Abstract
Background:
Endoscopic sinus surgery (ESS) is considered after medical therapy failure of chronic rhinosinusitis (CRS). The balloon sinuplasty dilates the natural ostium without moving mucosa or bone. It still lacks evidence from randomized controlled trials. The aim of this retrospective controlled study was to compare the symptom outcomes after maxillary sinus surgery with either the ESS or the balloon sinuplasty technique. No previous or additional sinonasal operations were accepted.
Methods:
Two hundred eight patients with CRS without nasal polyps underwent either balloon sinuplasty or ESS. The patients who met with the inclusion criteria (n = 45 in ESS group and n = 40 in balloon group) replied to a questionnaire of history factors, exacerbations, and a visual analog scale (VAS) scoring of the change in symptoms, on average 28 ± 6 (mean ± SD) months postoperatively.
Results:
The groups were identical in the response rate (64%), patient characteristics, and the improvement in all of the asked symptoms. Patients with CRS-related comorbidity and/or present occupational exposure had a statistically significantly better symptom reduction after ESS than after balloon sinusotomy. Moreover, the balloon sinusotomy group reported a statistically significant higher number of maxillary sinus punctures and antibiotic courses during the last 12 months.
Conclusion:
ESS might be superior to balloon sinuplasty, especially in patients with risk factors. There is a need to perform more controlled studies on the treatment choices of CRS.
Keywords: Balloon sinuplasty, chronic sinusitis, endoscopy, occupation, sinus surgery
Chronic rhinosinusitis (CRS) is a versatile, multifactorial immunologic disease of the nose and paranasal sinuses with ∼10% prevalence.1 CRS is diagnosed by its typical symptoms lasting >12 weeks and computed tomography (CT) scan and/or endoscopic changes.2 Its impact on the quality of life (QoL) is comparable with other chronic diseases.1 Several diseases have been reported to coexist with CRS by partly unknown mechanisms: asthma, aspirin sensitivity, atopy, chronic rhinitis, depression, anxiety, fatigue, fibromyalgia, immunodeficiency, cystic fibrosis, and primary ciliary dyskinesia.3–5 It has been shown that biological and chemical agents associate with work-related asthma and occupational exposure might cause 10–20% of adult-onset asthma.6–8 However, only few studies address the influence of occupational exposure on CRS.9,10 Basic management of CRS is composed of nasal saline irrigations and corticosteroids. Depending on the related comorbidities and the hyperinflammatory or infective nature of the exacerbations, additional treatment might be used.2
Endoscopic sinus surgery (ESS) is considered during recalcitrant and difficult-to-treat CRS. ESS might decrease inflammation by restoring the mucociliary clearance through the natural ostia.2 Uncontrolled studies have shown QoL improvement after ESS.5 Although not proven to be superior to conservative therapy, ESS seems to at least partially relieve symptoms and/or decrease inflammatory findings.2,11,12 The recurrence rate of CRS exacerbations is high, especially in patients who have nasal polyps, asthma, and/or aspirin sensitivity or occupational exposure.2,10,13
The principal behind balloon sinuplasty differs from that of ESS.14 The guide wire and the balloon catheter are advanced into the sinus ostium. The balloon pressure varies from 8 to 12 bar and is maintained for only a few seconds, causing the thin bony walls of the ostia to compress or fracture, resulting in a wider passage to the sinus. The disadvantages of the procedure are the lack of knowledge on its long-term effects, the costs of the disposable instruments, and its technical limitations in the ethmoidal area or in removing atypical mucosa.15 Several uncontrolled and three controlled studies have suggested balloon sinuplasty to be a safe and effective method.15–19 However, the limitations of these studies are the heterogeneity of patients and procedures, which makes the conclusions difficult to draw.
In this retrospective, controlled study, adult CRS patients underwent primary bilateral maxillary sinus procedures, with either the balloon sinuplasty or the ESS technique. The aim of this study was to compare, using a questionnaire, the number of exacerbations and the change in symptoms between the procedures.
MATERIALS AND METHODS
Patients
The Ethical Committee of Pirkanmaa Hospital District, Tampere, Finland, has approved the study plan. Informed consent was obtained from all of the patients. The inclusion criteria were based on the medical records: CRS diagnosis and operative indications fulfilled European position paper on rhinosinusitis and nasal polyps recommendations and surgical procedure to maxillary sinuses.2 The exclusion criteria were age <15 years; previous or concomitant additional sinonasal surgery; unilateral CRS; endoscopic signs of nasal polyposis (grade ≥2) during surgery; a history of aspirin sensitivity; and chronic bronchitis, cystic fibrosis, primary ciliary dyskinesia, tumor, or another disease with a severe impact on general immunity.20
The balloon sinusotomy group consisted of all CRS patients (n = 103) that underwent balloon sinusotomy at two private clinics (Terveystalo Health care OYJ of Finland, Tampere, Finland, and Koskiklinikka Tampereen Lääkärikeskus Oy, Tampere, Finland) between 2008 and 2010. The control ESS group consisted of all CRS patients (n = 105) who underwent uncinectomy and middle meatal antrostomy, at Päijät-Häme Central Hospital, Lahti, Finland, during 2008–2010. Forty-five patients in the ESS group and 40 patients in the balloon group met the inclusion criteria and received a letter with a questionnaire. The patients (n = 14) that had <18 months follow-up were contacted by telephone, on average, 1 year later and were given another questionnaire.
Operations
Only patients having bilateral maxillary sinus operations were included in the study. Thus, previous or concomitant surgeries, such as septoplasty or anterior ethmoidectomy or resection of bullous turbinate, were not accepted. The balloon sinuplasty was performed by one according to the manufacturer′s instructions (Acclarent, Inc., a member of Johnson & Johnson Co., New Brunswick, NJ). No pack was placed. No postoperative debridement was performed. Two authors (J.M., 80%, and J.S., 20%) performed uncinectomy and middle meatal antrostomy in the ESS group. Two-thirds of the lower part of the uncinate process was cut by the backbiting forceps. The maxillary ostium was enlarged to posterior–inferior direction to double its diameter. A small pack (3.5 × 0.6 × 1.2 cm, Merocel; Medtronic-Xomed, Jacksonville, FL) was placed into the middle meatus for 24 hours. Debridement control was approximately 4 weeks postoperatively.
Questionnaires
The questionnaire asked about the patient's medical history such as the presence of doctor-diagnosed allergic rhinitis, asthma, and previous nasal polyps; the presence of nonsteroidal anti-inflammatory drug–induced wheezing; smoking habits; medication; duration of CRS symptoms; and previous sinonasal operations. The regularly used medications excluding those for CRS or related diseases were (B = in the balloon sinuplasty, E = in the ESS group) for heart and vascular diseases (B = 4 patients, E = 4 patients), thyroxin (B = 4, E = 3), estrogen replacement (B = 1, E = 5), hypercholesterolemia (B = 1, E = 5), depression (B = 1, E = 4), reflux disease (B = 1, E = 2), diabetes mellitus (B = 1, E = 1), and prostate hyperplasia (B = 1, E = 1). The work exposure was evaluated according to reported current occupation and characterization of work place, characterization of substances and places of putative past or current exposure to poor indoor air quality, and by the question, “Has a doctor ever suspected an occupational hypersensitivity?” “If yes, please list the suspected substances.” The positive job exposure group was determined according to international categorization of high-risk occupations.6,8 Two more patients (1 in balloon sinuplasty and 1 in the ESS group) reporting severe occupational exposure to poor indoor air quality were added to this group as well. The main substances causing job exposure were bioaerosols (B = 2 patients, E = 2 patients), agricultural organic particles (B = 3, E = 3), wood dust (B = 1, E = 1), mites (B = 2, E = 5), textile dust (B = 1, E = 3), molds (B = 1, E = 1), flour (B = 1, E = 0), and reactive chemicals/metalwork (B = 1, E = 0).
The changes of symptoms were evaluated by using the visual analog scale (VAS) with the question, “How much did the following symptoms change after the operation?” The value 0 (cm) indicated “recovered totally,” and value 10 (cm) indicated “became as worse as it can be.” Twenty-two questions were similar to those of the 22-item Sino-Nasal Outcome Test (Table 1).2 In addition, 12 questions concerning general health or CRS relating/resembling symptoms were asked (Table 1). The bilaterally existing symptoms were asked separately from each side. Statistical evaluation was performed with eight VAS subscales (Table 1). CRS exacerbations were evaluated by the following question: “How many acute sinusitis treated by prescribed antibiotics have you had during the past year?” “How many maxillary sinus punctures/sinus x rays/ultrasonographys of maxillary sinuses has a doctor performed on you during the past year?”
Table 1.
The questions that belonged to the VAS questionnaire evaluating how the operation changed symptoms (ranging from 0 [cm], “recovered totally,” to 10 [cm] “became as worse as it can be)
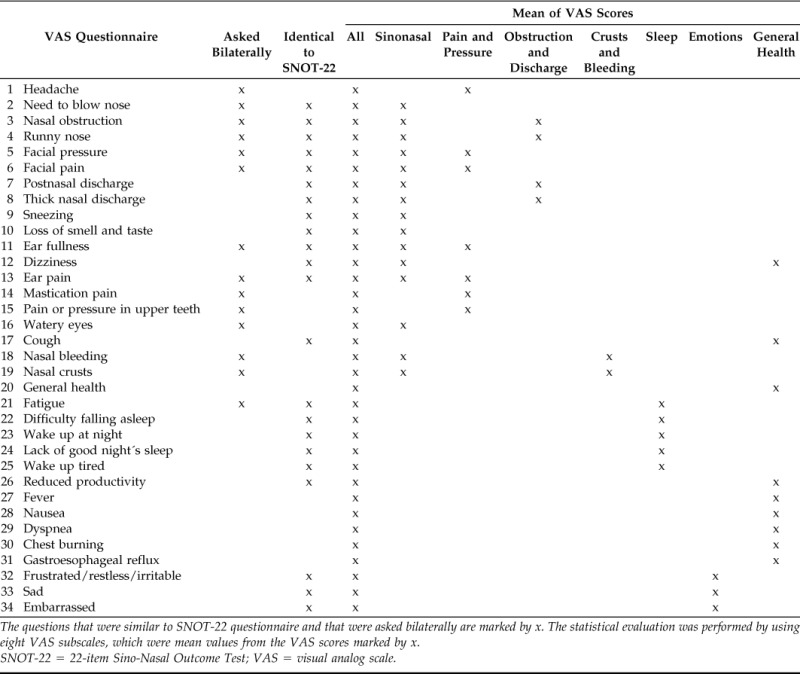
The questions that were similar to SNOT-22 questionnaire and that were asked bilaterally are marked by x. The statistical evaluation was performed by using eight VAS subscales, which were mean values from the VAS scores marked by x.
SNOT-22 = 22-item Sino-Nasal Outcome Test; VAS = visual analog scale.
Statistical Analysis
Statistics were performed with SPSS Base 16.0 Statistical Software Package (SPSS, Chicago, IL). The results were confirmed by a professional statistician. The nonparametric Fisher's exact test and Kruskal-Wallis and Mann Whitney U tests were used for comparisons of groups. A two-tailed value of p < 0.05 was considered significant in all tests.
RESULTS
Patient Characteristics
Twenty-nine patients in the ESS group and 24 patients in the balloon sinusotomy group responded. The groups were identical in all demographic variables (Table 2). There was a high prevalence of self-administered previously doctor-diagnosed nasal polyps (41% in the ESS group and 21% in the balloon sinusotomy group), although none of the patients were having intraoperative endoscopic signs of nasal polyps (Table 2). Preoperative sinus CT scans were available in 29 patients in the ESS-group and 20 in the balloon sinuplasty group (Table 2). In addition, preoperative sinus magnetic resonance imaging scans were from one patient in the balloon sinuplasty group. The Lund-Mackay scores on each side were retrospectively evaluated from the CT (or magnetic resonance imaging) scans. There were no differences between the groups in the Lund-Mackay (LM) scores of the maxillary sinus, whereas the LM total scores and the LM sore of the right ostiomeatal complex differed significantly (Table 2). The frontal sinuses were absent in three patients in the balloon sinuplasty group.
Table 2.
Patient characteristics
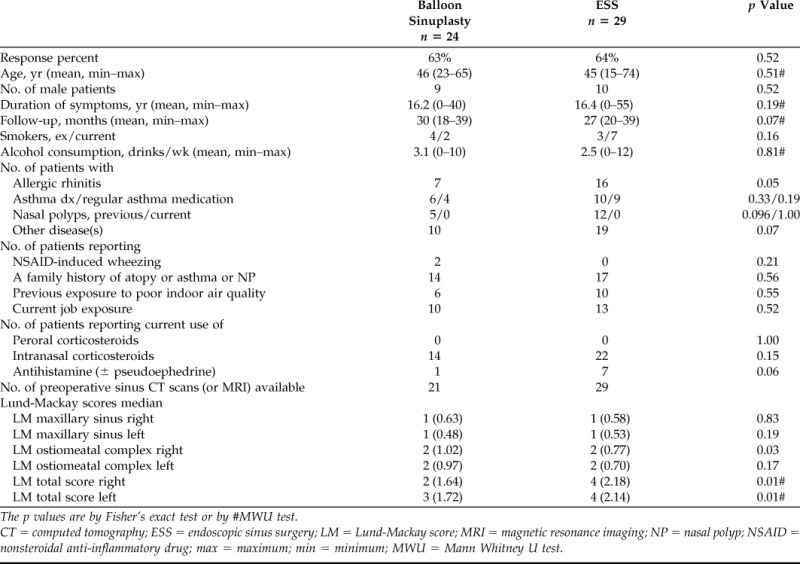
The p values are by Fisher's exact test or by #MWU test.
CT = computed tomography; ESS = endoscopic sinus surgery; LM = Lund-Mackay score; MRI = magnetic resonance imaging; NP = nasal polyp; NSAID = nonsteroidal anti-inflammatory drug; max = maximum; min = minimum; MWU = Mann Whitney U test.
Exacerbations
The balloon sinuplasty group reported a higher number of doctor-performed maxillary sinus punctures, ultrasonography examinations, and prescribed antibiotic courses for acute sinusitis during the last 12 months, which differed statistically significantly from the ESS group (Table 3). The number of performed sinus x rays during the past 12 months did not differ between the treatment groups (Table 3).
Table 3.
Comparison of patient-reported number of acute CRS exacerbations during the past 12 mo between the balloon sinusotomy and ESS groups
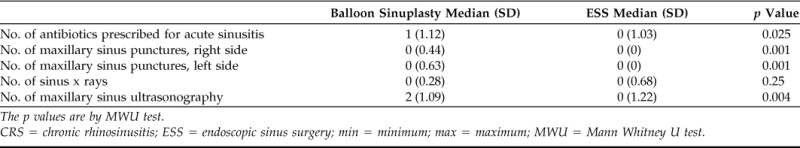
The p values are by MWU test.
CRS = chronic rhinosinusitis; ESS = endoscopic sinus surgery; min = minimum; max = maximum; MWU = Mann Whitney U test.
Visual Analog Scale
The mean of all of the VAS scores was 3.6 in all patients (3.7 in the balloon sinuplasty group and 3.5 in the ESS group). This indicated an average improvement of 28% of all the asked symptoms. The VAS scores for the change of symptoms and the eight VAS subscales did not differ between the balloon sinuplasty and ESS groups (p > 0.05, Fig. 1). The greatest improvement was achieved in the VAS scores concerning the change in nasal congestion, discharge, and facial pressure. This improvement was also equal in both groups (Fig. 1).
Figure 1.

(A) Comparison of mean visual analog scale (VAS) scores of change in symptoms between balloon sinuplasty and ESS groups in all patients and (B) in a subgroup having job exposure and asthma/previous nasal polyps/allergic rhinitis. The x-axis represents mean VAS scores change in symptoms (range, 0–10). We used the question “How much did the following symptoms change after the operation?” The value 0 (cm) indicated “recovered totally” and value 10 (cm) indicated “became as worse as it can be.” The y-axis represents the eight subscales that were the mean values of group-specific symptoms as shown in Table 1. Statistically significant differences are shown by asterisks (*p < 0.05) by Mann Whitney U test.
The Influence of CRS Comorbidities.
Allergic rhinitis and previously diagnosed nasal polyps did not have an influence on the VAS subscale values (p > 0.05). Asthma and current job exposure contributed to the elevated VAS subscales, indicating less improvement compared with patients without these risk factors (Table 4). Interestingly, this was only found in the balloon sinuplasty group but not in the ESS group (Table 4). The comparison of the two operation techniques in the asthma or job exposure subgroups did not bring differences of statistical importance (p > 0.05). However, when observing a patient subgroup having a combination of current job exposure and at least one CRS co morbidity (e.g., asthma/previous nasal polyps/allergic rhinitis), several VAS subscale values were significantly lower in the ESS group compared with the balloon sinuplasty group, indicating greater symptom reduction after ESS than after balloon sinuplasty (Table 5; Fig. 1).
Table 4.
Mean values of the mean VAS scores of change in symptoms (range, 1–10)
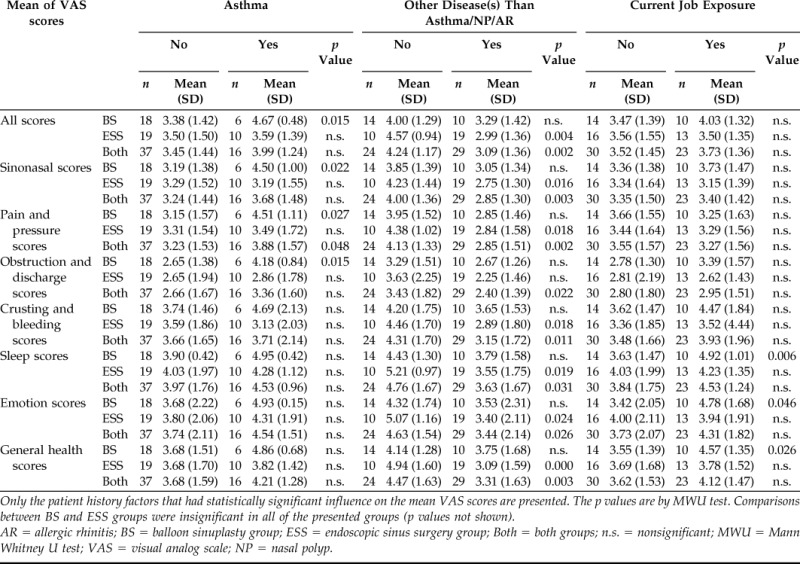
Only the patient history factors that had statistically significant influence on the mean VAS scores are presented. The p values are by MWU test. Comparisons between BS and ESS groups were insignificant in all of the presented groups (p values not shown).
AR = allergic rhinitis; BS = balloon sinuplasty group; ESS = endoscopic sinus surgery group; Both = both groups; n.s. = nonsignificant; MWU = Mann Whitney U test; VAS = visual analog scale; NP = nasal polyp.
Table 5.
Mean VAS scores of change in symptoms only in a subgroup having job exposure and allergic rhinitis/nasal polyps/asthma
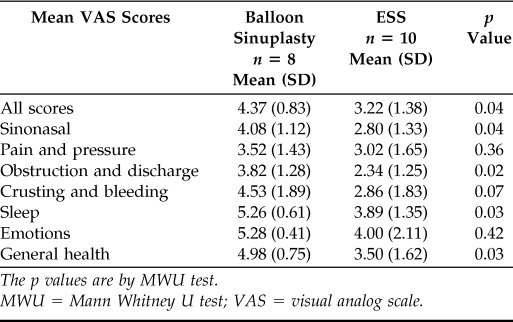
The p values are by MWU test.
MWU = Mann Whitney U test; VAS = visual analog scale.
The Influence of Other Diseases.
The patients who were regularly taking medication for at least one additional disease (e.g., other than CRS/allergic rhinitis/asthma) had significantly lower VAS subscale values, indicating a greater improvement in symptoms compared with patients without additional disease(s) (Table 4). Interestingly, this was found only in the ESS group but not in the balloon sinuplasty group (Table 4). The comparison of the two operation techniques in this subgroup did not bring statistically significant differences to the VAS subscale values (p > 0.05).
The Influence of Other Factors.
Female gender contributed significantly to lower VAS scores, but only in subscales of “emotions” and “general health” (p = 0.006 and p = 0.050, respectively). This was equally found in the balloon sinuplasty and the ESS groups. The VAS subscales were not influenced by the following patient factors: age, reported duration of CRS symptoms, length of the postoperative follow-up period, or alcohol consumption (p > 0.05). Similarly, the VAS subscales were not influenced by smoking habits, previous exposure to poor indoor air quality, a family history of atopy and/or asthma and/or nasal polyps, or the usage of intranasal corticosteroids or antihistamines (± pseudoephedrine; p > 0.05). The values characterizing the exacerbation rate were not associated with any of the demographic variables (p > 0.05).
DISCUSSION
This study was to compare balloon sinuplasty and ESS (uncinectomy and middle meatal antrostomy) in adult patients with non–polypous CRS, and with no previous sinonasal operations. The improvement of the VAS values of the change in symptoms for all of the patients was similar for both techniques. The average improvement after ESS was 17%, measured by the CRS survey score, which is in accordance with our findings of 28% improvement.21 QoL measures how an illness interferes with a patients' day-to-day life, whereas exacerbation rate might be better in estimating to what extent CRS is under control.22 We found that the number of patient-reported, doctor-diagnosed postoperative acute sinusitis, indicating exacerbation rate, was lower after ESS than after balloon sinuplasty. Currently, several patient series studies and three controlled studies exist on balloon sinusotomy, suggesting it as a safe method and comparable with ESS. In a prospective randomized trial, in which heterogeneous operation techniques were tolerated, balloon dilation of the frontal recess reduced the VAS symptom scores equally to the ESS procedure 12 months postoperatively.18 In a retrospective setup, with a short follow-up period, and a variation in the (re)operated sinuses, a significant reduction of symptom scores was achieved equally with both the ESS and the balloon sinuplasty techniques, but the patient satisfaction was slightly better in the balloon sinusotomy group.16 In a prospective nonrandomized pediatric CRS study, a significantly younger children group with adenoidectomy had improvement similar to the older children group who underwent balloon sinusotomy.17 In a preliminary study with a small number of patients, balloon sinuplasty with polypectomy was as effective as ESS with polypectomy.23 It has been suggested that balloon sinuplasty may potentially inadvertently impair mucociliary clearance of the sinuses through effects on secondary drainage pathways.24
The subset observation in our study suggests that patients with asthma or job exposure might experience less symptom reduction after balloon sinuplasty but not after ESS, compared with patients without asthma or without job exposure. Moreover, if the patient had both job exposure and at least one CRS comorbidity (asthma/previous nasal polyps/allergic rhinitis), he/she might benefit more from ESS than balloon sinuplasty. Although we and others have previously shown that a high mucosal eosinophilia might predict reduced postoperative outcomes, Badaai et al. showed that the presence of asthma would not be a negative or positive predictor for the total health-related QoL outcome.5,21,25,26 This finding is supported by observations in the present study that the symptoms of asthma patients improved equally to nonasthmatic patients, but only in the ESS group. Irritant exposure has been investigated less during CRS, whereas it is known to influence asthma onset and exacerbations.6,7,9 A recent study shows that occupational exposure might be a risk factor for the occurrence and recurrence of CRS.10 Chronic infection or other factors might play a role in CRS pathogenesis, especially in patients with respiratory comorbid diseases and occupational exposure. Others have studied that biofilms are associated with refractory CRS and revision ESS.27,28 Zhang et al. also observed that bacterial biofilms and asthma associate strongly with revision ESS.29 The overexpression of atopic and occupational risk factors during difficult-to-treat CRS supports the importance of Allergic Rhinitis and Its Impact on Asthma conceptual work.30
Interestingly, we found that the patients with other additional disease(s) than CRS-related respiratory comorbidities had greater improvement of symptoms, but, again, only in the ESS group. This is in accordance with previous findings that depression patients, as well as elderly patients that usually have multiple diseases and medications, have good ESS outcomes if they do not have chronic diseases severely affecting general immunity.31,32
Female patients had better improvement in the VAS subscale scores of emotions and general health, independently of the operation technique. In contrast, Smith et al. showed that postoperative QoL was adversely affected by female sex.33 Intraoperative nasal polyps and Samter's triad were medical record–based exclusion criteria in our study; however, 19 patients reported previous doctor-diagnosed nasal polyps, and two patients reported nonsteroidal anti-inflammatory drug–induced wheezing symptoms. The possible explanation might be the resolution of nasal polyposis and underdiagnosed ASA sensitivity.
Multiple comments can be made on the drawbacks of this retrospective controlled study. The sample size was low, especially related to the subgroup analyses. We used a nonvalidated questionnaire on the VAS scores and were not able to observe the differences in the preoperative symptoms. Because there is still no evidence-based approval in public health care of Finland, balloon sinuplasty was performed in the private sector, whereas ESS was performed in the public sector. Thus, there might have been some differences in the social background of the patients, which might have also influenced the results. In the retrospective evaluation, the preoperative radiological findings of all sinuses were found to be slightly milder in the balloon sinusotomy group. This could possibly indicate that CRS might have been less severe in the balloon sinuplasty group and that a selection bias might have occurred. On the other hand, the groups were identical in the preoperative opacification of maxillary sinuses, in the duration of CRS symptoms, and in other medical history factors. The acute exacerbations after surgery were treated equally at public and private sectors in both groups.
CONCLUSION
In our study, ESS was slightly better in terms of the number of acute exacerbations. A better reduction of symptoms was achieved by the ESS procedure compared with balloon sinuplasty in patients with occupational or CRS-related risk factors, as well as in patients with other disease(s) than known CRS-related comorbidities. A prospective randomized controlled study with an increased number of patients is warranted.
ACKNOWLEDGMENTS
The authors thank Timo Pessi, M.Sc. (Datawell Finland, Inc., Espoo, Finland), for providing consultation in the statistical analysis. S. Toppila-Salmi, J. Myller, M. Penttila, and A. Koskinen designed the study and collected the data; S. Toppila-Salmi and A. Koskinen were involved in the data interpretation, literature search, and writing. All authors were responsible for critical review of the text.
Footnotes
Funded by the ethical committees of the Pirkanmaa Hospital District. Also funded in part by research grants from the Ahokas Foundation, the Competitive Research Funds of Hospital District of Helsinki and Uusimaa, and Pirkanmaa Hospital District, the Finnish Anti-Tuberculosis Association, the Finnish Society of Allergology and Immunology, the Finnish Society of Otorhinolaryngology, the Medical Research Fund of Päijät-Häme Central Hospital, the Tampere Tuberculosis Foundation, the Väinö and Laina Kivi Foundation, and the Yrjö Jahnsson Foundation
M Penttila is a main shareholder in Medical Instrument Co. (Otoplug Oy, Tampere, Fnland) that is marketing both balloon sinuplasty and endoscopic sinus surgery surgical instruments. The remaining authors have no conflicts of interest to declare pertaining to this article
REFERENCES
- 1. Hastan D, Fokkens WJ, Bachert C, et al. Chronic rhinosinusitis in Europe—An underestimated disease. A GA(2)LEN study. Allergy 66:1216–1223, 2011. [DOI] [PubMed] [Google Scholar]
- 2. Fokkens W, Lund V, Mullol J, et al. European position paper on rhinosinusitis and nasal polyps 2012. Rhinol Suppl 23:1–298, 2012. [PubMed] [Google Scholar]
- 3. Bousquet J, Bachert C, Canonica GW, et al. Unmet needs in severe chronic upper airway disease (SCUAD). J Allergy Clin Immunol 1243:428–433, 2009. [DOI] [PubMed] [Google Scholar]
- 4. Jarvis D, Newson R, Lotvall J, et al. Asthma in adults and its association with chronic rhinosinusitis: The GA2LEN survey in Europe. Allergy 67:91–98, 2012. [DOI] [PubMed] [Google Scholar]
- 5. Rudmik L, Smith TL. Quality of life in patients with chronic rhinosinusitis. Curr Allergy Asthma Rep 11:247–252, 2011. [DOI] [PubMed] [Google Scholar]
- 6. Kogevinas M, Zock JP, Jarvis D, et al. Exposure to substances in the workplace and new-onset asthma: An international prospective population-based study (ECRHS-II). Lancet 370:336–341, 2007. [DOI] [PubMed] [Google Scholar]
- 7. Syamlal G, Mazurek JM, Bang KM. Prevalence of lifetime asthma and current asthma attacks in U.S. working adults: An analysis of the 1997–2004 National Health Interview Survey data. J Occup Environ Med 51:1066–1074, 2009. [DOI] [PubMed] [Google Scholar]
- 8. Butland BK, Ghosh R, Strachan DP, et al. Job choice and the influence of prior asthma and hay fever. Occup Environ Med 68(7):494–501, 2011. [DOI] [PubMed] [Google Scholar]
- 9. Cummings KJ, Gaughan DM, Kullman GJ, et al. Adverse respiratory outcomes associated with occupational exposures at a soy processing plant. Eur Respir J 36:1007–1015, 2010. [DOI] [PubMed] [Google Scholar]
- 10. Hox V, Delrue S, Scheers H, et al. Negative impact of occupational exposure on surgical outcome in patients with rhinosinusitis. Allergy 67:560–565, 2012. [DOI] [PubMed] [Google Scholar]
- 11. Ragab SM, Lund VJ, Scadding G. Evaluation of the medical and surgical treatment of chronic rhinosinusitis: A prospective, randomised, controlled trial. Laryngoscope 114:923–930, 2004. [DOI] [PubMed] [Google Scholar]
- 12. Ragab SM, Lund VJ, Scadding G, et al. Impact of chronic rhinosinusitis therapy on quality of life: A prospective randomized controlled trial. Rhinology 48:305–311, 2010. [DOI] [PubMed] [Google Scholar]
- 13. Mendelsohn D, Jeremic G, Wright ED, Rotenberg BW. Revision rates after endoscopic sinus surgery: A recurrence analysis. Ann Otol Rhinol Laryngol 120:162–166, 2011. [DOI] [PubMed] [Google Scholar]
- 14. Welch KC, Stankiewicz JA. A contemporary review of endoscopic sinus surgery: Techniques, tools, and outcomes. Laryngoscope 119:2258–2268, 2009. [DOI] [PubMed] [Google Scholar]
- 15. Ahmed J, Pal S, Hopkins C, Jayaraj S. Functional endoscopic balloon dilation of sinus ostia for chronic rhinosinusitis. Cochrane Database Syst Rev 7:CD008515, 2011. [DOI] [PubMed] [Google Scholar]
- 16. Friedman M, Schalch P, Lin HC, et al. Functional endoscopic dilatation of the sinuses: Patient satisfaction, postoperative pain, and cost. Am J Rhinol 22(2):204–209, 2008. [DOI] [PubMed] [Google Scholar]
- 17. Ramadan HH, Terrell AM. Balloon catheter sinuplasty and adenoidectomy in children with chronic rhinosinusitis. Ann Otol Rhinol Laryngol 119:578–582, 2010. [DOI] [PubMed] [Google Scholar]
- 18. Plaza G, Eisenberg G, Montojo J, et al. Balloon dilation of the frontal recess: A randomized clinical trial. Ann Otol Rhinol Laryngol 120:511–518, 2011. [DOI] [PubMed] [Google Scholar]
- 19. Khalid AN, Smith TL, Anderson JC, et al. Fracture of bony lamellae within the frontal recess after balloon catheter dilatation. Am J Rhinol Allergy 24:55–59, 2010. [DOI] [PubMed] [Google Scholar]
- 20. Lund VJ, Mackay IS. Staging in rhinosinusitis. Rhinology 31:183–184, 1993. [PubMed] [Google Scholar]
- 21. Al Badaai Y, Samaha M. Outcome of endoscopic sinus surgery for chronic rhinosinusitis patients: A Canadian experience. J Laryngol Otol 124:1095–1099, 2010. [DOI] [PubMed] [Google Scholar]
- 22. Scadding G, Hellings P, Alobid I, et al. Diagnostic tools in rhinology EAACI position paper. Clin Transl Allergy 1:2, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Bozdemir K, Kutluhan A, Çetin H, et al. Comparison of outcomes of simple polypectomy plus balloon catheter dilatation versus functional endoscopic sinus surgery in nasal polyposis: A preliminary study. Am J Rhinol Allergy 25:198–200, 2011. [DOI] [PubMed] [Google Scholar]
- 24. Mann WJ, Tóth M, Gouveris H, Amedee RG. The drainage system of the paranasal sinuses: A review with possible implications for balloon catheter dilation. Am J Rhinol Allergy 25:245–248, 2011. [DOI] [PubMed] [Google Scholar]
- 25. Soler ZM, Sauer D, Mace J, Smith TL. Impact of mucosal eosinophilia and nasal polyposis on quality-of-life outcomes after sinus surgery. Otolaryngol Head Neck Surg 142:64–71, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Myller JP, Toppila-Salmi SK, Toppila EM, et al. Mucosal eosinophils and l-selectin ligands are associated with invasive and noninvasive sinus surgery outcomes. Am J Rhinol Allergy 23:21–27, 2009. [DOI] [PubMed] [Google Scholar]
- 27. Psaltis AJ, Weitzel EK, Ha KR, Wormald PJ. The effect of bacterial biofilms on post-sinus surgical outcomes. Am J Rhinol 22:1–6, 2008. [DOI] [PubMed] [Google Scholar]
- 28. Singhal D, Psaltis AJ, Foreman A, Wormald PJ. The impact of biofilms on outcomes after endoscopic sinus surgery. Am J Rhinol Allergy 24:169–174, 2010. [DOI] [PubMed] [Google Scholar]
- 29. Zhang Z, Linkin DR, Finkelman BS, et al. Asthma and biofilm-forming bacteria are independently associated with revision sinus surgeries for chronic rhinosinusitis. J Allergy Clin Immunol 128:221–223.e1, 2011. [DOI] [PubMed] [Google Scholar]
- 30. Bousquet J, Khaltaev N, Cruz AA, et al. Allergic Rhinitis and Its Impact on Asthma (ARIA) 2008 update (in collaboration with the world health organization, GA(2)LEN and AllerGen). Allergy 63(suppl 86):8–160, 2008. [DOI] [PubMed] [Google Scholar]
- 31. Litvack JR, Mace J, Smith TL. Role of depression in outcomes of endoscopic sinus surgery. Otolaryngol Head Neck Surg 144:446–451, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Reh DD, Mace J, Robinson JL, Smith TL. Impact of age on presentation of chronic rhinosinusitis and outcomes of endoscopic sinus surgery. Am J Rhinol 21:207–213, 2007. [DOI] [PubMed] [Google Scholar]
- 33. Mendolia-Loffredo S, Laud PW, Sparapani R, et al. Sex differences in outcomes of sinus surgery. Laryngoscope 116:1199–1203, 2006. [DOI] [PubMed] [Google Scholar]


