Abstract
Treatment of a dural arteriovenous fistula (AVF), which is difficult to access by either the surgical or endovascular approach, is challenging. A hybrid technique, combining a microsurgical approach and endovascular embolization, can provide less invasive management of dural AVFs in a modern neurosurgical hybrid operating suite. We present a case of intracerebral hemorrhage in the left cerebellum secondary to dural AVF, Cognard type IV with numerous tiny feeders from the ascending pharyngeal artery branches. No adequate arterial or venous route for endovascular embolization was found by neuroangiography. The hybrid technique, combining keyhole pterional craniotomy and embolization with n-butyl cyanoacrylate glue injection via direct cannulation of the periclival venous plexus, succeeded in obliterating the dural AVF. Intraoperative angiography showed successful embolization of the dural AVF without any complication. This report illustrates the usefulness of the neurosurgical hybrid operating suite for the treatment of difficult dural AVFs.
Keywords: Technique, Intervention, Fistula
Background
Dural arteriovenous fistula (AVF) with retrograde venous reflux is a potentially hazardous condition which can lead to the development of intracerebral hemorrhage. Treatment of this highly risky dural AVF must be aggressive.1 In general, the therapeutic strategies for dural AVFs include gamma knife radiosurgery for deep-seated fistula lesions or low-grade fistula, surgical obliteration for easily accessible lesions, and endovascular embolization (either transarterial or transvenous) is preferred in the majority of cases in the Onyx (ev3, Irvine, California, USA) era.2 Combining craniotomy and endovascular embolization with glue injection via direct puncture of the fistula is an alternative approach for specific types of dural AVF, such as cases where the anatomy prevents endovascular access or recurrence after failed endovascular treatment.
We describe a case of dural AVF which was not suitable for gamma knife radiosurgery due to the high potential for early rebleeding, and which was also not suitable for endovascular treatment because of an inadequate arterial or venous route for safe embolization. This case was difficult to treat by either the surgical or endovascular approach. Successful treatment was achieved using a hybrid technique, combining a keyhole pterional craniotomy and direct puncture of the fistula for glue injection in a modern hybrid operating suite.
Case presentation
A 72-year-old woman with diabetes mellitus and hypertension presented with sudden onset of loss of consciousness. A brain CT scan showed intracerebral hemorrhage in the left cerebellum and a well-enhanced nodule around the hematoma (figure 1A,B).
Figure 1.
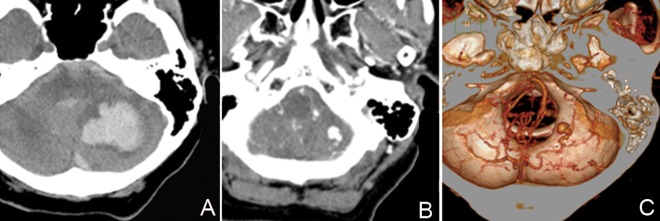
(A, B) CT scans showing left cerebellar hematoma and an enhanced nodule near the hematoma. (C) Reconstructive CT angiogram showing venous ectasia.
Investigations
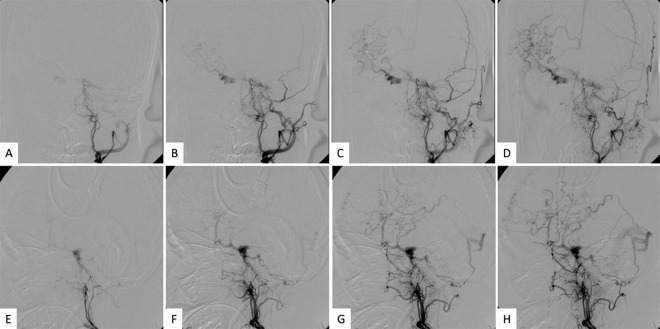
Brain CT angiography (CTA) showed a dural AVF, classified as Cognard type IV, with a venous ectasia near the hematoma (figure 1C). Digital subtraction angiography (DSA) demonstrated a dural AVF supplied by numerous tiny feeders from the branches of the ascending pharyngeal artery, which drained via the periclival venous plexus followed by reflux to the contralateral sylvian veins and via a posterior fossa vein to the transverse sinus (figure 2A–H).
Figure 2.
Series of preoperative digital subtraction angiograms of the left ascending pharyngeal artery (A–D: anteroposterior view; E–H: lateral view) show the feeders were from the branches of the ascending pharyngeal artery and drained via the periclival venous plexus to contralateral sylvian veins and via a posterior fossa vein to the transverse sinus.
Treatment
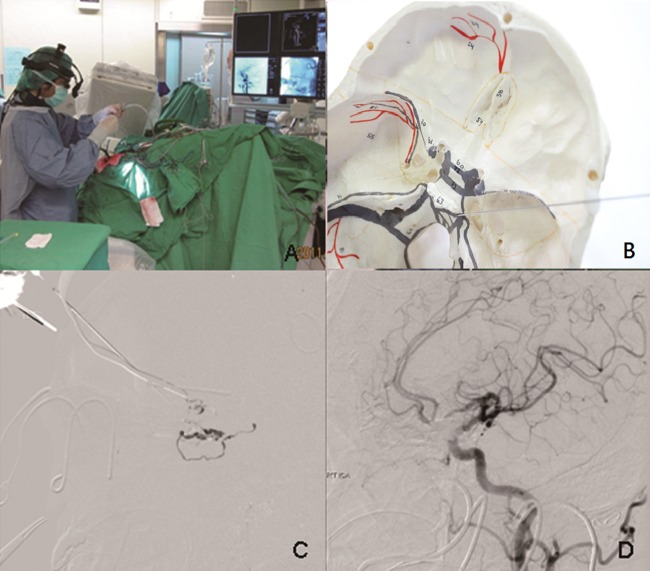
In the hybrid operating room which was equipped with a robotic angiographic fluoroscopy system, the Artis Zeego FD system (Siemens AG, Forchheim, Germany), the patient was placed in the supine position with the head turned 45° to the left side. Under general anesthesia, a short skin incision was made at the pterional area for keyhole craniotomy. The sylvian fissure was split and the brain was retracted gently. The posterior clinoid process was approached using microsurgical techniques and dilation of the venous plexus beneath the dura was confirmed by Doppler flow detector and intraoperative angiography. An 18-gauge spinal Quincke needle (Becton Dickinson, Madrid, Spain) was inserted into the periclival venous plexus under image guidance and tested with contrast injection (figure 3A,B). n-butyl cyanoacrylate (NBCA) glue was then injected slowly to fill the venous side of the dural AVF (figure 3C).
Figure 3.
(A) Photograph of hybrid surgery suite. (B) Skull model simulation of direct puncture to the periclival venous plexus with a needle. (C) Injection of n-butyl cyanoacrylate (NBCA) glue after craniotomy and direct puncture of the venous side of the fistula. (D) Intraoperative angiogram showing successful obliteration of the dural arteriovenous fistula.
Outcome and follow-up
The intraoperative DSA showed successful embolization of the dural AVF and the patient then recovered well without any complication (figure 3D).
Discussion
In the Onyx era, although the majority of high-grade dural AVFs were treated successfully by endovascular embolization,2 surgical obliteration is still important and necessary when anatomic features prevent endovascular treatment with either transarterial or transvenous access.3 However, some complex, deep-seated dural AVFs are difficult to gain surgical access without employing the invasive cranial base approach.4 Hybrid surgery, combining a keyhole craniotomy and direct puncture of the fistula, provides a less invasive and feasible alternative to treat difficult dural AVFs such as the case presented here.
The use of combined surgical and endovascular treatment of dural AVFs is hardly a new concept.5–8 However, this combination has rarely been reported due to the rarity of complex dural AVFs. Furthermore, most previous combined surgeries were performed in separate sessions due to the lack of facilities.9 In recent years the appearance of highly integrated surgical and endovascular cerebrovascular services has made hybrid surgery more widely available.10 This report highlights the value of the hybrid operating suite in allowing neurosurgeons to treat difficult dural AVFs effectively and safely with a less invasive method, combining open surgery and endovascular techniques simultaneously. In addition, the hybrid operating suite offers the ability to perform intraoperative cone beam CT images, which further enhances surgical results and patient safety during the procedure.
In our case, we approached the periclival venous plexus intradurally. The extradural approach described by Krist et al7 is another alternative method. The main difference between these methods is that the intradural approach allows relatively easy access to a deep-seated lesion through a keyhole craniotomy, whereas the extradural approach needs a larger craniotomy and wide dissection. In addition, although we used NBCA for embolization in this case as Onyx was not yet available in our hospital at that time, we believe that Onyx glue may provide better control than NBCA during hybrid surgery, based on the findings of our postoperative review.
Learning points.
Dural arteriovenous fistula (AVF) with retrograde venous reflux is a potentially hazardous condition which can lead to the development of intracerebral hemorrhage. Treatment of this highly risky dural AVF must be aggressive.
In general, treatment of dural AVF includes surgery, radiosurgery and endovascular embolization.
Hybrid surgery for complex dural AVFs is a less invasive and feasible alternative treatment.
The neurosurgical hybrid operating suite is very useful for the treatment of difficult dural AVFs.
Footnotes
Contributors: W-HC and C-CS made substantial contributions to the conception or design and acquisition of the work. S-CS and Y-ST were responsible for drafting the work or revising it critically for important intellectual content.
Competing interests: None.
Patient consent: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Pradilla G, Coon AL, Huang J, et al. Surgical treatment of cranial arteriovenous malformation and dural arteriovenous fistulas. Neurosurg Clin N Am 2012;23:105–22 [DOI] [PubMed] [Google Scholar]
- 2.Natarajan SK, Ghodke B, Kim LJ, et al. Multimodality treatment of intracranial dural arteriovenous fistulas in the Onyx era: a single center experience. World Neurosurg 2010;73:365–79 [DOI] [PubMed] [Google Scholar]
- 3.Kakarla UK, Deshmukh VR, Zabramski JM, et al. Surgical treatment of high-risk intracranial dural arteriovenous fistulae: clinical outcomes and avoidance of complications. Neurosurgery 2007;61:447–57 [DOI] [PubMed] [Google Scholar]
- 4.Kattner KA, Roth TC, Giannotta SL. Cranial base approaches for the surgical treatment of aggressive posterior fossa dural arteriovenous fistulae with leptomeningeal drainage: report of four technical cases. Neurosurgery 2002;50:1156–60 [DOI] [PubMed] [Google Scholar]
- 5.Hallaert GG, De Keukeleire KM, Vanhauwaert DJ, et al. Intracranial dural arteriovenous fistula successfully treated by combined open endovascular procedure. J Neurol Neurosurg Psychiatry 2010;81:685–9 [DOI] [PubMed] [Google Scholar]
- 6.Kong DS, Kwon KH, Kim JS, et al. Combined surgical approach with intraoperative endovascular embolization for inaccessible dural arteriovenous fistulas. Surg Neurol 2007;68:72–7 [DOI] [PubMed] [Google Scholar]
- 7.Krisht AF, Burson T. Combined pretemporal and endovascular approach to the cavernous sinus for the treatment of carotid-cavernous dural fistulae: technical case report. Neurosurgery 1999;44:415–18 [DOI] [PubMed] [Google Scholar]
- 8.Spiotta AM, Sivapatham T, Hussain MS, et al. Combined surgical and endovascular approach to a complex dural arteriovenous fistula involving the superior sagittal sinus and torcula. J Stroke Cerebrovasc Dis 2012;21:283–8 [DOI] [PubMed] [Google Scholar]
- 9.Rath SA, Derakshani S. Concepts of combined endovascular and surgical treatment for dural arteriovenous fistulae: concepts derived from experience in treating three unusual lesions. Acta Neurochir (Wien) 2004;146:229–35 [DOI] [PubMed] [Google Scholar]
- 10.Murayama Y, Arakawa H, Ishibashi T, et al. Combined surgical and endovascular treatment of complex cerebrovascular diseases in the hybrid operating room. J Neurointerv Surg 2013;5:489–93 [DOI] [PubMed] [Google Scholar]