhinoplasty. Aesthet Surg J 30:347–378, 2010. [DOI] [PubMed] [Google Scholar]
- 8. Udaka T, Suzuki H, Fujimura T, et al. Chronic nasal obstruction causes daytime sleepiness and decreased quality of life even in the absence of snoring. Am J Rhinol 21:564–569, 2007. [DOI] [PubMed] [Google Scholar]
- 9. Dykewicz MS, Hamilos DL. Rhinitis and sinusitis. J Allergy Clin Immunol 125(suppl 2):S103–S115, 2010. [DOI] [PubMed] [Google Scholar]
- 10. Stewart M, Ferguson B, Fromer L. Epidemiology and burden of nasal congestion. Int J Gen Med 3:37–45, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Shedden A. Impact of nasal congestion on quality of life and work productivity in allergic rhinitis: Findings from a large online survey. Treat Respir Med 4:439–446, 2005. [DOI] [PubMed] [Google Scholar]
- 12. Hopkins C, Gillett S, Slack R, et al. Psychometric validity of the 22-item Sinonasal Outcome Test. Clin Otolaryngol 34:447–454, 2009. [DOI] [PubMed] [Google Scholar]
- 13. Guyuron B, Bokhari F. Patient satisfaction following rhinoplasty. Aesthetic Plast Surg 20:153–157, 1996. [DOI] [PubMed] [Google Scholar]
- 14. Wallace DV, Dykewicz MS, Bernstein DI, et al. The Joint Force on Practice Parameters, representing the AAAAI, ACAAI, JCAAI. The diagnosis and management of rhinitis: An updated practice parameter. J Allergy Clin Immunol 122(suppl 2):S1–S84, 2008. [DOI] [PubMed] [Google Scholar]
- 15. Fokkens WJ, Lund VJ, Mullol J, et al. European position paper on rhinosinusitis and nasal polyps 2012. Rhinology 50(suppl 23):1–289, 2012. [PubMed] [Google Scholar]
- 16. Bauchau V, Durham SR. Prevalence and rate of diagnosis of allergic rhinitis in Europe. Eur Respir J 24:758–764, 2004. [DOI] [PubMed] [Google Scholar]
- 17. Hens G, Vanaudenaerde BM, Bullens DM, et al. Sinonasal pathology in nonallergic asthma and COPD: “United airway disease” beyond the scope of allergy. Allergy 63:261–267, 2008. [DOI] [PubMed] [Google Scholar]


