Abstract
Background
Overexpression of Oct4, an important transcription factor of embryonic stem cells (ESC), has been reported in several cancers. The aim of this study was to determine the emerging role of Oct4 in oral squamous cell carcinoma (OSCC) both in vitro and in vivo.
Methodology/Principal Finding
Tumourigenic activity and molecular mechanisms of Oct4 overexpression or knockdown by lentiviral infection in OSCC was investigated in vitro and in vivo. Initially, we demonstrated that Oct4 expression was increased in OSCC cell lines as compared to a normal oral epithelial cell line SG. Overexpression of Oct4 was demonstrated to enhance cell proliferation, invasiveness, anchorage-independent growth and xenotransplantation tumourigenicity. These findings were coupled with epithelial-mesenchymal transition (EMT) transformation in OSCCs. In contrast, the silence of Oct4 significantly blocked the xenograft tumorigenesis of OSCC-derived cancer stem cells (OSCC-CSCs) and significantly improved the recipient survival. Clinically, the level of Oct4 expression was higher in recurrent and metastatic OSCC specimens but lower in primary OSCC specimens.
Conclusion/Significance
Our results suggest that Oct4-mediated tumorigenecity is associated with the regulation of EMT. Oct4 might be a therapeutic target for OSCC.
Introduction
Oral squamous cell carcinoma (OSCC) is the sixth most prevalent malignancy worldwide and accounts for approximately 8–10% of all cancers in Southeast Asia [1]. The prognosis of OSCC remains dismal because more than 50% of patients die from this disease or complications within 5 years with current therapies [2]. Therefore, an improved comprehension of the cellular and molecular mechanisms which initiate tumorigenesis or promote cancer progression, was pursued to bring forth future progress of medical treatment of OSCC.
Oct4 is the key transcription factor that is involved in the maintenance of pluripotency and self-renewal in undifferentiated embryonic stem (ES) cells [3]. Oct4 could reprogram human somatic fibroblasts into embryonic stem cell-like pluripotent cells which are termed as inducible pluripotent stem cells (iPSC) [4]. Oct4 has been reported to be overexpressed in various cancers including germ cell tumors [5],breast [6], cervix [7], oral [8], prostate [9], lung [10], gastric [11], brain [12], liver [13], and ovarian cancer [14]. Oct4 is also to be a key determinant of cancer stem cells (CSCs) properties [15]. Previously, we have demonstrated that Oct4 is upregulated in OSCC-CSCs and OSCC specimens are negatively correlated with the survival rate of OSCC patients [8]. However, Oct4 mediated molecular mechanisms in OSCC still remain to be elucidated.
Epithelial mesenchymal transition (EMT) is a de-differentiation program that converts adherent epithelial cells into individual migratory cells. EMT is thought to be a key step in the induction of tumor malignancy, oncogenic progression, and cancer metastasis [16]. Recently, the interplay between EMT and a cancer stemness signature has gained huge interest in the field of cancer research [17]. Researchers have shown that EMT can promote stemness properties and further generate cells with the features of breast CSCs [18]. The EMT program is also reported to play an important role to maintain the property of tumor initiating cells in OSCCs [19]. The detailed molecular mechanisms involved in the regulatory links between Oct4 and EMT properties are still poorly understood. Herein, we demonstrate a critical role of Oct4 overexpression in the enhancement of stemness and EMT in OSCCs. In addition, an animal model revealed that the inhibition of Oct4 may improve the outcome of OSCCs.
Materials and Methods
OSCC tissues acquirement and preparation
Surgical tissue specimens from OSCC patients were collected after obtaining written informed consent and this study was approved by The Institutional Review Board in Chung Shan Medical University Hospital (CSMUH No: CS10249). Human primary OSCC carcinoma (T) tissue, normal paired noncancerous matched tissues (N), as well as available lymph node metastatic lesions (M) were obtained from surgical procedures sent to the pathology lab for frozen section diagnosis. Tumor tissues were microscopically screened to have >70% of their areas occupied by tumor cells; The remaining specimen (tumor, normal counterpart, and lymph node metastatic lesions) were snap frozen in liquid nitrogen and stored at −80°C for Real-time Reverse transcription–PCR (qRT-PCR).
Cell lines
Nine OSCC cell lines (SAS [20], FaDu [21], OECM1 [22], SCC4 [23], HSC3 [24], OC3 [25], Ca922 [26], SCC25 [27], and GNM [28] and one normal gingival epithelial cell line SG [29] were used in this study.
SYBR real-time reverse transcription-polymerase chain reaction (RT-PCR)
Total RNA of cells was purified using Trizol reagent (Invitrogen, Carlsbad, CA, USA) according to the manufacturer's protocol. Briefly, the total RNA (1 µg) of each sample was reversely transcribed by Superscript II RT (Invitrogen, Carlsbad, CA, USA). Then, the amplification was carried out in a total volume of 20 µl containing 0.5 µM of each primer, 4 mM MgCl2, 2 µl LightCycler™ –FastStart DNA Master SYBR green I (Roche Molecular Systems, Alameda, CA, USA) and 2 µl of 1:10 diluted cDNA. The GAPDH housekeeping gene was amplified as a reference standard. GAPDH primers were designed: GAPDH (forward): GGGCCAAAAGGGTCATCATC (nt 414–434, GenBank accession no. BC059110.1), GAPDH (reverse): ATGACCTTGCCCACAGCCTT (nt 713–733). PCR reactions were prepared in duplicate and heated to 95°C for 10 minutes followed by 40 cycles of denaturation at 95°C for 10 seconds, annealing at 55°C for 5 seconds, and extension at 72°C for 20 seconds. All PCR reactions were performed in triplicate. Standard curves (cycle threshold values versus template concentration) were prepared for each target gene and for the endogenous reference (GAPDH) in each sample. To confirm the specificity of the PCR reaction, PCR products were electrophoresed on a 1.2% agrose gel [30]. Primer sequences are listed in Table 1.
Table 1. The sequences of the primers for quantitative RT-PCR.
| Gene (Accession No.) | Primer Sequence (5′ to 3′) | Product size (bp) | Tm (°C) |
| Slug (NM_003068) | F: GTGATTATTTCCCCGTATCTCTAT, R: CAATGGCATGGGGGTCTGAAAG | 292 | 50 |
| E-caderin (NM_004360) | F: ATTCTGATTCTGCTGCTCTTG, R: AGTCCTGGTCCTCTTCTCC | 136 | 50 |
| N-caderin (NM_001792) | F: CCACGCCGAGCCCCAGTATC, R: CCCCCAGTCGTTCAGGTAATCA | 232 | 55 |
| Oct-4 (NM_002701) | F: GTGGAGAGCAACTCCGATG, R: TGCTCCAGCTTCTCCTTCTC | 86 | 60 |
| GAPDH (NM_002046) | F: CATCATCCCTGCCTCTACTG, R: GCCTGCTTCACCACCTTC | 180 | 60 |
Cell proliferation assay
An MTT assay kit (Sigma-Aldrich) was used to analyze the cell proliferation. Specifically, 1×103 cells were seeded in each well of a 24-well plate, and then 10 µL of MTT solution was added to the cells which were then incubated at 37°C for 3 hours. The supernatant was removed, and 200 µL of DMSO were added directly to the cells. The MTT color reaction was analyzed using a microplate reader set at A560 nm.
Stable overexpression of Oct4 in OSCC cells
Human full-length Oct4 cDNA was cloned into pCDH1-MCS1-EF1-copGFP (System Biosciences, Cat. No: CD511A-1; Mountain View, CA, USA). Lentivirus production was performed by co-transfection of a plasmid DNA mixture with lentivector plus helper plasmids (VSVG and Gag-Pol) into 293 T cells (American Type Culture Collection, Manassas, VA, USA) using Lipofectamine 2000 (LF2000, Invitrogen, Calsbad, CA, USA). The lentivirus M.O.I titer was determined by flow cytometry (average of 5×104 and 2×105 TU/ml). To generate the stable cell lines, sub-confluent OSCC cells were infected with lentivirus in the presence of 8 µg/ml polybrene (Sigma-Aldrich, St Louis, MO, USA). Stable Oct4-overexpressing OSCC cells were further purified by cell sorting with GFP positive cells. The pCDH1-MCS1-EF1-copGFP empty vector alone was utilized for the experimental control [31].
Construction of lentiviral-mediated RNAi for silencing Oct4
The pLV-RNAi vector, which co-expressed GFP protein in infected host cells, was purchased from Biosettia Inc. (Biosettia, San Diego, CA, USA). The method of cloning the double-stranded shRNA sequence was described in the manufacturer's protocol. Lentiviral vectors expressing shRNA that targets human Oct4 were synthesized and cloned into pLVRNAi to generate a lentiviral expression vector. Sh-Luc:5′-CCGGACTTACGCTGAGTACTTCGAACTCGAGTTCGAAGTACTCAGCGTAAGTTTTTTG-3′ was utilized for an experimental control. Lentivirus production was performed as above. Stable pLV-RNAi expressed OSCC cell lines were further purified by cell sorting with GFP positive cells [31].
In vitro cell invasion assay
For transwell migration assays, 2×105 cells were plated into the top chamber of a transwell (Corning, Acton, MA, USA) with a porous membrane (8.0 µm pore size). Cells were plated in medium with lower serum (0.5% FBS) and medium supplemented with higher serum (10% FBS) was used as a chemoattractant in the lower chamber. The cells were incubated for 24 h at 37°C and cells that did not migrate through the pores were removed by a cotton swab. Cells on the lower surface of the membrane were stained with Hoechst 33258 (Sigma-Aldrich Co., St. Louis, MO, USA) to show the nuclei; fluorescence was detected at a magnification of 100× using a fluorescence microscope (Carl Zeiss, Oberkochen, Germany). The number of fluorescent cells in a total of five randomly selected fields was counted. In vitro cell invasion analysis was conducted as described previously [8].
Tumorsphere-forming assay
Tumor cells were dissociated and cultured as tumorspheres in modified DMEM/F-12 supplemented with N2 (Invitrogen, Carlsbad, CA, USA), 10 ng/mL epidermal growth factor (EGF, Invitrogen, Carlsbad, CA, USA), 10 ng/mL basic fibroblast growth factor (bFGF, Invitrogen, Carlsbad, CA, USA), and penicillin/streptomycin at 103 live cells/low-attachment six-well plate (Corning Inc., Corning, NY, USA), and the medium was changed every other day until the tumor sphere formation was observed in about 2 weeks. For serial passage of spheroid cells, single cells were obtained from accurtase-treated spheroids and the cell density of passage was 1000 cells/ml in the serum-free medium as described above [30].
Soft agar colony forming assay
Each well (35 mm) of a six-well culture dish was coated with 2 ml of bottom agar (Sigma-Aldrich Co., St. Louis, MO, USA) mixture (DMEM, 10% (v/v) FCS, 0.6% (w/v) agar). After the bottom layer was solidified, 2 ml of top agar-medium mixture (DMEM, 10% (v/v) FCS, 0.3% (w/v) agar) containing 2×104 cells was added, and the dishes were incubated at 37°C for 4 weeks. Plates were stained with 0.005% Crystal Violet, then the colonies were counted. The total number of colonies with a diameter ≥100 µm was counted over five fields per well for a total of 15 fields in triplicate experiments [30].
Subcutaneous xenografts in nude mice
All the animal practices in this study were approved and in accordance with the Institutional Animal Care and Use Committee (IACUC) of Chung Shan Medical University, Taichung, Taiwan. 1×106 OSCC cells mixed with Matrigel (BD bioscience, San Diego, CA, USA) (1:1) were injected subcutaneously into BALB/c nude mice (6–8 weeks). Tumor volume (TV) was calculated using the following formula: TV (mm3) = (Length × Width 2)/2 [32].
Statistical analysis
A Statistical Package of Social Sciences software (version 13.0) (SPSS, Inc., Chicago, IL) was used for statistical analysis. Student's t test was used to determine statistical significance of the differences between experimental and control groups; p values less than 0.05 were considered statistically significant.
Results
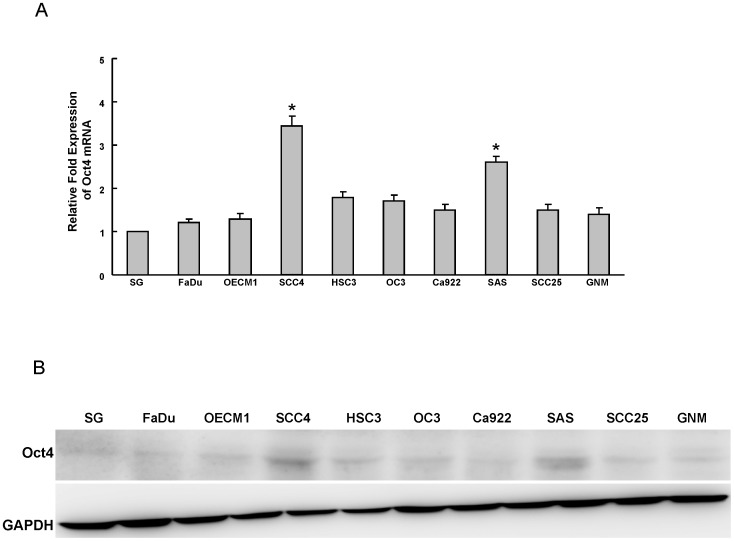
Expression of Oct4 in OSCC cell lines
To understand the expression of Oct4 in OSCC cell lines (OSCCs), the endogenous protein level of Oct4 in nine established OSCC cell lines and one normal oral epithelial cell line SG was examined by real-time RT-PCR and western blot analyses. As shown in figure 1A and 1B, Oct4 mRNA and protein were detectable in OSCC cell lines SSC4 and SAS OSCCs. However, it was lower or undetectable in normal oral epithelial cell line SG (Fig. 1A and B).
Figure 1. Determination of Oct4 expression in OSCC cells.
Oct4 mRNA (A) and protein (B) expression in nine OSCC lines and one normal oral epithelial cell (SG) were examined by real-time RT-PCR analysis and western blotting. The amount of GAPDH protein of different crude cell extracts was referred to as a loading control. Error bars correspond to SD. (*, p<0.05)
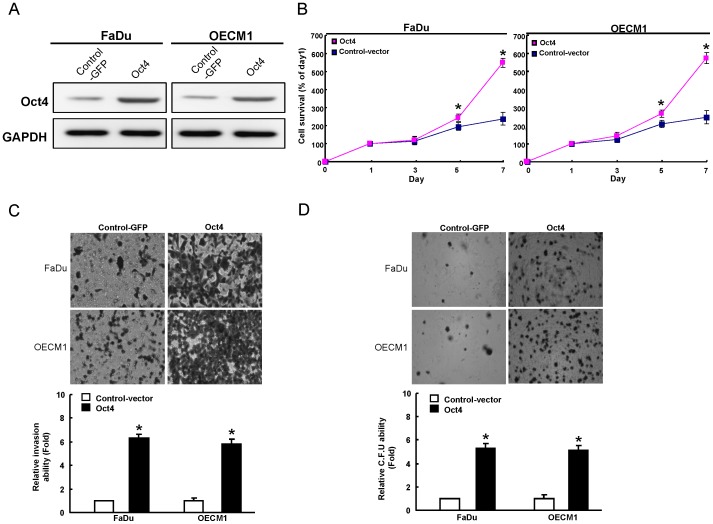
Oct4 overexpression enhanced cell proliferation, invasiveness, and colony formation
To further investigate the upregulation of Oct4 on the biological properties of OSCC cell lines, we generated stable Oct4-overexpressing OSCC cell lines through lentiviral-mediated transduction. As shown in figure 2A, two Oct4-overexpressing OSCC cell lines, FaDu and OECM1, displayed elevated Oct4 expression by western blot analysis. Oct4-overexpressing OSCC cell lines showed enhanced proliferative activity (Fig. 2B). In addition, Oct4-overexpressing OSCC cell lines also resulted in increased ability of cell invasiveness (Fig. 2C) and colony formation (Fig. 2D). Collectively, these results suggest that overexpression of Oct4 may promote in vitro tumorigenicity of OSCC cells.
Figure 2. Overexpression of Oct4 in OSCCs enhances in vitro tumorigenic properties.
(A) Total proteins were prepared from control vector–expressing and Oct4-overexpressing OSCCs (OECM1 and FaDu) and analyzed by immunoblotting against anti-Oct4 or anti-GAPDH antibodies as indicated. The amount of GAPDH protein of different crude cell extracts was referred to as a loading control. OECM1 and FaDu cells were transfected with Oct4 or control vector DNA and examined for (B) proliferation ability, (C) Matrigel invasion ability, and (D) anchorage-independent growth as described in the Materials and Methods section. The data shown are the means ± SD from three independent experiments.
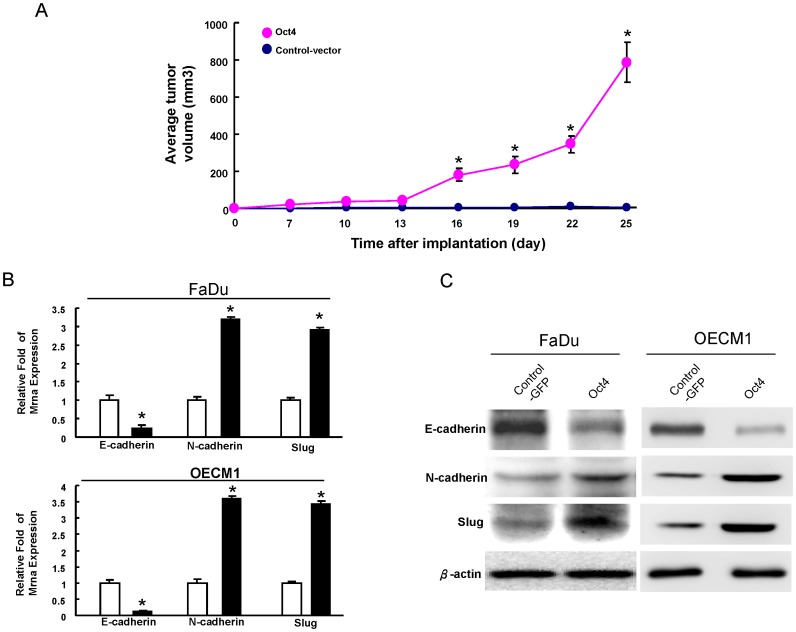
Oct4 overexpression enhances in vivo tumourigenicity and mesenchymal traits in OSCCs
The comparison between GFP expressing control cells and Oct4-overexpressing OSCC cell lines showed a significant increase in tumorigenic ability of OSCC cells in vivo (Fig. 3A). Previously, Yang et al. (2008) reported that OSCC cells expressed with elevated EMT markers were highly metastatic, tumorigenic, and resistant to radiotherapy/chemotherapy [33]. As shown in figures 3B and 3C, we also found the reduced expression of an epithelial marker, E-cadherin, but the enhanced expression of mesenchymal markers N-cadherin and Slug in Oct4-overexpressing OSCCs.
Figure 3. Overexpression of Oct4 in OSCCs promotes in vivo tumorigenicity and EMT properties.
(A) FaDu cells were transfected with Oct4 or control vector. The transfected cells were injected subcutaneously into the flank of nude mice. FaDu cells were transfected with or control vector and Oct4. Cell extracts from the transfected cells were analyzed for the EMT marker by real-time RT-PCR analysis (B) and western blot (C).
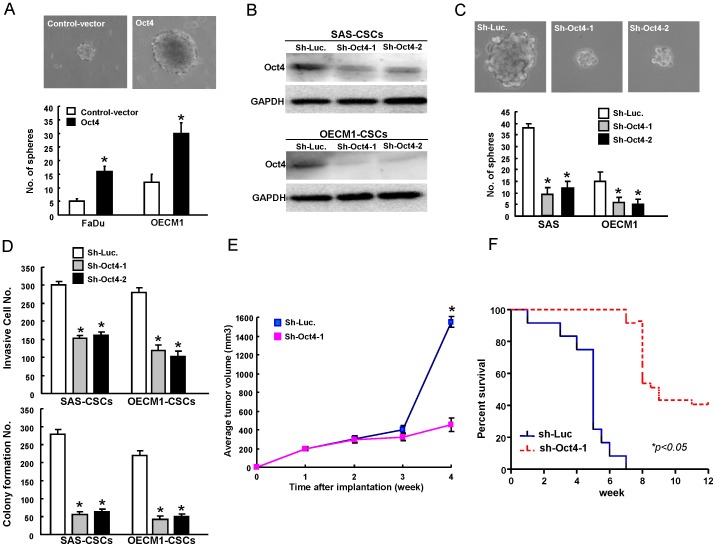
Targeting Oct4 effectively abrogates in vitro and in vivo malignant properties of OSCC-CSCs
Sphere-forming OSCC cells have been shown to exhibit cancer stem cells properties [8], [30]. In this study, we displayed the up-regulation of Oct4 in OSCC-CSCs from FaDu and OECM1 cells. Oct4-overexpressing OSCCs could enhance the sphere-forming ability (Fig. 4A). To further investigate whether Oct4 could play a role in maintaining CSCs properties of OSCC-CSC, the measurement of loss-of-function of Oct4 was first conducted. Down-regulation of Oct4 in OSCCs-CSCs was achieved by viral transduction with lentiviral vector expressing small hairpin RNA (shRNA) targeting Oct4 (sh- Oct4-1 and sh-Oct4-2). Lentiviral vector expressing shRNA against luciferase (sh-Luc) was used as the control. Immunoblotting analyses confirmed that lentivirus expressing both sh-Oct4-1 and sh- Oct4-2 markedly reduced the expression level of Oct4 protein in transduced OSCCs-CSCs (Fig. 4B). Down-regulation of Oct4 decreased the self-renewal capacity of OSCCs-CSCs (Fig. 4C). Infection with sh- Oct4 expressing lentivirus significantly decreased matrigel invasion and anchorage independent growth of OSCCs-CSCs (Fig. 4D). The inhibition of Oct4 expression significantly slowed down the tumor growth mediated by OSCC-CSC (Fig. 4E). Additionally, the survival of OSCCs-CSCs-transplanted mice was significantly improved upon Oct4 knockdown treatment (Fig. 4F). Taken together, these data further support the conclusion that the down-regulation of Oct4 may result in the reduction of CSCs properties in OSCCs.
Figure 4. Oct4 downregulation abrogate the cancer stemness in OSCC-CSCs.
(A) Representative images of tumor sphere formation ability of control-GFP or Oct4-overexpressing OSCCs. (B) Single cell suspensions of OSCC-CSCs were transduced with sh-Luc or sh-Oct4 lentivirus for 3 days. Total proteins prepared from infected cells were prepared and analyzed. The silencing effect of Oct4 shRNA in OSCC-CSCs was validated translationally by western blotting (OECM1 (left panel) and SAS (right panel)). Immunoblotting against anti-Oct-4 or anti-GAPDH antibodies was performed as indicated. The amount of GAPDH protein of different crude cell extracts was referred to as a loading control, and for further quantification. (C) OSCC-CSCs were first infected with sh-Oct-4-1, sh-Oct-4 -2 or sh-Luc lentivirus for 3 days, and then further cultivated under the serum-free defined selection medium. The cellular morphology of OSCC-CSCs treated with sh-Luc or Oct-4-shRNA lentivirus was examined. (D) To elucidate the capability of cell invasiveness (upper panel) and anchorage independent growth (lower panel) of OSCC-CSCs, OSCC-CSCs with Oct-4 down-regulation, single cell suspension of OSCC-CSCs infected with Oct-4-specific shRNA or control sh-Luc lentivirus for three days were plated onto transwells coated with matrigel and soft agar, respectively, and analyzed as described in the Materials and Methods section. Results are means ± SD of triplicate samples from three experiments. (E) Representative tumors of control and Oct4-knockdown OSCC-CSCs were generated, and the tumors were then dissected from the subcutaneous space of recipient mice (n = 3). (F) Kaplan–Meier survival analysis further indicated the mean survival rates of animals transplanted with control and Oct4-knockdown OSCC-CSCs.
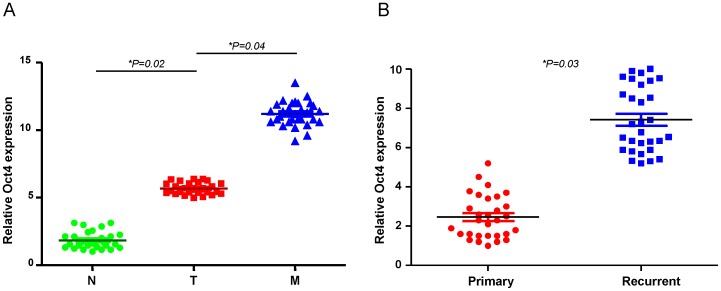
The upregulation of Oct4 expression in recurrent and metastatic OSCC patients
To validate the significance of Oct4 expression in clinical specimens, we collected paired samples of non-tumor (N), local tumor (T), and lymph node (LN) tissues from OSCC patients and subjected these samples to real-time RT-PCR analysis. Compared with non-tumor samples from the same patient, the expression of Oct4 was increased in all of the tumor samples (Fig. 5A). A similar upregulation of Oct4 was also observed in metastatic lymph nodes when compared with local tumors (T) (Fig. 5A). We also compared the levels of these molecules between primary and recurrent lesions in OSCC patient tissues. In line with our previous data, the level of Oct4 expression was higher in recurrent OSCC tumor samples but lower in primary lesions (Fig. 5B). These findings revealed a high Oct4 expression signature as a potential marker of metastasis and recurrence of OSCC.
Figure 5. Clinical significance of Oct4 expression in recurrent and metastatic OSCC patients.
(A) Quantitative RT-PCR analysis of Oct4 expression levels in clinical specimens from a non-tumor region (N) or a tumor region (T) or lymph node (N) of OSCC patients with metastases. (J) (B) Quantitative RT-PCR analysis of Oct4 expression levels in clinical specimens from primary (P) and recurrent (R) OSCC patients.
Discussion
OSCC is one of the leading causes of cancer-related deaths worldwide [34]. Its high invasiveness and frequent recurrence are the major reasons for treatment failures and a poor prognosis [2]. Accumulating data demonstrate that a CSCs hypothesis has been bolstered by the clinical observation that malignant tumors are relatively resistant to chemo-radiotherapies [35], [36]. OSCC-derived CSCs have been known to have the capacity to promote tumor progression and metastasis, and also contribute to radio-resistance and chemo-resistance [37], [38]. Thus, it is necessary to unravel the underlying mechanisms of the CSC pathway in OSCC and to further evaluate the therapeutic possibilities of CSC-targeted therapy clinically. It is generally accepted that several embryonic stem cell-specific signalings are reactivated in CSC by several cancer models [39]–[41]. The embryonic stem cell-specific transcriptional factor Oct4 was shown to be highly expressed in hepatic, colorectal, and brain CSCs [12], [13], [39]. Our previous report demonstrated high expression of Oct4 in malignancies of OSCC-CSCs and OSCC patients [8]. Chiou et al. also demonstrated the overexpression of Oct4 and Nanog transformed lung cancer cells into a CSCs-like state [42]. In the present study, we directly evaluated the role of Oct4 in the maintenance of tumorigenic potential of OSCCs by lentiviral shRNAi mediated overexpression and lentiviral-mediated knockdown of Oct4. Overexpression of Oct4 enhanced tumorigenic properties of OSCCs both in vitro and in vivo (Fig. 2& Fig. 3). Depletion of Oct4 decreased the sphere-forming capability, invasion ability, and xenograft tumorigenesis of OSCC-CSCs and largely improved recipient survival (Fig. 4). These results revealed that Oct4 could promote OSCC malignancy. Therefore, Oct4 may serve as a therapeutic target for the treatment of metastatic OSCC.
EMT is critical for embryonic development and oncogenic progression [16]. Yang et al. found that both Twist1 and Bmi-1 were mutually essential to promote EMT and tumor-initiating capability [43]. Enhanced EMT characteristics are associated with poor overall and metastasis-free survival in patients with OSCC [19], [33]. Recent studies suggested that EMT promotes stemness properties in normal breast tissue and breast cancer cells [18], [44]. Results support the idea that Oct4/Nanog signaling regulates tumor-initiating abilities, and promotes metastasis in lung cancer cells through regulation of EMT [42]. Slug Snail, and Twist, EMT-related transcription factors, have been reported to increase the metastatic ability and cancer stemness in cancer cells [45]-[47]. To the best of our knowledge, we are the first to report that Oct4 could regulate tumor initiating property and EMT traits, at least in part (Fig. 3). Overexpression of Oct4 in OSCC cells resulted in an EMT-favored pattern in which mesenchymal markers such as Slug and N-cadherin were increased (Fig. 3C). The discovered roles of Oct4 coupled with the EMT process has stimulated a huge interest in the field of cancer research as it indicates that misplaced cancer stemness properties contribute to tumor metastasis and recurrence, making cancer difficult to treat. A further understanding on the regulatory networks between EMT and stemness signatures may update our current knowledge on the development of therapeutic treatments for malignant cancers in the future.
It is of interest to further elucidate the mechanisms by which downstream factors regulated by Oct4 expression in OSCC in vivo and to understand how Oct4 mediates EMT and cancer stemness in OSCC. Overall, targeting Oct4 in malignant OSCC may create a new approach for therapeutic treatments in the future.
Funding Statement
This study was supported by a research grant from Chung Shan Medical University Hospital (CSH-2013-C-015) and the National Science Council (100-2632-B-040-001-MY3, 101-2314-B-040-016, 102-2628-B-040 -001 -MY3) in Taiwan, ROC. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Yu CC, Chang YC (2013) Enhancement of cancer stem-like and epithelial-mesenchymal transdifferentiation property in oral epithelial cells with long-term nicotine exposure: reversal by targeting SNAIL. Toxicol Appl Pharmacol 266: 459–469. [DOI] [PubMed] [Google Scholar]
- 2. Siegel R, Naishadham D, Jemal A (2013) Cancer statistics, 2013. CA Cancer J Clin 63: 11–30. [DOI] [PubMed] [Google Scholar]
- 3. Wang J, Rao S, Chu J, Shen X, Levasseur DN, et al. (2006) A protein interaction network for pluripotency of embryonic stem cells. Nature 444: 364–368. [DOI] [PubMed] [Google Scholar]
- 4. Park IH, Zhao R, West JA, Yabuuchi A, Huo H, et al. (2008) Reprogramming of human somatic cells to pluripotency with defined factors. Nature 451: 141–146. [DOI] [PubMed] [Google Scholar]
- 5. Looijenga LH, Stoop H, de Leeuw HP, de Gouveia Brazao CA, Gillis AJ, et al. (2003) POU5F1 (OCT3/4) identifies cells with pluripotent potential in human germ cell tumors. Cancer Res 63: 2244–2250. [PubMed] [Google Scholar]
- 6. Ezeh UI, Turek PJ, Reijo RA, Clark AT (2005) Human embryonic stem cell genes OCT4, NANOG, STELLAR, and GDF3 are expressed in both seminoma and breast carcinoma. Cancer 104: 2255–2265. [DOI] [PubMed] [Google Scholar]
- 7. Liu D, Zhou P, Zhang L, Wu G, Zheng Y, et al. (2011) Differential expression of Oct4 in HPV-positive and HPV-negative cervical cancer cells is not regulated by DNA methyltransferase 3A. Tumour Biol 32: 941–950. [DOI] [PubMed] [Google Scholar]
- 8. Chiou SH, Yu CC, Huang CY, Lin SC, Liu CJ, et al. (2008) Positive correlations of Oct-4 and Nanog in oral cancer stem-like cells and high-grade oral squamous cell carcinoma. Clin Cancer Res 14: 4085–4095. [DOI] [PubMed] [Google Scholar]
- 9. Ugolkov AV, Eisengart LJ, Luan C, Yang XJ (2011) Expression analysis of putative stem cell markers in human benign and malignant prostate. Prostate 71: 18–25. [DOI] [PubMed] [Google Scholar]
- 10. Chen YC, Hsu HS, Chen YW, Tsai TH, How CK, et al. (2008) Oct-4 expression maintained cancer stem-like properties in lung cancer-derived CD133-positive cells. PLoS One 3: e2637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chen Z, Xu WR, Qian H, Zhu W, Bu XF, et al. (2009) Oct4, a novel marker for human gastric cancer. J Surg Oncol 99: 414–419. [DOI] [PubMed] [Google Scholar]
- 12. Du Z, Jia D, Liu S, Wang F, Li G, et al. (2009) Oct4 is expressed in human gliomas and promotes colony formation in glioma cells. Glia 57: 724–733. [DOI] [PubMed] [Google Scholar]
- 13. Wang XQ, Ongkeko WM, Chen L, Yang ZF, Lu P, et al. (2010) Octamer 4 (Oct4) mediates chemotherapeutic drug resistance in liver cancer cells through a potential Oct4-AKT-ATP-binding cassette G2 pathway. Hepatology 52: 528–539. [DOI] [PubMed] [Google Scholar]
- 14. Zhang S, Balch C, Chan MW, Lai HC, Matei D, et al. (2008) Identification and characterization of ovarian cancer-initiating cells from primary human tumors. Cancer Res 68: 4311–4320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Peng S, Maihle NJ, Huang Y (2010) Pluripotency factors Lin28 and Oct4 identify a sub-population of stem cell-like cells in ovarian cancer. Oncogene 29: 2153–2159. [DOI] [PubMed] [Google Scholar]
- 16. Polyak K, Weinberg RA (2009) Transitions between epithelial and mesenchymal states: acquisition of malignant and stem cell traits. Nat Rev Cancer 9: 265–273. [DOI] [PubMed] [Google Scholar]
- 17. Han XY, Wei B, Fang JF, Zhang S, Zhang FC, et al. (2013) Epithelial-mesenchymal transition associates with maintenance of stemness in spheroid-derived stem-like colon cancer cells. PLoS One 8: e73341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mani SA, Guo W, Liao MJ, Eaton EN, Ayyanan A, et al. (2008) The epithelial-mesenchymal transition generates cells with properties of stem cells. Cell 133: 704–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lo JF, Yu CC, Chiou SH, Huang CY, Jan CI, et al. (2011) The epithelial-mesenchymal transition mediator S100A4 maintains cancer-initiating cells in head and neck cancers. Cancer Res 71: 1912–1923. [DOI] [PubMed] [Google Scholar]
- 20. Okumura K, Konishi A, Tanaka M, Kanazawa M, Kogawa K, et al. (1996) Establishment of high- and low-invasion clones derived for a human tongue squamous-cell carcinoma cell line SAS. J Cancer Res Clin Oncol 122: 243–248. [DOI] [PubMed] [Google Scholar]
- 21. Rangan SR (1972) A new human cell line (FaDu) from a hypopharyngeal carcinoma. Cancer 29: 117–121. [DOI] [PubMed] [Google Scholar]
- 22. Shieh TM, Lin SC, Liu CJ, Chang SS, Ku TH, et al. (2007) Association of expression aberrances and genetic polymorphisms of lysyl oxidase with areca-associated oral tumorigenesis. Clin Cancer Res 13: 4378–4385. [DOI] [PubMed] [Google Scholar]
- 23. Lin CW, Chen PN, Chen MK, Yang WE, Tang CH, et al. (2013) Kaempferol Reduces Matrix Metalloproteinase-2 Expression by Down-Regulating ERK1/2 and the Activator Protein-1 Signaling Pathways in Oral Cancer Cells. PLoS One 8: e80883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Yu FS, Yang JS, Yu CS, Lu CC, Chiang JH, et al. (2011) Safrole induces apoptosis in human oral cancer HSC-3 cells. J Dent Res 90: 168–174. [DOI] [PubMed] [Google Scholar]
- 25. Lin SC, Liu CJ, Chiu CP, Chang SM, Lu SY, et al. (2004) Establishment of OC3 oral carcinoma cell line and identification of NF-kappa B activation responses to areca nut extract. J Oral Pathol Med 33: 79–86. [DOI] [PubMed] [Google Scholar]
- 26. Chen HM, Liu CM, Yang H, Chou HY, Chiang CP, et al. (2011) 5-aminolevulinic acid induce apoptosis via NF-kappaB/JNK pathway in human oral cancer Ca9-22 cells. J Oral Pathol Med 40: 483–489. [DOI] [PubMed] [Google Scholar]
- 27. Chen CY, Chiou SH, Huang CY, Jan CI, Lin SC, et al. (2009) Tid1 functions as a tumour suppressor in head and neck squamous cell carcinoma. J Pathol 219: 347–355. [DOI] [PubMed] [Google Scholar]
- 28. Lee SS, Tsai CH, Ho YC, Chang YC (2008) The upregulation of heat shock protein 70 expression in areca quid chewing-associated oral squamous cell carcinomas. Oral Oncol 44: 884–890. [DOI] [PubMed] [Google Scholar]
- 29. Srisopark SS (1975) Phagocytosis of thorotrast by human gingival epithelial (SG line) cells in tissue culture: an electron microscopic study. J Dent Assoc Thai 25: 77–102. [PubMed] [Google Scholar]
- 30. Yu CC, Tsai LL, Wang ML, Yu CH, Lo WL, et al. (2013) miR145 targets the SOX9/ADAM17 axis to inhibit tumor-initiating cells and IL-6-mediated paracrine effects in head and neck cancer. Cancer Res 73: 3425–3440. [DOI] [PubMed] [Google Scholar]
- 31. Chen YS, Wu MJ, Huang CY, Lin SC, Chuang TH, et al. (2011) CD133/Src axis mediates tumor initiating property and epithelial-mesenchymal transition of head and neck cancer. PLoS One 6: e28053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wu MJ, Jan CI, Tsay YG, Yu YH, Huang CY, et al. (2010) Elimination of head and neck cancer initiating cells through targeting glucose regulated protein78 signaling. Mol Cancer 9: 283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Yang MH, Wu MZ, Chiou SH, Chen PM, Chang SY, et al. (2008) Direct regulation of TWIST by HIF-1alpha promotes metastasis. Nat Cell Biol 10: 295–305. [DOI] [PubMed] [Google Scholar]
- 34. Kamangar F, Dores GM, Anderson WF (2006) Patterns of cancer incidence, mortality, and prevalence across five continents: defining priorities to reduce cancer disparities in different geographic regions of the world. J Clin Oncol 24: 2137–2150. [DOI] [PubMed] [Google Scholar]
- 35. Wicha MS, Liu S, Dontu G (2006) Cancer stem cells: an old idea–a paradigm shift. Cancer Res 66: 1883–1890 discussion 1895–1886 [DOI] [PubMed] [Google Scholar]
- 36. Visvader JE, Lindeman GJ (2008) Cancer stem cells in solid tumours: accumulating evidence and unresolved questions. Nat Rev Cancer 8: 755–768. [DOI] [PubMed] [Google Scholar]
- 37. Hu FW, Tsai LL, Yu CH, Chen PN, Chou MY, et al. (2012) Impairment of tumor-initiating stem-like property and reversal of epithelial-mesenchymal transdifferentiation in head and neck cancer by resveratrol treatment. Mol Nutr Food Res 56: 1247–1258. [DOI] [PubMed] [Google Scholar]
- 38. Chen YW, Chen KH, Huang PI, Chen YC, Chiou GY, et al. (2010) Cucurbitacin I suppressed stem-like property and enhanced radiation-induced apoptosis in head and neck squamous carcinoma–derived CD44(+)ALDH1(+) cells. Mol Cancer Ther 9: 2879–2892. [DOI] [PubMed] [Google Scholar]
- 39. Saigusa S, Tanaka K, Toiyama Y, Yokoe T, Okugawa Y, et al. (2009) Correlation of CD133, OCT4, and SOX2 in rectal cancer and their association with distant recurrence after chemoradiotherapy. Ann Surg Oncol 16: 3488–3498. [DOI] [PubMed] [Google Scholar]
- 40. Zhang J, Espinoza LA, Kinders RJ, Lawrence SM, Pfister TD, et al. (2013) NANOG modulates stemness in human colorectal cancer. Oncogene 32: 4397–4405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Guo Y, Liu S, Wang P, Zhao S, Wang F, et al. (2011) Expression profile of embryonic stem cell-associated genes Oct4, Sox2 and Nanog in human gliomas. Histopathology 59: 763–775. [DOI] [PubMed] [Google Scholar]
- 42. Chiou SH, Wang ML, Chou YT, Chen CJ, Hong CF, et al. (2010) Coexpression of Oct4 and Nanog enhances malignancy in lung adenocarcinoma by inducing cancer stem cell-like properties and epithelial-mesenchymal transdifferentiation. Cancer Res 70: 10433–10444. [DOI] [PubMed] [Google Scholar]
- 43. Yang MH, Hsu DS, Wang HW, Wang HJ, Lan HY, et al. (2010) Bmi1 is essential in Twist1-induced epithelial-mesenchymal transition. Nat Cell Biol 12: 982–992. [DOI] [PubMed] [Google Scholar]
- 44. Morel AP, Lievre M, Thomas C, Hinkal G, Ansieau S, et al. (2008) Generation of breast cancer stem cells through epithelial-mesenchymal transition. PLoS One 3: e2888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hwang WL, Yang MH, Tsai ML, Lan HY, Su SH, et al. (2011) SNAIL regulates interleukin-8 expression, stem cell-like activity, and tumorigenicity of human colorectal carcinoma cells. Gastroenterology 141: 279–291, 291 e271–275. [DOI] [PubMed]
- 46. Guo W, Keckesova Z, Donaher JL, Shibue T, Tischler V, et al. (2012) Slug and Sox9 cooperatively determine the mammary stem cell state. Cell 148: 1015–1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Way TD, Huang JT, Chou CH, Huang CH, Yang MH, et al. (2013) Emodin represses TWIST1-induced epithelial-mesenchymal transitions in head and neck squamous cell carcinoma cells by inhibiting the beta-catenin and Akt pathways. Eur J Cancer. Epub ahead of print. [DOI] [PubMed]