Abstract
Background
We can conserve cultural heritage and gain extensive knowledge of plant species with pharmacological potential to cure simple to life-threatening diseases by studying the use of plants in indigenous communities. Therefore, it is important to conduct ethnobotanical studies in indigenous communities and to validate the reported uses of plants by comparing ethnobotanical studies with phytochemical and pharmacological studies.
Materials and methods
This study was conducted in a Tamang community dwelling in the Makawanpur district of central Nepal. We used semi-structured and structured questionnaires during interviews to collect information. We compared use reports with available phytochemical and pharmacological studies for validation.
Results
A total of 161 plant species belonging to 86 families and 144 genera to cure 89 human ailments were documented. Although 68 plant species were cited as medicinal in previous studies, 55 different uses described by the Tamang people were not found in any of the compared studies. Traditional uses for 60 plant species were consistent with pharmacological and phytochemical studies.
Conclusions
The Tamang people in Makawanpur are rich in ethnopharmacological understanding. The present study highlights important medicinal plant species by validating their traditional uses. Different plant species can improve local economies through proper harvesting, adequate management and development of modern techniques to maximize their use.
Keywords: Makawanpur district, Medicinal plants, Pharmacology, Phytochemistry, Tamang community
Background
Plants have been used for human benefit from time immemorial [1]. In the developing world, 70–80% of the population relies on plants for primary health care [2]. The use of plants as medicine is slowly increasing in the developed world [3] because they have minor or no side effects [4]. Although there is wide use of herbal medicine, traditional knowledge of the use of medicinal plants is influenced by rapid urbanization, migration, climate change, and the increasing number of modern healthcare systems throughout the world, including in Nepal [5-10]. The traditional use of plants by indigenous communities reflects the cultural aspects as well as biodynamic elements that have immense pharmacological potential to cure many diseases [11,12]. The documentation of traditional knowledge aids in the preservation of indigenous culture, identifies threatened species and contributes to the conservation and management of plant diversity [13,14]. The cultural and biological diversity of Nepal offers immense opportunities for ethnobotanical studies [7,15-17]. In Nepali traditional medicine, more than 2300 plant species [18] are used by 125 caste/ethnic communities speaking approximately 123 different languages [19].
In addition to documenting the traditional knowledge related to medicinal plants, scientific validation of traditional medicinal plants has been an important path of recent research [20]. Validation is performed by in-vitro[21-23] or in-vivo experiments [24-26] or by isolation of important secondary metabolites that are useful for treating particular types of diseases or disorders [21,27]. In addition, previously published studies can also aid in establishing links between traditional uses and modern scientific knowledge [20,28-31]. The practice of seeking evidence helps in identifying important medicinal plants and may also lead to the development of new or important pharmaceutical drugs [32] with future bioprospecting potential [33,34].
Many ethnopharmacological studies have been conducted in Nepal [15,35-37]; however, many parts of the country and communities remain unexplored. One of the unexplored communities is the Tamang community of the Makawanpur district, which constitutes 47.3% of the total district population [19]. In Nepal, the Tamang community is the fifth largest community, with 5.6% of the total population of the country [19], who mostly live in mountainous or hilly regions [35]. The Makawanpur district is one of the major Tamang dwelling areas in the hilly region of Nepal. Few ethnobotanical studies have been conducted in this district [38-48], although a considerable number of ethnobotanical studies relating to the Tamang community have been conducted in different parts of Nepal [20,22,49-57]. Previous studies in different parts of Nepal have revealed that the Tamang people have a unique culture and a rich traditional knowledge [20,35,55]. However, ethnopharmacological studies specifically targeting the Tamang community of the Makawanpur district are lacking, as are the validation of traditional uses. Therefore, in the present study, we aimed to document indigenous knowledge of the use of medicinal plants in the Tamang community of the Makawanpur district. We hypothesized that the Tamang people in Makawanpur have specialized knowledge of the use of plants, and a wealth of information on a wide range of medicinal plants is expected from the district because the Makawanpur district is located in an area that is rich in biodiversity. We also expected that the Tamang people use different species or known species for different diseases than previously reported because they form part of a distinct ethnic group with a unique identity. Our specific objectives were to address the following questions: (i) Which plant species are used against different diseases by the Tamang people in the Makawanpur district? (ii) What are the modes of preparation and administration of traditional herbal medicines? (iii) Is there any pharmacological or phytochemical evidence for the traditional uses?
Methods
Study area
The study areas included the Hadigaun, Aambhanjyang and Tistung village development committees (VDCs) (Figure 1). Study areas were selected based on a large Tamang population residing in the area compared with the population of other communities. Field visits were conducted in March 2011 and May 2011 because it is the peak time for plant growth. The duration of one field visit at a site ranged from 4 to 10 days.
Figure 1.
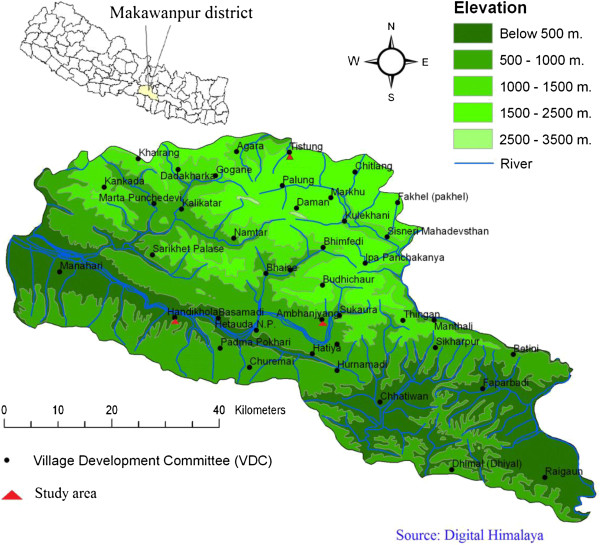
Map Makawanpur district showing study area.
The total number of households in Hadigaun was 3155, with 8900 males and 8970 females. The total number of households in Aambhanjyang was 1519, with 4251 males and 4279 females, and the total number of households in Tistung was 1190, with 3293 males and 3293 females [19]. The types of vegetation differed between sites. In Hadikhola (200–1000 m asl), tropical forest is present, with Shorea robusta as the dominant species and common associates of Terminalia alata, Adina cordifolia, Anogeisus latifolia, Lagerstroemia parviflora, Dillenia pentagyna, Syzygium cumini, and Semicarpus anacardium. There was an Acacia catechu-Dalbergia sissoo community along streams and rivers and a tropical deciduous riverine forest with Bombax ceiba, Holoptelea integrifolia, and Trewia nudiflora together with other species in the Shorea robusta forest. In Aambhanjyang (550–1680 m asl), there was subtropical forest with the remains of a Shorea robusta forest at lower elevations, and a Schima-Castanopsis forest at higher elevations. Schima wallichii occurs throughout, with Castanopsis indica more common below 1200 m, and Castanopsis tribuloides above this elevation. At higher elevations, there was riverine forest with Toona, and Albizzia species. This forest occurs in narrow strips along streams and is mixed in composition, with Toona ciliata, Albizzia mollis, and Pandanus nepalensis. In Tistung (1500–2500 m asl), there were pure stands of Pinus roxburgii characterized as lower temperate forest type.
Data collection
Prior to data collection, the objectives of the study were discussed by organizing a group meeting with local people, teachers, elderly men and women from each VDC. Verbal consent was obtained from the participants, and data were collected in a manner similar to other studies in Nepal [58,59].
The participants were chosen to represent both genders and all age groups. We used semi-structured questionnaires in groups in each study area, and questions aimed to collect information on the types of diseases and presence of plant species and their uses. Thirty people in Hadigaun, 17 in Aambhanjyang and 10 in Tistung area participated in the study, of which 22 were women, primarily housewives aged 25–60 years, and 35 were men 40–79 years old (Additional file 1: Table S1). We also conducted separate in-depth interviews with four local healers using structured questionnaires targeting the specific uses of each plant species. The local healers who participated in in-depth interviews included Saila Syantang (70 years old) in Tistung, Lal Bahadhur Thing (68 years old) and Bir Bahadhur Parja (70 years old) in Hadikhola, and Chandra Bahadhur Syantang (50 years old) in the Ambhanjyang VDCs. In addition, we also collected information on veterinary use. The information collected through non-structured questionnaires and structured questionnaires was summarized into a single table providing all plant names, and their uses. The final table included information on vernacular names, life forms, growth, local status, growth ranges, sources, parts used, preparation, administration, and uses. We also included information regarding published studies that cite uses similar to those reported by the Tamang people from the Makawanpur district.
Plant collection and exhibition of plant species were performed during the group or individual interviews. We also asked local people to show plant species obtained outside the Makawanpur district. Most of the collected plants were identified in the field using flora books [60-62]. The identified species were photographed for further references, and unidentified species were preserved as herbarium specimens. The unidentified plant specimens were stored between paper sheets in an herbarium press, and tightened to prevent distortion of the plant. The paper sheets were changed every day for at least three days. The tightly packed herbarium press was kept in sunlight during the daytime to allow evaporation of the moisture to dry the plant specimen, and to prevent infection with fungi using this natural drying technique [63]. The plants were later identified using the same flora books described above and also by comparison with herbarium specimens deposited at the National Herbarium and Plant Laboratories (KATH), Godawari, Lalitpur, Nepal. All specimens collected were deposited at KATH. We followed the nomenclature of Press et al. (2000) [64].
Comparing traditional knowledge
The uses of plant species described by the Tamang people in the Makawanpur district were compared with several studies related to the Makawanpur district [38-43,45-48] and Tamang communities from different parts of Nepal [20,22,49-57,65]. We also consulted several books that described medicinal plants throughout Nepal. These books were the outcome of studies conducted in different parts of Nepal [35,66] or specific regions [67] or review books on medicinal plants [15,36,68]. We also consulted recent studies that were not included in the books described above [7,17,20,29,30,47,59,69-72]. The pharmacological studies included tests of crude or purified plant extracts against a particular type of microbe or disease. Phytochemical studies included isolation of compound(s), and such compounds were sometimes tested against microbes or diseases. To identify the studies, we searched for relevant literature on plant species in different electronic databases (ISI Web of Science, MEDLINE, Science Direct, Scopus, and Google Scholar) and by searching masters and Ph. D. dissertations at Tribhuvan University Central Library, Kirtipur, Nepal.
Results
Medicinal plant diversity, and uses
The present survey found 161 plant species belonging to 86 families and 144 genera that are used to cure 89 human ailments by the Tamang people in the Makawanpur district (Additional file 2: Table S2). Angiosperms constituted the highest number of plants species (132 dicotyledones, and 18 monocotyledones) followed by pteridophytes (6), gymnosperms (3), and mushrooms (1). Herbs were the major sources of medicine (45%), followed by trees (33%), and shrubs (23%).
The highest number of plant species was used for gastrointestinal-related diseases followed by cuts and wounds, and fever. Thirty-five plant species were used for other categories (antidotes, improved lactation, cooling agents, tonics, and for religious purposes) (Figure 2).
Figure 2.
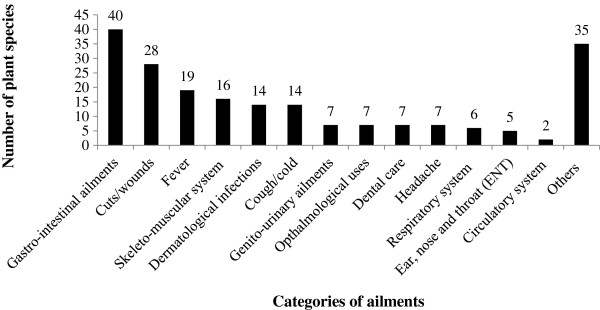
Use frequency of plant species in different disease categories by Tamang community in Makawanpur district. The plant species might have repeated for each disease category.
Some of the plants were edible and were also used as food (Dryoathyrium boryanum, Musa paradisiaca, Myrica esculenta, Psidium guajava, and Rubus ellipticus). Wide varieties of trees or shrubs were major sources of fuel or sometimes timber for daily uses (e.g., construction, and making wooden tools such as ploughs). Other species were used for religious purposes (e.g., Shorea robusta, Pinus roxburghii, and Pinus wallichiana).
Parts, preparation, modes of use, and harvesting
The plant parts used for various types of ailments included the underground parts (roots, rhizomes, bulbs, and tubers), young shoots, stems, bark and wood, leaves and petioles, flowers, fruits and seeds, resins, and the whole plant. The most frequently used plant parts were fruits and seeds (for 51 different plant species), followed by leaves and petioles (37 plant species). The whole plant was also frequently used (38 plant species) (Figure 3).
Figure 3.
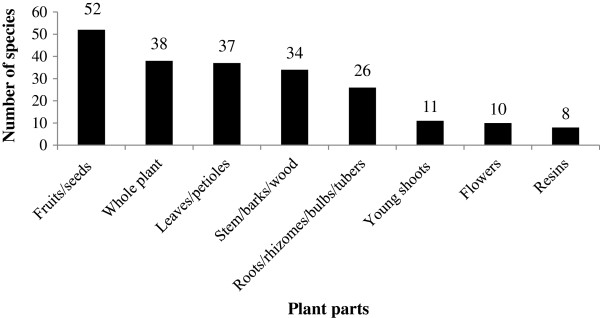
Use frequency of different plant parts by Tamang community in Makawanpur district.
The plants were used in various forms for different ailments. The most frequently used form was powder, followed by paste, and juice. Many species were also used as medicine in a raw form (Figure 4). The primary mode of administration of medicine to cure different ailments was oral (56.47%), followed by external or topical application (40.59%). Three species were used as a toothbrush (Hedera nepalensis, Prunus cornuta, and Smilax zeylanica). Vitex negundo was used by fuming and administered through the nasal passage. Drymaria diandra was mixed with water for steam therapy.
Figure 4.
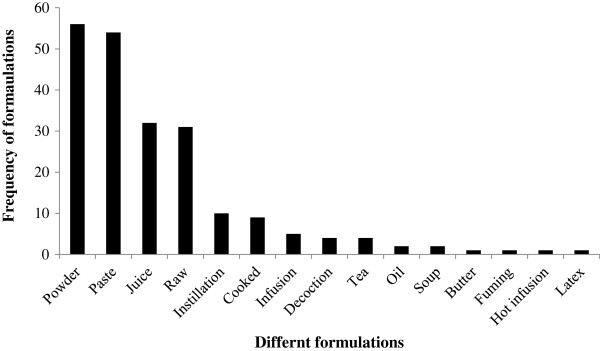
Use frequency of different formulations used adopted by Tamang community in Makawanpur district.
Plant species were primarily harvested from the wild (147 plant species), and only a few species were cultivated (14 plant species) (Additional file 2: Table S2). Plants were generally collected as per local needs without any rules, and regulations. Four species (Malus sylvestris, Nardostachys grandiflora, Pycnoporus cinnabarinus, and Valeriana jatamansii) were obtained from the Rasuwa district, and one species from its only habitat in western Nepal (Pterocarpus marsupium) (Additional file 2: Table S2).
Differences between respondents
During the interviews, we found that elderly people were most familiar with the various types of medicinal plant species. The majority of the participants knew plants used for common ailments such as stomach problems, cough, and cold. When comparing males and females, females were better at identifying plant species than males because they regularly visit forests for firewood or fodder collection. The majority of young people were not familiar with plant species, and their uses. The local healers participated and described the uses of the plants but were reluctant to share their full indigenous knowledge on the uses of plants, and did not reveal the detailed doses of administration. Most of the people reported that traditional knowledge was passed through verbal communication, and repeated practice. The healers reported that knowledge of the use of plants was passed to one of their family members without revealing this knowledge to the others.
Veterinary medicines
There were 14 plant species belonging to 14 families used for veterinary diseases. Most of these plants were given as the whole plant by oral administration, and a few were used topically. The plants were used for a wide variety of diseases, such as diarrhea, wounds, infections, and foot-and-mouth disease (Table 1).
Table 1.
Veterinary uses of medicinal plants in Makawanpur area
| Scientific Names | Administration | Uses |
|---|---|---|
|
Asparagus racemosus Willd. |
Oral |
Better milk production |
|
Auricularia polytricha (Mont.) Sacc. |
Oral |
Dyspepsia |
|
Bauhinia malabarica Roxb. |
Topical |
Wounds in neck |
|
Cannabis sativa L. |
Oral |
Diarrhea |
|
Cissampelos pareira L. |
Oral |
To kill tapeworm |
|
Coriandrum sativum L. |
Oral |
Better milk production |
|
Didymocarpus albicalyx C. B. Clarke |
Oral |
Energies the weak animals |
|
Elephantopus scaber L. |
Oral/Topical |
Sex stimulants in female animals |
|
Lindera neesiana (Wall. ex Nees) Kurz |
Oral |
Diarrhea |
|
Mangifera indica L. |
Topical |
Eye problems |
|
Persicaria chinensis (L.) H. Gross |
Oral |
Diuretic |
|
Viscum album L. |
Oral/Topical |
Wide ranges of diseases especially for buffalos |
|
Zanthoxylum oxyphyllum Edgew. |
Topical |
To kill lice and teaks |
| Zingiber officinale Rosc. | Oral/Topical | Foot mouth diseases and other communicable diseases |
Comparison of reported uses
From a literature comparison, we found that there were similar use reports for 93 plant species used against 64 different ailments in various studies. Although 68 plant species were described as medicinal in various studies, 55 different uses by the Tamang people were not found in any of the literature compared. Moreover, five plant species (Gaultheria hookeri, Malvaviscus arboreus, Osmanthus suavis, Sambucus hookeri, and Schoenoplectus juncoides) were not found as medicinal plant species in any of the studies we considered for comparison (Additional file 2: Table S2).
Pharmacological and phytochemical studies were found for 60 plant species (Additional file 3: Table S3). A comparison of Tamang use with pharmacological and phytochemical studies showed complete or partial consistency for 52 of 60 plant species. The studies for eight plant species (Astilbe rivularis, Citrus aurantifolia, Cucumis sativus, Eupatorium adenophorum, Pinus wallichiana, Rhododendron arboreum, Scutellaria repens and Valeriana jatamansii) were related to the isolation of different compounds, but the compounds had not been pharmacologically tested against the disease mentioned by Tamangs of Makawanpur (Additional file 3: Table S3).
Discussion
Traditional uses of medicinal plants by the Tamang people in Makawanpur
In the present study, we reported 161 plant species that are used by the Tamang people in the Makawanpur district as medicine. The number of reported medicinal plant species is higher than in studies carried out in the Chepang community [45], in various communities [40], in the Daman area in the Makawanpur district [46], and in the Tamang community in the Rasuwa district [20] in Nepal. This observation shows that the Tamang people in the Makawanpur district have extensive knowledge of how to use plants as medicine against different diseases. The dominance of herbs followed by trees, and shrubs is consistent with the different studies from Nepal [7,17,18,20]. The preference for herbs over other forms may be because herbs are more abundant [7], and more easily collected and transported [20].
The most frequently cured disease category was gastrointestinal diseases. Similar to other rural communities, the prevalence of gastrointestinal diseases in the Tamang community is due to poor sanitation, and contaminated drinking water [73]. The plants are used as food, timber and fuel, and also as veterinary medicine in the Makawanpur district, demonstrating that the residents fulfill different requirements from plants as reported in various previous studies [15,35,36].
Fruits and seeds, and leaves and petioles are most frequently used because they are easily available. The preference for fruits and seeds or leaves and petioles for primary health care shows that indigenous knowledge is quite specialized because these parts contain high concentrations of bioactive compounds [74], comparable to underground plant parts [75,76].
Comparison of reported uses
Although 93 plant species showed similar uses with other studies from different parts of Nepal (Additional file 2: Table S2), we found pharmacological or phytochemical studies for only 60 of these plant species (Additional file 3: Table S3). These 52 medicinal plant species have good bioprospecting potential because they are scientifically proven to be important in cures for different diseases, which demonstrates that the Tamang people in the Makawanpur area have reliable knowledge on the use of plants for their primary health care.
When looking across the different studies, we found that uses for five different plant species were not exactly the same as previously reported, but the previously reported uses were similar. For example, we reported that Aconitum ferox was used for toothache, and was described as an analgesic in other studies [15,68]. Amaranthus spinosus, which is used against skin diseases in Makawanpur, is reported as being used for wounds [38], to remove pus in boils and for various skin problems such as boils, burns, pimples, and eczema [35]. Likewise, Artemisia indica, which is reported to be used for scabies, was previously reported as being used for bathing children [47], lacerations [20] or against wounds or ringworm [35]. Cassia fistula, used for digestion problems in the studied area, was previously reported as a laxative or appetite stimulant in Nepal [35,43]. Cinnamomum tamala, reported to be beneficial for digestion, was previously described as a carminative [15] or used for diarrhea [35].
Given that we have revealed previously unreported uses for 68 of 161 species, it is important to have explicit documentation of the use of plants in different parts of Nepal so that the valuable but disappearing traditional knowledge will be preserved. Further investigation of plant species related to pharmacological and phytochemical studies may lead to the discovery of new bioactive compounds for treating life-threatening illnesses [77,78].
Harvesting and sustainable management of medicinal plants
Harvesting of plant species from the wild is a common trend worldwide [79-81]. Seven of the species used by the Tamang people in Makawanpur are protected [82], including Acacia catechu, Bombax ceiba, Juglans regia, Shorea robusta, and Taxus wallichiana. None of these plant species was traded outside the study area. However, many of these plant species (e.g., Acacia catechu, Acorus calamus, Asparagus racemosus and Paris polyphylla) possess the potential to boost the economy in the future [83]. The use of plants from the wild in these regions demonstrates that medicinal plants face the long-term danger of depletion, and therefore, their cultivation should be initiated to save this component of biodiversity, and maintain the existing ecosystems. In addition, populations of many medicinal plant species are often reduced by deforestation, habitat encroachment, shifting cultivation, forest fires, grazing, and other anthropogenic activities. Therefore, cultivation techniques for several medicinal plant species are currently being tested at Daman Botanical Garden and Tistung Botanical Garden (e.g., Acorus calamus, Amomum subulatum, Asparagus racemosus, Astible rivularis, Berginia ciliata, Lobelia pyrimidalis, and Mentha piperata) by the Department of Plant Resources under the Ministry of Forest and Soil Conservation, Nepal. Knowledge of the cultivation techniques required should be transferred to the local farmers in the study area.
Conclusions
The Tamang community in the Makawanpur district has rich indigenous knowledge of the use of medicinal plants to maintain their primary health. Traditional herbal remedies are important and effective in the Tamang community because many traditional uses are scientifically proven through phytochemical and pharmacological studies. However, a large number of plant species remain untested for bio-efficacy and toxicity. Such tests may reveal novel remedies that have bioprospecting potential. Most of the plant species are harvested in the wild; the practice of cultivation and domestication of at least the most rare and most highly used plant species is needed for sustainability.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
DL carried out field research. MR supervised the work. DL, MR, BT and ZM analysed the data and wrote the manuscript. All authors approved the final version of the manuscript.
Supplementary Material
Details of informants interviewed in Hadigaun, Aambhanjyang and Tistung village development committees of Makawanpur district.
Medicinal plants used by Tamang community in Makawanpur district, central Nepal [38,84-93].
Comparison of local use and phytochemical and pharmacological studies of medicinal plants [94-186].
Contributor Information
Dol Raj Luitel, Email: luiteldr2@gmail.com.
Maan B Rokaya, Email: rokayamaan@gmail.com.
Binu Timsina, Email: binu.timsina@gmail.com.
Zuzana Münzbergová, Email: zuzmun@natur.cuni.cz.
Acknowledgements
We are thankful to the local people who shared their knowledge on uses of plants. The study was supported by GAČR 13-10850P and partly by institutional support RVO 67985939. This work was also partly supported by the grant No. CZ.1.05/1.1.00/02.0073 of the MSMT.
References
- Sumner J. The Natural History of Medicinal Plants. 1. Portland, Oregon, USA: Timber Press; 2000. [Google Scholar]
- Traditional Medicine: Fact Sheet 34. [ http://www.who.int/inf-fs/en/fact134.html] (accessed on 28 2013)
- Bernal J, Mendiola JA, Ibáñez E, Cifuentes A. Advanced analysis of nutraceuticals. J Pharm Biomed Anal. 2011;55:758–774. doi: 10.1016/j.jpba.2010.11.033. [DOI] [PubMed] [Google Scholar]
- Jordan SA, Cunningham DG, Marles RJ. Assessment of herbal medicinal products: Challenges, and opportunities to increase the knowledge base for safety assessment. Toxicol Appl Pharmacol. 2010;243:198–216. doi: 10.1016/j.taap.2009.12.005. [DOI] [PubMed] [Google Scholar]
- Abdullahi AA. Trends and challenges of traditional medicine in Africa. Afr J Tradit Complement Altern Med. 2011;8(5 Suppl):115–123. doi: 10.4314/ajtcam.v8i5S.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinlan MB, Quinlan RJ. Modernization and medicinal plant knowledge in a Caribbean horticultural village. Med Anthropol Q. 2007;21:169–192. doi: 10.1525/maq.2007.21.2.169. [DOI] [PubMed] [Google Scholar]
- Rokaya MB, Münzbergová Z, Timsina B. Ethnobotanical study of medicinal plants from the Humla district of western Nepal. J Ethnopharmacol. 2010;130:485–504. doi: 10.1016/j.jep.2010.05.036. [DOI] [PubMed] [Google Scholar]
- Shanley P, Luz L. The impacts of forest degradation on medicinal plant use and implications for health care in eastern Amazonia. BioScience. 2003;53:573–584. doi: 10.1641/0006-3568(2003)053[0573:TIOFDO]2.0.CO;2. [DOI] [Google Scholar]
- Telwala Y, Brook BW, Manish K, Pandit MK. Climate-induced elevational range shifts and increase in plant Species richness in a Himalayan biodiversity epicentre. PLoS ONE. 2013;8:e57103. doi: 10.1371/journal.pone.0057103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teshome-Bahiru W. Impacts of urbanisation on the traditional medicine of Ethiopia. Anthropologist. 2005;8:43–52. [Google Scholar]
- Cox PA, Balick MJ. The ethnobotanical approach to drug discovery. Sci Am. 1994;270:82–87. [PubMed] [Google Scholar]
- Etkin NL. Anthropological methods in ethnopharmacology. J Ethnopharmacol. 1993;38:93–104. doi: 10.1016/0378-8741(93)90004-O. [DOI] [PubMed] [Google Scholar]
- Berkes F, Colding J, Folke C. Rediscovery of traditional ecological knowledge as adaptive management. Ecol Appl. 2000;10:1251–1262. doi: 10.1890/1051-0761(2000)010[1251:ROTEKA]2.0.CO;2. [DOI] [Google Scholar]
- Watson A, Alessa L, Glaspell B. The relationship between traditional ecological knowledge, evolving cultures, and wilderness protection in the circumpolar north. Conserv Ecol. 2003;8:2. [Google Scholar]
- Baral SR, Kurmi PP. A Compendium of Medicinal Plants in Nepal. Kathmandu, Nepal: Rachana Sharma; 2006. [Google Scholar]
- Rijal A. Living knowledge of the healing plants: Ethno-phytotherapy in the Chepang communities from the Mid-Hills of Nepal. J Ethnobiol Ethnomedicine. 2008;4:23. doi: 10.1186/1746-4269-4-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrestha PM, Dhillion SS. Medicinal plant diversity and use in the highlands of Dolakha district, Nepal. J Ethnopharmacol. 2003;86:81–96. doi: 10.1016/S0378-8741(03)00051-5. [DOI] [PubMed] [Google Scholar]
- Rokaya MB, Münzbergová Z, Shrestha MR, Timsina B. Distribution patterns of medicinal plants along an elevational gradient in central Himalaya, Nepal. J Mt Sci. 2012;9:201–213. doi: 10.1007/s11629-012-2144-9. [DOI] [Google Scholar]
- CBS. National Population and Housing Census 2011 (National Report) Kathmandu, Nepal: Central Bureau of Statistics, Government of Nepal; 2012. [Google Scholar]
- Uprety Y, Asselin H, Boon EK, Yadav S, Shrestha KK. Indigenous use and bio-efficacy of medicinal plants in the Rasuwa District, Central Nepal. J Ethnobiol Ethnomedicine. 2010;6:3. doi: 10.1186/1746-4269-6-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krenn L, Presser A, Pradhan R, Bahr B, Paper DH, Mayer KK, Kopp B. Sulfemodin 8-O-beta-D-glucoside, a new sulfated anthraquinone glycoside, and antioxidant phenolic compounds from Rheum emodi. J Nat Prod. 2003;66:1107–1109. doi: 10.1021/np0301442. [DOI] [PubMed] [Google Scholar]
- Taylor RSL, Edel F, Manandhar NP, Towers GHN. Antimicrobial activities of southern Nepalese medicinal plants. J Ethnopharmacol. 1996;50:97–102. doi: 10.1016/0378-8741(95)01335-0. [DOI] [PubMed] [Google Scholar]
- Taylor RSL, Manandhar NP, Towers GHN. Screening of selected medicinal plants of Nepal for antimicrobial activities. J Ethnopharmacol. 1995;46:153–159. doi: 10.1016/0378-8741(95)01242-6. [DOI] [PubMed] [Google Scholar]
- Adzu B, Tarfa F, Amos S, Gamaniel KS. The efficacy of Sphaeranthus senegalensis Vaill extract against diarrhoea in rats. J Ethnopharmacol. 2004;95:173–176. doi: 10.1016/j.jep.2004.06.036. [DOI] [PubMed] [Google Scholar]
- Alam MMA, Javed K, Jafri MA. Effect of Rheum emodi (Revand Hindi) on renal functions in rats. J Ethnopharmacol. 2005;96:121–125. doi: 10.1016/j.jep.2004.08.028. [DOI] [PubMed] [Google Scholar]
- Arunachalam K, Parimelazhagan T. Antidiabetic activity of Ficus amplissima Smith. bark extract in streptozotocin induced diabetic rats. J Ethnopharmacol. 2013;147:302–310. doi: 10.1016/j.jep.2013.03.004. [DOI] [PubMed] [Google Scholar]
- Rokaya MB, Maršík P, Münzbergová Z. Active constituents in Rheum acuminatum and Rheum australe (Polygonaceae) roots: A variation between cultivated and naturally growing plants. Biochem Syst Ecol. 2012;41:83–90. [Google Scholar]
- Gaire BP, Subedi L. Medicinal plant diversity and their pharmacological aspects of Nepal Himalayas. Pharmacogn J. 2011;2:6–17. [Google Scholar]
- Kunwar RM, Burlakoti C, Chowdhary C, Bussman R. Medicinal plants in western Nepal: Indigenous uses and pharmacological validity. Med Aromat Plant Sci Biotechnol. 2010;4:28–42. [Google Scholar]
- Kunwar RM, Shrestha KP, Bussmann RW. Traditional herbal medicine in Far-west Nepal: a pharmacological appraisal. J Ethnobiol Ethnomedicine. 2010;6:35. doi: 10.1186/1746-4269-6-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maroyi A. Traditional use of medicinal plants in south-central Zimbabwe: review and perspectives. J Ethnobiol Ethnomedicine. 2013;9:31. doi: 10.1186/1746-4269-9-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman DJ, Cragg GM. Natural products as sources of new drugs over the last 25 Years. J Nat Prod. 2007;70:461–477. doi: 10.1021/np068054v. [DOI] [PubMed] [Google Scholar]
- Douwes E, Crouch NR, Edwards TJ, Mulholland DA. Regression analyses of southern African ethnomedicinal plants: informing the targeted selection of bioprospecting and pharmacological screening subjects. J Ethnopharmacol. 2008;119:356–364. doi: 10.1016/j.jep.2008.07.040. [DOI] [PubMed] [Google Scholar]
- Soejarto DD, Fong HHS, Tan GT, Zhang HJ, Ma CY, Franzblau SG, Gyllenhaal C, Riley MC, Kadushin MR, Pezzuto JM, Xuan LT, Hiep NT, Hung NV, Vu BM, Loc PK, Dac LX, Binh LT, Chien NQ, Hai NV, Bich TQ, Cuong NM, Southavong B, Sydara K, Bouamanivong S, Ly HM, Thuy TV, Rose WC, Dietzman GR. Ethnobotany/ethnopharmacology and mass bioprospecting: Issues on intellectual property and benefit-sharing. J Ethnopharmacol. 2005;100:15–22. doi: 10.1016/j.jep.2005.05.031. [DOI] [PubMed] [Google Scholar]
- Manandhar NP. Plants and People of Nepal. Portland, Oregon, USA: Timber Press; 2002. [Google Scholar]
- Rajbhandari KR. Ethnobotany of Nepal. Kathmandu, Nepal: WWF Nepal Program; 2001. [Google Scholar]
- Shrestha KK, Tiwari NN, Rajbhandari S, Poudel RC, Uprety Y. Ethnobotany in Nepal: Review and Perspectives. Kathmandu, Nepal: WWF Nepal Program; 2004. [Google Scholar]
- Basnet B, Joshi R, Lekhak HD. In: Environ Agric Biodivers Agric Pollut South Asia. Jha PK, Baral SR, Karmacharya SB, Lekhak HD, Lacoul P, Baniya CB, editor. Kathmandu, Nepal: Ecological Society (ECOS); 2001. Ethnobotanical survey of Chepang tribe of Makawanpur district, Nepal; pp. 245–252. [Google Scholar]
- Bhattarai NK. Folk anthelmintic drugs of central Nepal. Pharm Biol. 1992;30:145–150. doi: 10.3109/13880209209053980. [DOI] [Google Scholar]
- Bhattarai NK. Folk herbal medicines of Makawanpur district, Nepal. Pharm Biol. 1991;29:284–295. doi: 10.3109/13880209109082899. [DOI] [Google Scholar]
- Hasan MK, Gatto P, Jha PK. Traditional uses of wild medicinal plants and their management practices in Nepal-A study in Makawanpur district. Int J Med Aromat Plants. 2013;3:102–112. [Google Scholar]
- Khan MH. In: Ethnobot Conserv Community Dev. Shrestha KK, Jha PK, Shengji P, Rastogi A, Rajbhandary S, Joshi M, editor. Kathmandu, Nepal: Ethnobotanical Society of Nepal; 1998. Documentation of indigenous knowledge in the Chepang community of Shakti Khor VDC, Chitawan; pp. 96–101. [Google Scholar]
- Manandhar NP. An inventory of some vegetable drug resources of Makawanpur District, Nepal. Fitoterapia. 1995;66:231–238. [Google Scholar]
- Manandhar NP. Folklore medicine of Chitwan district, Nepal. Ethnobotany. 1990;2:31–38. [Google Scholar]
- Manandhar NP. Medicinal plants used by Chepang tribes of Makawanpur District, Nepal. Fitoterapia. 1989;60:61–68. [Google Scholar]
- Pathak L, Pandey SR. Ethno-medicinal plants of Daman area, Central Nepal. Plant Resour Bull. 2005;26:30–32. [Google Scholar]
- Uprety Y, Boon E, Poudel RC. Traditional Use of Plant Resources by Bankariya Ethnic Group in Makawanpur District, Central Nepal. Germany: GRIN Verlag; 2008. [Google Scholar]
- Uprety Y, Poudel RC, Shrestha KK, Rajbhandary S, Tiwari NN, Shrestha UB, Asselin H. Diversity of use and local knowledge of wild edible plant resources in Nepal. J Ethnobiol Ethnomedicine. 2012;8:16. doi: 10.1186/1746-4269-8-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kharel S. Ethnomycological study on wild edible mushrooms of Bhardeo VDC, Lalitpur, Nepal. Kirtipur, Nepal: Central Department of Botany, Tribhuvan University; 1998. (M.Sc. Thesis). [Google Scholar]
- Manandhar NP. Medicinal plant-lore of Tamang tribe of Kabhrepalanchok district, Nepal. Econ Bot. 1991;45:58–71. doi: 10.1007/BF02860050. [DOI] [Google Scholar]
- Shrestha I, Shrestha K. Proceeding Nepal-Jpn Jt Symp Conserv Util Himal Med Resour. Kathmandu, Nepal: Ministry of Forest and Soil Conservation- HMG/N, Department of Plant Resources and Society for the Conservation and Development of Himalayan Medicinal Resources (SCDHMR), Japan; 2000. Ethno-medico-botanical studies of Langtang National Park, Nepal; pp. 178–181. [Google Scholar]
- Shrestha I, Inglis A, Shrestha K. Proceeding Int Semin Mt. Kathmandu, Nepal: Royal Nepal Academy of Science and Technology (RONAST); 2003. Documenting and mapping medicinal plants of Lantang National Park, central Nepal; pp. 361–371. [Google Scholar]
- Shrestha P. Proc Natl Conf Sci Technol April 24--29 1988 RONAST Katmandu. Royal Nepal Academy of Science and Technology (RONAST); 1989. Ethnobotanical observation on the Tamangs of Kathmandu valley; pp. 353–358. [Google Scholar]
- Shrestha P. Contribution to the ethnobotany of the Tamangs of Kathmandu valley. Cent Nepal Asian Stud. 1988;15:247–266. [Google Scholar]
- Tamang G. An Ethnobiological study of the Tamang people. Our Nat. 2003;1:37–41. [Google Scholar]
- Tamang G. Ethnobiology of Tamang Tribe (A case study of Gorsyang VDC) Kathmandu, Nepal: Central Department of Zoology, Tribhuvan University; 1998. (M.Sc. Thesis). [Google Scholar]
- Toffin G, Wiart J. Recherches surl’ethnobotanidue des Tamang dumassif du Ganesh Himal Nepal Central): Les plantes non cultivees. J Agric Trad Bota Appl. 1985;32:127–175. [Google Scholar]
- Kunwar RM, Mahat L, Acharya RP, Bussmann RW. Medicinal plants, traditional medicine, markets and management in far-west Nepal. J Ethnobiol Ethnomedicine. 2013;9:24. doi: 10.1186/1746-4269-9-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uprety Y, Poudel RC, Asselin H, Boon E. Plant biodiversity and ethnobotany inside the projected impact area of the Upper Seti Hydropower Project, Western Nepal. Environ Dev Sustain. 2011;13:463–492. doi: 10.1007/s10668-010-9271-7. [DOI] [Google Scholar]
- Polunin O, Stainton A. Flowers of the Himalaya. New Delhi, India: Oxford University Press; 1984. [Google Scholar]
- Stainton A. Flowers of the Himalaya: A Supplement. New Delhi, India: Oxford University Press; 1988. [Google Scholar]
- Storrs A, Storrs J. Trees and Shrubs of Nepal and the Himalayas. New Dehli, India: Books Faith India; 1998. [Google Scholar]
- Bridson DM, Forman L. The Herbarium Handbook. Kew: Royal Botanic Gardens; 1998. [Google Scholar]
- Press JR, Shrestha KK, Sutton DA. Annotated Checklist of the Flowering Plants of Nepal. Kathmandu: Natural History Museum, London and Central Department of Botany, Tribhuvan University; 2000. [Google Scholar]
- Mikage M. Field research on the medicinal plant researches around the Tamang Village, Kaski district, west Nepal. Newsl Himal Bot. 2000;27:1–5. [Google Scholar]
- Ghimire SK, Sapkota IB, Oli BR, Parajuli-Rai R. Non-Timber Forest Products of Nepal Himalaya: Database of Some Important Species Found in the Mountain Protected Areas and Surrounding Regions. 1. Kathmandu, Nepal: WWF; 2008. [Google Scholar]
- Lama YC, Ghimire SK, Aumeeruddy-Thomas Y. Medicinal Plants of Dolpo: Amchis’ Knowledge and Conservation. Kathmandu, Nepal: Worldwide Fund for Nature Conservation (WWF) Nepal; 2001. [Google Scholar]
- Joshi KK, Joshi SD. Genetic Heritage of Medicinal and Aromatic Plants of Nepal Himalayas. Kathmandu, Nepal: Buddha Academic Publications; 2001. [Google Scholar]
- Bhattarai K, Maren I, Chaudhary R. Medicinal plant knowledge of the Panchase region in the middle hills of the Nepalese Himalayas. Banko Janakari. 2011;21:31–39. [Google Scholar]
- Joshi A, Joshi K. Plant diversity and ethnobotanical notes on tree species of Syabru village, Langtang national park, Nepal. Ethnobot Leafl. 2009;13:651–664. [Google Scholar]
- Kunwar RM, Uprety Y, Burlakoti C, Chowdhary CL, Bussmann RW. Indigenous use and ethnopharmacology of medicinal plants in far-west Nepal. Ethnobot Res Appl. 2009;7:005–028. [Google Scholar]
- Shrestha KK, Ghimire SK. Plant Diversity Inventory of the Proposed Kanchunjunga Conservation Area (Ghunsa and Simbua Valley) Kathmandu, Nepal: WWF Nepal Program; 1996. [Google Scholar]
- Anonymous. People’s Perception on Sanitation: Findings from Nepal. GPO Box: 20214, Kathmandu, Nepal: WaterAid in Nepal; 2011. p. Vii+64. [Google Scholar]
- Harris CS, Burt AJ, Saleem A, Le PM, Martineau LC, Haddad PS, Bennett SAL, Arnason JT. A single HPLC-PAD-APCI/MS method for the quantitative comparison of phenolic compounds found in leaf, stem, root and fruit extracts of Vaccinium angustifolium. Phytochem Anal. 2007;18:161–169. doi: 10.1002/pca.970. [DOI] [PubMed] [Google Scholar]
- Giday M, Asfaw Z, Elmqvist T, Woldu Z. An ethnobotanical study of medicinal plants used by the Zay people in Ethiopia. J Ethnopharmacol. 2003;85:43–52. doi: 10.1016/S0378-8741(02)00359-8. [DOI] [PubMed] [Google Scholar]
- Srithi K, Balslev H, Wangpakapattanawong P, Srisanga P, Trisonthi C. Medicinal plant knowledge and its erosion among the Mien (Yao) in northern Thailand. J Ethnopharmacol. 2009;123:335–342. doi: 10.1016/j.jep.2009.02.035. [DOI] [PubMed] [Google Scholar]
- Cragg GM, Newman DJ. Plants as a source of anti‒cancer and anti‒HIV agents. Ann Appl Biol. 2003;143:127–133. doi: 10.1111/j.1744-7348.2003.tb00278.x. [DOI] [Google Scholar]
- Heinrich M, Gibbons S. Ethnopharmacology in drug discovery: an analysis of its role and potential contribution. J Pharm Pharmacol. 2001;53:425–432. doi: 10.1211/0022357011775712. [DOI] [PubMed] [Google Scholar]
- Abe R, Ohtani K. An ethnobotanical study of medicinal plants and traditional therapies on Batan Island, the Philippines. J Ethnopharmacol. 2013;145:554–565. doi: 10.1016/j.jep.2012.11.029. [DOI] [PubMed] [Google Scholar]
- Cakilcioglu U, Khatun S, Turkoglu I, Hayta S. Ethnopharmacological survey of medicinal plants in Maden (Elazig-Turkey) J Ethnopharmacol. 2011;137:469–486. doi: 10.1016/j.jep.2011.05.046. [DOI] [PubMed] [Google Scholar]
- Kadir MF, Bin Sayeed MS, Mia MMK. Ethnopharmacological survey of medicinal plants used by indigenous and tribal people in Rangamati, Bangladesh. J Ethnopharmacol. 2012;144:627–637. doi: 10.1016/j.jep.2012.10.003. [DOI] [PubMed] [Google Scholar]
- HMGN. Forest Act, 1993 and Forest Regulation, 1995. Kathmandu, Nepal: Ministry of Forests and Soil Conservation; 1993. [Google Scholar]
- Tiwari NN, Poudel RC, Uprety Y. Study on Domestic Market of Medicinal and Aromatic Plants (MAPs) in Kathmandu Valley. Kathmandu, Nepal: Winrock International; 2004. p. 46. [Google Scholar]
- Anonymous. Medicinal Plants of Nepal. Kathmandu, Nepal: Ministry of Forest and Soil Conservation, Department of Plant Resources; 1997. [3] [Google Scholar]
- Joshi SG. Medicinal Plants. Delhi, India: Oxford & IBH Publishing Company Pvt. Limited; 2000. [Google Scholar]
- Anonymous. Medicinal Plants of Nepal. Kathmandu, Nepal: Ministry of Forest and Soil Conservation, Department of Plant Resources; 2001. [10] [Google Scholar]
- Siwakoti M, Siwakoti S. Ethnobot Midicinal Plants Indian Subcont Eds Maheshwori JK. Jodhapur, India: Scientific publishers; 2000. Ethnobotanical uses of plants among the Satar tribes of Nepal; pp. 79–108. [Google Scholar]
- Department of Plant Resources (DPR) Fungi of Nepal Part II: Mastigomycotina, Zygomycotina and Ascomycotina. Kathmandu, Nepal: Bulletin of the Department of Plant Resources (DPR), Government of Nepal; 1997. [16] [Google Scholar]
- Acharya SK. Folk uses of some medicinal plants of Pawan Nagar, Dang District. J Nat Hist Mus. 1996;15:25–36. [Google Scholar]
- Parajuli SP. Ethnobotanical study of at Khandbari municipality of Sankhuwasabha district, Nepal. Banko Jankari. 2000;10:29–34. [Google Scholar]
- Bhattacharjee SK. Handbook of Medicinal PlantsFolk Uses of Some Medicinal Plants of Pawan Nagar, Dang District. 3. Jaipur, India: Pointer publishers; 2001. [Google Scholar]
- Joshi AR, Edington JM. The use of medicinal plants by two village communities in the central development region of Nepal. Econ Bot. 1990;44:71–83. doi: 10.1007/BF02861069. [DOI] [Google Scholar]
- Pohle P. Useful Plants of Manang District: A Contribution to the Ethnobotany of the Nepal-Himalaya. Stuttgart: Franz Steiner Verlag Wiesbaden GMBH; 1990. [Google Scholar]
- Ray D, Sharatchandra K, Thokchom I. Antipyretic, antidiarrhoeal, hypoglycaemic and hepatoprotective activities of ethyl acetate extract of Acacia catechu Willd. in albino rats. Indian J Pharmacol. 2006;38:408–413. doi: 10.4103/0253-7613.28207. [DOI] [Google Scholar]
- Wang Y-H, Wang W-Y, Chang C-C, Liou K-T, Sung Y-J, Liao J-F, Chen C-F, Chang S, Hou Y-C, Chou Y-C, Shen Y-C. Taxifolin ameliorates cerebral ischemia-reperfusion injury in rats through its anti-oxidative effect and modulation of NF-kappa B activation. J Biomed Sci. 2006;13:127–141. doi: 10.1007/s11373-005-9031-0. [DOI] [PubMed] [Google Scholar]
- Gulzar A, Manjul PS, Anita S, Upendra K, Yatendra K. Preliminary phytochemical and antimicrobial screening of leaves extract of Acacia catechu Willd. J Pharm Res. 2010;3:2583–2584. [Google Scholar]
- Parajuli B. Ethnobotany and antimicrobial activities of medicinal plants used diarrhoea and dysentery in Nawalparasi district, Nepal. Kirtipur, Nepal: Central Department of Botany, Tribhuvan University; 2004. (M.Sc. Thesis). [Google Scholar]
- Baidya MR. Screening and evaluation of in-vitro antimicrobial activity of medicinal plants of Nepal. Kirtipur, Nepal: Central Department of Microbilogy, Tribhuvan University; 2001. (M.Sc. Thesis). [Google Scholar]
- Dongmo AB, Nguelefack T, Lacaille-Dubois MA. Antinociceptive and anti-inflammatory activities of Acacia pennata wild (Mimosaceae) J Ethnopharmacol. 2005;98:201–206. doi: 10.1016/j.jep.2005.01.030. [DOI] [PubMed] [Google Scholar]
- Chevallier A. The Encyclopedia of Medicinal Plants. London, UK: Dorling Kindersley Ltd.; 1996. [Google Scholar]
- Bhogi Hanuman J, Katz A. Diterpenoid alkaloids from ayurvedic processed and unprocessed Aconitum ferox. Phytochemistry. 1994;36:1527–1535. doi: 10.1016/S0031-9422(00)89756-3. [DOI] [Google Scholar]
- Sabitha RA, Satyakala M, Sandya DV, Suryanarayana MU. Evaluation of antibacterial activity from rhizome extract of Acorus calamus Linn. J Sci Ind Res. 2003;62:529–650. [Google Scholar]
- Phongpaichit S, Pujenjob N, Rukachaisirikul V, Ongsakul M. Antimicrobial activities of the crude methanol extract of Acorus calamus Linn. Songklanakarin J Sci Technol. 2005;27:517–523. [Google Scholar]
- Valsaraj R, Pushpangadan P, Smitt UW, Adsersen A, Nyman U. Antimicrobial screening of selected medicinal plants from India. J Ethnopharmacol. 1997;58:75–83. doi: 10.1016/S0378-8741(97)00085-8. [DOI] [PubMed] [Google Scholar]
- Gautam S. Medicinal Plants used to treat respiratory complaints in Nawalparasi District (Southern Nepal) and their antibacterial activities. Kirtipur, Nepal: Central Department of Botany, Tribhuvan University; 2002. (M.Sc. Thesis). [Google Scholar]
- Bhattarai S. Antibacterial Activity of Selected Ethnomedicinal Plants of Nawalparasi District, Central Nepal. Research. Bhaktapur, Nepal: University Grant Commission; 2007. [Google Scholar]
- Panthi MP. Plant diversity and resources utilization in Agrhakhanchi and Manang districts of Nepal. Kirtipur, Nepal: Central Department of Botany, Tribhuvan University; 2006. (Ph.D. Thesis). [Google Scholar]
- Maharjan N, Singh A, Manandhar MD, Basnyat S, Lekhak B, Kalauni SK. Evaluation of antibacterial activities of medicinal plants. Nepal J Sci Technol. 2012;13:209–214. [Google Scholar]
- Gyawali R, Bhandari J, Amatya S, Piya E, Pradhan UL, Paudyal R, Shrestha R, Shrestha TM. Antibacterial and cytotoxic activities of high altitude essential oils from Nepalese Himalaya. J Med Plants Res. 2013;7:738–743. [Google Scholar]
- Rani P, Khullar N. Antimicrobial evaluation of some medicinal plants for their anti-enteric potential against multi-drug resistant Salmonella typhi. Phytother Res. 2004;18:670–673. doi: 10.1002/ptr.1522. [DOI] [PubMed] [Google Scholar]
- Raja SB, Murali MR, Malathi GK, Anbarasu K, Devaraj SN. Effect of aqueous extract of Aegle marmelos fruit on adherence and and β-Lactam eesistance of enteropathogenic Escherichia coli by down regulating outer membrane protein C. Am J Infect Dis. 2009;5:154–162. doi: 10.3844/ajidsp.2009.154.162. [DOI] [Google Scholar]
- Brijesh S, Daswani P, Tetali P, Antia N, Birdi T. Studies on the antidiarrhoeal activity of Aegle marmelos unripe fruit: Validating its traditional usage. BMC Complement Altern Med. 2009;9:47. doi: 10.1186/1472-6882-9-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharrif MM, Verma SK. Aloe vera their chemicals composition and applications: A review. Int J Biol Med Res. 2011;2:446–471. [Google Scholar]
- Basmatker G, Jais N, Daud AN. Aloe vera: a valuable multifunctional cosmetic ingredient. Int J Med Aromat Plants. 2011;1:338–341. [Google Scholar]
- Chaudhary DN, Singh JN, Singh BP. Effect of some medicinal plants on fertility of albino rats. Indian J Pharmacol. 1991;23:253–257. [Google Scholar]
- Gupta RS, Sharma R, Sharma A, Bhatnager AK, Dobhal MP, Joshi YC, Sharma MC. Effect of Alstonia scholaris bark extract on testicular function of Wistar rats. Asian J Androl. 2002;4:175–178. [PubMed] [Google Scholar]
- Gupta RS, Bhatnager AK, Joshi YC, Sharma MC, Khushalani V, Kachhawa JBS. Induction of antifertility with lupeol acetate in male albino rats. Pharmacology. 2005;75:57–62. doi: 10.1159/000086947. [DOI] [PubMed] [Google Scholar]
- Hilou A, Nacoulma OG, Guiguemde TR. In vivo antimalarial activities of extracts from Amaranthus spinosus L. and Boerhaavia erecta L. in mice. J Ethnopharmacol. 2006;103:236–240. doi: 10.1016/j.jep.2005.08.006. [DOI] [PubMed] [Google Scholar]
- Timsina G. Evaluation of antimicrobial activities of some medicinal plants used in traditional medicine in Nepal. Kirtipur, Nepal: Central Department of Botany, Tribhuvan University; 2003. (M.Sc. Thesis). [Google Scholar]
- Chiu N, Chang K. The Illustrated Medicinal Plants in Taiwan. Vol. 1. Taiwan: SMC publication Inc.; 1995. [Google Scholar]
- Rashid S, Rather MA, Shah WA, Bhat BA. Chemical composition, antimicrobial, cytotoxic and antioxidant activities of the essential oil of Artemisia indica Willd. Food Chem. 2013;138:693–700. doi: 10.1016/j.foodchem.2012.10.102. [DOI] [PubMed] [Google Scholar]
- Parajuli S. Medicinal Plants used in cuts and wounds in Kaski district (Western Nepal) and their antimicrobial activities. Kirtipur, Nepal: Central Department of Botany, Tribhuvan University; 2001. (M.Sc. Thesis). [Google Scholar]
- Baliga MS, Shivashankara AR, Haniadka R, Dsouza J, Bhat HP. Phytochemistry, nutritional and pharmacological properties of Artocarpus heterophyllus Lam (jackfruit): A review. Food Res Int. 2011;44:1800–1811. doi: 10.1016/j.foodres.2011.02.035. [DOI] [Google Scholar]
- Sabnis PB, Gaitonde BB, Jetmalani M. Effects of alcoholic extracts of Asparagus racemosus on mammary glands of rats. Indian J Exp Biol. 1968;6:55–57. [PubMed] [Google Scholar]
- Pandey SK, Sahay A, Pandey RS, Tripathi YB. Effect of Asparagus racemosus rhizome (Shatavari) on mammary gland and genital organs of pregnant rat. Phytother Res PTR. 2005;19:721–724. doi: 10.1002/ptr.1590. [DOI] [PubMed] [Google Scholar]
- Joglekar GV, Ahuja RH, Balwani JH. Galactagogue effect of Asparagus racemosus. Indian Med J. 1967;61:165. [PubMed] [Google Scholar]
- Gewali MB, Awale S. Aspects of Traditional Medicine in Nepal. Japan: Institute of Natural Medicine. University of Toyama; 2008. [Google Scholar]
- Bhowmik D, Yadav JC, Tripathi KK, Kumar KPS. Herbal remedies of Azadirachta indica and its medicinal application. J Chem Pharm Res. 2010;2:62–72. [Google Scholar]
- Pokhrel NR, Adhikari RP, Baral MP. In-vitro evaluation of the antimicrobial activity of Bauhinia variegata, locally known as koiralo. World J Microbiol Biotechnol. 2002;18:69–71. doi: 10.1023/A:1013969628634. [DOI] [Google Scholar]
- Sharma C, Aneja KR, Kasera R. Screening of Berberis aristata DC. for antimicrobial potential against the pathogens causing ear infection. Int J Pharmacol. 2011;7:536–541. [Google Scholar]
- Bhattarai S. Ethnobotany and antimicrobial activities of selected medicinal plants of Nepal Himalaya. Kirtipur, Nepal: Central Department of Botany, Tribhuvan University; 2009. (Ph.D. Thesis). [Google Scholar]
- Bhattarai S, Chaudhary RP, Taylor RS. Ethnomedicinal plants used by the people of Manang district, central Nepal. J Ethnobiol Ethnomedicine. 2006;2:41. doi: 10.1186/1746-4269-2-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahato RB. Diversity, use and conservation of plants in Palpa district, Nepal. Kirtipur, Nepal: Central Department of Botany, Tribhuvan University; 2006. (Ph.D. Thesis). [Google Scholar]
- Shrestha MP. Medicinal plants used by local communities of Tokha (Chandeshwari) area and antimicrobial activities of some selected plants. Kirtipur, Nepal: Central Department of Botany, Tribhuvan University; 2004. (M.Sc. Thesis). [Google Scholar]
- Yang XM, Wang ZK, Wang ZH, Li RX. Analysis of nutritive components and mineral element of Bergenae pacumbis inTibet. J Chang Veg. 2009;22:57–58. [Google Scholar]
- Zhang Y, Liao C, Li J, Liu X. A review on resource status, bioactive ingredients, clinical applications and biological progress in Bergenia. J Med Plants Res. 2011;5:4396–4399. [Google Scholar]
- Huang KC. The Pharmacology of Chinese Herbs. 2. New York, USA: CRC Press; 1999. [Google Scholar]
- Pertwee RG. Cannabinoids and the gastrointestinal tract. Gut. 2001;48:859–867. doi: 10.1136/gut.48.6.859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spadaro F, Costa R, Circosta C, Occhiuto F. Volatile composition and biological activity of key lime Citrus aurantifolia essential oil. Nat Prod Commun. 2012;7:1523–1526. [PubMed] [Google Scholar]
- Zhou J, Xie G, Yan Z. Encyclopedia of Traditional Chinese Medicines: Molecular Structures, Pharmacological Activities, Natural Sources and Applications - Indexes. Volume 3, 5. Springer; 2011. [Google Scholar]
- Mukherjee PK, Nema NK, Maity N, Sarkar BK. Phytochemical and therapeutic potential of cucumber. Fitoterapia. 2013;84:227–236. doi: 10.1016/j.fitote.2012.10.003. [DOI] [PubMed] [Google Scholar]
- Jananie RK, Priya V, Vijayalashmi K. Determination of bioactive components of Cynodon dactylon by GC-MS analysis. N Y Sci J. 2011;4:16–20. [Google Scholar]
- Garg VK, Paliwal SK. Anti-Inflammatory activity of aqueous extract of Cynodon dactylon. Int J Pharmacol. 2011;7:370–375. [Google Scholar]
- Ma K-J, Zhu Z-Z, Yu C-H, Zhang H, Liu J, Qin L-P. Analgesic, anti-inflammatory, and antipyretic activities of the ethanol extract from Desmodium caudatum. Pharm Biol. 2011;49:403–407. doi: 10.3109/13880209.2010.520322. [DOI] [PubMed] [Google Scholar]
- Wei Y, Zhang K, Zhang G, Ito Y. Isolation of five bioactive components from Eupatorium adenophorum Spreng using stepwise elution by high-speed counter-current chromatography. J Liq Chromatogr Relat Technol. 2011;34:2505–2515. doi: 10.1080/10826076.2011.591030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vijaya K, Ananthan S, Nalinib R. Antibacterial effect of theaflavin, polyphenon 60 (Camelliasinensis) and Euphorbia hirta on Shigella spp. - a cell culture study. J Ethnopharmacol. 1995;49:115–118. doi: 10.1016/0378-8741(95)90039-X. [DOI] [PubMed] [Google Scholar]
- Jackson C, Agboke A, Nwoke V. In vitro evaluation of antimicrobial activity of combinations of nystatin and Euphorbia hirta leaf extract against Candida albicans by the checkerboard method. J Med Plants Res. 2009;3:666–669. [Google Scholar]
- Lanhers MC, Fleurentin J, Dorfman P, Mortier F, Pelt JM. Analgesic, antipyretic and antiinflammatory properties of Euphorbia hirta. Planta Med. 1991;57:225–231. doi: 10.1055/s-2006-960079. [DOI] [PubMed] [Google Scholar]
- Martinez V, Mariano A, Teresa OR, Lazcano ME, Bye R. Anti-inflammatory active compounds from the n-hexane extract of Euphorbia hirta. J Mex Chem Soc. 1999;43:103–105. [Google Scholar]
- Sreelekshmi R, Latha PG, Arafat MM, Shyamal S, Shine VJ, Anuja GI, Suja SR, Rajasekharan S. Anti-inflammatory, analgesic and anti-lipid peroxidation studies on stem bark of Ficus religiosa Linn. Nat Prod Radiance. 2007;6:377–381. [Google Scholar]
- Viswanathan S, Thirugnanasambantham P, Reddy MK, Narasimhan S, Subramaniam GA. Anti-inflammatory and mast cell protective effect of Ficus religiosa. Anc Sci Life. 1990;10:122–125. [PMC free article] [PubMed] [Google Scholar]
- Jung HW, Son HY, Minh CV, Kim YH, Park YK. Methanol extract of Ficus leaf inhibits the production of nitric oxide and proinflammatory cytokines in LPS-stimulated microglia via the MAPK pathway. Phytother Res. 2008;22:1064–1069. doi: 10.1002/ptr.2442. [DOI] [PubMed] [Google Scholar]
- Jatav VS, Singh S, Khatri P, Sharma A. Recent pharmacological trends of Glycyrrhiza glabra Linn. Unani Res. 2011;1:1–11. doi: 10.5530/ur.2.2011.3. [DOI] [Google Scholar]
- Igbinsosa OO, Igbinosa EO, Aiyegoro OA. Antimicrobial activity and phytochemical screening of stem bark extracts from Jatropha curcas (Linn) Afr J Pharm Pharmacol. 2009;3:058–062. [Google Scholar]
- Erdemoglu N, Küpeli E, Yeşilada E. Anti-inflammatory and antinociceptive activity assessment of plants used as remedy in Turkish folk medicine. J Ethnopharmacol. 2003;89:123–129. doi: 10.1016/S0378-8741(03)00282-4. [DOI] [PubMed] [Google Scholar]
- Talapatra SK, Karmacharya B, De SC. ( - )-Regiolone, an α-tetralone from Juglans regia: structure, stereochemistry and conformation. Phytochem Anal. 1988;27:3929–3932. [Google Scholar]
- Babula P, Adam V, Havel L, Kizek R. Naphthoquinones and their pharmacological properties. Ceská Slov Farm. 2007;56:114–120. [PubMed] [Google Scholar]
- Claeson UP, Malmfors T, Wikman G, Bruhn JG. Adhatoda vasica: a critical review of ethnopharmacological and toxicological data. J Ethnopharmacol. 2000;72:1–20. doi: 10.1016/S0378-8741(00)00225-7. [DOI] [PubMed] [Google Scholar]
- Jain VC, Shah DP, Sonani NG, Dhakara S, Patel NM. Pharmacognostical and preliminary phytochemical investigation of Lawsonia inermis L. leaf. Romanian J Biol-Plant Biol. 2010;55:127–133. [Google Scholar]
- Comai S, Dall’Acqua S, Grillo A, Castagliuolo I, Gurung K, Innocenti G. Essential oil of Lindera neesiana fruit: Chemical analysis and its potential use in topical applications. Fitoterapia. 2010;81:11–16. doi: 10.1016/j.fitote.2009.06.017. [DOI] [PubMed] [Google Scholar]
- Orhan I, Küpeli E, Şener B, Yesilada E. Appraisal of anti-inflammatory potential of the clubmoss, Lycopodium clavatum L. J Ethnopharmacol. 2007;109:146–150. doi: 10.1016/j.jep.2006.07.018. [DOI] [PubMed] [Google Scholar]
- Perry LM, Metzger J. Medicinal Plants of East and Southeast Asia: Attributed Properties and Uses. London: MIT Press; 1980. [Google Scholar]
- Panthi MP, Chaudhary RP. Antibacterial acitivity of some selected foklore medicinal plants fom west Nepal. Sci World. 2006;4:16–21. [Google Scholar]
- Thakur SC, Thakur SS, Chaube SK, Singh SP. An etheral extract of Kamala (Mallotus philippinensis (Moll.Arg) Lam.) seed induce adverse effects on reproductive parameters of female rats. Reprod Toxicol. 2005;20:149–156. doi: 10.1016/j.reprotox.2004.12.008. [DOI] [PubMed] [Google Scholar]
- Lewis DA, Fields WN, Shaw GP. A natural flavonoid present in unripe plantain banana pulp (Musa sapientum L. var. paradisiaca) protects the gastric mucosa from aspirin-induced erosions. J Ethnopharmacol. 1999;65:283–288. doi: 10.1016/S0378-8741(99)00005-7. [DOI] [PubMed] [Google Scholar]
- Alisi CS, Nwanyanwu CE, Akujobi CO, Ibegbulem CO. Inhibition of dehydrogenase activity in pathogenic bacteria isolates by aqueous extracts of Musa paradisiaca (var sapientum) Afr J Biotechnol. 2008;7:1684–5315. [Google Scholar]
- Rao VS, Rao A, Karanth KS. Anticonvulsant and neurotoxicity profile of Nardostachys jatamansi in rats. J Ethnopharmacol. 2005;102:351–356. doi: 10.1016/j.jep.2005.06.031. [DOI] [PubMed] [Google Scholar]
- Vinutha B, Prashanth D, Salma K, Sreeja SL, Pratiti D, Padmaja R, Radhika S, Amit A, Venkateshwarlu K, Deepak M. Screening of selected Indian medicinal plants for acetylcholinesterase inhibitory activity. J Ethnopharmacol. 2007;109:359–363. doi: 10.1016/j.jep.2006.06.014. [DOI] [PubMed] [Google Scholar]
- Agrawal J, Pal A. Nyctanthes arbor-tristis Linn—A critical ethnopharmacological review. J Ethnopharmacol. 2013;146:645–658. doi: 10.1016/j.jep.2013.01.024. [DOI] [PubMed] [Google Scholar]
- Raghavendra MP, Satish S, Raveesha KA. Phytochemical analysis and antibacterial activity of Oxalis corniculata; a known medicinal plant. mySCIENCE. 2006;1:72–78. [Google Scholar]
- Matsuda H, Pongpiriyadacha Y, Morikawa T, Kishi A, Kataoka S, Yoshikawa M. Protective effects of steroid saponins from Paris polyphylla var. yunnanensis on ethanol- or indomethacin-induced gastric mucosal lesions in rats: structural requirement for activity and mode of action. Bioorg Med Chem Lett. 2003;13:1101–1106. doi: 10.1016/S0960-894X(03)00052-0. [DOI] [PubMed] [Google Scholar]
- Liu X, Cui C, Zhao M, Wang J, Luo W, Yang B, Jiang Y. Identification of phenolics in the fruit of emblica (Phyllanthus emblica L.) and their antioxidant activities. Food Chem. 2008;109:909–915. doi: 10.1016/j.foodchem.2008.01.071. [DOI] [PubMed] [Google Scholar]
- Duke JA. CRC Handbook of Medicinal Herbs. Boca Raton, FL: CRC Press; 1985. [Google Scholar]
- Tomczyk M, Latté KP. Potentilla—A review of its phytochemical and pharmacological profile. J Ethnopharmacol. 2009;122:184–204. doi: 10.1016/j.jep.2008.12.022. [DOI] [PubMed] [Google Scholar]
- Olajide O, Awe S, Makinde J. Pharmacological studies on the leaf of Psidium guajava. Fitoterapia. 1999;70:25–31. doi: 10.1016/S0367-326X(98)00010-0. [DOI] [Google Scholar]
- Zhang WJ, Chen BT, Wang CY, Zhu QH, Mo Z. Mechanism of quercetin as an antidiarrheal agent. Yi Jun Yi Xue Xue Bao. 2003;23:1029–1031. [PubMed] [Google Scholar]
- Coutino RR, Hernandez CP, Giles RH. Lectins in fruits having gastrointestinal activity: their participation in the hemagglutinating property of Escherichia coli O157:H7. Arch Med Res. 2001;32:251–257. doi: 10.1016/S0188-4409(01)00287-9. [DOI] [PubMed] [Google Scholar]
- Matsuura Y, Miyaichi Y, Tomimori T. Studies on the Nepalese crude drugs. XIX. On the flavonoid and phenylethanoid constituents of the root of Scutellaria repens Buch.-Ham. ex D. Don. Yakugaku Zasshi. 1994;114:775–788. doi: 10.1248/yakushi1947.114.10_775. [DOI] [PubMed] [Google Scholar]
- Bhargava S, Rao PS, Bhargava P, Shukla S. Antipyretic Potential of Swertia chirata Buch Ham. Root Extract. Sci Pharm. 2009;77:617–623. [Google Scholar]
- Tita B, Bello U, Faccendini P, Bartolini R, Bolle P. Taraxacum officinale W.: pharmacological effect of ethanol extract. Pharmacol Res. 1993;27:23–24. [Google Scholar]
- Nisar M, Khan I, Ahmad B, Ali I, Ahmad W, Choudhary MI. Antifungal and antibacterial activities of Taxus wallichiana Zucc. J Enzyme Inhib Med Chem. 2008;23:256–260. doi: 10.1080/14756360701505336. [DOI] [PubMed] [Google Scholar]
- Sah S, Shrestha R, Koirala S, Bhattarai K. Phytochemical and antimicrobial assessment of five medicinal plants found in Terai region. Nepal J Sci Technol. 2013;13:79–86. [Google Scholar]
- Chandramu C, Manohar RD, Krupadanam DGL, Dashavantha RV. Isolation, characterization and biological activity of betulinic acid and ursolic acid from Vitex negundo L. Phytother Res. 2003;17:129–134. doi: 10.1002/ptr.1088. [DOI] [PubMed] [Google Scholar]
- Dharmasiri M, Jayakody JRA, Galhena G, Liyanage SS, Ratnasooriya W. Anti-inflammatory and analgesic activities of mature fresh leaves of Vitex negundo. J Ethnopharmacol. 2003;87:199–206. doi: 10.1016/S0378-8741(03)00159-4. [DOI] [PubMed] [Google Scholar]
- Kaur R, Kaur H. The Antimicrobial activity of essential oil and plant extracts of Woodfordia fruticosa. Arch Appl Sci Res. 2010;2:302–309. [Google Scholar]
- Bhattarai S, Bhuju DR. Antimicrobial Activity of Useful Parts of Woodfordia fruticosa (Linn.) Kurz. of Nepal. Int J Pharm Biol Arch. 2011;2:756–761. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Details of informants interviewed in Hadigaun, Aambhanjyang and Tistung village development committees of Makawanpur district.
Medicinal plants used by Tamang community in Makawanpur district, central Nepal [38,84-93].
Comparison of local use and phytochemical and pharmacological studies of medicinal plants [94-186].


