Abstract
Objectives
Few studies have investigated overweight trajectories and psychosocial adjustment among adolescents. We conducted analyses with data from the multisite Study of Early Child Care and Youth Development (SECCYD).
Methods
Sample included 1,350 youth born in 1991. Data consisted of repeated measures of weight, height, and multiple subscales of internalizing and externalizing behavioral problems measured by the Child Behavior Checklist (CBCL) from age nine to age 15.
Results
Three trajectory patterns were identified: never/rarely overweight/obese (59.5%), late start/light overweight/obese (12.1%), and chronically/heavy overweight/obese (28.4%). Youths with chronically/heavy overweight/obese trajectory pattern had significantly higher scores of internalizing problems over time, as well as syndrome subscales of somatic complaints, social problems and social withdrawal over time than youths with the never/rare overweight/obese trajectory pattern. There was no significant difference in either broad-band behavioral problems or narrow-band syndrome subscales between youths with the never/rare overweight/obese trajectory pattern and those with the late start/light overweight/obesity trajectory pattern.
Conclusions
Study findings may advance knowledge on the distinct developmental trajectory patterns of overweight youth and their linkages to the psychosocial adjustment during the period of pubertal transition. The results highlight the need for future prevention research to improve the physical development and mental well-being of adolescents.
Keywords: Overweight Trajectories, Psychosocial Adjustment, Adolescents
Introduction
More than 17% of U.S. adolescents are considered obese (Ogden et al., 2006). Given the fact that obesity is viewed as a non-desirable and stigmatizing characteristic in the American culture, and that many youth are preoccupied with cultural expectations of a slim body as the standard of beauty, being obese has been assumed to predispose youth to depressive symptoms (Merikangas et al., 2012; Roberts, 2000; Sanchez-Villegas et al., 2012; Ting et al., 2012), social isolation (Strauss and Pollack, 2003; Xie, 2005), low self-esteem (Lau et al., 2004), poor health-related quality of life (Pinhas-Hamiel et al., 2006; Tyler et al., 2007), and psychosocial adjustment problems(Erermis et al., 2004). With the development of cognitive functioning during adolescence, the process of self-appraisal and social comparison of body image and physical attractiveness is presumed more operative and relevant to psychosocial adjustment problems among adolescents than among children (Bradley et al., 2008; Harter, 2006). However, mixed empirical findings concerning the extent and nature of psychosocial adjustment problems among obese youth are reported in the literature. Several cross-sectional studies reported a modest relationship (Eisenberg et al., 2003; Falkner et al., 2001) while others report no relationship (Daniels, 2005; Erickson et al., 2000; Lamertz et al., 2002) between being obese in adolescence and psychosocial adjustment problems in that population segment. Few studies have been conducted utilizing longitudinal design and the direction of causality remains unresolved. Early history of obesity and chronic obese or overweight status may lead to the risk of psychosocial adjustment problems (Bradley et al., 2008; Mustillo et al., 2003; Zametkin et al., 2004), whereas early psychosocial adjustment problems may also shape subsequent overweight or obese status (Goodman and Whitaker, 2002; Pine et al., 1997).
Bradley and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Network examined the complex interrelationships between obesity and internalizing and externalizing problems from infancy to middle childhood with data from the multisite NICHD Study of Early Child Care and Youth Development (SECCYD) (Bradley et al., 2008). Longitudinal analyses were conducted on relationships between BMI and scores on the Child Behavior Checklist (CBCL) from age 2 years through the 6th grade. There was no consistent association between BMI and psychosocial adjustment problems prior to school entry and modest significant lagged associations from BMI to internalizing problems were observed as early as in 1st grade, although no relation was found between being overweight and conduct problems. In this paper, we used the SECCYD data and applied the advanced group-based growth mixture and mixed-effect modeling approaches to further investigate the obesity trajectories and their links to multiple psychosocial adjustment problems in adolescents during the period of pubertal transition.
Methods
Sample and Data
The SECCYD followed a sample of 1,364 children from infancy (1 month) through age 15 (about grade 9) and their families, who were recruited from 10 locations in the US in 1991. The initial cohort includes 24% ethnic minority children (13% African American, 6% Hispanic, 2% Asian or Native American, and 3% Other), 11% mothers who had not completed high school, and 14% single-parent mothers. Additional details about the data collection procedures and instruments can be found in the study's Manuals of Operations and Instrument Documentation (http://secc.rti.org/summary.cfm) and in previous publications (O'Brien et al., 2007). Although we focused our analyses on the pubertal transition period (age 9 to 15), data on socio-demographic characteristics, overweightness and psychosocial adjustment collected prior to adolescence were also included in our analyses. There were only 14 underweight cases at grade 3 (about age 9), a number insufficient to achieve sufficient statistical power. To avoid misclassification with normal cases, we excluded underweight cases and included only normal and overweight/obese cases in the analysis. As age 9 served as the baseline for the analysis period of the developmental trajectory, we excluded cases based only on underweight at age 9 and not underweight at other ages. As a result, the final sample used for this analysis was 1,350 (697 boys and 653 girls). Not all 1,350 subjects had valid height and weight measures, creating a smaller, but statistically robust, subset of 1,350 total subjects. The exact number of subjects with valid weight and height measures varied from age group to age group, as grouped by grade 3 through grade 9 to age 15 years (i.e. 924 at grade 3, 916 at grade 5, 905 at grade 6, 791 at grade 7, 732 at grade 8 and 836 at grade 9). There was no significant difference in gender (χ2=3.07, p=0.08) and ethnicity (χ2=0.56, p=0.46) between subjects with and without complete weight and height data, but subjects with missing data reported significantly higher income-to-need ratio at grade 3 than those without missing cases in weight and height (5.38±5.14 vs. 4.15±3.32, p=0.002). The full information maximum likelihood (FIML) was applied to compute maximum likelihood parameter estimates and standard errors from data with missing values. FIML provides efficient estimation of statistical parameters from incomplete data, and parameter estimates from FIML provide less biased information than ad hoc procedures, such as listwise deletion, pairwise deletion, or single imputation of means (Little, 2002; LK Muthen, Muthen, BO, 2001; Schafer, 1997).
Measures
Weight and Height were measured following standardized procedures and measures at grades 3, 5, 6, 7, 8 and age 15 were included in our analysis. BMI was calculated by dividing weight (kg) by height (m) squared. Overweight and obesity were defined based on BMI values between 85th and 95th, and ≥95th for age- and gender-specific percentile cutoffs referenced in the 2000 CDC Growth Charts of children and adolescents in the United States(Committee., 2007; Kuczmarski et al., 2002). The categories of overweight and obesity were combined in the analysis to create a single overweight/obesity category.
Internalizing and Externalizing Problems were measured by the Child Behavior Checklist (CBCL) (Achenbach, 1991). The CBCL is a parental report of child function that includes measures of social competence, school function, emotional adjustment, and behavior problems. Standardized scores can be produced in eight syndrome subscales, which include withdrawn, somatic complaints, anxious/depressed, social problems, thought problems, attention problems, delinquent behavior, and aggressive behavior. The standardized scores are also produced for three total scales combining the eight syndromes: internalizing scales based on syndrome subscales such as withdrawn, somatic complaints, and anxious/depressed syndromes, the externalizing scale based on syndrome subscales such as the delinquent and aggressive behaviors, and a total social competence score based on all eight syndromes. Average scores of child ratings from mother and father/other adults at grades 3, 4, 5, 6 and age 15 (coded as time 0, 1, 2, 3, 6) were used in our analysis. The inter-rater correlation coefficients between mother's and father/other adult's ratings ranged from 0.40 to 0.47 for internalizing problems and from 0.55 to 0.61 for externalizing problems from grade 3 (about age 9 years) to age 15 years.
Pubertal Timing was measured by an annual physical exam and Tanner staging by a nurse practitioner starting at 9½ years of age, following the standard instructions from the American Academy of Pediatrics Manual Assessment of Sexual Maturity States in Girls(Herman-Giddens, 1995) and Tanner's original criteria (Tanner, 1990) in boys. The age of onset of menarche was asked annually by a nurse starting at 10½ years of age. Adolescents who did not agree to participate in the Tanner staging assessment were asked to complete the self-reported Pubertal Development Scale (PDS)(Petersen, 1988). Stages of pubertal status can be approximated from the PDS based on self-reported growth spurt, body and facial hair development, and skin and voice changes. Specific stages include pre-puberty, beginning puberty, mid-puberty, end of puberty, and post-puberty. A high reliability of PDS (range = .68-.78) as well as validity (median correlation = .70) were reported. The PDS also included a question assessing girls' menstrual status and their age (in months) at first menstruation. A total of 432 girls and 427 boys had valid pubertal assessments for at least 1 of the 7 assessments (taken annually from age 9 1/2 years) (Susman et al., 2010). The sample size of PDS reports varied from year to year (271-495 for boys and 254-482 for girls). The timing of pubertal onset was quantified as a variable created by the NICHD SECCYD with the latent transition analysis and nonlinear mixed modeling based on two dimensions of development (genital and pubic hair for boys and breast and pubic hair for girls) (Blozis, 2004; Collins, 2002). The variable provided an estimated age of pubertal onset for the 959 subjects (476 girls and 483 boys) with values ranging from 1 (began puberty at <9.5 years) to 6 (began puberty at >13.5 years). We used this variable for the present analysis.
Other socio-demographic variables including gender, self-reported ethnicity, and income-to-needs ratios as a proxy measure of socioeconomic status were also included in the analysis. An income-to-needs ratio was calculated by dividing self-reported income by the poverty level for that family size based on the Federal Poverty Guidelines (O'Brien et al., 2007).
Data Analysis
Descriptive statistics (mean, standard deviation and percentage) were calculated to reflect the background characteristics of the sample. Group-based Growth Mixture Modeling (GMM) approach implemented in SAS Proc Traj was employed to classify the growth trajectory patterns of overweight/obese status subjects (JONES, 2001; Nagin, 1999). We used GMM because the estimated response growth curve from conventional longitudinal models is based on the assumption that all individuals in the sample come from a single population, which may not be able to capture the heterogeneity of growth trajectories of behavioral outcomes during adolescence. The GMM approach is able to identify the underlying growth curves of overweight/obese status (i.e. the average growth trajectory class or membership) as a categorical latent variable, and estimate posterior probabilities of class membership for all individuals (B. Muthen, 2001; Nagin, 1999). The heterogeneity of developmental trajectory in growth factors (i.e. initial status and slope) was captured in a categorical latent class variable. The number of latent classes was determined by Bayesian Information Criterion (BIC) which is derived using the likelihood function (-2lnL), number of parameters (k) and the sample size (n) (Schwarz, 1978). The model with the smallest BIC indicates that the specified model is the best fit with the data (B. Muthen, 2001; Nagin, 1999). The BIC generally penalizes free parameters more strongly than does the Akaike Information Criterion (AIC), though it depends on the size of n and relative magnitude of n and k. Preliminary analyses suggested linear trajectory pattern rather than other patterns (e.g. quadratic and cubic) best fit with the data. Additionally, theoretical justification and interpretability were also considered to determine the number of latent classes (Bauer and Curran, 2003; Jung, 2008; Muthen, 2003; Rindskopf, 2003). Each adolescent was assigned to a most probable trajectory class of overweight/obese status based on the estimated posterior probability of trajectory class membership. Misclassification of group membership was evaluated by the average posterior probability with close to 1 being considered as an acceptable value for adequate classification (Nagin, 1999). Similar trajectory patterns were observed with either categorical overweight/obese status or continuous BMI z-scores. In this study we reported the patterns analyzed with categorical overweight/obese status. Finally, General Linear Mixed-Effect modeling implemented in SAS Proc Mixed was used to link the identified trajectory patterns of overweight/obese status to the repeatedly measured internalizing and externalizing behavioral problems. Gender, ethnicity, income-to-needs ratio, and timing of puberty were adjusted in the models. All statistical analyses were carried out using SAS (version 8.0; SAS Institute, Cary, NC).
Results
The majority of the analysis sample was White (80.59%), and proportions of American Indian or Eskimo, Aleutian, Asian or Pacific Islander, and African American were 0.37%, 1.56% and 12.96%, respectively. Average income-to-needs ratio was 4.40 (SD of 3.79) at grade 3, and the mean score of timing for puberty was 2.81 (SD of 1.14). The score was significantly higher in boys (3.27±1.10) than girls (2.33±0.99) (p<0.001). Table 1 presents a summary of weight status across ages 9-15. Higher proportions of overweight/obese was observed in boys than girls with significant difference found at grade 8 (p=0.014) and age 15 (p<0.01).
Table 1. Weight Status from Ages 9-15.
| Weight Status (n (%)) | Female | Male | All |
|---|---|---|---|
| Grade 3 (About age 9) | |||
| Normal | 335(71.1%) | 296(65.3%) | 631(68.3%) |
| Overweight | 69(14.6%) | 67(14.8%) | 136(14.7%) |
| Obese | 67(14.2%) | 90(19.9%) | 157(17%) |
| Grade 5 | |||
| Normal/Underweight | 312(68.4%) | 289(62.8%) | 601(65.6%) |
| Overweight | 67(14.7%) | 67(14.6%) | 134(14.6%) |
| Obese | 77(16.9%) | 104(22.6%) | 181(19.8%) |
| Grade 6 | |||
| Normal/Underweight | 310(67.1%) | 283(63.9%) | 593(65.5%) |
| Overweight | 76(16.5%) | 66(14.9%) | 142(15.7%) |
| Obese | 76(16.5%) | 94(21.2%) | 170(18.8%) |
| Grade 7 | |||
| Normal/Underweight | 266(68.6%) | 252(62.5%) | 518(65.5%) |
| Overweight | 61(15.7%) | 62(15.4%) | 123(15.6%) |
| Obese | 61(15.7%) | 89(22.1%) | 150(19%) |
| Grade 8 | |||
| Normal/Underweight | 246(71.3%) | 243(62.8%) | 489(66.8%) |
| Overweight | 56(16.2%) | 61(15.8%) | 117(16%) |
| Obese | 43(12.5%) | 83(21.4%) | 126(17.2%) |
| Grade 9 (about Age 15) | |||
| Normal/Underweight | 310(73.8%) | 264(63.5%) | 574(68.7%) |
| Overweight | 56(13.3%) | 75(18%) | 131(15.7%) |
| Obese | 54(12.9%) | 77(18.5%) | 131(15.7%) |
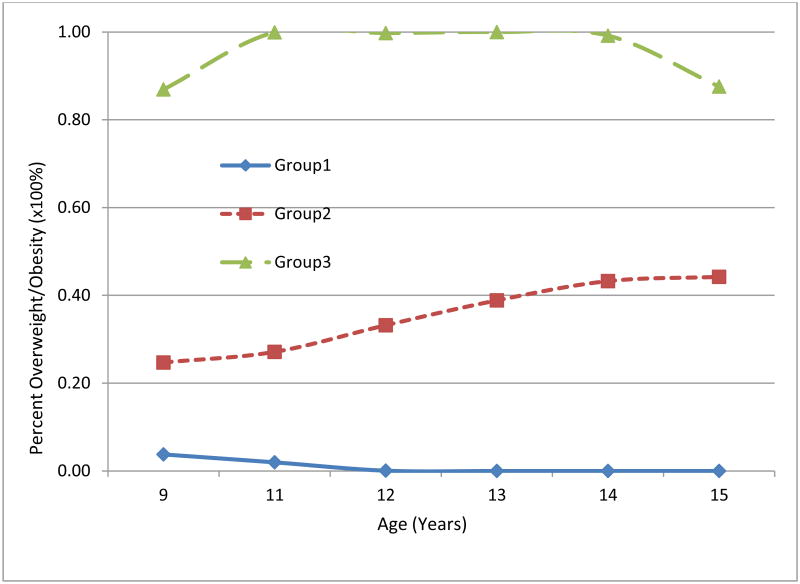
The GMM modeling approach was applied to identify the developmental trajectories of overweight or obesity status. Two-group (BIC=-1664.72), three-group (BIC=-1613.21), and four-group (BIC=-1625.97) models were tested (Table 2). Based on the BIC criterion, a three-group model was selected as the best fitting model. Figure 1 presents the observed trajectories for each of three trajectory groups. The three trajectory groups were labeled as never/rarely overweight/obese (Group 1, 59.5%), late start/light overweight/obese (Group 2, 12.1%), and chronically/heavy overweight/obese (Group 3, 28.4%). The average class posterior probability for each group was 0.933 (Group 1), 0.947 (Group 2) and 0.965 (Group 3), respectively.
Table 2. Bayesian Information Criteria (BIC) and Average Class Probability for Mixture Models.
| Model | Bayesian Information Criterion (BIC) | ||
|---|---|---|---|
| Two-Group Model | -1664.72 | ||
| Three-Group Model | -1613.21 | ||
| Four-Group Model | -1625.97 | ||
| Five-Group Model | NA | ||
| Average Class Probability | |||
|
| |||
| Final Three-Group Model | 1 | 2 | 3 |
|
| |||
| Group 1 | 0.933 | 0.055 | 0.012 |
| Group 2 | 0.027 | 0.947 | 0.026 |
| Group 3 | 0.005 | 0.03 | 0.965 |
Figure 1.
Percent of overweight/obesity versus age for three groups of trajectories. Groups of weight trajectory patterns: Group 1 for never/rarely overweight/obese; Group 2 for late start/light overweight/obese; Group 3 for chronically/heavy overweight/obese.
Tables 3 and 4a and 4b present results comparing mean scores of broad-band behavioral problems (i.e. internalizing, externalizing behavioral problems, and total competence score) as well as each specific narrow-band syndrome subscales across identified trajectory groups of overweight/obese status over the period from age 9 to age 15. With adjustments for gender, ethnicity, income-to-needs ratio and timing of pubertal onset, youths with chronically/heavy overweight/obese trajectory pattern (i.e. group 3) had significantly higher scores of internalizing problems over time (p=0.016 for time x group interaction and p=0.018 for time x time x group interaction) than youths with a never/rare overweight/obese trajectory pattern (i.e. group 1). Additionally, syndrome subscales of somatic complaints (p=0.028 for time x group interaction and borderline significant p=0.06 for time x time x group interaction), social problems (p=0.026 for time x group interaction and p=0.044 for time x time x group interaction) and social withdrawal overtime (p=0.012 for time x group interaction and p=0.046 for time x time x group interaction) than youths with a never/rare overweight/obese trajectory pattern (i.e. group 1). There was no significant difference in either broad-band behavioral problems or narrow-band syndrome subscales between youths with a never/rare overweight/obese trajectory pattern and those with a late start/light overweight/obese trajectory pattern. In addition, we also explored potential gender interactions with identified trajectory groups on these behavioral problems. There were no significant gender interactions on either broad-band behavioral problems or specific narrow-band syndrome subscales.
Table 3.
Broad-band Behavioral Problems across Groups of Weight Trajectory Patterns.
| Unadjusted Mean (SD) | Adj. Mean Difference(95% CI) | P-Value | Adj. Mean Difference(95% CI) | P-Value | |||
|---|---|---|---|---|---|---|---|
| Group 1 | Group 2 | Group 3 | Group 1 vs. 2 | Group 1 vs. 3 | |||
| Externalizing Behavioral Problems | |||||||
| Time 0 | 47.03 (8.91) |
47.37 (8.78) |
48.87 (8.70) |
0.17 (-1.72 - 2.07) | 0.86 | -1.21 (-2.62 - 0.21) | 0.096 |
| Time 1 | 45.96 (8.90) |
46.86 (8.90) |
48.14 (9.01) |
-0.04 (-1.94 - 1.86) | 0.97 | -1.48 (-2.90 - -0.05) | 0.043 |
| Time 2 | 44.82 (9.10) |
45.81 (9.82) |
46.80 (9.13) |
-0.26 (-2.16 - 1.65) | 0.79 | -1.14 (-2.57 - 0.28) | 0.117 |
| Time 3 | 45.62 (9.21) |
46.25 (9.23) |
47.22 (9.85) |
0.15 (-1.75 - 2.04) | 0.88 | -0.99 (-2.42 - 0.44) | 0.174 |
| Time 6 | 45.10 (9.62) |
46.02 (9.02) |
47.36 (10.33) |
0.05 (-1.85 - 1.96) | 0.96 | -1.47 (-2.91 - -0.03) | 0.046 |
| Time*Group | 0.635 | ||||||
| Time*Time*Group | 0.570 | ||||||
| Internalizing Behavioral Problems | |||||||
| Time 0 | 48.13 (8.91) |
48.10 (8.34) |
49.39 (8.97) |
0.34 (-1.52 - 2.19) | 0.72 | -0.92 (-2.30 - 0.47) | 0.195 |
| Time 1 | 47.33 (8.78) |
47.62 (8.59) |
49.21 (8.81) |
0.11 (-1.74 - 1.96) | 0.91 | -1.53 (-2.92 - -0.13) | 0.032 |
| Time 2 | 47.69 (8.95) |
47.84 (8.17) |
49.79 (8.84) |
0.41 (-1.45 - 2.27) | 0.66 | -1.60 (-3.00 - -0.21) | 0.025 |
| Time 3 | 46.75 (8.74) |
47.74 (9.35) |
49.74 (9.75) |
-0.39 (-2.24 - 1.47) | 0.68 | -2.37 (-3.76 - -0.97) | 0.001 |
| Time 6 | 46.19 (8.86) |
46.86 (8.37) |
47.93 (9.91) |
0.06 (-1.81 - 1.92) | 0.95 | -1.21 (-2.62 - 0.20) | 0.094 |
| Time*Group | 0.016 | ||||||
| Time*Time*Group | 0.018 | ||||||
| Total Social Competence Score | |||||||
| Time 0 | 46.87 (9.39) |
47.28 (8.94) |
49.35 (8.97) |
0.12 (-1.88 - 2.11) | 0.91 | -1.83 (-3.33 - -0.34) | 0.016 |
| Time 1 | 45.41 (9.41) |
46.46 (9.57) |
48.57 (9.16) |
-0.18 (-2.18 - 1.82) | 0.86 | -2.41 (-3.92 - -0.91) | 0.002 |
| Time 2 | 44.85 (9.78) |
45.46 (9.73) |
47.81 (9.40) |
0.14 (-1.87 - 2.15) | 0.89 | -2.10 (-3.60 - -0.59) | 0.006 |
| Time 3 | 44.79 (9.63) |
45.56 (10.33) |
48.22 (10.14) |
0.10 (-1.90 - 2.10) | 0.92 | -2.61 (-4.12 - -1.11) | 0.001 |
| Time 6 | 44.03 (10.41) |
45.14 (9.60) |
47.09 (11.01) |
-0.07 (-2.08 - 1.94) | 0.95 | -2.22 (-3.74 - -0.70) | 0.004 |
| Time*Group | 0.286 | ||||||
| Time*Time*Group | 0.340 | ||||||
Results from random-effect models with adjustment of gender, ethnicity, income-to-needs ratio and timing of puberty. Time 0, 1,2,3,6 were coded for assessment occasions at grade 3, 4, 5, 5 and 9 (about age 15). Groups of weight trajectory patterns: Group 1 for never/rarely overweight/obese; Group 2 for late start/light overweight/obese; Group 3 for chronically/heavy overweight/obese.
Table 4a.
Narrow-band Syndrome Subscales of Behavioral Problems across Groups of Weight Trajectory Patterns.
| Unadjusted Mean (SD) | Adj. Mean Difference(95% CI) | P-Value | Adj. Mean Difference(95% CI) | P-Value | |||
|---|---|---|---|---|---|---|---|
| Group 1 | Group 2 | Group 3 | Group 1 vs. 2 | Group 1 vs. 3 | |||
| Aggressive Behavior | |||||||
| Time 0 | 52.73 (4.56) |
52.86 (5.39) |
53.45 (5.13) |
0.10 (-0.90 - 1.10) | 0.85 | -0.54 (-1.29 - 0.21) | 0.158 |
| Time 1 | 52.36 (4.49) |
52.78 (4.86) |
53.20 (5.13) |
-0.04 (-1.05 - 0.96) | 0.93 | -0.69 (-1.44 - 0.07) | 0.074 |
| Time 2 | 52.20 (4.55) |
52.80 (5.08) |
52.75 (4.57) |
-0.35 (-1.35 - 0.66) | 0.50 | -0.32 (-1.08 - 0.43) | 0.400 |
| Time 3 | 52.46 (4.38) |
52.74 (4.87) |
53.28 (5.22) |
0.12 (-0.88 - 1.12) | 0.81 | -0.57 (-1.33 - 0.18) | 0.137 |
| Time 6 | 52.28 (4.66) |
52.35 (4.57) |
53.32 (6.10) |
0.33 (-0.68 - 1.33) | 0.53 | -0.75 (-1.51 - 0.02) | 0.055 |
| Time*Group | 0.724 | ||||||
| Time*Time*Group | 0.614 | ||||||
| Anxious/Depressed Syndromes | |||||||
| Time 0 | 53.25 (4.84) |
52.75 (4.46) |
53.77 (5.58) |
0.64 (-0.36 - 1.63) | 0.21 | -0.39 (-1.13 - 0.35) | 0.303 |
| Time 1 | 52.73 (4.74) |
52.72 (4.44) |
53.41 (5.05) |
0.17 (-0.82 - 1.17) | 0.73 | -0.64 (-1.39 - 0.11) | 0.095 |
| Time 2 | 52.83 (4.80) |
52.59 (4.31) |
53.38 (4.76) |
0.40 (-0.60 - 1.40) | 0.44 | -0.43 (-1.18 - 0.32) | 0.264 |
| Time 3 | 52.54 (4.48) |
52.91 (5.30) |
53.69 (5.36) |
-0.20 (-1.20 - 0.79) | 0.69 | -0.91 (-1.66 - -0.16) | 0.017 |
| Time 6 | 52.30 (4.10) |
52.13 (4.13) |
52.87 (4.81) |
0.46 (-0.54 - 1.46) | 0.37 | -0.38 (-1.14 - 0.38) | 0.326 |
| Time*Group | 0.149 | ||||||
| Time*Time*Group | 0.132 | ||||||
| Attentiveness Problems | |||||||
| Time 0 | 54.16 (5.94) |
54.24 (6.02) |
54.48 (6.07) |
0.23 (-0.91 - 1.37) | 0.69 | -0.12 (-0.98 - 0.73) | 0.779 |
| Time 1 | 53.65 (5.57) |
53.88 (5.58) |
54.05 (5.90) |
0.19 (-0.95 - 1.34) | 0.74 | -0.11 (-0.97 - 0.75) | 0.803 |
| Time 2 | 53.47 (5.55) |
53.57 (5.47) |
53.59 (5.15) |
0.19 (-0.96 - 1.34) | 0.75 | 0.27 (-0.59 - 1.14) | 0.531 |
| Time 3 | 53.17 (4.92) |
53.40 (5.17) |
53.85 (5.67) |
0.08 (-1.06 - 1.22) | 0.89 | -0.31 (-1.17 - 0.55) | 0.477 |
| Time 6 | 52.95 (4.73) |
52.96 (5.12) |
53.73 (5.88) |
0.33 (-0.82 - 1.48) | 0.58 | -0.48 (-1.35 - 0.39) | 0.279 |
| Time*Group | 0.730 | ||||||
| Time*Time*Group | 0.466 | ||||||
| Delinquent Behavior | |||||||
| Time 0 | 52.76 (4.49) |
52.86 (4.82) |
53.22 (4.69) |
0.25 (-0.71 - 1.22) | 0.61 | -0.09 (-0.81 - 0.64) | 0.813 |
| Time 1 | 52.52 (4.50) |
52.75 (4.31) |
52.94 (4.87) |
0.17 (-0.80 - 1.14) | 0.73 | -0.11 (-0.84 - 0.62) | 0.773 |
| Time 2 | 52.51 (4.37) |
52.90 (4.91) |
52.91 (4.56) |
0.02 (-0.96 - 0.99) | 0.97 | -0.00 (-0.73 - 0.73) | 0.995 |
| Time 3 | 52.44 (4.28) |
52.80 (4.60) |
52.97 (4.88) |
0.05 (-0.92 - 1.02) | 0.92 | -0.15 (-0.87 - 0.58) | 0.696 |
| Time 6 | 52.82 (4.89) |
52.83 (4.39) |
53.84 (5.56) |
0.43 (-0.54 - 1.41) | 0.39 | -0.68 (-1.43 - 0.06) | 0.072 |
| Time*Group | 0.759 | ||||||
| Time*Time*Group | 0.416 | ||||||
Results from random-effect models with adjustment of gender, ethnicity, income-to-needs ratio and timing of puberty. Time 0, 1,2,3,6 were coded for assessment occasions at grade 3, 4, 5, 5 and 9 (about age 15). Groups of weight trajectory patterns: Group 1 for never/rarely overweight/obese; Group 2 for late start/light overweight/obese; Group 3 for chronically/heavy overweight/obese.
Table 4b.
Narrow-band Syndrome Subscales of Behavioral Problems across Groups of Weight Trajectory Patterns.
| Unadjusted Mean (SD) | Adj. Mean Difference(95% CI) | P-Value | Adj. Mean Difference(95% CI) | P-Value | |||
|---|---|---|---|---|---|---|---|
| Group 1 | Group 2 | Group 3 | Group 1 vs. 2 | Group 1 vs. 3 | |||
| Somatic Complaints | |||||||
| Time 0 | 54.51 (5.18) |
54.43 (5.38) |
55.09 (5.53) |
0.35 (-0.79 - 1.49) | 0.55 | -0.43 (-1.28 - 0.42) | 0.321 |
| Time 1 | 54.51 (5.42) |
54.96 (5.33) |
55.40 (5.08) |
-0.20 (-1.34 - 0.94) | 0.73 | -0.60 (-1.46 - 0.26) | 0.174 |
| Time 2 | 54.69 (5.41) |
55.15 (5.40) |
55.90 (5.97) |
-0.02 (-1.18 - 1.13) | 0.97 | -0.81 (-1.68 - 0.05) | 0.064 |
| Time 3 | 54.26 (5.25) |
55.14 (6.04) |
56.13 (6.36) |
-0.57 (-1.71 - 0.57) | 0.33 | -1.50 (-2.36 - -0.64) | 0.001 |
| Time 6 | 54.27 (5.49) |
55.16 (5.50) |
55.51 (6.45) |
-0.48 (-1.63 - 0.68) | 0.42 | -0.84 (-1.72 - 0.04) | 0.061 |
| Time*Group | 0.028 | ||||||
| Time*Time*Group | 0.060 | ||||||
| Social Problems | |||||||
| Time 0 | 52.29 (4.39) |
52.82 (4.72) |
54.28 (6.07) |
-0.41 (-1.41 - 0.60) | 0.43 | -1.89 (-2.64 - -1.14) | <.0001 |
| Time 1 | 51.90 (4.00) |
52.82 (4.99) |
54.36 (5.90) |
-0.62 (-1.62 - 0.39) | 0.23 | -2.32 (-3.07 - -1.56) | <.0001 |
| Time 2 | 52.03 (4.32) |
52.85 (4.87) |
54.33 (6.02) |
-0.69 (-1.70 - 0.32) | 0.18 | -2.11 (-2.87 - -1.36) | <.0001 |
| Time 3 | 52.07 (3.97) |
52.76 (5.54) |
55.23 (6.53) |
-0.28 (-1.29 - 0.72) | 0.58 | -2.90 (-3.66 - -2.15) | <.0001 |
| Time 6 | 51.66 (3.69) |
52.33 (4.70) |
54.03 (5.68) |
-0.45 (-1.47 - 0.56) | 0.38 | -2.26 (-3.02 - -1.49) | <.0001 |
| Time*Group | 0.026 | ||||||
| Time*Time*Group | 0.044 | ||||||
| Thought Problems | |||||||
| Time 0 | 53.25 (5.09) |
52.73 (4.23) |
53.67 (5.14) |
0.54 (-0.45 - 1.53) | 0.29 | -0.43 (-1.17 - 0.31) | 0.259 |
| Time 1 | 52.92 (4.97) |
53.18 (4.70) |
53.35 (4.86) |
-0.04 (-1.03 - 0.96) | 0.94 | -0.21 (-0.96 - 0.54) | 0.583 |
| Time 2 | 52.82 (4.78) |
52.56 (4.31) |
53.06 (4.62) |
0.39 (-0.61 - 1.39) | 0.45 | 0.08 (-0.67 - 0.83) | 0.831 |
| Time 3 | 52.46 (4.48) |
52.87 (4.85) |
52.70 (4.81) |
-0.15 (-1.14 - 0.84) | 0.77 | 0.08 (-0.67 - 0.82) | 0.841 |
| Time 6 | 52.46 (4.31) |
52.46 (4.28) |
52.87 (5.13) |
0.18 (-0.82 - 1.18) | 0.72 | -0.09 (-0.85 - 0.67) | 0.820 |
| Time*Group | 0.181 | ||||||
| Time*Time*Group | 0.243 | ||||||
| Withdrawn | |||||||
| Time 0 | 52.82 (4.53) |
52.80 (4.09) |
53.03 (4.50) |
0.24 (-0.73 - 1.22) | 0.62 | 0.02 (-0.71 - 0.74) | 0.967 |
| Time 1 | 52.54 (4.60) |
52.50 (4.01) |
53.10 (4.80) |
0.30 (-0.67 - 1.28) | 0.54 | -0.36 (-1.10 - 0.37) | 0.332 |
| Time 2 | 52.75 (4.81) |
52.58 (3.95) |
53.36 (5.05) |
0.39 (-0.59 - 1.37) | 0.44 | -0.39 (-1.12 - 0.35) | 0.300 |
| Time 3 | 52.29 (4.29) |
53.00 (5.14) |
53.57 (5.70) |
-0.43 (-1.41 - 0.54) | 0.38 | -1.06 (-1.79 - -0.32) | 0.005 |
| Time 6 | 52.18 (4.41) |
52.06 (4.16) |
53.21 (5.50) |
0.45 (-0.54 - 1.43) | 0.37 | -0.69 (-1.44 - 0.05) | 0.068 |
| Time*Group | 0.012 | ||||||
| Time*Time*Group | 0.046 | ||||||
Results from random-effect models with adjustment of gender, ethnicity, income-to-needs ratio and timing of puberty. Time 0, 1,2,3,6 were coded for assessment occasions at grade 3, 4, 5, 5 and 9 (about age 15). Groups of weight trajectory patterns: Group 1 for never/rarely overweight/obese; Group 2 for late start/light overweight/obese; Group 3 for chronically/heavy overweight/obese.
Discussion
The developmental course of overweight or obese status may not follow the same trajectory pattern among adolescents. In this study, three distinct trajectory patterns were identified and labeled as never/rarely overweight/obese (59.5%), late start/light overweight/obese (12.1%), and chronically/heavy overweight/obese (28.4%). In prior studies among children and adolescents, multiple distinct trajectories have been reported. Li et al. examined overweight trajectory patterns among 1,739 White, Black, and Hispanic children followed from age 2 to age 12 from the National Longitudinal Study of Youth 1979 (NLSY79). A three-group trajectory pattern similar to our findings was identified, and the groups were labeled as early onset overweight, late onset overweight, and never overweight (Li et al., 2007). Balistreri et al. used data from the Early Childhood Longitudinal Study-Kindergarten Cohort (ECLS-K), a nationally representative sample of US kindergartners, to identify three distinct patterns of weight gain from kindergarten through eighth grade (Balistreri and Van Hook, 2011). The trajectory patterns were labeled as consistently normal weight, always overweight/obesity and gradually becoming overweight/obesity. Similarly, Mustillo et al. reported a four-group trajectory pattern over an 8-year period among 991 White youth aged 9 to 16 years living in rural areas in the Great Smoky Mountains Study (Mustillo et al., 2003). Four developmental trajectories of obesity were labeled as no obesity, chronic obesity, childhood obesity and adolescent obesity. Lee et al used the same SECCYD data source as in this study and reported three-group trajectory patterns (i.e. highest, intermediate and lowest trajectories) of BMI z-scores among boys aged 2 to 12 years (Lee et al., 2010). Nonnemaker et al and Chen et al used the data of the 1997 National Longitudinal Survey of Youth (NLSY97) to extend the exploration from adolescence to young adulthood with a separate age ranges of 12-23 and 12-28 year olds and identified four to seven trajectory patterns of overweight and obesity risks (Chen, 2012; Nonnemaker et al., 2009). Identifying the underlying heterogeneous developmental trajectories during adolescence provides insights into the natural history of overweight development. Future research should now search for genetic, familial and other processes that lead to these different patterns. Such research has the potential for providing information to be used for the development of tailored obesity prevention programs (Rapkin and Dumont, 2000).
Given that obesity status is viewed as an undesirable and stigmatizing characteristic in the American culture, the process of self-appraisal or social comparison may account for why obese individuals are at a heightened risk for negative psychological and behavioral outcomes, beyond the physical conditions associated with obesity (Crosnoe and Muller, 2004; Needham and Crosnoe, 2005). The Reflected Self-Appraisal Hypothesis is based on Cooley's concept of the “looking-glass self”, which posits that an individual's self-concept, defined as the internalized view we have of ourselves, is socially constructed through the judgment of others and self-appraisal (Cooley, 1964; Hayes, 1986; Rose, 1994). The Social Comparison Theory suggests that individuals engage in a process of self-evaluation, comparing themselves to others who they believe possess desirable social and cultural traits and, in turn, engage in behaviors designed to achieve the desired characteristics (Festinger, 1954). Based on these mechanisms, the beliefs, feelings and thoughts about our body (i.e. weight, size, shape, function, capacities and appearance) are affected and refined by external social influences when we make external social comparisons with others and internalize the reflected appraisals. Our analysis using longitudinal data revealed that the chronically/heavy overweight/obese trajectory was significantly and positively associated with internalizing behavioral problems as well as several related syndrome subscales including somatic complaints, social problems and social withdrawal. The increased behavioral problems observed among adolescents with chronically/heavy overweight/obese trajectories could be attributed to the stigmatization of overweight/obese status in Westernized societies, specifically American culture. Our results were consistent with findings from a longitudinal study conducted by Mustillo and colleagues that explored the differential effects of transitory or chronic overweight trajectories on the risk of psychiatric disorder among children aged 9 to 16 years. A significant association was observed only in children with chronic overweight trajectories (Mustillo et al., 2003). Bradley et al (Bradley et al., 2008) also found that as a child entered middle school, higher BMI scores predicted the development of internalized problems, such as depression and anxiety. In addition, Anderson and associates reported a modest relationship between BMI and externalizing behaviors using the data from SECCYD (Anderson et al., 2010). Their results from Linear Mixed-Effect Models indicated that externalizing behavior was correlated to higher BMI starting at age 2 until 12 years. Additionally, for children with high levels of externalizing behavior, there was an increase in ¾ of a BMI unit in comparison to children with low levels of externalizing behavior. Such findings were not replicated in this study, however. We did not observe the linkage of overweight trajectory to externalizing behavioral problems or externalizing related syndrome subscales such as aggressive behavior and delinquent behavior.
Major strengths of this study lie in its ability to assess how the relationship between obesity and psychosocial aspects change over time with the application of an advanced statistical approach to identify the heterogeneous overweight/obesity trajectories. A limitation of this study is the use of BMI as a proxy measure of adiposity as it does not differentiate body weight due to fat mass and lean body mass. We lacked measures to determine abdominal adiposity, such as waist circumference, or other markers of total adiposity such as body fat mass measured by skinfold thickness or bioelectrical impedance analysis, which would also be relevant to psychological behavioral problems. The potential risks of Type I error inflation due to multiple testing in the analyses may not be completely ignored, as the nominal p values of unadjusted or adjusted mean difference between groups were reported. However, the p values for comparisons between the chronically/heavy overweight/obese trajectory pattern (i.e. group 3) and the never/rare overweight/obese trajectory pattern (i.e. group 1) on several behavioral problems at certain time points (e.g. p=0.001 for internalizing behavioral problems at time 3) remained statistically significant after conservative Bonferroni correction. Finally, the latent growth curve mixture and mixed-effect modeling approaches adopted in this study allows for the identification of the heterogeneity of overweight growth trajectories and enables us to further investigate the linkages of identified trajectory patterns to the psychosocial and adjustment behavioral problems over time. However, we may not be able to completely eliminate the possibility of the causal path from psychosocial problems to overweight trajectories. Other alternative modeling approaches such as the dynamic Latent Different Score (LDS) modeling may aid in the investigation of the developmental course of reciprocal interrelations of overweight and psychosocial problems (McArdle, 2001; McArdle, 1994). Despite these limitations, study findings may advance knowledge on the distinct developmental trajectory patterns of overweight/obesity status and their linkages to the psychosocial adjustment during the period of pubertal transition. The results highlight the need for future prevention research to improve the physical development and mental well-being of adolescents.
Highlights.
We investigated the distinct developmental trajectory patterns of overweight status
A longitudinal data of 1,350 youth during the period from age 9to 15 was used
Chronically/heavy overweight/obese trajectory was linked to internalizing problems
Linkage was also observed in somatic complaints, social problems and withdrawal
Acknowledgments
This research was supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development (Grant # R03HD058122) and was also partially supported by the National Institute of Diabetes and Digestive and Kidney Diseases (Grant # R21DK088313).
Footnotes
Authors Contribution: BX was responsible for the data analysis and preparation of the manuscript. KI and CL conducted literature search and review and prepared the introduction section of the manuscript. DVP and EJS contributed to preparation of the manuscript. No author has any financial or personal relationships with the organization sponsoring this research. The corresponding author has full access to all the data in the study and had final responsibility for the decision to submit for publication.
Conflict of Interest Statement: The authors declare that there are no conflicts of interests.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Achenbach TM. Manual for the Teacher's Report Form and 1991 Profile. University of Vermont, Department of Psychiatry; Burlington, VT: 1991. [Google Scholar]
- Anderson SE, He X, Schoppe-Sullivan S, Must A. Externalizing behavior in early childhood and body mass index from age 2 to 12 years: longitudinal analyses of a prospective cohort study. BMC Pediatr. 2010;10:49. doi: 10.1186/1471-2431-10-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balistreri KS, Van Hook J. Trajectories of overweight among US school children: a focus on social and economic characteristics. Matern Child Health J. 2011;15:610–9. doi: 10.1007/s10995-010-0622-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer DJ, Curran PJ. Distributional assumptions of growth mixture models: implications for overextraction of latent trajectory classes. Psychological methods. 2003;8:338–63. doi: 10.1037/1082-989X.8.3.338. [DOI] [PubMed] [Google Scholar]
- Blozis S. Structured latent curve models for the study of change in multivaiate repeated measures. Psychological methods. 2004;9:334–53. doi: 10.1037/1082-989X.9.3.334. [DOI] [PubMed] [Google Scholar]
- Bradley RH, Houts R, Nader PR, O'Brien M, Belsky J, Crosnoe R. The relationship between body mass index and behavior in children. J Pediatr. 2008;153:629–34. doi: 10.1016/j.jpeds.2008.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X, Brogan K. Developmental trajectories of overweight and obesity of US youth through the life course of adolescence to young adulthood. Adolescent Health, Medicine and Therapeutics. 2012;3:33–42. doi: 10.2147/AHMT.S30178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins L, Flaherty BP. Latent clas models for longitudinal data. In: Hagenaars J, McCutcheon AL, editors. Applied Latent Class Analysis. Cambridge University Press; Cambridge: 2002. pp. 287–303. [Google Scholar]
- Committee., B.S.a.t.E. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007 Dec;120(Supplement):S164–S92. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- Cooley C. Human nature and the social order. Schocken; New York: 1964. [Google Scholar]
- Crosnoe R, Muller C. Body mass index, academic achievement, and school context: examining the educational experiences of adolescents at risk of obesity. J Health Soc Behav. 2004;45:393–407. doi: 10.1177/002214650404500403. [DOI] [PubMed] [Google Scholar]
- Daniels J. Weight and weight concerns: Are they associated with reported depressive symptoms in adolescents? J Pediatr Health Care. 2005;19:33–41. doi: 10.1016/j.pedhc.2004.07.007. [DOI] [PubMed] [Google Scholar]
- Eisenberg ME, Neumark-Sztainer D, Story M. Associations of weight-based teasing and emotional well-being among adolescents. Archives of pediatrics & adolescent medicine. 2003;157:733–8. doi: 10.1001/archpedi.157.8.733. [DOI] [PubMed] [Google Scholar]
- Erermis S, Cetin N, Tamar M, Bukusoglu N, Akdeniz F, Goksen D. Is obesity a risk factor for psychopathology among adolescents? Pediatr Int. 2004;46:296–301. doi: 10.1111/j.1442-200x.2004.01882.x. [DOI] [PubMed] [Google Scholar]
- Erickson SJ, Robinson TN, Haydel KF, Killen JD. Are overweight children unhappy?: Body mass index, depressive symptoms, and overweight concerns in elementary school children. Archives of pediatrics & adolescent medicine. 2000;154:931–5. doi: 10.1001/archpedi.154.9.931. see comments. [DOI] [PubMed] [Google Scholar]
- Falkner NH, Neumark-Sztainer D, Story M, Jeffery RW, Beuhring T, Resnick MD. Social, educational, and psychological correlates of weight status in adolescents. Obes Res. 2001;9:32–42. doi: 10.1038/oby.2001.5. [DOI] [PubMed] [Google Scholar]
- Festinger L. A theory of social comparison processes. Human Relations. 1954;7:117–40. [Google Scholar]
- Goodman E, Whitaker RC. A prospective study of the role of depression in the development and persistence of adolescent obesity. Pediatrics. 2002;110:497–504. doi: 10.1542/peds.110.3.497. [DOI] [PubMed] [Google Scholar]
- Harter S. Developmental and Individual Difference Perspectives on Self-Esteem. In: Mroczek DK, Little TD, editors. Handbook of Personality Development. Erlbaum; Mahwah, NJ: 2006. pp. 311–34. [Google Scholar]
- Hayes D, Rose CE. Body and mind: the effect of exercise, overweight, and physical health on psychological well-being. J Health Soc Behav. 1986;27:387–400. [PubMed] [Google Scholar]
- Herman-Giddens MB, C J. Assessment of sexual maturity stages in girls. American Academy of Pediatrics; Elk Grove Village, IL: 1995. [Google Scholar]
- JONES BL, Nagin DS, Roeder K. A SAS Procedure Based on Mixture Models for Estimating Developmental Trajectories. SOCIOLOGICAL METHODS & RESEARCH. 2001;29:374–93. [Google Scholar]
- Jung T, Wickrama KAS. An Introduction to Latent Class Growth Analysis and Growth Mixture Modeling. Social and Personality Psychology Compass. 2008:302–17. [Google Scholar]
- Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, Wei R, Curtin LR, Roche AF, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital & Health Statistics - Series 11: Data From the National Health Survey. 2002:1–190. [PubMed] [Google Scholar]
- Lamertz CM, Jacobi C, Yassouridis A, Arnold K, Henkel AW. Are obese adolescents and young adults at higher risk for mental disorders? A community survey. Obes Res. 2002;10:1152–60. doi: 10.1038/oby.2002.156. [DOI] [PubMed] [Google Scholar]
- Lau PW, Lee A, Ransdell L, Yu CW, Sung RY. The association between global self-esteem, physical self-concept and actual vs ideal body size rating in Chinese primary school children. Int J Obes Relat Metab Disord. 2004;28:314–9. doi: 10.1038/sj.ijo.0802520. [DOI] [PubMed] [Google Scholar]
- Lee JM, Kaciroti N, Appugliese D, Corwyn RF, Bradley RH, Lumeng JC. Body mass index and timing of pubertal initiation in boys. Archives of pediatrics & adolescent medicine. 2010;164:139–44. doi: 10.1001/archpediatrics.2009.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li C, Goran MI, Kaur H, Nollen N, Ahluwalia JS. Developmental trajectories of overweight during childhood: role of early life factors. Obesity (Silver Spring) 2007;15:760–71. doi: 10.1038/oby.2007.585. [DOI] [PubMed] [Google Scholar]
- Little R, Rubin DB. Statistical Analysis With Missing Data. John Wiley & Sons; New York, NY: 2002. [Google Scholar]
- McArdle JJ. A latent difference score approach to longitudinal dynamic structural analyses. In: Cudeck R, du Toit S, Sorbom D, editors. Structural Equation Modeling: Present and future. SSI; Lincolnwood, IL: 2001. pp. 342–80. [Google Scholar]
- McArdle JJN, J R. Structuring data to study development and change. In: Cohen SHR, H W, editors. Life-span developmental psychology: Methodological innovations. Lawrence Erlbaum Associates, Inc.; Hillsdale, NJ: 1994. pp. 223–67. [Google Scholar]
- Merikangas AK, Mendola P, Pastor PN, Reuben CA, Cleary SD. The association between major depressive disorder and obesity in US adolescents: results from the 2001-2004 National Health and Nutrition Examination Survey. J Behav Med. 2012;35:149–54. doi: 10.1007/s10865-011-9340-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustillo S, Worthman C, Erkanli A, Keeler G, Angold A, Costello EJ. Obesity and psychiatric disorder: developmental trajectories. Pediatrics. 2003;111:851–9. doi: 10.1542/peds.111.4.851. [DOI] [PubMed] [Google Scholar]
- Muthen B. Latent variable mixture modeling. In: Marcoulides G, Schumacker RE, editors. New Developments and Techniques in Structural Equation Modeling. Lawrence Erlbaum Associates; 2001. pp. 1–33. [Google Scholar]
- Muthen B. Statistical and substantive checking in growth mixture modeling: comment on Bauer and Curran (2003) Psychological methods. 2003;8:369–77. doi: 10.1037/1082-989X.8.3.369. discussion 84-93. [DOI] [PubMed] [Google Scholar]
- Muthen L, Muthen BO. Mplus User's Guide (Second Edition) 2nd. Muthen & Muthen; Los Angeles, CA, USA: 2001. [Google Scholar]
- Nagin D. Analyzing developmental trajectories: A semi-parametric, group-based approach. Psychological methods. 1999;4:139–57. doi: 10.1037/1082-989x.6.1.18. [DOI] [PubMed] [Google Scholar]
- Needham BL, Crosnoe R. Overweight status and depressive symptoms during adolescence. J Adolesc Health. 2005;36:48–55. doi: 10.1016/j.jadohealth.2003.12.015. [DOI] [PubMed] [Google Scholar]
- Nonnemaker JM, Morgan-Lopez AA, Pais JM, Finkelstein EA. Youth BMI trajectories: evidence from the NLSY97. Obesity (Silver Spring) 2009;17:1274–80. doi: 10.1038/oby.2009.5. [DOI] [PubMed] [Google Scholar]
- O'Brien M, Nader PR, Houts RM, Bradley R, Friedman SL, Belsky J, Susman E. The ecology of childhood overweight: a 12-year longitudinal analysis. Int J Obes (Lond) 2007 doi: 10.1038/sj.ijo.0803611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. Jama. 2006;295:1549–55. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- Petersen A, Crockett L, Richards M, Boxer A. A self-report measure of pubertal status: Reliability, validity, and initial forms. Journal of Youth and Adolescence. 1988;17:117–33. doi: 10.1007/BF01537962. [DOI] [PubMed] [Google Scholar]
- Pine DS, Cohen P, Brook J, Coplan JD. Psychiatric symptoms in adolescence as predictors of obesity in early adulthood: a longitudinal study. Am J Public Health. 1997;87:1303–10. doi: 10.2105/ajph.87.8.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinhas-Hamiel O, Singer S, Pilpel N, Fradkin A, Modan D, Reichman B. Health-related quality of life among children and adolescents: associations with obesity. Int J Obes (Lond) 2006;30:267–72. doi: 10.1038/sj.ijo.0803107. [DOI] [PubMed] [Google Scholar]
- Rapkin BD, Dumont KA. Methods for identifying and assessing groups in health behavioral research. Addiction. 2000;95(Suppl 3):S395–417. doi: 10.1080/09652140020004304. [DOI] [PubMed] [Google Scholar]
- Rindskopf D. Mixture or homogeneous? Comment on Bauer and Curran (2003) Psychological methods. 2003;8:364–8. doi: 10.1037/1082-989X.8.3.364. discussion 84-93. [DOI] [PubMed] [Google Scholar]
- Roberts DF. Media and youth: access, exposure, and privatization. J Adolesc Health. 2000;27:8–14. doi: 10.1016/s1054-139x(00)00128-2. [DOI] [PubMed] [Google Scholar]
- Rose CE. Overweight and depression. J Health Soc Behav. 1994;35:63–79. [PubMed] [Google Scholar]
- Sanchez-Villegas A, Field AE, O'Reilly EJ, Fava M, Gortmaker S, Kawachi I, Ascherio A. Perceived and actual obesity in childhood and adolescence and risk of adult depression. J Epidemiol Community Health. 2012 doi: 10.1136/jech-2012-201435. [DOI] [PubMed] [Google Scholar]
- Schafer J. Analysis of incomplete multivariate data. Chapman & Hall; London: 1997. [Google Scholar]
- Schwarz G. Estimating the dimension of a model. Ann Statist. 1978;6:461–4. [Google Scholar]
- Strauss RS, Pollack HA. Social marginalization of overweight children. Archives of pediatrics & adolescent medicine. 2003;157:746–52. doi: 10.1001/archpedi.157.8.746. [DOI] [PubMed] [Google Scholar]
- Susman EJ, Houts RM, Steinberg L, Belsky J, Cauffman E, Dehart G, Friedman SL, Roisman GI, Halpern-Felsher BL, et al. Longitudinal development of secondary sexual characteristics in girls and boys between ages 91/2 and 151/2 years. Archives of pediatrics & adolescent medicine. 2010;164:166–73. doi: 10.1001/archpediatrics.2009.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanner J. Fetus into man: Physical growth from conception to maturity (revised) Harvard University Press; Cambridge, MA: 1990. [Google Scholar]
- Ting WH, Huang CY, Tu YK, Chien KL. Association between weight status and depressive symptoms in adolescents: role of weight perception, weight concern, and dietary restraint. Eur J Pediatr. 2012;171:1247–55. doi: 10.1007/s00431-012-1753-1. [DOI] [PubMed] [Google Scholar]
- Tyler C, Johnston CA, Fullerton G, Foreyt JP. Reduced quality of life in very overweight Mexican American adolescents. J Adolesc Health. 2007;40:366–8. doi: 10.1016/j.jadohealth.2006.10.015. [DOI] [PubMed] [Google Scholar]
- Xie B, Chou C, Spruijt-Metz D, Liu C, Xia J, Gong J, Li Y, Johnson CA. Effects of Perceived Peer Isolation and Social Support availability on the Relationship between Relative Body Mass Index and Depressive Symptoms. Int J Obes. 2005;29:1137–43. doi: 10.1038/sj.ijo.0803006. [DOI] [PubMed] [Google Scholar]
- Zametkin AJ, Zoon CK, Klein HW, Munson S. Psychiatric aspects of child and adolescent obesity: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 2004;43:134–50. doi: 10.1097/00004583-200402000-00008. [DOI] [PubMed] [Google Scholar]