Abstract
Background
The role of infection preventionists (IPs) is expanding in response to demands for quality and transparency in health care. Practice analyses and survey research have demonstrated that IPs spend a majority of their time on surveillance and are increasingly responsible for prevention activities and management; however, deeper qualitative aspects of the IP role have rarely been explored.
Methods
We conducted a qualitative content analysis of in-depth interviews with 19 IPs at hospitals throughout the United States to describe the current IP role, specifically the ways that IPs effect improvements and the facilitators and barriers they face.
Results
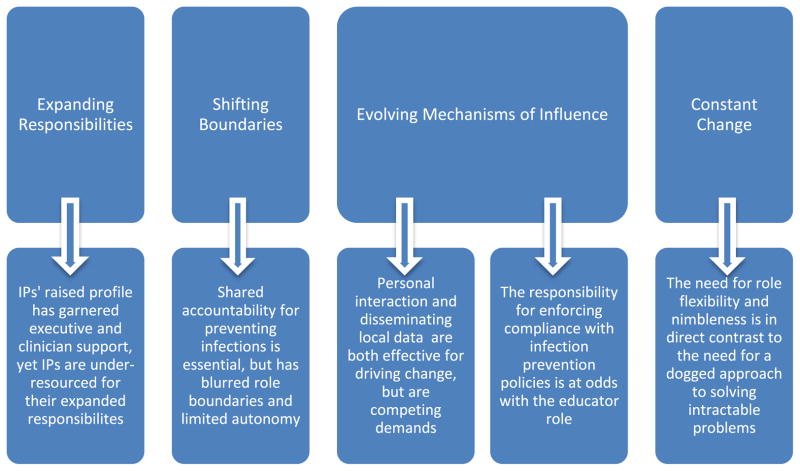
The narratives document that the IP role is evolving in response to recent changes in the health care landscape and reveal that this progression is associated with friction and uncertainty. Tensions inherent in the evolving role of the IP emerged from the interviews as 4 broad themes: (1) expanding responsibilities outstrip resources, (2) shifting role boundaries create uncertainty, (3) evolving mechanisms of influence involve trade-offs, and (4) the stress of constant change is compounded by chronic recurring challenges.
Conclusion
Advances in implementation science, data standardization, and training in leadership skills are needed to support IPs in their evolving role.
Keywords: Infection preventionist, Infection control, Professional role, Qualitative research
Infection preventionists (IPs) are essential constituents of successful infection control programs in health care institutions.1,2 In the past 2 decades, the role of IPs has changed.3 IPs have shifted their focus from monitoring infections to proactively intervening to prevent them.4 They have expanded their scope of practice beyond educating and setting policy to leading performance improvement teams.5
Some changes in the IP role have been routinely documented. Every 5 years, the Certification Board in Infection Control delineates tasks performed and responsibilities assumed by IPs to determine test content.6,7 The list of tasks in the most recent practice analysis in 2009 was dramatically different from 2005.6 Based on the working patterns reported by IP respondents in 2009, 2 practice domains warranted an increased share of test items: preventing/ controlling the transmission of infectious agents and management and communication.6 These changes highlight the growing importance of IPs’ intervention and leadership roles. Other surveys have shown that, although IP staffing has increased significantly since 1976, it has not kept pace with increasing responsibilities.1,3,8,9 Although IPs continue to spend the largest percentage of their time on surveillance, many are not well resourced for this activity; only 35% of infection control programs have help with data management, 32% use an electronic surveillance system to track infections, and 13% have access to statistical expertise.8
Deeper qualitative aspects of the evolving IP role such as mechanisms of influence on clinician practice have rarely been explored. Recently, qualitative studies of infection control programs have indirectly offered insights into the IP role. In a study of organizational culture conducted by Sinkowitz-Cochran et al, hospital employees indicated that their Institute for Healthcare Improvement initiatives were successful and sustainable because the processes were hardwired into daily activities and because they received data feedback.10 In a study of how multidisciplinary teams achieved practice improvements in the area of antimicrobial resistance, Olson et al found that teams used local clinical data as one form of credible evidence to influence key stakeholders, and strong professional relationships were a critical component of success.11 Krein et al studied personnel at hospitals engaged in initiatives to reduce bloodstream infections and found that a collective focus on patient safety, an affirming emotional context, and engaged clinical leadership were factors associated with successful outcomes.12 Further analyses by the same study team underscored the importance of IPs as leaders and identified the potential of intrinsically motivated champions to implement change.13,14 In a study of adherence by intensive care unit staff to guidelines designed to reduce rates of health care-associated infections (HAI), Gurses et al found that systemic ambiguity regarding responsibilities and expectations for guideline adherence were barriers to compliance.15 Although inferences about the IP role may be drawn from these qualitative studies, these components of the IP role have not yet been documented in actual practice.
It is estimated that current evidence-based strategies could prevent 55% to 70% of HAI.16 Therefore, understanding the role of professionals charged with implementing those strategies is imperative. In addition, a rich role description could clarify the nature and value of IP work for clinicians and administrators, thereby facilitating full partnerships with IPs. Finally, an in-depth role description could assist the profession to define itself and provide anticipatory guidance for new IPs. Therefore, our purpose was to describe the evolving role of IPs in acute care hospitals, specifically the ways that IPs effect improvements and the facilitators and barriers they face.
METHODS
We conducted a qualitative content analysis of in-depth, semi-structured interviews with IPs at nonspecialty acute care hospitals throughout the United States. These were a subset of interviews conducted between October 2010 and February 2011 for a mixed-methods study, the “Prevention of Nosocomial Infections and Cost Effectiveness, Refined” (R01 NR010107, PI: P. W. Stone). Approval for the study was granted by institutional review boards at Columbia University Medical Center, New York University Medical Center, and RAND Corporation.
Sample
Hospitals were purposively sampled from among 250 hospitals that responded to a quantitative survey in the first phase of the study. The inclusion criteria included having a medical or medical/ surgical intensive care unit with at least 500 device-days per year and participating in the National Healthcare Safety Network. Additionally, hospitals were purposively selected for maximum variation in size, geographic region, as well as HAI rates, and degree of implementation of HAI prevention strategies, which were based on previous responses to surveys.8,17,18 Participant hospitals were recruited via e-mail to the infection control director. An incentive of $1,000 was offered per hospital. The contact individual was asked to identify key informants from a variety of disciplines; 1 or 2 IPs were interviewed at each hospital. Sampling was completed when interviews at 11 hospitals began to yield only repetitive and confirmatory information (ie, saturation was reached).
Interviews
Topics addressed in the semistructured interview guide included the structure and function of the infection control department, personnel and roles, education of clinicians, compliance monitoring, impact of technologic advances and mandatory reporting of HAI, and facilitators and barriers to infection prevention. Questions were preselected but open-ended and ordered from least to most sensitive. IP interviews lasted between 45 and 90 minutes. (The guide is available from the authors upon request.)
The research team consisted of 4 senior faculty (2 nurses, 1 sociologist, and 1 physician-epidemiologist) and 4 PhD student research assistants (3 nurses and 1 epidemiologist). Prior to commencing field work, team members received training in interview techniques from an expert qualitative researcher (V.H.R.). The qualitative expert gave each of the researchers feedback after practice interviews and their first on-site interviews. Each interview was conducted by a single team member in a private location at a time convenient to the participant. The interviews were audiotaped and transcribed verbatim along with verbal field notes. Peer debriefings occurred in biweekly team meetings held throughout the study. Primary data analysis was initiated concurrently with data collection.
Statistical analysis
Content analysis was employed because it is useful for capturing intangible variables such as the attitudes, beliefs, and opinions of IPs concerning their evolving role in preventing HAI.19,20 Two researchers analyzed the data (L.J.C. and E.L.L.). Interview transcripts were read as whole documents and line by line during an extended period of immersion. Ideas that were repeated by multiple informants were identified, as well as divergent opinions, unique terms, and apt metaphors. Working independently using track changes, the researchers identified informants’ ideas and coded them into categories as they emerged. Agreement on the codes assigned and the broader themes was reached through consensus.
RESULTS
Nineteen IPs at hospitals in all 4 geographic regions of the United States participated. Eighteen were female, and 1 was male; 18 were white, and 1 was black. Two were medical laboratory technologists, and 17 were nurses. Four of the informants had associate degrees, 8 had bachelor’s degrees, and 2 had master’s degrees; education level was not available for 5 respondents. All informants worked in hospitals with more than 1 IP. The average tenure in their current position was 8.5 (range, 1–21) years, and experience as an IP ranged from 1 to 26 years. Ten informants were certified in infection prevention and control.
The IPs’ narratives documented that their role was evolving in response to recent changes in the health care landscape and revealed that, although the evolution is progressive in nature, it is associated with friction and uncertainty. Tensions inherent in the evolving role of the IP emerged from the interviews as 4 broad themes: (1) expanding responsibilities outstrip resources, (2) shifting role boundaries create uncertainty, (3) evolving mechanisms of influence involve trade-offs, and (4) the stress of constant change is compounded by chronic recurring challenges. The themes are summarized in Figure 1 and described below with exemplar quotations.
Fig 1.
Role tensions identified by infection preventionists.
Expanding responsibilities outstrip resources
IPs described their raised profile and expanded responsibilities as a welcome change; however, they related being under-resourced for their growing portfolio. One IP described being under scrutiny: “Everybody knows who we are.... we’re on the hot seat and we know it.” IPs reported receiving increased attention from executives and clinicians and feeling pressure to produce tangible results. One IP explained: “As data goes public, and as the consumer is more aware of the possibilities of the harm that can happen to them in the health care environment, the focus on infection control practitioners to really prevent infections as opposed to just do surveillance is expanding.” Pressure from hospital executives was described by another IP: “they ask questions, they expect action.”
Although IPs were generally positive about their expanded responsibilities, most conceded that there are “not enough hours in the day.” An experienced IP director with a staff of 5 IPs at a large academic medical center said: “We don’t feel like we’re fully resourced, and we do feel that demands on Infection Prevention and Control are simply growing exponentially. And it’s not just regulatory requirements. It’s things like pandemic flu and other emerging diseases, and the complexity of our patient population.” Many IPs reported that, whereas their staffing has improved recently, it has not increased in proportion to the increase in demands. They express being overwhelmed: “We’re desperately trying to do the work of ten with five.”
IPs recounted how, to stretch their limited resources, they use technologies such as hospital intranets to facilitate staff education, laboratory advances to expedite surveillance culture results, and electronic surveillance systems (ESS) to support case finding. One IP touted the benefits of an ESS: “I do think we’re much more in tune to recognizing what a potential cluster may be… we’re much more organized. We can call up a line list at our fingertips.” Her colleague echoed her sentiment when discussing the impact of a new mandatory reporting law: “It has minimally affected our work only because we’re very lucky to have this data mining program… if we didn’t have it, I don’t know what we would have done.”
However, the IPs acknowledged that the investment of time spent learning and adapting information systems to local needs is high and that there are lost opportunity costs, especially the opportunity to interact with staff on the units. As one IP confided: “The vast majority of our time is on the computer…. It’s a constant battle to get it where we need it to be to really be efficient… so we can be out there on the floors.” Another IP explained that ESS can paradoxically lessen opportunities for prevention activities by expanding surveillance activities. “It’s been wonderful. But, as you have access to more information, then you’re able to do more with it, so you add on more responsibilities and more areas of surveillance…. We’ve just added and added and added and added to it.”
Shifting role boundaries create uncertainty
The IP informants described a fundamental change in accountability for HAI, which is altering their professional role. They reported that the responsibility for preventing infections no longer resides solely with the IP department; now, it is shared across the institution. This shift was clearly evident in the following quote: “I believe over the last three years unit ownership and departmental ownership of infection prevention measures has gone up significantly. We always recognize in our department that we’re not going to do this by ourselves. It’s only with their good collaboration that we’re going to make progress in reducing infection.” IP narratives revealed that hospital executives are increasingly engaged in infection prevention efforts, administrators are beginning to demand accountability, and clinicians are gradually assuming responsibility for prevention efforts. As one IP stated: “Without that administrative support, things we’ve tried to implement in the past just didn’t go anywhere. But now that we have the administrative support… we can accomplish a lot more, a whole lot faster.” Another IP detailed how the Vice President for Clinical Effectiveness at her hospital had linked HAI reduction to evaluations and bonuses: “She was responsible for getting… it into the employee’s evaluation, the evaluation of central line associated bloodstream infection. So we wanted to cut them by half, and that was our target, and bonuses were held to that.” A third IP recounted how frontline staff had undertaken a program of isolation compliance monitoring: “They own it, it’s their thing. It’s not my data, that ’s their mechanism. And I think that’s what makes that work.”
Although shared accountability and strong leadership support were viewed as essential to the success of IP programs, some IPs were emotionally ambivalent about the shift in ownership because it had diffused responsibility and blurred their role boundaries. IPs disclosed feelings of uncertainty and loss. In recounting a transfer of responsibility for hand hygiene monitoring and reporting, one IP stated: “We were sort of offended at first because we felt like hand hygiene was our thing, our thing to teach, our thing to improve.” Another IP opined: “I think infection preventionists are the type of people that are usually self-motivated, they want what’s best for the patient, but they tend to be…they like to be in charge of certain things… we’re used to a certain autonomy.”
Several of the IP informants recounted how their infection control programs had been subsumed under a quality improvement department. Although most described this as a positive development, some revealed that the administrative and reporting structures were unstable or were further removed from executive decision makers and clinicians. Two IPs who previously reported to a Chief Medical Officer, and who currently report to a Vice President for Quality through a Performance Improvement Manager were disappointed with the change, saying: “the most important thing for infection control is to be not too far from the top. The closer you are to the top, the easier it is to get things done. You put too many layers through and… things get lost in translation.” In some cases, essential clinical expertise was judged to be lacking among the quality directors to whom IPs reported. This was clearly expressed by an experienced IP: “Our present COO…is very influenced by this quality department. And they don’t speak the language. They don’t know what they’re talking about.”
Shared ownership of HAI prevention has prompted many IPs to refine their role to that of consultant and facilitative leader. Simply put: “The goal is to get everybody at the table and talk about it.” In many instances, IPs spoke of the need to sharpen their skills at facilitation. In the words of an IP with 15 years of experience: “We’re used to being very good at making decisions…. What we’re not as good at is getting everybody else’s opinions first. And so we’re really trying to drive that down and involve as many frontline people as we can before we make a decision to implement a change.”
Evolving mechanisms of influence involve trade-offs
The IP narratives document that IPs employ various mechanisms of influence to effect changes that reduce HAI and that all the mechanisms involve trade-offs. The 3 most commonly discussed mechanisms were personal interaction, data reporting, and education.
Personal interaction
Many IPs cited personal interaction as their preferred mechanism of influence. One IP succinctly stated: “I work through relationships with people. That’s my biggest asset.” IPs shared a common belief in the value of being accessible, visible, and available to staff. Asked what she would do if she were queen for a day, an IP responded: “I would like to be out on the floors more, talking with staff, rounding, doing education, talking to the patients…. And really being the resource that people need me to be, visible. You get some of the best questions when you’re in the milieu.” IPs explained that making rounds provides multiple opportunities for influence by engaging frontline staff and by monitoring and giving feedback on practices and processes. One IP revealed that, without regular personal interaction, staff “become a little too complacent and too lax.”
IPs reported that competing demands, especially demands to generate data, diminished opportunities for personal interaction that leads to real change. One respondent clearly articulated the reason IPs value personal interaction:
“I think if we hardwire processes, then we will eventually have good outcomes. And to hardwire processes you need to change behaviors. And you need to make people see why it’s important and that it’s real. And what it means to them, why it’s important to them. What’s in it for me? And in order to do that, I have to get out of my office and away from the computer, and stop crunching numbers and be out there.”
Several IPs described using intermediaries to extend their interpersonal interactions. They gained indirect influence through champions and physician hospital epidemiologists (HE). One IP explained a common approach: “We’re only a couple of people, so we work through different means and different channels. We have a group of infection prevention associates. These are unit-based nursing staff and respiratory staff that are the liaisons to their department. And we educate them and then they educate their staff.” Another IP spoke of gaining indirect influence with physicians through the expertise and professional status of the physician HE with whom she works: “He’s very highly respected, so the doctors do listen to him. I mean, there is some pushback. Not everybody is there yet. But we have a way to get to the doctors to train them. Otherwise we don’t have direct influence.”
Data
IPs reported that local data are an important mechanism of influence. The IPs explained that, in concert with good relationships, good data build their credibility in the institution. In the words of one IP: “I think that sort of internal shift has occurred, where we just sort of try to get organized and be very thorough in our surveillance, consistent and that sort of thing. And sort of forge social relationships, increase our credibility.” This sense was echoed by another IP: “we need to be very data… data, data, data… not emotional, not an I feel this, I feel that.”
However, IPs acknowledged that generating and disseminating data can be a burden because of the volume and type of data demanded. One IP director expressed a widespread sense of exasperation: “the number of people you have to report to; it’s nuts. Collaboratives and surveys, and all kinds of things. Everyone wants data in different ways and tied up different ways.” IPs confided that occasionally data are requested in inappropriate formats or for inappropriate use—solely to enhance the institution’s image or for punitive purposes. Recounting frequent internal requests for data, one IP said: “They want the data that we collect so they can do the reporting requirements and they want the data to be good, they don’t want any bad data. So that’s disappointing to us. We want honest data…we don’t want data misused.” Several IPs questioned the accuracy and utility of mandated surveillance data. In the words of one IP: “I don’t want to say [colleagues are] gaming the system, but I know that people have different sets of definitions.”
On balance, most IPs considered the powerful influence of data to be worth the cost of collection, as reflected in the following quote: “the whole mandatory data gathering…. I am learning to live with it because it is extremely important when you see the outcomes that you can achieve because you have good information in front of you and you can kind of put it in people’s face. It really does make a difference.”
Education
The narratives revealed that IPs also exert influence by informing and instructing. Fulfilling the educator role was framed as challenging. Several IPs described the challenge of bringing to life invisible infectious threats. One IP explained: “I think the reason that it’s difficult to enforce the infection prevention and control measures that we all know work very well, is that you can’t see what you’re dealing with…. And the other reason is that in infection prevention and control, it’s very difficult to tie the outcome to specific actions, or lack of actions.”
Communicating information to contract physicians, off-shift workers, and large numbers of employees was another challenge cited by IPs. This was illustrated by an IP who recalled the 2009 influenza epidemic: “Communication is just difficult, especially with a facility with 3,000 employees…. I think that was the biggest barrier, being able to get the information out to people and trying to deal with the public as well.” As a further challenge, HAI compete with many other issues for attention. An IP who had recently worked in the clinical area expressed the need to make infection prevention relevant to clinicians: “This is a little slice of what all of our clinical people are doing, we have to make it a really important slice for them.”
Choosing appropriate and feasible teaching strategies was also described as challenging. IPs frequently reported using online learning modules to educate staff, although they admitted that this strategy does not engage all learners. As one IP stated: “I think people like to hear it, and they like the opportunity to ask questions. I think it means more to them. When you have to read something, I think you do what you have to do and you may or may not be engaged when you’re doing it.” To meet these challenges, several IPs reported enlisting the assistance of educators in their staff development departments: “they learn our language and are able then to better communicate back to the rest of their staff.”
The IPs’ comments reflected an assumption that re-educating staff would ensure compliance with policy. One IP’s statement evidenced this belief: “It’s an effective policy when everybody’s aware of it. And if everybody is aware of it, people don’t want to not do the right thing.” This was echoed in the claim of another IP: “once we tell them and explain why, we really don’t have any problem.” Coaxing was the IP’s preferred method of influencing noncompliant staff—through personal relationships and positive one-to-one interactions. In the words of one IP: “you just have to kind of keep at it and kind of let them know that…. I don’t think you’re an awful person, but we really do need to do this. I know you’re busy, but this is important.” In contrast, rigorous policing was perceived as being at odds with relationship building, as shown by the following IP statement: “I think that in the past the infection control practitioner was the police, and that’s not the direction we are going in anymore because that’s just not getting the job done.” Another IP summed up a common sentiment: “you don’t want to be just the nag.”
Tensions arose when IPs recognized noncompliance despite reeducation and coaxing but lacked the institutional power to enforce a policy, yet those with authority did not enforce the policy. An IP new to the role described the problem: “We’re given the responsibility…but we really don’t have any kind of authority over the staff.” Several IPs were bothered by the lack of muscle behind their institutions’ policies. To illustrate this, one IP contrasted the lax enforcement of isolation policies with the stringent enforcement of parking rules at her institution. Several IPs expressed disappointment with the institutional response to noncompliance with hand hygiene policy at their hospitals. Said one IP: “We need to do more than what we’re doing. It needs to be less acceptable and not tolerated from higher up.” Another IP agreed, stating: “we are not interested in addressing infection prevention and control failures on an individual basis. When it really comes down to making people comply, you have to get individualized.” Only a few IPs affirmed that their institutions had formal mechanisms in place to address noncompliance.
Feedback of infection rates to staff was described by IPs as an effective tool for both educating and improving compliance. As one IP commented: “I think between bringing the key players to the table and slowly but surely getting their buy-in; and feeding them back information about the successes that they’ve had as a team on a frequent basis to keep them motivated; I think those are some of the qualities that have helped me be successful. As opposed to being the disciplinarian for bad outcomes.”
The stress of constant change is compounded by chronic recurring challenges
The tensions created by IPs’ expanding responsibilities, shifting boundaries, and evolving mechanisms of influence were indicative of the general tension created by continuous change. Several IPs commented on how changes in health care delivery have necessitated changes in their practice: “We’re trying to get away from just the inpatient hospital. We’re a system, and we want to affect patients, their whole health and well-being…. So we want to adapt infection prevention to that, which I think adapts very well.” Some IPs described keeping up with changes in their patient population: “the babies are littler, many more multiples, the NICU has changed, the environment is different. And we have a new neonatologist…. It’s a whole new world.” Other IPs noted the movement of consumer quality organizations toward proscriptive guidance based on growth in the evidence base: “The Joint Commission and CDC and IHI… we are starting to get things, I think in infection control, more standardized and not as willy-nilly or touchy-feely… because this is what the evidence shows.” IPs disclosed that the need for role flexibility and nimbleness can be exhilarating. In the words of one IP: “this is probably easily the best job I’ve ever had. I’ve had experiences and a variety that most people just don’t get.”
However, the changes were also termed “painful sometimes,” and the stress of adaptation was compounded by chronic challenges. Ongoing adherence and practice issues were described as especially disheartening. IPs cited a lack of compliance with hand hygiene policies, isolation precautions, and construction measures as intractable problems. One IP expressed discouragement over the reluctance of nurses to speak up: “I’ve tried to, for years, say you’re the patient’s advocate… when you see something not being done right. But we’re just not there yet.” Another IP expressed a common frustration succinctly: “If people would just wash their hands, life would be so much better.”
IPs agreed that a dogged approach is necessary to manage both constant change and chronic recurring challenges. One IP stated: “you just have to take it little bits at a time, you can’t just say we’re doing this and it’s either a success or not. It’s just incrementally.” Another IP acknowledged: “Nothing we’ve done has been easy, but we’re persisting.”
DISCUSSION
These in-depth interviews have documented that the role of IPs in acute care settings has evolved from siloed expert to facilitator of quality improvement, and that some uncertainty, perceived loss of autonomy, and stretching of resources have accompanied the change. IPs reported using personal interaction, local data, and education to influence clinical practices to reduce HAI risk; however, these mechanisms of influence compete for the IPs’ time and are not always effective at ensuring compliance with institutional policies. These findings from IPs practicing in acute care hospitals across the United States reinforce those of an earlier statewide study conducted by our team, in which 25 health care professionals in California described how mandatory reporting of HAI data drew needed attention to IPs but created frustration because of unfair comparisons among hospitals and an increased workload for which electronic surveillance systems did not fully compensate.21 The findings also confirm that, nationally, as was first noted in reports from that earlier California study, infection prevention has become an organizational goal toward which IPs lead interdisciplinary teams and that additional layers present in the new reporting structures can act as barriers to success. As in the present study, the California informants influenced practice through data feedback and education.
Measures put in place at the outset of this study to ensure scientific adequacy support the trustworthiness of our findings. The fact that 2 IP researchers immersed themselves in the data and engaged in regular peer debriefings with an expert qualitative researcher and other members of the research team supports the credibility of the findings. Purposeful sampling of informants from hospitals of various sizes, in different regions, and with a range of HAI rates enhances the transferability of the findings. The use of thick verbatim description allows readers to determine how well the findings fit into their own specific contexts. We did not conduct member checks with informants because of the passage of time between interviews; however, peer review by IPs diminishes concerns about lack of credibility.
Our findings support the relevancy of the Association for Professionals in Infection Control and Epidemiology (APIC) Strategic Plan 2020.22 Two goals in particular, if achieved, would lessen some of the tensions identified by IPs in our study: the implementation science goal and the data standardization goal. APIC’s support for implementation science will generate findings that inform IPs about what mechanisms of influence are most effective for improving clinical practices. This will enable IPs to divest themselves of unrealistic or unproductive role assumptions and invest only in personal interactions, data feedback, or educational strategies that are proven effective. For example, the assumption expressed by IPs in the study that simply educating staff about an HAI policy is sufficient to change behavior is concerning because growing evidence supports a systems approach toward adherence issues. Implementation research will clarify the most productive approaches to behavioral change. APIC’s promotion of standardized, quality HAI data and interoperable electronic medical records will allow IPs to streamline surveillance processes and to achieve a better balance of resources with responsibilities. Our findings also support the applicability of the APIC Competency Model, which illustrates the competencies individual IPs should pursue as they advance in their careers.5 The need for ongoing competency in the leadership domain in particular is reflected in our informants’ narratives about shifting boundaries. To lead improvement efforts in which the outcomes are everyone’s responsibility, while maintaining a sense of personal pride in their unique expertise, IPs must hone their skills in collaboration, program management, and communication.
In conclusion, the results of this study utilizing careful content analysis and thick verbatim description clarify the evolving role of the IP and provide insights into the tensions experienced by IPs as they adapt their practice to meet the growing demands for quality and accountability in health care.
Acknowledgments
This research was supported by an award from the National Institute of Nursing Research (R01NR010107, PI: P.W.S.). L.J.C. is supported by a pre-doctoral fellowship from the National Institute of Nursing Research (T32 NR013454 Training in Interdisciplinary Research to Prevent Infections [TIRI] Codirectors: Larson and Saiman; to L.J.C.).
The authors thank Yoko Furuya, MD, and Shanelle Nelson, PhD, for their contribution to data collection and all of the participating hospitals.
Footnotes
The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Nursing Research or the National Institutes of Health.
Conflicts of interest: None to report.
References
- 1.Haley RW, Culver DH, White JW, Morgan WM, Emori TG, Munn VP, et al. The efficacy of infection surveillance and control programs in preventing nosocomial infections in US hospitals. Am J Epidemiol. 1985;121:182–205. doi: 10.1093/oxfordjournals.aje.a113990. [DOI] [PubMed] [Google Scholar]
- 2.Scheckler WE, Brimhall D, Buck AS, Farr BM, Friedman C, Garibaldi RA, et al. Requirements for infrastructure and essential activities of infection control and epidemiology in hospitals: a consensus panel report. Society for Healthcare Epidemiology of America. Infect Control Hosp Epidemiol. 1998;19:114–24. doi: 10.1086/647779. [DOI] [PubMed] [Google Scholar]
- 3.Goldrick BA. The practice of infection control and applied epidemiology: a historical perspective. Am J Infect Control. 2005;33:493–500. doi: 10.1016/j.ajic.2005.04.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murphy DM. From expert data collectors to interventionists: changing the focus for infection control professionals. Am J Infect Control. 2002;30:120–32. doi: 10.1067/mic.2002.120526. [DOI] [PubMed] [Google Scholar]
- 5.Murphy DM, Hanchett M, Olmsted RN, Farber MR, Lee TB, Haas JP, et al. Competency in infection prevention: a conceptual approach to guide current and future practice. Am J Infect Control. 2012;40:296–303. doi: 10.1016/j.ajic.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 6.Feltovich F, Fabrey LJ. The current practice of infection prevention as demonstrated by the practice analysis survey of the Certification Board of Infection Control and Epidemiology, Inc. Am J Infect Control. 2010;38:784–8. doi: 10.1016/j.ajic.2010.05.020. [DOI] [PubMed] [Google Scholar]
- 7.Curchoe R, Fabrey L, LeBlanc M. The changing role of infection prevention practice as documented by the Certification Board of Infection Control and Epidemiology practice analysis survey. Am J Infect Control. 2008;36:241–9. doi: 10.1016/j.ajic.2007.10.010. [DOI] [PubMed] [Google Scholar]
- 8.Stone PW, Dick A, Pogorzelska M, Horan TC, Furuya EY, Larson E. Staffing and structure of infection prevention and control programs. Am J Infect Control. 2009;37:351–7. doi: 10.1016/j.ajic.2008.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.O’Boyle C, Jackson M, Henly SJ. Staffing requirements for infection control programs in US health care facilities: Delphi project. Am J Infect Control. 2002;30:321–33. doi: 10.1067/mic.2002.127930. [DOI] [PubMed] [Google Scholar]
- 10.Sinkowitz-Cochran RL, Garcia-Williams A, Hackbarth AD, Zell B, Baker GR, McCannon CJ, et al. Evaluation of organizational culture among different levels of healthcare staff participating in the Institute for Healthcare Improvement’s 100,000 Lives Campaign. Infect Control Hosp Epidemiol. 2012;33:135–43. doi: 10.1086/663712. [DOI] [PubMed] [Google Scholar]
- 11.Olson CA, Tooman TR, Alvarado CJ. Knowledge systems, health care teams, and clinical practice: a study of successful change. Adv Health Sci Educ Theory Pract. 2010;15:491–516. doi: 10.1007/s10459-009-9214-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Krein SL, Damschroder LJ, Kowalski CP, Forman J, Hofer TP, Saint S. The influence of organizational context on quality improvement and patient safety efforts in infection prevention: a multi-center qualitative study. Soc Sci Med. 2010;71:1692–701. doi: 10.1016/j.socscimed.2010.07.041. [DOI] [PubMed] [Google Scholar]
- 13.Saint S, Kowalski CP, Banaszak-Holl J, Forman J, Damschroder L, Krein SL. The importance of leadership in preventing healthcare-associated infection: results of a multisite qualitative study. Infect Control Hosp Epidemiol. 2010;31:901–7. doi: 10.1086/655459. [DOI] [PubMed] [Google Scholar]
- 14.Damschroder LJ, Banaszak-Holl J, Kowalski CP, Forman J, Saint S, Krein SL. The role of the champion in infection prevention: results from a multisite qualitative study. Qual Saf Health Care. 2009;18:434–40. doi: 10.1136/qshc.2009.034199. [DOI] [PubMed] [Google Scholar]
- 15.Gurses AP, Seidl KL, Vaidya V, Bochicchio G, Harris AD, Hebden J, et al. Systems ambiguity and guideline compliance: a qualitative study of how intensive care units follow evidence-based guidelines to reduce healthcare-associated infections. Qual Saf Health Care. 2008;17:351–9. doi: 10.1136/qshc.2006.021709. [DOI] [PubMed] [Google Scholar]
- 16.Umscheid CA, Mitchell MD, Doshi JA, Agarwal R, Williams K, Brennan PJ. Estimating the proportion of healthcare-associated infections that are reasonably preventable and the related mortality and costs. Infect Control Hosp Epidemiol. 2011;32:101–14. doi: 10.1086/657912. [DOI] [PubMed] [Google Scholar]
- 17.Furuya EY, Dick A, Perencevich EN, Pogorzelska M, Goldmann D, Stone PW. Central line bundle implementation in US intensive care units and impact on bloodstream infections. PLoS ONE. 2011;6:e15452. doi: 10.1371/journal.pone.0015452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pogorzelska M, Stone PW, Furuya EY, Perencevich EN, Larson EL, Goldmann D, et al. Impact of the ventilator bundle on ventilator-associated pneumonia in intensive care unit. Int J Qual Health Care. 2011;23:538–44. doi: 10.1093/intqhc/mzr049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sandelowski M. Whatever happened to qualitative description? Res Nurs Health. 2000;23:334–40. doi: 10.1002/1098-240x(200008)23:4<334::aid-nur9>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 20.Forman J, Creswell JW, Damschroder L, Kowalski CP, Krein SL. Qualitative research methods: key features and insights gained from use in infection prevention research. Am J Infect Control. 2008;36:764–71. doi: 10.1016/j.ajic.2008.03.010. [DOI] [PubMed] [Google Scholar]
- 21.Uchida M, Stone PW, Conway LJ, Pogorzelska M, Larson EL, Raveis VH. Exploring infection prevention: policy implications from a qualitative study. Policy Polit Nurs Pract. 2011;12:82–9. doi: 10.1177/1527154411417721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.APIC Board of Directors. APIC Strategic Plan 2020. Am J Infect Control. 2012;40:291–3. doi: 10.1016/j.ajic.2012.03.003. [DOI] [PubMed] [Google Scholar]