Abstract
Background
Clinicians are sometimes advised to make decisions using thresholds in measured variables, derived from prognostic studies.
Objectives
We studied why there are conflicting apparently-optimal prognostic thresholds, for example in exercise peak oxygen uptake (pVO2), ejection fraction (EF), and Brain Natriuretic Peptide (BNP) in heart failure (HF).
Data Sources and Eligibility Criteria
Studies testing pVO2, EF or BNP prognostic thresholds in heart failure, published between 1990 and 2010, listed on Pubmed.
Methods
First, we examined studies testing pVO2, EF or BNP prognostic thresholds. Second, we created repeated simulations of 1500 patients to identify whether an apparently-optimal prognostic threshold indicates step change in risk.
Results
33 studies (8946 patients) tested a pVO2 threshold. 18 found it prognostically significant: the actual reported threshold ranged widely (10–18 ml/kg/min) but was overwhelmingly controlled by the individual study population's mean pVO2 (r = 0.86, p<0.00001). In contrast, the 15 negative publications were testing thresholds 199% further from their means (p = 0.0001). Likewise, of 35 EF studies (10220 patients), the thresholds in the 22 positive reports were strongly determined by study means (r = 0.90, p<0.0001). Similarly, in the 19 positives of 20 BNP studies (9725 patients): r = 0.86 (p<0.0001).
Second, survival simulations always discovered a “most significant” threshold, even when there was definitely no step change in mortality. With linear increase in risk, the apparently-optimal threshold was always near the sample mean (r = 0.99, p<0.001).
Limitations
This study cannot report the best threshold for any of these variables; instead it explains how common clinical research procedures routinely produce false thresholds.
Key Findings
First, shifting (and/or disappearance) of an apparently-optimal prognostic threshold is strongly determined by studies' average pVO2, EF or BNP. Second, apparently-optimal thresholds always appear, even with no step in prognosis.
Conclusions
Emphatic therapeutic guidance based on thresholds from observational studies may be ill-founded. We should not assume that optimal thresholds, or any thresholds, exist.
Introduction
Although most clinicians are aware that the majority of biological variables with diagnostic and prognostic value act continuously within populations, they are encouraged to accept recommendations for decision strategies that specify a threshold of a measured continuous variable. Such thresholds often arise from cohort studies that dichotomise patients into subgroups with significantly different prognoses.
Peak oxygen consumption (peak VO2) is the most widely accepted quantitative prognostic marker in heart failure following the seminal work of Mancini et al. [1] who reported that cardiac transplantation could be deferred in heart failure patients with a peak VO2 of greater than 14 ml/kg/min. Current eligibility for cardiac transplantation, more than twenty years on, still hinges on whether the peak VO2 is less than a threshold of 14 ml/kg/min [2] or 12 ml/kg/min in those patients taking beta-blockers [3]. The presence of two conflicting diagnostic thresholds illustrates that studies [4]–[7] and international guidelines [8]–[10] have since assessed a variety of alternative, competing, “optimal” thresholds for peak VO2 with conflicting results. Some recent studies even question the prognostic effectiveness of peak VO2 [11]–[13], having tested a threshold and failing to find it statistically significant.
The same is true for many other variables used in daily practice. Two examples from imaging and biochemistry, of variables obviously continuous in nature but often dichotomized, are left ventricular ejection fraction (EF)[14]–[16] and Brain Natriuretic Peptide (BNP)[17]–[20]. Each has a range of competing reportedly “optimal” prognostic thresholds.
There are two alternative explanations for these discrepancies. One widely-accepted explanation is that there is a true universal threshold in each variable beyond which prognosis is poor, but modern therapy such as beta-blockade is affecting prognosis so powerfully that the prognostic thresholds have changed [10], [21].
An alternative explanation is that we have misunderstood what a statistically significant difference in prognosis between subgroups tells us. In this explanation, if (for example) a tested peak VO2 threshold is far from the middle of a particular cohort, dichotomisation will yield groups of markedly unequal sizes, which would reduce the statistical power to detect a mortality difference between the groups. In contrast, testing a peak VO2 threshold nearer the middle, with more equal group sizes, may yield a statistically significant result. If this second explanation is the true one, then variation in the mean value of peak VO2 between studies could be enough to make their apparently optimal prognostic thresholds differ.
In this article we comprehensively explore the cause of the discrepancy between studies in their selected optimum prognostic cut point, first by examining published data and separately by performing numerical simulations in which we could know the underlying shape of the relationship between risk factor and risk.
Methods
Part 1: Examination of Published Studies
We performed a PubMed literature search (http://www.ncbi.nlm.nih.gov/PubMed) for the three variables of interest (peak VO2, LVEF and BNP), in the setting of heart failure, in the period 1990 to 2010. We used as keywords (limit of research: human, all adults 19+ years) “oxygen consumption, heart failure, mortality”, which extracted 287 articles, “ejection fraction, heart failure, mortality”, which extracted 2296 articles, and “BNP, heart failure, mortality”, which extracted 346 articles. Three authors read the full articles to extract the data of interest (as shown in Table 1). Reference lists of these articles were also searched for additional articles.
Table 1. The 33 studies reporting a positive (white) or negative (grey) statistical significance of a prognostic threshold of peak VO2.
| Author | Publication Year | Number of patients | Age (years) | Males (%) | EF (%) | Primary outcome | Max duration of follow-up (months) | Number of events | Mean±SD peak VO2 (ml/kg/min) | Tested threshold (ml/kg/min) | Tested threshold prognostically significant? |
| Szlachcic | 1985 | 27 | 56±16 | 100 | 22±16 | overall mortality | 24 | 14 | 11,5±1,4 | 10 | yes |
| Cohn* | 1986 | 273 | 53±13 | 100 | Nr | overall mortalty | 60 | nr | 15±nr | 14,5 | yes |
| Likoff | 1987 | 201 | 62±10 | 75 | 20±10 | overall mortality | 28 | 85 | 13,0±4,0 | 13 | yes |
| Mancini | 1991 | 116 | 50±11 | 84 | 19±7 | overall mortality | 25 | 25 | 14,7±5,3 | 14 | yes |
| Parameshwar | 1992 | 127 | 55±9 | 89 | 22±12 | overall mortality+urgent transplant | 42 | 41 | 15,3±5,3 | 14 | yes |
| Van den Broek | 1992 | 94 | 57±11 | 83 | 22±9 | overall mortality | 36 | 21 | 17,0±5,0 | 16 | yes |
| Saxon | 1993 | 528 | 50±12 | 80 | 20±7 | cardiac mortality+urgent transplant | 12 | 129 | 12,0±4,0 | 11 | yes |
| Di Salvo | 1995 | 67 | 51±10 | 79 | 22±7 | cardiac mortality | nr | 32 | 11,8±4,2 | 14 | no |
| Chomsky | 1996 | 185 | 51±11 | 78 | 22±7 | cardiac mortality | 100 | 35 | 12,9±3,0 | 10 | yes |
| Cohen-Solal | 1997 | 178 | 52±11 | 90 | 25±11 | overall mortality+urgent transplant | 24 | 38 | 17,6±5,6 | 17 | yes |
| Robbins | 1999 | 470 | 52±11 | 71 | 21±8 | cardiac mortality | 60 | 26 | 18,0±6,0 | 14 | no |
| Metra | 1999 | 219 | 55±10 | 93 | 22±7 | cardiac mortality+urgent transplant | 40 | 29 | 14,2±4,4 | 14 | yes |
| Isnard | 2000 | 264 | 51±12 | 81 | 27±10 | overall mortality+urgent transplant | 82 | 83 | 17,1±6,8 | 14 | no |
| Osman | 2000 | 225 | 54±12 | 80 | 23±13 | overall mortality | 40 | 29 | 16,0±5,9 | 14 | yes |
| Davies | 2000 | 50 | 76±5 | 70 | 33±14 | overall mortality | 60 | 26 | 15,2±4,5 | 14,7 | yes |
| Clark | 2000 | 60 | 59±12 | nr | 30±15 | overall mortality | 100 | 20 | 19,9±7,7 | 17,5 | yes |
| Williams | 2001 | 219 | 56±13 | 76 | Nr | overall mortality | 63 | 27 | 23,1±9,2 | 14 | no |
| Ponikowski | 2001 | 80 | 58±9 | 76 | 24±12 | overall mortality | 36 | 37 | 18,3±6,7 | 14 | no |
| Hansen | 2001 | 311 | 54±10 | 84 | 22±10 | cardiac mortality | 38 | 65 | 14,7±5,5 | 14 | yes |
| Mejhert | 2002 | 67 | 74±6 | 66 | 36±11 | overall mortality | 60 | 14 | 11,7±3,7 | 14 | no |
| Gitt | 2002 | 223 | 63±11 | 86 | 29±8 | cardiac mortality | 24 | 46 | 15,8±5,3 | 14 | yes |
| Rostagno | 2003 | 214 | 64±10 | 55 | 41±14 | overall mortality | 70 | 66 | 18,7±4,1 | 14 | no |
| Schalcher | 2003 | 146 | 52±10 | 87 | 27±13 | overall mortality+urgent transplant | 61 | 41 | 18,4±5,4 | 14 | no |
| O' Neill* | 2005 | 1196 | 54±11 | 75 | 19±7 | overall mortality | 72 | nr | 16,6±5,1 | 14 | yes |
| Bard | 2006 | 355 | 51±10 | 72 | 22±8 | overall mortality+urgent transplant | 46 | 145 | 17,3±5,0 | 14 | no |
| Nanas | 2006 | 98 | 51±12 | 89 | 31±13 | cardiac mortality | 30 | 27 | 19,1±5,9 | 15 | no |
| Guazzi | 2007 | 288 | 55±13 | 67 | 33±13 | cardiac mortality | 33 | 62 | 15,5±5,0 | 14,1 | no |
| Guazzi | 2007 | 156 | 61±9,4 | 80 | 35±10 | cardiac mortality | 42 | 34 | 16,8±4,5 | 14,4 | no |
| Rossi | 2007 | 273 | 62±9 | 87 | 33±8 | cardiac mortality | 75 | 40 | 16,6±4,5 | 16 | yes |
| Arena | 2008 | 353 | 59±14 | 72 | 28±9 | cardiac mortality+urgent transplant | 48 | 104 | 14,5±5,6 | 14 | no |
| Kazuhiro | 2009 | 148 | 63±12 | 100 | 35±11 | cardiac mortality | 67 | 13 | 18,2±3,7 | 14 | no |
| Arena | 2010 | 520 | 58±12 | 77 | 35±14 | cardiac mortality | 48 | 79 | 16,6±6,2 | 14 | no |
| Sachdeva | 2010 | 1215 | 53±13 | 75 | 23±7 | overall mortality | 24 | 234 | 13,1±2,0 | 14 | yes |
EF = left ventricular ejection fraction; nr = not reported.
Selection criteria
We included all studies on prognostic markers (peak VO2, LVEF or BNP) in heart failure that met the following criteria:
quoted a mean or median value for the study population
reported statistical significance of a single threshold
Clinical trials, which might have a confounding effect of allocation to study arms, were excluded, unless they reported results for a control arm independently. We included studies regardless of whether the prognostic threshold was found to be statistically significant or non-significant.
Part 2: Evaluation in a population known to have no step in risk
We determined, using survival data of a simulated population with a gradual spectrum of a notional continuous risk factor, and definitely no step change in prognosis, whether an “optimal threshold” for the risk factor would appear to arise when the data were analysed by the techniques typically used in prognostic studies and at what value such thresholds appeared.
In the case of peak VO2, mortality rises progressively across a wide range, for example giving 2-year mortality of 3%, 7%, 10%, 13%, and 18% in subpopulations with mean peak VO2 of 17, 15, 13, 11, 9 ml/kg/min, respectively [22]. For this reason we started simulating a condition in which the relationship between the risk factor and mortality was linear. We subsequently studied non-linear relationships (see below). We deliberately designed the simulation to be applicable to any clinical risk factor.
To do this, we created a simulation of 1500 patients, with a spectrum of a notional risk factor from 0.01 to 15.00, which is linearly related to a patient annual mortality of 0.01–15% (no sharp step in mortality – only a smooth gradation). We simulated using Microsoft Excel survival over 10 years, yielding an ending survival status (alive/dead) and duration for each subject, as required for survival analysis. For example for the 314th patient, whose annual mortality was 3.14%, the survival state was initialized as “alive” and then on 10 occasions (one for each simulated year) he was subjected to 3.14% probability of dying. If the simulated states changed to “dead” in this way, year of death was noted. If he survived all 10 years, the outcome was deemed censored, i.e. “alive” at 10 years.
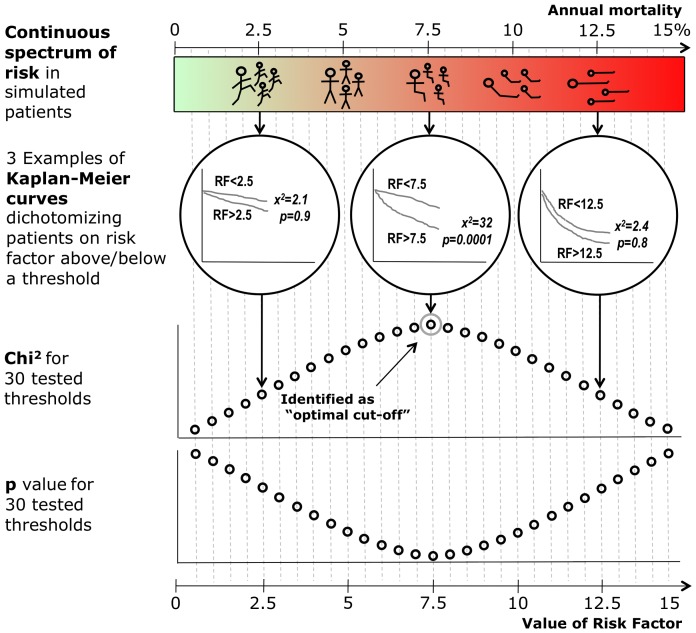
Identifying optimal prognostic threshold by Kaplan-Meier analysis
We then used Kaplan-Meier analysis to examine the prognostic power of a range of potential threshold values of the risk factor in Statview 5.0 (SAS Institute Inc., Cary, NC). In Figure 1 we show how this was done with three example Kaplan-Meier curves. One threshold is low (2.5), the second is at the median of the group (7.5), and the third is high (12.5). Although only 3 thresholds are shown for illustrative purposes in Figure 1, a wide range of cut-offs were actually tested. In the lower panels, the results of this full range of tested thresholds are shown. The threshold that gave the highest chi-squared value (equivalent to the smallest p value) was taken as the “optimal” threshold.
Figure 1. Simulated population characterized by gradually increasing risk and effectiveness of a series of potential prognostic thresholds by Kaplan-Meier and log-rank analysis.
In 1500 notional patients, with a wide spread of annual mortality (evenly distributed from 0.01 to 15.00%), we run survival simulation and use Kaplan-Meier and log-rank analysis to examine the prognostic power of many potential threshold values of the risk factor. For three examples amongst the many thresholds tested, the upper panels show the resulting Kaplan-Meier curves. In the lower panels, the results of the full range of tested thresholds are shown. The threshold that gave the highest chi-squared value (equivalent to the smallest p value) was taken as the “optimal” threshold.
Examining populations of different average risk
To test whether the optimal threshold identified by the procedure described above is a true phenomenon or simply an artefact that tracks the middle of the patients that are studied, we took a series of overlapping 500-patient sub-populations from different parts of the full 1500-patient spectrum and re-ran the analysis within each of these subsets. This mirrors clinical studies examining patient groups with different severities of the disease.
The first such subset covered the lowest risk part of the population spectrum, with the risk factor varying from 0 to 5 and annual mortality accordingly varying from 0 to 5%. The next subset had risk factor 2.5 to 7.5 (annual mortality 2.5 to 7.5%), and so on, until the risk range 10 to 15 (annual mortality 10 to 15%). For each of these subsets, we identified the optimum prognostic threshold of the risk factor by the methods described above.
Identifying optimal prognostic threshold by ROC analysis
Separately from the Kaplan-Meier method for identification of the optimal prognostic threshold, we also used ROC analysis to identify the optimal prognostic threshold. We repeated the comparison in each subpopulation with the various subranges of mortality risk as shown above.
Identifying optimal prognostic threshold in populations with a non-linear relationship between the variable tested and mortality
In order to extend the applicability of our simulation findings to other risk factors which might not have a simple linear relationship between their value and their associated mortality risk, we repeated the simulation of 1500 notional patients to study different shapes of relationship. We studied a wide range of possible shapes of relationship between risk factor and mortality, including:
A step (on a background of a linear slope)
A large step (on a background of a linear slope)
A step between two plateaus at different levels
A linear slope segment and then a plateau
A linear slope segment between two plateaus at different levels
A plateau segment between two linear slope segments
A continuously curved relationship (for example, exponential or sigmoidal)
For each possible shape of relationship we ran ten simulations and observed the distribution of apparently-optimal prognostic thresholds in relation to the shape of the relationship between risk factor and mortality.
Statistical Analysis
Statistical analysis was performed using Statview 5.0 (SAS Institute Inc., Cary, NC). Values are presented as mean±standard deviation (SD) for normally distributed continuous data, as median and interquartile range (IQR) for non-normally distributed continuous data and as percentages for categorical data. p<0.05 was considered statistically significant.
The differences between two groups were evaluated using the Mann-Whitney test and the uncorrected Chi2 test, with the highest Chi2 being taken as the most statistically significant. Spearman's rank correlation coefficient was used to express the relationship between the apparently-optimal threshold in a group, and the average level of risk factor in that group.
Survival analysis was by the Kaplan-Meier method with the log-rank test.
Apparently-optimal prognostic thresholds were also identified by testing a range of possible thresholds, forming in effect a Receiver-Operating Characteristic (ROC) curve, and then defining as apparently-optimal the threshold that maximised the sum of sensitivity and specificity. To simplify the analysis and minimize problematic right censoring, we designed our simulation to only censor at the end of follow-up.
Results
Peak VO2 thresholds in published data
Of the 287 studies identified, 113 were excluded because they either had zero or numerous thresholds, 20 because they did not report average peak VO2, 29 because they did not report survival, 33 because the setting was not heart failure, and 59 because they were clinical trials with no separate report within the control arm. Therefore 33 studies (8946 patients, Table 1, left hand plot) matched the selection criteria and underwent analysis. Of these, 18 found the threshold in peak VO2 [4]–[7], [23]–[35] to be prognostically significant, while 15 found it was not [11]–[13], [36]–[47] (Table 1).
Examining the published studies in cohorts of 5 years from the first published study in 1988, the proportion of studies reporting a statistically significant prognostic threshold for peak VO2 has declined from 100% (1986–1990) to 22% (2006–10, p = 0.03 for trend, Table 2).
Table 2. Apparent loss of prognostic power of Peak VO2 threshold over time and likelihood of different prognostic thresholds giving positive results.
| Number of studies testing a peak VO2 threshold and finding it to be prognostically significant | Number of studies testing a peak VO2 threshold and finding it to be not prognostically significant | |
| Publication year | ||
| 1986–1990 | 3 (100%) | 0 (0%) |
| 1991–1995 | 4 (80%) | 1 (20%) |
| 1996–2000 | 6 (75%) | 2 (25%) |
| 2001–2005 | 3 (38) | 5 (62%) |
| 2006–2010 | 2 (22%) | 7 (78%) |
| Threshold tested (ml/kg/min) | ||
| 9–10.9 | 2 (100%) | 0 (0%) |
| 11–12.9 | 1 (100%) | 0 (0%) |
| 13–14.9 | 11 (44%) | 14 (56%) |
| 15–16.9 | 2 (66%) | 1 (34%) |
| 17–18.9 | 2 (100%) | 0 (0%) |
The thresholds chosen for testing varied widely from 10 to 18 ml/kg/min. Studies testing thresholds in the range 13–14.9 and 15–16.9 ml/kg/min were less likely to report positive results (Table 2), and, in particular, studies testing a threshold of 14 ml/kg/min were the least likely to be prognostically significant when compared to all the other possible thresholds (44% versus 92%, p = 0.01).
Predictors of the peak VO2 threshold reported by published studies
The variation in optimal peak VO2 threshold in the positive studies was almost completely predictable from the individual studies' mean VO2 values (r = 0.86, p<0.00001, Figure 2, panel a). There was also a correlation of the threshold with left ventricular ejection fraction (r = 0.60, p = 0.011) and the individual study's mean ejection fraction.
Figure 2. Relationships between the threshold tested and the individual studies' mean: examples from peak VO2 (panel a), LVEF (panel b) and BNP (panel c).
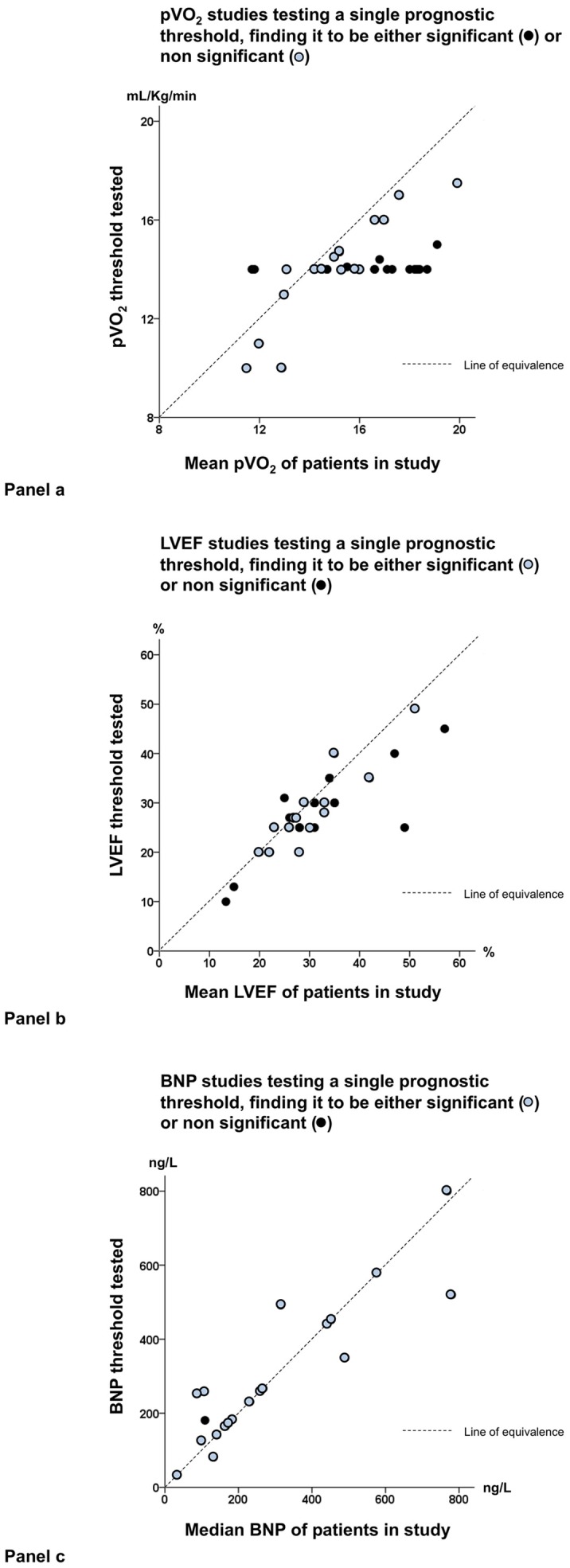
In the studies testing a threshold and finding it to be significant (open circles), the threshold reported may be either slightly higher than the mean of the study or slightly lower, but in all cases it is not far from the mean; in contrast it is often far from the mean in the studies testing a threshold and finding it to be non significant (black dots). Dotted lines in each panel represent the line of equivalence.
The threshold did not correlate with year of study (r = 0.30, p = 0.23), number of subjects (r = −0.17, p = 0.49), or mean age (r = 0.30, p = 0.23).
Why some studies appeared to not confirm a statistically significant prognostic threshold in peak VO2
In 15 studies, the peak VO2 threshold was found not to be prognostic: Table 3 shows the characteristics of the “positive” versus “negative” studies. The most obvious contender was study size, since larger studies (in the sense of more subjects enrolled, or more subjects with events) would have greater power to detect a threshold. However neither number of subjects, nor number of events, nor any of the main features of the studies or their populations was significantly different between groups.
Table 3. Comparison of the main features of studies testing a threshold and finding it to be significant or non significant.
| Studies testing a peak VO2 threshold and finding it to be prognostically significant | Studies testing a peak VO2 threshold and finding it to be not prognostically significant | |
| Sample size (n) | 210 (11–282) | 214 (98–353) |
| Mean age (years) | 56±6 | 57±8 |
| Males (%) | 83 | 77 |
| Left ventricular ejection fraction (%) | 23.9±4.6 | 29.8±6.3* |
| Number of events observed (n) | 37 (25–60) | 37 (27–79) |
| Follow-up duration (months) | 39 (24–63) | 54 (40–64) |
| Endpoint: cardiac versus all-cause mortality (n) | 6/12 | 8/7 |
| Absolute difference between mean peak VO2 | 1.2±0.8 | 3.5±2.4** |
| and threshold tested (ml/kg/min) |
p<0.01 **p<0.0001 versus studies testing a peak VO2 threshold and finding it to be prognostically significant.
Apart from a relatively small difference in ejection fraction (still in the range of severe systolic dysfunction), only one feature differed. The positive studies were all testing thresholds near the individual study means, whereas the negative studies were testing thresholds that were 3 times as far away from the individual study means: absolute difference between VO2 threshold tested and mean VO2 for the study was 1.2±0.9 ml/kg/min for the positive studies and 3.5±2.0 ml/kg/min for the negative studies, p = 0.0001.
Overall, only five studies also analyzed peak VO2 as a continuous variable, four positive studies [24], [25], [27], [30] and one negative study [37]. The negative study [37], was only negative when peak VO2 was dichotomized; it confirmed a significant relationship with outcome when peak VO2 was analysed as a continuous variable.
Published thresholds in ejection fraction
Of the 35 studies (out of 2296 studies) matching the inclusion criteria for EF (10220 patients), 22 found the threshold in EF to be prognostically significant [15], [16], [48]–[67], while 13 found it was not (Table 4) [14], [68]–[79].
Table 4. The 35 studies reporting a positive (white) or negative (grey) statistical significance of a prognostic threshold of ejection fraction.
| Author | Publication Year | Number of patients | Age (years) | Males (%) | Primary outcome | Max duration of follow-up (months) | Number of events | Mean±SD EF (%) | Tested threshold (%) | Tested threshold prognostically significant? |
| Itoh | 1992 | 298 | 63±11 | 57 | overall mortality | 40 | 167 | 35±nr | 40 | yes |
| Mehta | 1992 | 112 | 66±8 | 74 | cardiac mortality | 78 | 31 | 33±nr | 30 | yes |
| Rihal | 1994 | 102 | 61±14 | 63 | overall mortality | 36 | 35 | 23±8 | 25 | yes |
| Omland | 1995 | 145 | 61±10 | 80 | overall mortality | 44 | 36 | 51±10 | 49,1 | yes |
| Andreas | 1996 | 36 | 54±12 | 90 | overall mortality | 53 | 16 | 20±8 | 20 | yes |
| Giannuzzi | 1996 | 508 | 59±9 | 88 | overall mortality+hospitalization | 58 | 148 | 26±5 | 25 | yes |
| Szabo | 1997 | 159 | 61±nr | 85 | overall mortality | 69 | 30 | 26.6±9 | 27 | yes |
| Anker | 1997 | 171 | 60±11 | 90 | overall mortality | 18 | 49 | 30±15 | 25 | yes |
| Wijbenga | 1998 | 64 | 59±10 | 86 | overall mortality+transplantation | 30 | 64 | 31±8 | 30 | yes |
| Niebauer | 1999 | 99 | 58±2 | 90 | overall mortality | 36 | 73 | 13,3±nr | 10 | no |
| Metra | 1999 | 219 | 55±10 | 93 | overall mortality+urgent transplantation | 144 | 38 | 22±7 | 20 | yes |
| Isnard | 2000 | 264 | 51±12 | 80 | cardiac mortality+urgent transplantation | 206 | 83 | 27±10 | 27 | yes |
| Ghio | 2000 | 140 | 52±11 | 75 | cardiac mortality+urgent transplantation | 38 | 52 | 22±2 | 20 | yes |
| McDonagh | 2001 | 1640 | 50,4±nr | 48 | overall mortality | 48 | 80 | 47±nr | 40 | no |
| Neglia | 2002 | 64 | 52±12 | 87 | cardiac mortality | 82 | 24 | 34±10 | 35 | no |
| Corrà | 2002 | 600 | 58±7 | 88 | cardiac mortality+urgent transplantation | 102 | 87 | 26±4 | 25 | yes |
| Szachniewicz | 2003 | 176 | 63±nr | 86 | overall mortality | 18 | 32 | 42±nr | 35 | yes |
| Gardner | 2003 | 142 | 50±10 | 82 | cardiac mortality+urgent transplantation | 55 | 24 | 14.9±7 | 13 | no |
| Martinez-Selles | 2003 | 1065 | 75±nr | 49 | overall mortality | 51 | 507 | 35±7 | 30 | no |
| Shiba | 2004 | 684 | 67±13 | 66 | overall mortality | 33 | 175 | 49±15 | 25 | no |
| Guazzi | 2005 | 128 | 60±9 | 79 | cardiac mortality | 51 | 24 | 34±10 | 35 | yes |
| Kistorp | 2005 | 195 | 69±nr | 71 | overall mortality | 30 | 46 | 30±8 | 25 | yes |
| Junger | 2005 | 209 | 54±10 | 86 | overall mortality | 35 | 45 | 22±10 | 20 | yes |
| Peterson | 2005 | 61 | 53±11 | 86 | overall mortality+urgent transplantation | 139 | 32 | 26±9 | 27 | no |
| Bloomfield | 2006 | 549 | 56±10 | 71 | cardiac mortality | 24 | 51 | 25±6 | 31 | no |
| Rossi | 2007 | 273 | 62±nr | 87 | overall mortality | 45 | 44 | 31±3 | 30 | yes |
| Arslan | 2007 | 43 | 62±10 | 86 | overall mortality | 24 | 16 | 35±6 | 30 | yes |
| Guazzi | 2007 | 288 | 55±13 | 62 | overall mortality | 33 | 62 | 33±13 | 28 | yes |
| vonHaeling | 2007 | 525 | 61±12 | 94 | overall mortality | 28 | 171 | 28±4 | 20 | yes |
| Nishio | 2007 | 145 | 67±1.8 | 70 | cardiac mortality+hospitalization | 33 | 28 | 31±nr | 30 | no |
| Dini | 2007 | 356 | 70±6 | 22 | cardiac death | 34 | 54 | 31±3 | 25 | no |
| Whalley | 2008 | 228 | 70±3 | 66 | cardiac mortality+hospitalization | 18 | 26 | 57±12 | 45 | no |
| Dini | 2008 | 142 | 71±11 | 78 | overall mortality | 50 | 85 | 28±7 | 25 | no |
| Parissis | 2009 | 300 | 65±11 | 83 | cardiac mortality+hospitalization | 12 | 92 | 28±4 | 25 | no |
| Smilde | 2009 | 90 | 60±8 | 85 | overall mortality | 156 | 47 | 29±9 | 30 | yes |
EF = left ventricular ejection fraction; nr = not reported.
In the 22 studies where EF was found to be prognostically significant, the threshold varied widely from 20 to 49%, but was strongly associated with study sample means (r = 0.90, p<0.0001, Figure 2, panel b). In contrast, in the 13 studies where EF was found to be not prognostically significant, the tested threshold was relatively far (124% further than positive studies) from the individual study means: absolute difference between EF threshold tested and mean EF for the positive study averaged 2.5±2.3% for the positive studies and 5.8±6.5% for the negative studies, p<0.05). Examining the published studies in cohorts of 5 years from the first published study in 1992, again a progressive decline was observed in the percentage of studies reporting a threshold which was prognostically significant, from 100% (1991–1995) to 45% (2006–2010).
Published thresholds in Brain Natriuretic Peptide
Of 20 studies (out of 346 studies) matching the inclusion criteria for BNP (9725 patients), 19 studies found the threshold in BNP to be prognostically significant [17], [20], [80]–[95], and one study found it was not (Table 5) [96]. In the positive studies, the threshold widely varied from 132 to 800 ng/L, but was again strongly determined by the study median (r = 0.86, p<0.0001, Figure 2, panel c).
Table 5. The 20 studies reporting a positive (white) or negative (grey) statistical significance of a prognostic threshold of brain natriuretic peptide.
| Author | Publication Year | Number of patients | Age (years) | Males (%) | Primary outcome | Max duration of follow-up (months) | Number of events | Median (IQR) BNP (ng/L) | Tested threshold (ng/L) | Tested threshold prognostically significant? |
| Omland | 1996 | 131 | 68±1 | 75 | overall mortality | 48 | 31 | 33,1 (nr) | 33,3 | yes |
| Yu | 1999 | 91 | 61±nr | 70 | cardiac mortality | 12 | 25 | 165 (nr) | 165 | yes |
| Bettencourt | 2004 | 84 | 69±9 | 60 | overall mortality | nr | 17 | 260,4 (122,4–543,8) | 260,4 | yes |
| de Groote | 2004 | 150 | 55±13 | nr | cardiac mortality | 24 | 35 | 107 (3,5–876) | 260 | yes |
| Hulsmann | 2005 | 112 | 68±12 | 64 | overall mortality | 43 | nr | 231 (nr) | 231 | yes |
| Watanabe | 2005 | 417 | 64±14 | 69 | overall mortality+hospitalization | nr | 124 | 132 (nr) | 81 | yes |
| Lamblin | 2005 | 546 | 56±nr | 82 | cardiac mortality+urgent trasplantantion | 53 | 113 | 173 (nr) | 173 | yes |
| Bertinchant | 2005 | 63 | 54±7.2 | 89 | cardiac mortality+hospitalization | nr | 47 | 89,5 (11–1413) | 254 | yes |
| Horwich | 2006 | 316 | 53±13 | 74 | overall mortality | 48 | nr | 452 (nr) | 452 | yes |
| Masson | 2006 | 3916 | nr | nr | overall mortality | nr | 758 | 99 (nr) | 125 | yes |
| Sun | 2007 | 50 | 67±6 | 58 | cardiac mortality | 24 | 12 | 780 (nr) | 520 | yes |
| Frantz | 2007 | 206 | 60±nr | 80 | overall mortality+hospitalization | 12 | 81 | 141 (nr) | 141 | yes |
| Christ | 2007 | 123 | 63±12 | 85 | overall mortality+urgent trasplantantion | 36 | 28 | 183 (11–1672) | 183 | yes |
| Dhaliwal | 2009 | 464 | 67±7 | 99 | overall mortality+hospitalization | nr | 126 | 490 (233–796) | 350 | yes |
| Moertl | 2009 | 96 | 69±12 | 58 | overall mortality+hospitalization | 24 | 34 | 267 (nr) | 267 | yes |
| Niessner | 2009 | 351 | 75±nr | 66 | overall mortality+hospitalization | 16 | 175 | 441 (231–842) | 441 | yes |
| Cohen-Solal | 2009 | 1038 | 66±nr | 70 | overall mortality | 6 | nr | 768 (nr) | 800 | yes |
| El-Saed | 2009 | 173 | 67±11 | 98 | overall mortality | 24 | 31 | 315 (nr) | 492 | yes |
| Voors | 2009 | 224 | 68±10 | 70 | overall mortality+resuscitated arrest | 12 | 63 | 109 (nr) | 181 | no |
| Sachdeva | 2010 | 1215 | 53±13 | 75 | overall mortality+urgent trasplantantion | 24 | 442 | 575 (190–1300) | 579 | yes |
EF = left ventricular ejection fraction; nr = not reported.
Survival simulation study
Thresholds from Kaplan Meyer analysis
In these simulations, even with a purely smooth gradation of risk and definitely no step change, each 1500-patient population yielded its own apparent “optimal” prognostic threshold (Figure 3, Figure 4 panel a and Figure 5).
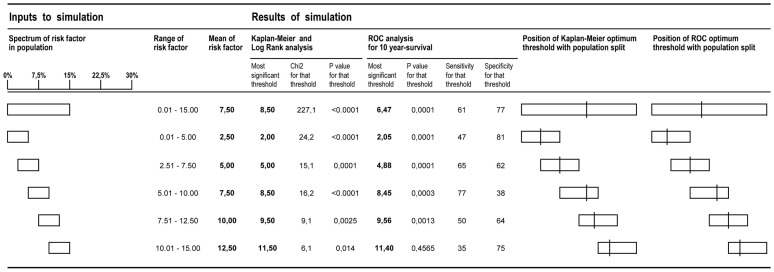
Figure 3. Mathematical simulation of sample selection from the general population: correlations between the sample mean and the apparently-optimal prognostic threshold.
Sub-populations with different ranges of risk simulating a shift in the mean peak VO2 were created and strong correlations between population mean and optimal thresholds by Kaplan-Meier and ROC analysis were found.
Figure 4. Apparently-optimal prognostic thresholds in twelve different types of relationship between the risk factor and mortality.
For each type of relationship, 10 simulations were conducted, and the 10 apparently-optimal thresholds derived from Kaplan Mayer analysis were found. They are shown by vertical arrows (where multiple arrows would have been superimposed, they have been placed one above another).
Figure 5. Apparent optimal prognostic threshold, by Kaplan-Meier and ROC method, arising from a mathematically simulated population with known, smooth gradation of risk.
The position of the apparently optimal threshold is almost completely determined by the risk factor mean. Several overlapping samples are taken from a single population of smoothly varying risk.
This apparent optimal threshold was always close to the mean of the population being studied, because in general thresholds tested far from the mean consistently had lower prognostic power. As we moved across the spectrum of risk examining different sub-populations of 500 patients with different average risks, drawn from the main population, we observed an almost exactly corresponding change in the optimal threshold as calculated by the Kaplan-Meier method (Figure 5). This was true for each sub-population tested (with samples characterized by an annual mortality of 0–5%, 2.5–7.5%, 5–10%, 7.5–12.5, 10–15%, Figure 5). We observed a strong correlation between the optimal threshold within a population and the mean risk factor within that sub-population (r = 0.99, p<0.001 Figure 3).
Thresholds from ROC analysis
The ROC analysis, like the Kaplan-Meier analysis, also found an apparently optimal prognostic threshold in each simulated population even though they definitely had only smoothly-varying risk. Again, this apparently-optimal threshold in the risk factor was found to shift to match the average risk factor level in the patient subset (r = 0.99, p<0.001, Figure 3, Figure 5).
Identifying optimal prognostic threshold in populations with a non linear relationship between the variable tested and mortality
When we employed a nonlinear relationship between risk factor and mortality, some subtleties emerged. If the risk factor was linearly predictive of mortality, then the apparent optimal prognostic threshold was found to be simply approximately the middle of the population (Figure 4, panel a). If there was a step increase in mortality on a background of an approximately linear gradation, the step was reliably identified as long as it was distinctly larger than the gradation (Figure 4, panels b and c). If the risk factor was simply a step relation with mortality, with no gradation above or below that step, then that step was found, even if small (Figure 4, panel d).
If there was a slope of risk and a plateau (as is likely with some real-life risk factors such as peak VO2, EF and BNP) the location of the apparently optimal threshold was more complex. In situations where most of the patients were on the plateau, then the optimal threshold lay at the junction between plateau and gradient. If, on the other hand, most of the patients were on the gradient, then the apparent optimal threshold lay about half-way along the gradient (Figure 4, panels e, f, g and h). These latter two observations were true regardless of whether it is a rising or falling gradient.
If the risk shape was, instead, a slope between two plateaus, the middle of the slope was the most favoured location for the apparently optimal threshold (Figure 4, panels i). If there was a plateau between two slopes, the optimal threshold tended to be near the end of (either) one of the slopes, where it meets the plateau (Figure 4, panel j). If there was a smooth curve of mortality (regardless of whether convex or concave) the apparent optimal threshold lay near the middle, but a little displaced toward the steeper side of the curve (Figure 4, panels k and l).
Discussion
In this study we have identified using the most commonly used prognostic measurements in heart failure, namely peak VO2, EF and BNP, that commonly-used methods of defining an apparently “optimal” prognostic threshold can be simply a manifestation of the middle of the risk factor spectrum of the individual population studied, and should never be taken to signify any meaningful step change in prognosis. Even in an artificial population known to consist of a completely smooth gradation of risk, such methods give an apparent prognostic threshold but its location reflects little more than the population average.
Does the finding of a clear optimal threshold with Kaplan-Meier analysis mean that there is really a step change in prognosis?
We deliberately simulated notional populations without step increase in risk but rather gradually increasing risk, and examined the effectiveness of a series of potential prognostic thresholds. The most significant difference between the Kaplan-Meier curves was found when the threshold was near the mean population risk. As the tested threshold was moved progressively further from the middle of the population in either direction, the Kaplan-Meier curves became less statistically significantly separated, so that dichotomising near the extremes of low or high values of risk cause the curves to be not statistically significantly different from each other.
The commonly-used methods produce an apparently-optimal prognostic dichotomy point effortlessly, but there is no real clinical phenomenon occurring at that point. Maximally-significant separation of the Kaplan-Meier curves need not represent a biological step change: it could easily be merely identifying the middle of that risk factor in that individual study, in a manner that is opaque, expensive and roundabout.
Does ROC analysis resolve the pitfalls of the Kaplan-Meier approach to finding a biological threshold?
ROC analysis has a reputation for making statistical analysis of diagnostic value more comprehensive. It has been used in some studies to identify an optimal threshold of peak VO2 [97]–[99].
However, our simulated populations show that ROC analysis is as susceptible as the Kaplan-Meier method, i.e. it tends to find the optimal threshold to be the middle of the population.
Neither Kaplan-Meier nor ROC methods can be relied upon to be illuminating a true biological threshold in prognosis. Each is heavily biased towards reporting the centre of the risk spectrum of that study. Indeed, the search for such dichotomies has been demonstrated to be a seriously underpowered way to look for prognostic relationships [100].
Lessons learnt from peak VO2, EF, and BNP studies
Paradoxically, while early studies were unanimous in confirming particular threshold values of peak VO2 to be prognostically important in heart failure [4]–[6], [23]–[25], more recent studies seemed to cast doubt on this, with only a quarter of studies between 2003–2010 confirming statistically significant prognostic cut-off values. Further, the widely recommended threshold of 14 ml/kg/min [8]–[10] was found to be the least likely be statistically significant.
The explanation for this appears to be that the significant, and in general older, studies tested several values and picked the most significant (or deliberately used the middle of their population), benefitting from the flexibility to choose their own threshold, close to their mean peak VO2. The studies that found no prognostic relationship, which tended to be more recent, chose to test the clinically established threshold of 14 ml/kg/min as their cut-off value, which happened to be relatively far away from their own population mean.
A similar pattern was seen with EF. The community is aware that for EF there is no special universal prognostic threshold and even clinical guidelines [101] recognise that a sharp change in prognosis at a threshold is unlikely.
BNP is a more recent entrant. 95% of studies found BNP to be prognostic, which may be a sign of its strong prognostic value, or the relative ease of conducting large studies, or the lack of a rigid predetermined threshold to test against. Even up to 2005, guidelines resisted the temptation to specify a prognostic threshold for BNP [102], and by 2008 when pressure for a diagnostic threshold became irresistible, this was kept 300% wide (100–400 pg/ml), perhaps subtly telegraphing the undesirability of a threshold out of context of clinical background information and individual risk-benefit evaluation [103].
Selecting “optimal” cut points without a strong reason to suspect a true biologic threshold is unwise [104]–[106]. It may better to assume a smooth graded relationship of a continuous variable with outcome. Moreover, excessive reverence for a statistically optimal single cut point and cementing of it in clinical guidelines, may impair that variable's prognostic power when compared with other variables proposed later. Taken to its extreme, setting cut points that are effectively the middle of the first positive study can lead to artificial discovery of new prognostic markers statistically independent of the old (because the old are handicapped).
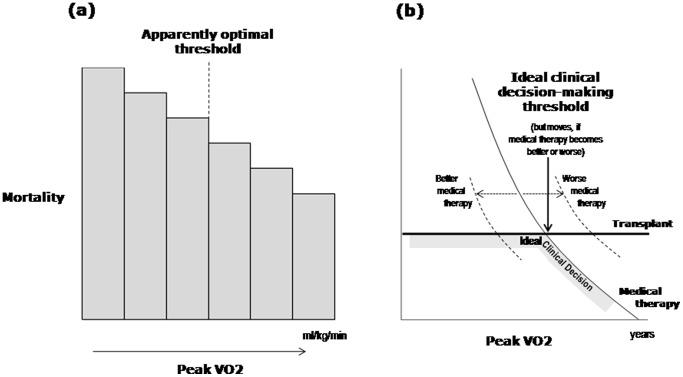
Two easily-confused but different types of “threshold”
It is important to distinguish between two different entities, each of which might reasonably be called a “threshold”. The first, discussed extensively in this study, is the value of a variable which most impressively separates a population into high-risk and low risk groups: an “observed prognostic threshold”. This study shows that such observed thresholds routinely arise even when the variable has a non-stepped, smoothly continuous relation to risk. A better term than “optimal risk threshold” would be “middle of the risk spectrum”, albeit less exciting.
The second type of threshold is the “clinical decision-making threshold” which is more subtle. Physicians need at times to decide whether to intervene: this is a dichotomy with no intermediate status. Correct decision-making depends on comparing the risk of intervening against the risk of not intervening, in the context of how the individual patient views such risks. Only in an imaginary disease with somehow just one important variable, and in which patients consistently value outcomes in the same way as a statistical model does, might a decisional threshold be applicable. Even still, this would be different from identifying a step change in prognosis, and certainly different from identifying the most statistically significant breakpoint (often simply the middle of the studied group).
That these two types of threshold differ is sketched in Figure 5, which imagines a situation where, with only medical therapy, mortality falls smoothly with rising peak VO2, while with transplantation mortality is at a fixed level. In this thought experiment, it is assumed that no other variables are relevant. Above a certain level of peak VO2, medical therapy is safer; below it, transplantation is safer. This is therefore the ideal clinical-decision-making threshold. But if improved medical therapy were developed, for example, this ideal decision-making threshold moves left. Exactly where this decision-making threshold lies cannot established by looking only at outcomes in non-transplanted (or transplanted) population alone. It can only be established by examining outcomes in both non-transplanted and transplanted populations. In real life, other variables are very important, and therefore the decision-making threshold cannot be established by comparing outcomes in patients who have been allocated by routine clinical methods to transplant or no transplant. A randomized controlled trial is the most secure basis, because this design gives the best chance of matching all variables, both those that can be observed and quantified and those that cannot.
Prognostic studies
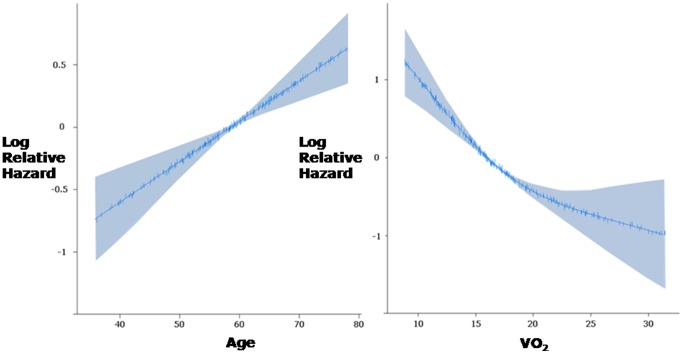
If it is desired to test for a prognostic threshold in a variable, there are straightforward statistical methods for doing so. For example, a flexible nonlinear function can be fitted and displayed with confidence bands for incremental log odds over the whole span of the marker; seeking a point such that risk is flat on both sides of that point but the risk on one side is much different from the risk on the other side (Figure 6). Such a phenomenon amongst cardiovascular prognostic studies is a rarity.
Figure 6. Two different types of threshold: apparently-optimal versus decision-making thresholds.
Cartoon illustrating two distinct, unrelated, values that are both called “threshold”. The statistically optimal threshold value of a continuous risk factor for subdividing the population (left panel) has no relevance to the question of what value of a risk factor should be used to decide whether to intervene or not (right panel). The former, the “observed prognostic threshold”, will generally be the middle of whatever population happens to be studied, if mortality varies roughly linearly with the risk factor. The latter, the “ideal clinical decision-making threshold”, will critically depend also on the outcomes with intervention, and will move as the success of the package of medical therapy (and of transplantation) changes with time. There is no sense in using one as a proxy for the other.
If for academic reasons there is a desire to seek a clinical decision-making threshold for a condition that has a single dominant prognostic marker, the reliable method is to conduct a randomized controlled trial which enrolls patients with values in the vicinity of the suspected threshold, and see where (with random allocation) the flexible nonlinear risk curves cross over (Figure 7). For all diseases evaluated by continuously distributed variables, the location of this crossover will always have a wide uncertainty (error bar) unless a very large number of events occur. Pooled analysis using multiple trial datasets has successfully used this approach to explore a decision-making threshold in QRS duration for implantation of biventricular pacing devices [107].
Figure 7. Example of use of flexible non-linear function to describe the relationships between age (left) and peak VO2 (right) and log odds of death using 208 patients.
The shaded areas represent the 95% confidence intervals for this function. Flexible non-linear functions have numerous benefits over categorization, including improved precision, avoidance of assumption of a discontinuous relationship, maximisation of applicability to the individual and importantly avoidance of giving other variables or interactions artificially high weights. Inspection of the resulting plots above can make obvious the lack of a discontinuity in risk.
Without elucidation of why we believe thresholds exist it might be difficult to advance our methods of deciding on advanced intervention (such as transplantation, or device implantation) beyond their current state. Continuous markers such as peak VO2, EF and BNP can be treated alongside other risk markers in multivariate fashion to finely grade prognosis. Clinging to or arguing over particular historically-documented threshold values may impede, rather than support, advances such as incorporating new information from potentially simple, cheap and effective supplemental prognostic markers [108]–[110]. Simple clinical variables such as age, sex and ECG QRS duration may capture as much or more prognostic power as more elaborately-obtained variables [108], [111]. Even strong markers when used in this dichotomous fashion may not live up to expectations [112]. Recognising and displaying [113] their continuous and progressive value may be preferable [114]. Cutpoints can synthesise apparent relationships when there are really none [115], and apparently-optimal diagnostic cutpoints can shift substantially with change in even a simple covariate such as cough [116].
Nor is it correct to assume that maximisation of diagnostic accuracy is a wise target, since this is only optimal if false positive and false negative categorisation are exactly equally undesirable. Cutpoints, especially when automatically constructed, impede our ability to understand the spectrum of risk, hide the existence of the intermediate zone, and encourage information destruction.
Clinical implications
Reporting an optimal prognostic threshold of a variable, without enumerating the actual shape of the risk profile, may be little more than an elaborate and time-consuming way of describing the middle of the population being studied. Conversely studies testing a pre-specified prognostic threshold, and finding no statistical significance, do not invalidate the prognostic meaning of the variable, especially if the average value in that study is far from the pre-specified threshold.
When making decisions about individual patients in the clinical setting we as physicians are often cautious about extrapolating from studies, acknowledging the differences between the population recruited (and the care delivered) in formally designed trials versus “real-life” practice. This same caution is rarely extended to the application of cutpoints to the individual patient, even though published cutpoints turn out to often be merely an indirect index of the middle of the sample described. We therefore risk treating patients simply according to whether, in the context of a previous study, they are above-average or below-average.
It might well be reasonable for a resource in short supply to be offered to simply the higher risk half of the population, but we should openly state that the threshold for therapy is merely the mid-point of the first adequately-powered prognostic study; it is not necessary to pretend that a threshold identified thus has any physiological universality or clinical permanence. This applies not only to heart failure but throughout clinical medicine, since many prognostic variables (e.g. blood pressure, cholesterol, prostate specific antigen) are continuous variables.
Clinician scientists wishing to ascribe special status to a threshold should perhaps be obligated to provide evidence of several criteria.
There must be a difference in outcome below versus above the threshold.
There should be almost flat risk profiles on both sides of the threshold.
Enough data should be accrued to test whether the threshold is a true point of discontinuity when risk is evaluated using a flexible function of the marker.
For commonly-used cardiological markers, the second and third will only rarely be confirmed.
Study limitations
This study does not prove the cause of the disagreement in optimal threshold in peak VO2 or EF or BNP between studies, or of the apparent loss of prognostic significance of this parameter over time. It only shows that the most statistically significant threshold has nothing to do with the optimal clinical decision-making threshold, nor is its existence evidence of any specialchange in risk at that point.
This study cannot establish the optimal clinical decision-making thresholds for therapy. If they exist, they can only be obtained reliably by randomized controlled trials.
Conclusions
Conflict between reported optimal prognostic thresholds in variables such as peak VO2, EF, BNP between studies result almost entirely from differences in average values of these variables between studies.
Clinical guideline writers should hesitate to specify a threshold in a variable for therapeutic decisions arising from such observational studies. Their readers might question how a committee can know what is best for an individual patient whom it has not met, knowing only whether one continuous variable is above or below an essentially meaningless threshold; this might weaken the credibility of the guideline as a whole.
Manuscript authors should not expend effort synthesising, and clinicians should not spend time reading, unnecessarily elaborate explanations for apparent movement of thresholds between studies, since the widely-used procedures generate for almost any continuous risk factor an artifactual apparently-optimal threshold near the middle of any patient group examined. We should study prognosis without these misapprehensions.
Supporting Information
PRISMA checklist.
(DOC)
Funding Statement
RB (PG/07/065) and DPF (FS/10/038) were supported by the British Heart Foundation. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Mancini DM, Eisen H, Kussmaul W, Mull R, Edmunds LH Jr, et al. (1991) Value of peak exercise oxygen consumption for optimal timing of cardiac transplantation in ambulatory patients with heart failure. Circulation 83: 778–86. [DOI] [PubMed] [Google Scholar]
- 2. Mudge GH, Goldstein S, Addonizio LJ, Caplan A, Mancini D, et al. (1993) 24th Bethesda Conference: Cardiac transplantation. Task Force 3: Recipient guidelines/prioritization. J Am Coll Cardiol 22: 21–31. [DOI] [PubMed] [Google Scholar]
- 3. Banner NR, Bonser RS, Clark AL, Cowburn PJ, Gardner RS, et al. (2011) UK guidelines for referral and assessment of adults for heart transplantation. Heart 97: 1520–1527. [DOI] [PubMed] [Google Scholar]
- 4. Szlachcic J, Massie BM, Kramer BL, Topic N, Tubau J (1985) Correlates and prognostic implication of exercise capacity in chronic congestive heart failure. Am J Cardiol 55: 1037–42. [DOI] [PubMed] [Google Scholar]
- 5. Likoff MJ, Chandler SL, Kay HR (1987) Clinical determinants of mortality in chronic congestive heart failure secondary to idiopathic dilated or to ischemic cardiomyopathy. Am J Cardiol 59: 634–81. [DOI] [PubMed] [Google Scholar]
- 6. Van den Broek SA, van Veldhuisen DJ, de Graeff PA, Landsman ML, Hillege H, et al. (1992) Comparison between New York Heart Association classification and peak oxygen consumption in the assessment of functional status and prognosis in patients with mild to moderate chronic congestive heart failure secondary to either ischemic or idiopathic dilated cardiomyopathy. Am J Cardiol 70: 359–63. [DOI] [PubMed] [Google Scholar]
- 7. Clark AL, Coats AJ (2000) Exercise endpoints in patients with chronic heart failure. Int J Cardiol. 73: 61–6. [DOI] [PubMed] [Google Scholar]
- 8. Guidelines for the diagnosis and treatment of chronic heart failure: executive summary (update 2005): The Task Force for the Diagnosis and Treatment of Chronic Heart Failure of the European Society of Cardiology (2005) Eur Heart J. 26: 1115 40. [DOI] [PubMed] [Google Scholar]
- 9. ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (2005) Circulation. 112: e154–235. [DOI] [PubMed] [Google Scholar]
- 10. Listing criteria for heart transplantation: International Society for Heart and Lung Transplantation guidelines for the care of cardiac transplant candidates-2006 (2006) J Heart Lung Transplant. 25: 1024–42. [DOI] [PubMed] [Google Scholar]
- 11. Di Salvo TG, Mathier M, Semigran MJ, Dec GW (1995) Preserved right ventricular ejection fraction predicts exercise capacity and survival in advanced heart failure. J Am Coll Cardiol 25: 1143–53. [DOI] [PubMed] [Google Scholar]
- 12. Isnard R, Pousset F, Trochu J, Chafirovskaïa O, Carayon A, et al. (2000) Prognostic value of neurohormonal activation and cardiopulmonary exercise testing in patients with chronic heart failure. Am J Cardiol 86: 417–21. [DOI] [PubMed] [Google Scholar]
- 13. Rostagno C, Olivo G, Comeglio M, Boddi V, Banchelli M, et al. (2003) Prognostic value of 6-minute walk corridor test in patients with mild to moderate heart failure: comparison with other methods of functional evaluation. Eur J Heart Fail 5: 247–52. [DOI] [PubMed] [Google Scholar]
- 14. Niebauer J, Clark AL, Anker SD, Coats AJ (1999) Three year mortality in heart failure patients with very low left ventricular ejection fractions. Int J Cardiol 70: 245–7. [DOI] [PubMed] [Google Scholar]
- 15. Mehta D, Saksena S, Krol RB (1992) Survival of implantable cardioverter-defibrillator recipients: role of left ventricular function and its relationship to device use. Am Heart J 124: 1608–14. [DOI] [PubMed] [Google Scholar]
- 16. Omland T, Bonarjee VV, Lie RT, Caidahl K (1995) Neurohumoral measurements as indicators of long-term prognosis after acute myocardial infarction. Am J Cardiol 76: 230–5. [DOI] [PubMed] [Google Scholar]
- 17. Masson S, Latini R, Anand IS, Vago T, Angelici L, et al. (2006) Direct comparison of B-type natriuretic peptide (BNP) and amino-terminal proBNP in a large population of patients with chronic and symptomatic heart failure: the Valsartan Heart Failure (Val-HeFT) data. Clin Chem 52: 1528–38. [DOI] [PubMed] [Google Scholar]
- 18. Bertinchant JP, Combes N, Polge A, Fabbro-Peray P, Raczka F, et al. (2005) Prognostic value of cardiac troponin T in patients with both acute and chronic stable congestive heart failure: comparison with atrial natriuretic peptide, brain natriuretic peptide and plasma norepinephrine. Clin Chim Acta 352: 143–53. [DOI] [PubMed] [Google Scholar]
- 19. Sun T, Wang L, Zhang Y (2007) Prognostic value of B-type natriuretic peptide in patients with chronic and advanced heart failure. Intern Med J 37: 168–71. [DOI] [PubMed] [Google Scholar]
- 20. Cohen-Solal A, Logeart D, Huang B, Cai D, Nieminen MS, et al. (2009) Lowered B-type natriuretic peptide in response to levosimendan or dobutamine treatment is associated with improved survival in patients with severe acutely decompensated heart failure. J Am Coll Cardiol 53: 2343–8. [DOI] [PubMed] [Google Scholar]
- 21. Peterson LR, Schechtman KB, Ewald GA, Geltman EM, de las Fuentes L, et al. (2003) Timing of cardiac transplantation in patients with heart failure receiving beta-adrenergic blockers. J Heart Lung Transplant 22: 1141–8. [DOI] [PubMed] [Google Scholar]
- 22. Francis DP, Shamim W, Davies LC, Piepoli MF, Ponikowski P, et al. (2000) Cardiopulmonary exercise testing for prognosis in chronic heart failure: continuous and independent prognostic value from VE/VCO(2)slope and peak VO(2). Eur Heart J 21: 154–61. [DOI] [PubMed] [Google Scholar]
- 23. Cohn JN, Archibald DG, Ziesche S, Franciosa JA, Harston WE, et al. (1986) Effect of vasodilator therapy on mortality in chronic congestive heart failure. Results of a Veterans Administration Cooperative Study. N Engl J Med 314: 1547–52. [DOI] [PubMed] [Google Scholar]
- 24. Parameshwar J, Keegan J, Sparrow J, Sutton GC, Poole-Wilson PA (1992) Predictors of prognosis in severe chronic heart failure. Am Heart J 123: 421–6. [DOI] [PubMed] [Google Scholar]
- 25. Saxon LA, Stevenson WG, Middlekauff HR, Fonarow G, Woo M, et al. (1993) Predicting death from progressive heart failure secondary to ischemic or idiopathic dilated cardiomyopathy. Am J Cardiol 72: 62–5. [DOI] [PubMed] [Google Scholar]
- 26. Chomsky DB, Lang CC, Rayos GH, Shyr Y, Yeoh TK, et al. (1996) Hemodynamic exercise testing. A valuable tool in the selection of cardiac transplantation candidates. Circulation 94: 3176–3. [DOI] [PubMed] [Google Scholar]
- 27. Cohen-Solal A, Barnier P, Pessione F, Seknadji P, Logeart D, et al. (1997) Comparison of the long-term prognostic value of peak exercise oxygen pulse and peak oxygen uptake in patients with chronic heart failure. Heart 78: 572–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Metra M, Faggiano P, D'Aloia A, Nodari S, Gualeni A, et al. (1999) Use of cardiopulmonary exercise testing with hemodynamic monitoring in the prognostic assessment of ambulatory patients with chronic heart failure. J Am Coll Cardiol 33: 943–50. [DOI] [PubMed] [Google Scholar]
- 29. Osman AF, Mehra MR, Lavie CJ, Nunez E, Milani RV (2000) The incremental prognostic importance of body fat adjusted peak oxygen consumption in chronic heart failure. J Am Coll Cardiol 36: 2126–31. [DOI] [PubMed] [Google Scholar]
- 30. Davies LC, Francis DP, Piepoli M, Scott AC, Ponikowski P, et al. (2000) Chronic heart failure in the elderly: value of cardiopulmonary exercise testing in risk stratification. Heart 83: 147–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hansen A, Haass M, Zugck C, Krueger C, Unnebrink K, et al. (2001) Prognostic value of Doppler echocardiographic mitral inflow patterns: implications for risk stratification in patients with chronic congestive heart failure. J Am Coll Cardiol 37: 1049–55. [DOI] [PubMed] [Google Scholar]
- 32. Gitt AK, Wasserman K, Kilkowski C, Kleemann T, Kilkowski A, et al. (2002) Exercise anaerobic threshold and ventilatory efficiency identify heart failure patients for high risk of early death. Circulation 106: 3079–84. [DOI] [PubMed] [Google Scholar]
- 33. O'Neill JO, Young JB, Pothier CE, Lauer MS (2005) Peak oxygen consumption as a predictor of death in patients with heart failure receiving beta-blockers. Circulation 111: 2313–8. [DOI] [PubMed] [Google Scholar]
- 34. Rossi A, Cicoira M, Bonapace S, Golia G, Zanolla L, et al. (2007) Left atrial volume provides independent and incremental information compared with exercise tolerance parameters in patients with heart failure and left ventricular systolic dysfunction. Heart 93: 1420–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Sachdeva A, Horwich TB, Fonarow GC (2010) Comparison of usefulness of each of five predictors of mortality and urgent transplantation in patients with advanced heart failure. Am J Cardiol 106: 830–5. [DOI] [PubMed] [Google Scholar]
- 36. Robbins M, Francis G, Pashkow FJ, Snader CE, Hoercher K, et al. (1999) Ventilatory and heart rate responses to exercise : better predictors of heart failure mortality than peak oxygen consumption. Circulation 100: 2411–7. [DOI] [PubMed] [Google Scholar]
- 37. Williams SG, Cooke GA, Wright DJ, Snader CE, Hoercher K, et al. (2001) Peak exercise cardiac power output; a direct indicator of cardiac function strongly predictive of prognosis in chronic heart failure. Eur Heart J 2001 22: 1496–503. [DOI] [PubMed] [Google Scholar]
- 38. Ponikowski P, Chua TP, Anker SD, Francis DP, Doehner W, et al. (2001) Peripheral chemoreceptor hypersensitivity: an ominous sign in patients with chronic heart failure. Circulation 104: 544–9. [DOI] [PubMed] [Google Scholar]
- 39. Mejhert M, Linder-Klingsell E, Edner M, Kahan T, Persson H (2002) Ventilatory variables are strong prognostic markers in elderly patients with heart failure. Heart 88: 239–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Schalcher C, Rickli H, Brehm M, Weilenmann D, Oechslin E, et al. (2003) Prolonged oxygen uptake kinetics during low-intensity exercise are related to poor prognosis in patients with mild-to-moderate congestive heart failure. Chest 124: 580–6. [DOI] [PubMed] [Google Scholar]
- 41. Nanas SN, Nanas JN, Sakellariou DC, Dimopoulos SK, Drakos SG, et al. (2006) VE/VCO2 slope is associated with abnormal resting haemodynamics and is a predictor of long-term survival in chronic heart failure. Eur J Heart Fail 8: 420–7. [DOI] [PubMed] [Google Scholar]
- 42. Bard RL, Gillespie BW, Clarke NS, Egan TG, Nicklas JM (2006) Determining the best ventilatory efficiency measure to predict mortality in patients with heart failure. J Heart Lung Transplant 25: 589–95. [DOI] [PubMed] [Google Scholar]
- 43. Guazzi M, Raimondo R, Vicenzi M, Arena R, Proserpio C, et al. (2007) Exercise oscillatory ventilation may predict sudden cardiac death in heart failure patients. J Am Coll Cardiol 50: 299–308. [DOI] [PubMed] [Google Scholar]
- 44. Guazzi M, Arena R, Ascione A, Piepoli M, Guazzi MD (2007) Exercise oscillatory breathing and increased ventilation to carbon dioxide production slope in heart failure: an unfavorable combination with high prognostic value. Am Heart J 153: 859–67. [DOI] [PubMed] [Google Scholar]
- 45. Arena R, Myers J, Abella J, Pinkstaff S, Brubaker P, et al. (2008) The partial pressure of resting end-tidal carbon dioxide predicts major cardiac events in patients with systolic heart failure. Am Heart J 156: 982–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Arena R, Myers J, Abella J, Peberdy MA, Bensimhon D, et al. (2010) The prognostic value of the heart rate response during exercise and recovery in patients with heart failure: influence of beta-blockade. Int J Cardiol 138: 166–73. [DOI] [PubMed] [Google Scholar]
- 47. Izawa KP, Watanabe S, Osada N, Kasahara Y, Yokoyama H, et al. (2009) Handgrip strength as a predictor of prognosis in Japanese patients with congestive heart failure. Eur J Cardiovasc Prev Rehabil 16: 21–7. [DOI] [PubMed] [Google Scholar]
- 48. Itoh A, Saito M, Haze K, Hiramori K, Kasagi F (1992) Prognosis of patients with congestive heart failure: its determinants in various heart diseases in Japan. Intern Med 31: 304–9. [DOI] [PubMed] [Google Scholar]
- 49. Rihal CS, Nishimura RA, Hatle LK, Bailey KR, Tajik AJ (1994) Systolic and diastolic dysfunction in patients with clinical diagnosis of dilated cardiomyopathy. Relation to symptoms and prognosis. Circulation 90: 2772–9. [DOI] [PubMed] [Google Scholar]
- 50. Andreas S, Hagenah G, Moller C, Werner GS, Kreuzer H (1996) Cheyne-Stokes respiration and prognosis in congestive heart failure. Am J Cardiol 78: 1260–4. [DOI] [PubMed] [Google Scholar]
- 51. Giannuzzi P, Temporelli PL, Bosimini E, Silva P, Imparato A, et al. (1996) Independent and incremental prognostic value of Doppler-derived mitral deceleration time of early filling in both symptomatic and asymptomatic patients with left ventricular dysfunction. J Am Coll Cardiol 28: 383–90. [DOI] [PubMed] [Google Scholar]
- 52. Szabó BM, van Veldhuisen DJ, van der Veer N, Brouwer J, De Graeff PA, et al. (1997) Prognostic value of heart rate variability in chronic congestive heart failure secondary to idiopathic or ischemic dilated cardiomyopathy. Am J Cardiol 79: 978–80. [DOI] [PubMed] [Google Scholar]
- 53. Anker SD, Ponikowski P, Varney S, Chua TP, Clark AL, et al. (1997) Wasting as independent risk factor for mortality in chronic heart failure. Lancet 349: 1050–3. [DOI] [PubMed] [Google Scholar]
- 54. Wijbenga JA, Balk AH, Meij SH, Simoons ML, Malik M (1998) Heart rate variability index in congestive heart failure: relation to clinical variables and prognosis. Eur Heart J 19: 1719–24. [DOI] [PubMed] [Google Scholar]
- 55. Metra M, Faggiano P, D'Aloia A, Nodari S, Gualeni A, et al. (1999) Use of cardiopulmonary exercise testing with hemodynamic monitoring in the prognostic assessment of ambulatory patients with chronic heart failure. J Am Coll Cardiol 33: 943–50. [DOI] [PubMed] [Google Scholar]
- 56. Isnard R, Pousset F, Trochu J, Chafirovskaïa O, Carayon A, et al. (2000) Prognostic value of neurohormonal activation and cardiopulmonary exercise testing in patients with chronic heart failure. Am J Cardiol 86: 417–21. [DOI] [PubMed] [Google Scholar]
- 57. Ghio S, Recusani F, Klersy C, Sebastiani R, Laudisa ML, et al. (2000) Prognostic usefulness of the tricuspid annular plane systolic excursion in patients with congestive heart failure secondary to idiopathic or ischemic dilated cardiomyopathy. Am J Cardiol 85: 837–42. [DOI] [PubMed] [Google Scholar]
- 58. Corrà U, Mezzani A, Bosimini E, Scapellato F, Imparato A, et al. (2002) Ventilatory response to exercise improves risk stratification in patients with chronic heart failure and intermediate functional capacity. Am Heart J 143: 418–26. [DOI] [PubMed] [Google Scholar]
- 59. Szachniewicz J, Petruk-Kowalczyk J, Majda J, Majda J, Kaczmarek A, et al. (2003) Anaemia is an independent predictor of poor outcome in patients with chronic heart failure. Int J Cardiol 90: 303–8. [DOI] [PubMed] [Google Scholar]
- 60. Guazzi M, Reina G, Tumminello G, Guazzi MD (2005) Exercise ventilation inefficiency and cardiovascular mortality in heart failure: the critical independent prognostic value of the arterial CO2 partial pressure. Eur Heart J 26: 472–80. [DOI] [PubMed] [Google Scholar]
- 61. Kistorp C, Faber J, Galatius S, Gustafsson F, Frystyk J, et al. (2005) Plasma adiponectin, body mass index, and mortality in patients with chronic heart failure. Circulation 112: 1756–62. [DOI] [PubMed] [Google Scholar]
- 62. Jünger J, Schellberg D, Müller-Tasch T, Raupp G, Zugck C, et al. (2005) Depression increasingly predicts mortality in the course of congestive heart failure. Eur J Heart Fail 7: 261–7. [DOI] [PubMed] [Google Scholar]
- 63. Rossi A, Cicoira M, Bonapace S, Golia G, Zanolla L, et al. (2007) Left atrial volume provides independent and incremental information compared with exercise tolerance parameters in patients with heart failure and left ventricular systolic dysfunction. Heart 93: 1420–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Arslan S, Erol MK, Gundogdu F, Sevimli S, Aksakal E, et al. (2007) Prognostic value of 6-minute walk test in stable outpatients with heart failure. Tex Heart Inst J 34: 166–9. [PMC free article] [PubMed] [Google Scholar]
- 65. Guazzi M, Arena R, Ascione A, Piepoli M, Guazzi MD (2007) Exercise oscillatory breathing and increased ventilation to carbon dioxide production slope in heart failure: an unfavorable combination with high prognostic value. Am Heart J 153: 859–67. [DOI] [PubMed] [Google Scholar]
- 66. von Haehling S, Jankowska EA, Morgenthaler NG, Vassanelli C, Zanolla L, et al. (2007) Comparison of midregional pro-atrial natriuretic peptide with N-terminal pro-B-type natriuretic peptide in predicting survival in patients with chronic heart failure. J Am Coll Cardiol 50: 1973–80. [DOI] [PubMed] [Google Scholar]
- 67. Smilde TD, van Veldhuisen DJ, van den Berg MP (2009) Prognostic value of heart rate variability and ventricular arrhythmias during 13-year follow-up in patients with mild to moderate heart failure. Clin Res Cardiol 98: 233–9. [DOI] [PubMed] [Google Scholar]
- 68. McDonagh TA, Cunningham AD, Morrison CE, McMurray JJ, Ford I, et al. (2001) Left ventricular dysfunction, natriuretic peptides, and mortality in an urban population. Heart 86: 21–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Neglia D, Michelassi C, Trivieri MG, Sambuceti G, Giorgetti A, et al. (2002) Prognostic role of myocardial blood flow impairment in idiopathic left ventricular dysfunction. Circulation 105: 186–93. [DOI] [PubMed] [Google Scholar]
- 70. Gardner RS, Ozalp F, Murday AJ, Robb SD, McDonagh TA (2003) N-terminal pro-brain natriuretic peptide. A new gold standard in predicting mortality in patients with advanced heart failure. Eur Heart J 24: 1735–43. [DOI] [PubMed] [Google Scholar]
- 71. Martínez-Sellés M, García Robles JA, Prieto L, Domínguez Muñoa M, Frades E, et al. (2003) Systolic dysfunction is a predictor of long term mortality in men but not in women with heart failure. Eur Heart J 24: 2046–53. [DOI] [PubMed] [Google Scholar]
- 72. Shiba N, Nochioka K, Miura M, Kohno H, Shimokawa H (2011) Trend of westernization of etiology and clinical characteristics of heart failure patients in Japan-first report from the CHART-2 study. Circ J 75: 823–33. [DOI] [PubMed] [Google Scholar]
- 73. Petersson M, Friberg P, Eisenhofer G, Lambert G, Rundqvist B (2005) Long-term outcome in relation to renal sympathetic activity in patients with chronic heart failure. Eur Heart J 26: 906–13. [DOI] [PubMed] [Google Scholar]
- 74. Bloomfield DM, Bigger JT, Steinman RC, Namerow PB, Parides MK, et al. (2006) Microvolt T-wave alternans and the risk of death or sustained ventricular arrhythmias in patients with left ventricular dysfunction. J Am Coll Cardiol 47: 456–63. [DOI] [PubMed] [Google Scholar]
- 75. Nishio Y, Sato Y, Taniguchi R, Shizuta S, Doi T, et al. (2007) Cardiac troponin T vs other biochemical markers in patients with congestive heart failure. Circ J 71: 631–5. [DOI] [PubMed] [Google Scholar]
- 76. Dini FL, Conti U, Fontanive P, Andreini D, Banti S, et al. (2007) Right ventricular dysfunction is a major predictor of outcome in patients with moderate to severe mitral regurgitation and left ventricular dysfunction. Am Heart J 154: 172–9. [DOI] [PubMed] [Google Scholar]
- 77. Whalley GA, Wright SP, Pearl A, Gamble GD, Walsh HJ, et al. (2008) Prognostic role of echocardiography and brain natriuretic peptide in symptomatic breathless patients in the community. Eur Heart J 29: 509–16. [DOI] [PubMed] [Google Scholar]
- 78. Dini FL, Fontanive P, Panicucci E, Andreini D, Chella P, et al. (2008) Prognostic significance of tricuspid annular motion and plasma NT-proBNP in patients with heart failure and moderate-to-severe functional mitral regurgitation. Eur J Heart Fail. 10: 573–80. [DOI] [PubMed] [Google Scholar]
- 79. Parissis JT, Farmakis D, Nikolaou M, Birmpa D, Bistola V, et al. (2009) Plasma B-type natriuretic peptide and anti-inflammatory cytokine interleukin-10 levels predict adverse clinical outcome in chronic heart failure patients with depressive symptoms: a 1-year follow-up study. Eur J Heart Fail 11: 967–72. [DOI] [PubMed] [Google Scholar]
- 80. Omland T, Aakvaag A, Bonarjee VV, Caidahl K, Lie RT, et al. (1996) Plasma brain natriuretic peptide as an indicator of left ventricular systolic function and long-term survival after acute myocardial infarction. Comparison with plasma atrial natriuretic peptide and N-terminal proatrial natriuretic peptide. Circulation 93: 1963–9. [DOI] [PubMed] [Google Scholar]
- 81. Yu CM, Sanderson JE (1999) Plasma brain natriuretic peptide: an independent predictor of cardiovascular mortality in acute heart failure. Eur J Heart Fail 1: 59–65. [DOI] [PubMed] [Google Scholar]
- 82. Bettencourt P, Friões F, Azevedo A, Dias P, Pimenta J, et al. (2004) Prognostic information provided by serial measurements of brain natriuretic peptide in heart failure. Int J Cardiol 93: 45–8. [DOI] [PubMed] [Google Scholar]
- 83. de Groote P, Soudan B, Lamblin N, Rouaix-Emery N, Mc Fadden E, et al. (2004) Is hormonal activation during exercise useful for risk stratification in patients with moderate congestive heart failure? Am Heart J 148: 349–55. [DOI] [PubMed] [Google Scholar]
- 84. Hülsmann M, Berger R, Mörtl D, Gore O, Meyer B, et al. (2005) Incidence of normal values of natriuretic peptides in patients with chronic heart failure and impact on survival: a direct comparison of N-terminal atrial natriuretic peptide, N-terminal brain natriuretic peptide and brain natriuretic peptide. Eur J Heart Fail 7: 552–6. [DOI] [PubMed] [Google Scholar]
- 85. Watanabe J, Shiba N, Shinozaki T, Koseki Y, Karibe A, et al. (2005) Prognostic value of plasma brain natriuretic peptide combined with left ventricular dimensions in predicting sudden death of patients with chronic heart failure. J Card Fail 11: 50–5. [DOI] [PubMed] [Google Scholar]
- 86. Lamblin N, Mouquet F, Hennache B, Dagorn J, Susen S, et al. (2005) High-sensitivity C-reactive protein: potential adjunct for risk stratification in patients with stable congestive heart failure. Eur Heart J 26: 2245–50. [DOI] [PubMed] [Google Scholar]
- 87. Bertinchant JP, Combes N, Polge A, Fabbro-Peray P, Raczka F, et al. (2005) Prognostic value of cardiac troponin T in patients with both acute and chronic stable congestive heart failure: comparison with atrial natriuretic peptide, brain natriuretic peptide and plasma norepinephrine. Clin Chim Acta 352: 143–53. [DOI] [PubMed] [Google Scholar]
- 88. Horwich TB, Hamilton MA, Fonarow GC (2006) B-type natriuretic peptide levels in obese patients with advanced heart failure. J Am Coll Cardiol 47: 85–90. [DOI] [PubMed] [Google Scholar]
- 89. Frantz RP, Lowes BD, Grayburn PA, White M, Krause-Steinrauf H, et al. (2007) Baseline and serial neurohormones in patients with congestive heart failure treated with and without bucindolol: results of the neurohumoral substudy of the Beta-Blocker Evaluation of Survival Study (BEST). J Card Fail. 13: 437–44. [DOI] [PubMed] [Google Scholar]
- 90. Christ M, Thuerlimann A, Laule K, Klima T, Hochholzer W, et al. (2007) Long-term prognostic value of B-type natriuretic peptide in cardiac and non-cardiac causes of acute dyspnoea. Eur J Clin Invest 37: 834–41. [DOI] [PubMed] [Google Scholar]
- 91. Dhaliwal AS, Deswal A, Pritchett A, Aguilar D, Kar B, et al. (2009) Reduction in BNP levels with treatment of decompensated heart failure and future clinical events. J Card Fail 15: 293–9. [DOI] [PubMed] [Google Scholar]
- 92. Moertl D, Berger R, Hammer A, Huelsmann M, Hutuleac R, et al. (2009) B-type natriuretic peptide predicts benefit from a home-based nurse care in chronic heart failure. J Card Fail 15: 233–40. [DOI] [PubMed] [Google Scholar]
- 93. Niessner A, Hohensinner PJ, Rychli K, Neuhold S, Zorn G, et al. (2009) Prognostic value of apoptosis markers in advanced heart failure patients. Eur Heart J 30: 789–96. [DOI] [PubMed] [Google Scholar]
- 94. El-Saed A, Voigt A, Shalaby A (2009) Usefulness of brain natriuretic peptide level at implant in predicting mortality in patients with advanced but stable heart failure receiving cardiac resynchronization therapy. Clin Cardiol 32: E33–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Sachdeva A, Horwich TB, Fonarow GC (2010) Comparison of usefulness of each of five predictors of mortality and urgent transplantation in patients with advanced heart failure. Am J Cardiol 106: 830–5. [DOI] [PubMed] [Google Scholar]
- 96. Voors AA, von Haehling S, Anker SD, Hillege HL, Struck J, et al. (2009) C-terminal provasopressin (copeptin) is a strong prognostic marker in patients with heart failure after an acute myocardial infarction: results from the OPTIMAAL study. Eur Heart J 30: 1187–94. [DOI] [PubMed] [Google Scholar]
- 97. Roul G, Moulichon ME, Bareiss P, Gries P, Koegler A, et al. (1995) Prognostic factors of chronic heart failure in NYHA class II or III: value of invasive exercise haemodynamic data. Eur Heart J 16: 1387–98. [DOI] [PubMed] [Google Scholar]
- 98. Rossi A, Cicoira M, Bonapace S, Golia G, Zanolla L, et al. (2007) Left atrial volume provides independent and incremental information compared with exercise tolerance parameters in patients with heart failure and left ventricular systolic dysfunction. Heart 93: 1420–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Arena R, Myers J, Aslam SS, Varughese EB, Peberdy MA (2006) Impact of time past exercise testing on prognostic variables in heart failure. Int J Cardiol 106: 88–94. [DOI] [PubMed] [Google Scholar]
- 100. Royston P, Altman DG, Sauerbrei W (2006) Dichotomizing continuous predictors in multiple regression: a bad idea. Stat Med 25: 127–41. [DOI] [PubMed] [Google Scholar]
- 101. Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, et al. (2005) Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 18: 1440–63. [DOI] [PubMed] [Google Scholar]
- 102. Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, et al. (2005) ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure): developed in collaboration with the American College of Chest Physicians and the International Society for Heart and Lung Transplantation: endorsed by the Heart Rhythm Society. Circulation 112: e154–235. [DOI] [PubMed] [Google Scholar]
- 103. Dickstein K, Cohen-Solal A, Filippatos G, McMurray JJ, Ponikowski P, et al. (2008) ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the diagnosis and treatment of acute and chronic heart failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur J Heart Fail 10: 933–89. [DOI] [PubMed] [Google Scholar]
- 104. Altman DG, Lausen B, Sauerbrei W, Schumacher M (1994) Dangers of using “optimal” cutpoints in the evaluation of prognostic factors. Journal of the National Cancer Institute 86: 829–835. [DOI] [PubMed] [Google Scholar]
- 105. Hilsenbeck SG, Clark GM, McGuire WL (1992) Why do so many prognostic factors fail to pan out? Breast Cancer Research and Treatment 22: 197–206. [DOI] [PubMed] [Google Scholar]
- 106. Schulgen G, Lausen B, Olsen JH, Schumacher M (1994) Outcome-oriented cutpoints in analysis of quantitative exposures, American Journal of Epidemiology. 140: 172–184. [DOI] [PubMed] [Google Scholar]
- 107.Cleland JG, Abraham WT, Linde C, Gold MR, Young JB, et al. (2013) An individual patient meta-analysis of five randomized trials assessing the effects of cardiac resynchronization therapy on morbidity and mortality in patients with symptomatic heart failure. Eur Heart J In press. [DOI] [PMC free article] [PubMed]
- 108. Raphael CE, Whinnett ZI, Davies JE, Fontana M, Ferenczi EA, et al. (2009) Quantifying the paradoxical effect of higher systolic blood pressure on mortality in chronic heart failure. Heart 95: 56–62. [DOI] [PubMed] [Google Scholar]
- 109. Gheorghiade M, Rossi JS, Cotts W, Shin DD, Hellkamp AS, et al. (2007) Characterization and prognostic value of persistent hyponatremia in patients with severe heart failure in the ESCAPE Trial. Arch Intern Med 167: 1998–2005. [DOI] [PubMed] [Google Scholar]
- 110. Pfister R, Diedrichs H, Schiedermair A, Rosenkranz S, Hellmich M, et al. (2008) Prognostic impact of NT-proBNP and renal function in comparison to contemporary multi-marker risk scores in heart failure patients. Eur J Heart Fail 10: 315–20. [DOI] [PubMed] [Google Scholar]
- 111. Ohman EM, Armstrong PW, Christenson RH, Granger CB, Katus HA, et al. (1996) Cardiac troponin T levels for risk stratification in acute myocardial ischemia. GUSTO IIA Investigators. N Engl J Med 335: 1333–41. [DOI] [PubMed] [Google Scholar]
- 112. Pepe MS, Janes H, Longton G, Leisenring W, Newcomb P (2004) Limitations of the odds ratio in gauging the performance of a diagnostic, prognostic, or screening marker. Am J Epidemiol 159: 882–90. [DOI] [PubMed] [Google Scholar]
- 113. Karvanen J, Harrell FE Jr (2009) Visualizing covariates in proportional hazards model. Stat Med 28: 1957–66. [DOI] [PubMed] [Google Scholar]
- 114. Royston P, Altman DG, Sauerbrei W (2006) Dichotomizing continuous predictors in multiple regression: a bad idea. Stat Med 25: 127–41. [DOI] [PubMed] [Google Scholar]
- 115. Wainer H (2006) Finding what is not there through the unfortunate binning of results: The Mendel effect. Chance 19: 49–56. [Google Scholar]
- 116. Harrell FE Jr, Margolis PA, Gove S, Mason KE, Mulholland EK, et al. (1998) Development of a clinical prediction model for an ordinal outcome: the World Health Organization Multicentre Study of Clinical Signs and Etiological agents of Pneumonia, Sepsis and Meningitis in Young Infants. WHO/ARI Young Infant Multicentre Study Group. Stat Med 17: 909–44. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA checklist.
(DOC)