Abstract
The endothelial Tie1 receptor is ligand-less, but interacts with the Tie2 receptor for angiopoietins (Angpt). Angpt2 is expressed in tumor blood vessels, and its blockade inhibits tumor angiogenesis. Here we found that Tie1 deletion from the endothelium of adult mice inhibits tumor angiogenesis and growth by decreasing endothelial cell survival in tumor vessels, without affecting normal vasculature. Treatment with VEGF or VEGFR-2 blocking antibodies similarly reduced tumor angiogenesis and growth; however, no additive inhibition was obtained by targeting both Tie1 and VEGF/VEGFR-2. In contrast, treatment of Tie1-deficient mice with a soluble form of the extracellular domain of Tie2, which blocks Angpt activity, resulted in additive inhibition of tumor growth. Notably, Tie1 deletion decreased sprouting angiogenesis and increased Notch pathway activity in the postnatal retinal vasculature, while pharmacological Notch suppression in the absence of Tie1 promoted retinal hypervasularization. Moreover, substantial additive inhibition of the retinal vascular front migration was observed when Angpt2 blocking antibodies were administered to Tie1-deficient pups. Thus, Tie1 regulates tumor angiogenesis, postnatal sprouting angiogenesis, and endothelial cell survival, which are controlled by VEGF, Angpt, and Notch signals. Our results suggest that targeting Tie1 in combination with Angpt/Tie2 has the potential to improve antiangiogenic therapy.
Introduction
Angiogenesis, the sprouting of new blood vessels from preexisting ones, is required for a variety of physiological processes, such as embryonic development, reproduction, wound healing, and organ regeneration in adults. Furthermore, angiogenesis is involved in several pathological processes, including age-related macular degeneration and cancer (1, 2), and compounds that inhibit the VEGF/VEGFR-2 pathway are in clinical use for the treatment of these diseases. However, targeting the VEGF/VEGFR-2 pathway is often insufficient to control tumor growth. Thus, novel approaches to further develop antiangiogenic therapies for cancer are needed (3).
The angiopoietin (Angpt) growth factors Angpt1 and Angpt2 and the Tie receptors Tie1 and Tie2 form another endothelial receptor tyrosine kinase signaling system with a pivotal role in embryonic vessel morphogenesis and vascular homeostasis (4). Constitutive deletion of Tie1, Tie2, or Angpt1 results in embryonic lethality (5–8). In adults, Angpt1-mediated signals are important for stabilization of the vascular endothelium after angiogenic processes (8). Angpt2 is required for lymphatic development, and postnatally, both Angpt1 and Angpt2 contribute to the development of the retinal vasculature (9, 10).
The Angpt-Tie pathway also regulates tumor angiogenesis (4, 11). Angpt2 levels are increased in many human cancers, and its blockage inhibits tumor growth and angiogenesis (12–14). Blocking Angpt2 also inhibits tumor metastasis via hematogenous and lymphatic routes (13, 15).
All angiopoietins bind to Tie2, while Tie1 is as an orphan receptor (4, 12, 14). However, Tie1 interacts with Tie2, and both translocate to endothelial cell-cell contacts upon Angpt stimulation (16–18). During embryonic development, Tie1 is required for the integrity of the vascular endothelium, particularly in regions undergoing angiogenic capillary growth (5). Tie1 expression is increased in adults during wound healing, ovarian follicle maturation, and tumor angiogenesis (11, 19). According to Woo et al., postnatal loss of 40%–80% of Tie1 did not result in obvious pathology, but instead conferred an atheroprotective effect, in a murine model (20).
In the present study, we showed that endothelial-specific deletion of Tie1 inhibited tumor angiogenesis and growth and delayed developmental angiogenesis occurring postnatally in the retina. Interestingly, angiopoietin inhibitors increased antiangiogenic effects on both tumor and retinal angiogenesis in Tie1-deleted mice.
Results
Validation of a conditional Tie1 loss-of-function mouse model.
To study the importance of Tie1 during postnatal angiogenesis, given that homozygous constitutive Tie1 deletion (Tie1–/–) is embryonic lethal, we generated conditionally Tie1-targeted mice (Tie1flox/flox) using the Cre/loxP system to delete the first coding exon of Tie1 (5, 21, 22). We validated the mouse model by deleting Tie1 ubiquitously, using the Tie1flox/flox allele and the PGK-Cre transgenic strain, in which the expression of the Cre recombinase starts during the diploid phase of oogenesis (Supplemental Figure 1; supplemental material available online with this article; doi:10.1172/JCI68897DS1; and refs. 22, 23). Southern, Northern, and Western blotting demonstrated virtually complete Tie1 gene ablation at the DNA, mRNA, and protein levels in all PGK-Cre/Tie1flox/flox (referred to herein as Tie1Δ/Δ) embryos analyzed (Supplemental Figure 1, C–F, and Supplemental Figure 2). Tie1 mRNA and protein levels in samples of PGK-Cre/Tie1flox/+ (Tie1Δ/+) embryos were about half of those seen in WT and Tie1flox/flox control samples (Supplemental Figure 1, E and F). At E14.5, Tie1Δ/Δ embryos exhibited a pronounced edematous phenotype and hemorrhages (Supplemental Figure 1A), resembling transgenic embryos in which ubiquitous Tie1 deletion is achieved by insertion of the LacZ gene into the Tie1 locus (5, 21). The Tie1Δ/Δ mice died by E17.5 (data not shown).
Examination of histological sections of the thoracic region, stained for the blood vascular endothelial marker endomucin and the lymphatic endothelial markers Prox1 and Lyve1, showed the presence of mispatterned first lymphatic structures that have been previously described as lymph sacs, in Tie1Δ/Δ but not control embryos at E14.5 (Supplemental Figure 3). This phenotype was similar to that reported for embryos that express homozygous hypomorphic Tie1 alleles (22). We visualized the developing lymphatic vasculature in more detail by planar illumination–based ultramicroscopy of whole-mount immunostained E12.5 embryos (24) in which Tie1 had been deleted from endothelial cells (referred to herein as Tie1iECΔ/Δ) (Supplemental Table 1 and Supplemental Methods). Analysis of 3D reconstructions of images obtained by optical sectioning of embryos stained for Pecam1 and Prox1 showed that the first lymphatic structures, recently described as peripheral longitudinal lymphatic vessel (PLLV) and primordial thoracic duct (pTD) (24), were present in anatomically correct positions in the E12.5 Tie1iECΔ/Δ embryos. However, these structures appeared abnormally dilated, and the superficial lymphatic vessels, which extend dorsally from the PLLV, were disrupted when compared with those of control embryos (Supplemental Figure 1B). These results are consistent with our previous analysis of Tie1 hypomorphic and Tie1Δ/Δ embryos at E14.5 (Supplemental Figure 3 and ref. 22) and indicate that Tie1 has an endothelial cell–autonomous role in lymphatic vasculature development.
Endothelial Tie1 deletion inhibits tumor angiogenesis and growth.
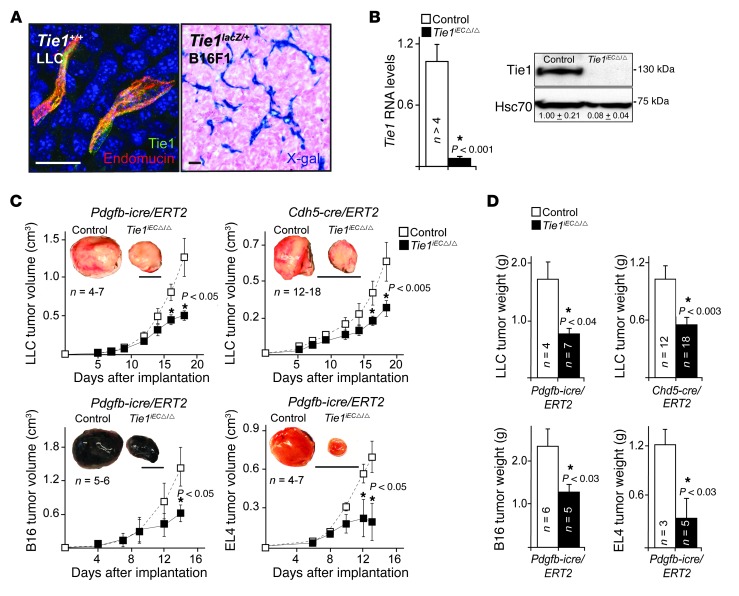
We next assessed the function of Tie1 during tumor angiogenesis. Previous in situ hybridization studies have shown elevated Tie1 mRNA expression in the vascular endothelium of malignant human tumors compared with normal vessel endothelium (19, 25). We confirmed Tie1 expression in angiogenic tumor vessels by immunohistochemical staining and by using heterozygous Tie1lacZ/+ mice, in which the endogenous Tie1 locus drives LacZ gene expression and thus unambiguously marks transgene-expressing cells (Figure 1A). Interestingly, immunohistochemical staining showed variable levels of Tie1 expression in the tumor vasculature. We crossed Tie1flox/flox mice with Cdh5(PAC)-cre/ERT2 and Pdgfb-icre/ERT2 mice (Supplemental Methods). This enabled inducible Tie1 deletion by endothelial-specific Cre recombinase activation after tamoxifen administration (Figure 1B and Supplemental Table 1). We implanted Lewis lung carcinoma (LLC), B16F10 melanoma (B16), or EL4 leukemia/lymphoma (EL4) cells to the Tie1iECΔ/Δ mice and found significantly reduced tumor growth compared with controls (Figure 1, C and D).
Figure 1. Endothelial Tie1 deficiency inhibits tumor growth.
(A) Tie1 expression in the LLC (Tie1, green; endomucin, red; DNA, blue) and B16F1 (X-gal, blue) tumor vasculatures in Tie1+/+ and Tie1lacZ/+ mice, respectively. (B) Tie1 mRNA expression analyzed by quantitative RT-PCR (P < 10–5) and Tie1 and Hsc70 Western blots from control and Tie1iECΔ/Δ lung extracts. Numbers denote relative Tie1 levels. n = 7–10 lungs/genotype. (C) Growth curves of LLC, EL4, and B16F10 (B16) tumors. (D) Tumor weight at termination. Scale bars: 20 μm (A); 10 mm (C). Error bars denote SEM. Significant differences are shown by asterisks, with P values indicated.
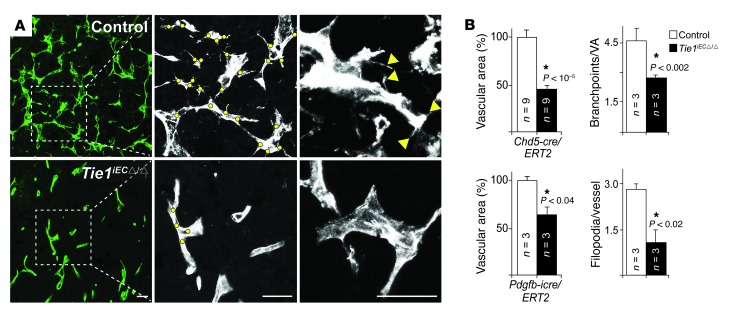
Immunohistochemical staining indicated that Tie1 expression and blood vessel density were reduced in tumors grown in Tie1iECΔ/Δ versus control mice (Supplemental Figure 4 and Figure 2, A and B). Notably, whereas LLC tumor vessels in control mice tended to grow in a branching honeycomb-like pattern, those in Tie1iECΔ/Δ mice showed significantly decreased density of angiogenic sprouts and filopodial extensions (Figure 2, A and B). These results indicated that Tie1 is crucial for tumor growth and angiogenesis.
Figure 2. Endothelial Tie1 deficiency inhibits tumor angiogenesis.
(A) Endomucin immunofluorescence for LLC tumor blood vessels (green or white). Dots denote branchpoints; arrowheads denote filopodia. (B) Vessel density (expressed as area percentage), branchpoints per vessel area (VA), and filopodia per vessel. Scale bars: 100 μm. Error bars denote SEM. Significant differences are shown by asterisks, with P values indicated.
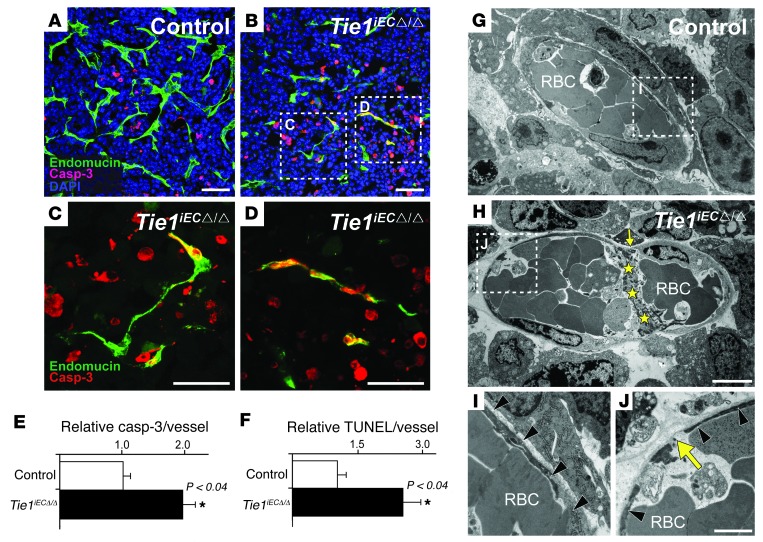
As Tie1 has been reported to promote endothelial cell survival in the late phase of angiogenic capillary growth during mouse embryonic development (21), we assessed endothelial cell apoptosis in the tumor vasculature. Apoptosis was significantly increased in Tie1iECΔ/Δ tumor vessels (Figure 3, A–F). Electron microscopy indicated that the degenerating endothelial cells were occasionally associated with small intravascular fibrin deposits in Tie1iECΔ/Δ tumors (Figure 3, G–J, and Supplemental Figure 5). However, we found no significant differences in endothelial cell proliferation between Tie1iECΔ/Δ and control tumors (Supplemental Figure 6).
Figure 3. Endothelial Tie1 deficiency increases endothelial cell apoptosis in tumor blood vessels.
(A and B) Endomucin (green), caspase-3 (red), and nuclear (blue) staining. (C and D) Higher-magnification views of boxed regions in B. (E) Quantification of caspase-3/endomucin and (F) TUNEL/endomucin double-positive endothelial cells per tumor vessel. (G–J) TEM of control and Tie1iECΔ/Δ tumor blood vessels. (I and J) Higher-magnification views of boxed regions in G and H. Black arrowheads denote continuous endothelial cell layer; yellow arrows denote sites where no endothelial cell is apparent; yellow stars denote fibrin. RBC, red blood cell. Scale bars: 50 μm (A–D); 5 μm (G and H); 2 μm (I and J). Error bars denote SEM. Significant differences are shown by asterisks, with P values indicated.
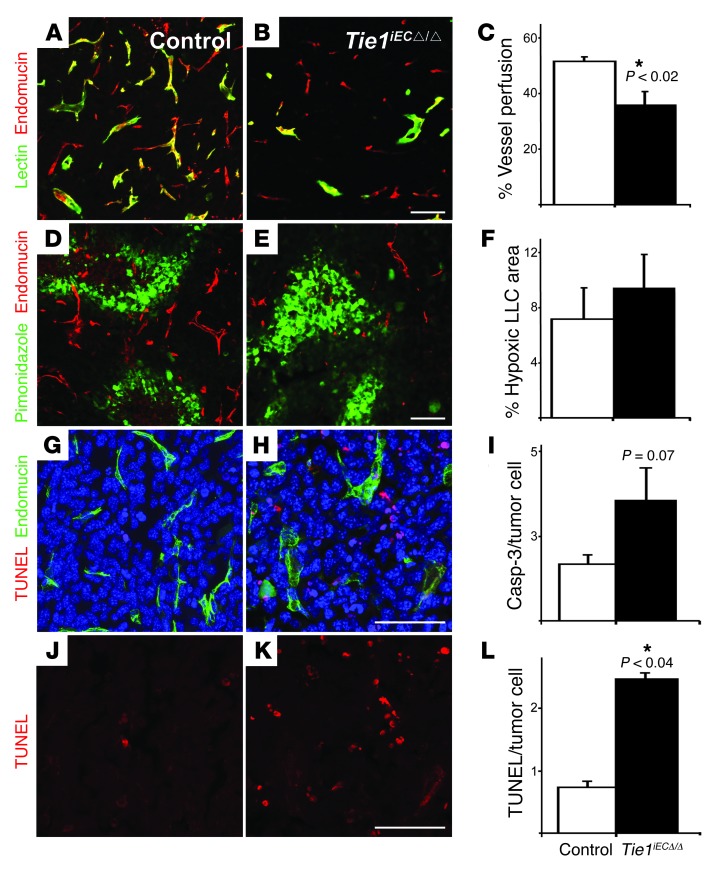
We also analyzed parameters of vessel maturation, integrity, and functionality in the tumors. The percentage of blood vessels coated with NG2 proteoglycan–positive pericytes or α-SMA–positive smooth muscle cells was similar in Tie1iECΔ/Δ and control tumors (Supplemental Figure 7). Intravascular perfusion with Lycopersicon esculentum (tomato) lectin showed a decreased proportion of perfused tumor vessels, and pimonidazole hydrochloride staining indicated a trend toward increased tumor hypoxia, in Tie1iECΔ/Δ versus control tumors (Figure 4, A–F). Furthermore, tumor cell apoptosis was increased in Tie1iECΔ/Δ mice (Figure 4, G–L). Thus, inhibition of tumor angiogenesis by Tie1 deletion was associated with reduced endothelial cell viability in the tumor vessels as well as increased tumor hypoxia and tumor cell death.
Figure 4. Vessel perfusion, hypoxia, and apoptosis in tumors of control and Tie1iECΔ/Δ mice.
(A and B) LLC tumor sections from mice injected i.v. with biotinylated L. esculentum lectin 10 minutes before tumor excision at day 18 after tumor cell implantation. Lectin (green) staining marks functional tumor blood vessels. (C) Vessel perfusion, determined as percent of lectin-positive area relative to percent of endomucin-positive area per field. n = 3–6 tumors/genotype (Pdgfb-icre/ERT2 deletor). (D and E) LLC tumor sections from mice injected i.p. with pimonidazole (hypoxia marker) 1.5 hours before tumor excision. Pimonidazole (green) staining marks the hypoxic area. (F) Percent hypoxic area relative to total field area. n = 9 tumors/genotype (both Cdh5(PAC)-cre/ERT2 and Pdgfb-icre/ERT2 deletors). Note the trend toward increased hypoxia in Tie1iECΔ/Δ tumors. (G and H) Staining for TUNEL (red), endomucin (green), and DAPI (blue). (J and K) TUNEL staining alone from G and H, shown for better visualization. (I and L) Tumor cell apoptosis indices, calculated as ratio of (I) cleaved Caspase-3 and (L) TUNEL fluorescent cells to total DAPI-positive tumor cells per field. n = 3–6 tumors/genotype (both Cdh5(PAC)-cre/ERT2 and Pdgfb-icre/ERT2 deletors). Scale bars: 100 μm. Error bars denote SEM. Significant differences are shown by asterisks, with P values indicated.
Endothelial Tie1 has been suggested to play a role in inflammation, and inflammatory cells regulate tumor angiogenesis and growth (20, 26). Therefore, we investigated whether Tie1 deletion affects endothelial expression of leukocyte adhesion receptors or leukocyte recruitment to the tumor stroma. P-selectin and intercellular adhesion molecule 1 (Icam1) expression were reduced in Tie1iECΔ/Δ tumor endothelium, but there were no significant differences in leukocyte (CD45), monocyte/macrophage (F4/80), or granulocyte (Lys6/Gr-1) recruitment to the tumors (Supplemental Figures 8 and 9). These results suggest that inflammatory cells do not contribute substantially to the decreased tumor growth in Tie1iECΔ/Δ mice.
Tie1 deletion does not harm the healthy vasculature or renal function.
It was previously shown that stringent blocking of VEGF signaling in healthy adult mice for 2 weeks results in significant capillary regression in certain organs (27, 28). As adult Tie1iECΔ/Δ mice exhibited increased endothelial cell apoptosis in tumor isografts, we next analyzed the effect of Tie1 deficiency on normal healthy vessels. We used the Pdgfb-icre/ERT2 deletor strain to induce endothelial Tie1 deletion in 8- to 10-week-old mice. After a deletion period of 3 weeks (corresponding to that in the tumor models), we analyzed the blood vasculature in the lungs, kidneys, heart, thyroid, salivary glands, small intestine, trachea, and skin. Quantitation of Pecam1 and endomucin staining indicated that blood vessel density was not significantly different in Tie1iECΔ/Δ versus control tissues (Supplemental Figure 10, A and B). Analysis of interendothelial adherens junctions of blood capillaries immunostained for cadherin 5 (Cdh5; also known as VE-cadherin) and quantitation of the diameter of postcapillary venules in the tracheal mucosa did not reveal statistically significant differences between Tie1iECΔ/Δ and control mice (Supplemental Figure 10, C–H). In addition, analysis of lungs by H&E and Masson’s trichrome staining and by transmission EM (TEM) did not reveal substantial changes between Tie1iECΔ/Δ and control mice (Supplemental Figure 10, I–M).
The ultrastructural features of renal glomerular capillaries, such as endothelial cell fenestrations, basement membrane thickness, or podocyte foot processes were not altered by either endothelial-specific or ubiquitous (Rosa26/creERT deletor; ref. 29) Tie1 deletion (3 weeks and 5 months, respectively; Supplemental Figure 11A, Supplemental Table 1, and Supplemental Methods). In line with this, Tie1 deletion did not alter blood urea nitrogen or creatinine concentrations in serum. Moreover, no significant changes were observed in polypeptides in urine when comparing control versus Tie1-deficient mice (Supplemental Figure 11, B and C), which suggests that Tie1 is not necessary for the maintenance of kidney function under basal conditions. Thus, despite the effects of Tie1 deficiency on tumor angiogenesis, normal vessels were not significantly affected in various adult Tie1iECΔ/Δ mouse tissues after a 3-week deletion period.
Endothelial Tie1 deletion does not improve antiangiogenic therapy directed against VEGF or VEGFR-2.
Recent results have suggested that blocking Angpt2 increases the efficacy of antiangiogenic therapy directed against the VEGF/VEGFR-2 pathway (30–32). We tested whether endothelial Tie1 deletion in combination with blocking antibodies against VEGF or VEGFR-2 provides additive inhibition of tumor angiogenesis and growth. The VEGFR-2 blocking antibody DC101 (33) and the VEGF blocking antibody mcr84 (34) were both capable of significantly inhibiting angiogenesis and growth of LLC, EL4, and B16F1 tumors in control mice. Although Tie1 deletion was equally effective in reducing tumor growth, no additive antiangiogenic effects were seen when either antibody was used in combination with endothelial Tie1 deletion (Supplemental Figure 12). Interestingly, when VEGF was injected and allowed to circulate for 10 minutes, decreased VEGFR-2 protein was detected in Tie1iECΔ/Δ versus control lung lysates. The decreased VEGFR-2 levels may help to explain the reduced endothelial cell survival in the tumors and the ineffectiveness of VEGF signaling inhibition in Tie1iECΔ/Δ mice (Supplemental Figure 13).
Previous studies assessing the safety of very-high-affinity anti-VEGF antibodies showed some renal and hepatic damage, including glomerulosclerosis and loss of glomerular structural integrity (35). We thus analyzed kidney glomeruli in the tumor-bearing mice treated with placebo or mcr84 antibody, which has a low toxicity profile in mice (34). Morphological and immunohistochemical analysis showed no statistically significant differences in glomerular tufts, Bowman’s space, or vascular density in the kidney glomeruli (Supplemental Figure 14). Furthermore, the liver histology in H&E staining was unaltered, and total body weights were similar in all mice throughout the experiment (data not shown). Thus, in our tumor model, the combination of endothelial Tie1 deletion and mcr84 antibody treatment did not induce kidney or liver damage (Supplemental Figure 14 and data not shown).
Effect of Tie1 deletion on Tie2 signaling pathways in vivo.
Previous in vitro studies have suggested that silencing of endothelial Tie1 increases Angpt2-induced Tie2 phosphorylation and that VEGF enhances Tie2 responsiveness to Angpt1 by modulating the Tie1/Tie2 ratio on the cell surface (36, 37). However, in our experiments, total Tie2 phosphotyrosine was not significantly altered in the lungs of Tie1-deleted mice, even in the presence of VEGF, which was injected i.v. and allowed to circulate for 10 minutes (Supplemental Figure 15A). Interestingly however, phosphorylation of Tie2 at Y1106, which is known to bind the Dok-R protein and to promote Angpt1-mediated endothelial cell migration (38), was decreased when Tie1 was deleted (Supplemental Figure 15B).
Combinatorial targeting of Tie1 and angiopoietins results in additive tumor growth inhibition.
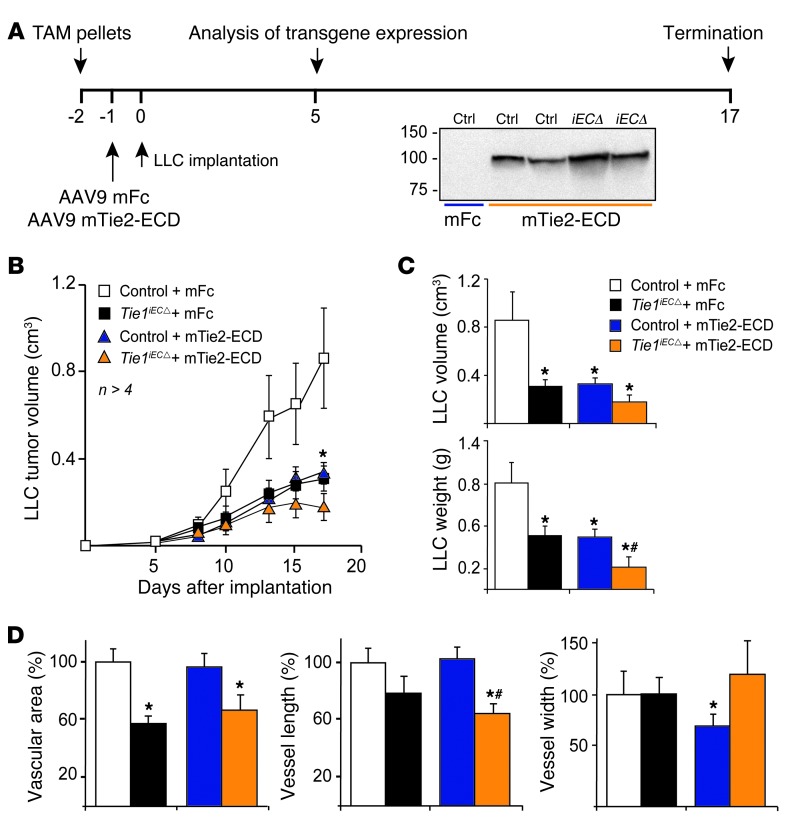
The dominant Tie2 ligand in tumors is Angpt2, which is produced by the angiogenic tumor endothelium (39, 40). We thus tested whether combinatorial targeting of Tie1 and Angpts provides additive inhibition of tumor angiogenesis and growth. Because we could not identify a tumor isograft model that is sensitive to anti-Angpt2 antibodies (our unpublished observations), we used an adeno-associated virus (AAV) vector to deliver a soluble form of the extracellular domain (ECD) of mouse Tie2 (referred to herein as mTie2-ECD; Figure 5A), which binds Angpt1 and Angpt2 and blocks their activity (13, 41). In agreement with previous reports (32, 41), mTie2-ECD treatment inhibited the growth of LLC tumor isografts in mice (Figure 5, B and C). However, the antitumor effect was significantly greater when mTie2-ECD was used in combination with endothelial Tie1 deletion (Figure 5, B and C). Compared with mTie2-ECD alone, the combinatorial targeting decreased the length and increased the width of the vessels in the tumor sections and tended to increase pericyte recruitment (Figure 5D and data not shown).
Figure 5. Combinatorial targeting of Tie1 and Angpts results in greater inhibition of tumor growth than targeting either alone.
(A) Experimental settings for induction of Tie1 deletion by tamoxifen (TAM) pellets, soluble extracellular domain of murine Tie2 (mTie2-ECD) or soluble murine Fc gamma receptor (mFc) expression, and LLC tumor implantation. (B) LLC tumor growth curves. (C) Tumor volume and weight at 18 days. (D) Vascular area, vessel length, and vessel width (expressed as a percentage of control plus mFc). Error bars denote SEM. *P < 0.05 versus control plus IgG; #P < 0.05 versus control plus mTie2-ECD.
Endothelial Tie1 deletion inhibits postnatal retinal angiogenesis.
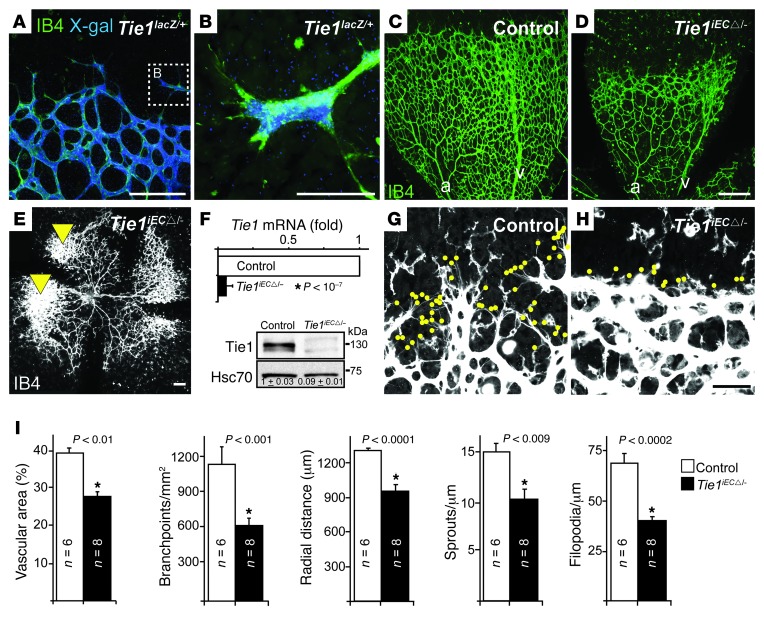
The mouse retina provides an excellent opportunity to study postnatal angiogenesis and has been widely used for that purpose (42). We used β-galactosidase staining of retinas from heterozygous Tie1+/lacZ mice at P5 to demonstrate Tie1 expression in retinal endothelial cells, including the tip cells of the endothelial sprouts at the vascular front (Figure 6, A and B, and Supplemental Figure 16, A–D).
Figure 6. Endothelial Tie1 deficiency inhibits postnatal retinal angiogenesis.
(A) β-galactosidase staining of a Tie1lacZ/+ retina at P6. (B) A Tie1-expressing tip cell. (C–E) IB4–stained P6 retinas. a, arteriole; v, venule. Arrowheads denote vascular tufts. (F) Quantitative RT-PCR and Western blot of lungs from control and Tie1iECΔ/– (Cdh5(PAC)-cre/ERT2 and Pdgfb-icre/ERT2 deletors) P6 pups. Numbers denote mean densitometric readouts of relative Tie1 levels. n = 3–4 lungs/genotype. (G and H) High-magnification images of the angiogenic front. Dots denote filopodia. (I) Quantification of vascular area, branchpoints, radial distance from optic nerve, sprouts, and filopodia. Scale bars: 100 μm (A, C–E, G, and H); 50 μm (B). Error bars denote SEM. Significant differences are shown by asterisks, with P values indicated.
To delete Tie1 in the retinal endothelium, we first confirmed that administration of 4-hydroxytamoxifen (OHT) resulted in effective Cre recombinase activation in the retinal endothelial cells, using Pdgfb-icre/ERT2 mice bred with the Rosa26-R reporter strain (43–45). OHT treatment from P1 to P4 induced strong Cre activation in the whole retinal vascular bed, as detected by β-galactosidase staining in P5 retinal endothelial cells of the Pdgfb-icre/ERT2;Rosa26-R pups (Supplemental Figure 16, E–H). However, although Tie1iECΔ/Δ pups developed without major signs of distress until sacrifice at P5 or P6, analysis of their retinas revealed a statistically significant decrease in vessel area, vessel branchpoints, and the distance of the migratory angiogenic vessel front from the optic nerve (Supplemental Figure 17). Notably, no significant retinal phenotype was observed in pups in which the Tie1 deletion was only 80%–85% complete (data not shown).
To maximize the extent of Tie1 deletion, we combined Tie1 conditional and constitutive targeted alleles (Figure 6, C–I). Tamoxifen-induced Tie1 deletion in Cdh5(PAC)-cre/ERT2;Tie1flox/– and Pdgfb-icre/ERT2;Tie1flox/– pups (referred to herein as Tie1iECΔ/–) resulted in near-complete Tie1 ablation, and the resulting retinal phenotype was severely aggravated compared with that of Tie1iECΔ/Δ pups (Figure 6, C–I, and Supplemental Figure 17). Interestingly, in some Tie1iECΔ/– pups, we also observed the presence of endothelial cell tufts (Figure 6E), a feature not seen in Tie1iECΔ/Δ pups. Furthermore, the filopodial extensions of the tip cells were significantly reduced, and in some Tie1iECΔ/– pups, the migratory front of the retinal vasculature was almost devoid of endothelial sprouts (Figure 6H and Supplemental Figure 18). Further analysis of the vessels revealed a few pericyte-positive (i.e., NG2 staining), but endothelium-negative (i.e., lacking isolectin B4 [IB4] staining) cellular structures, particularly in capillary branches extending from the arterioles of the Tie1iECΔ/– retinas (Supplemental Figure 18), suggestive of occasional vessel branch regression. Nevertheless, the retinal vasculature seemed normal when Tie1 was deleted between P7 and P9 and analyzed at P17 (data not shown). These results indicate that Tie1 deficiency delays normal development of the postnatal retinal vasculature during angiogenesis, but does not affect the vascular remodeling phase. Furthermore, the reduced vascular area and decreased number of angiogenic sprouts and filopodial extensions observed in the Tie1-deficient postnatal retinas resembled changes observed in the tumor vasculature in the Tie1-deficient adult mice.
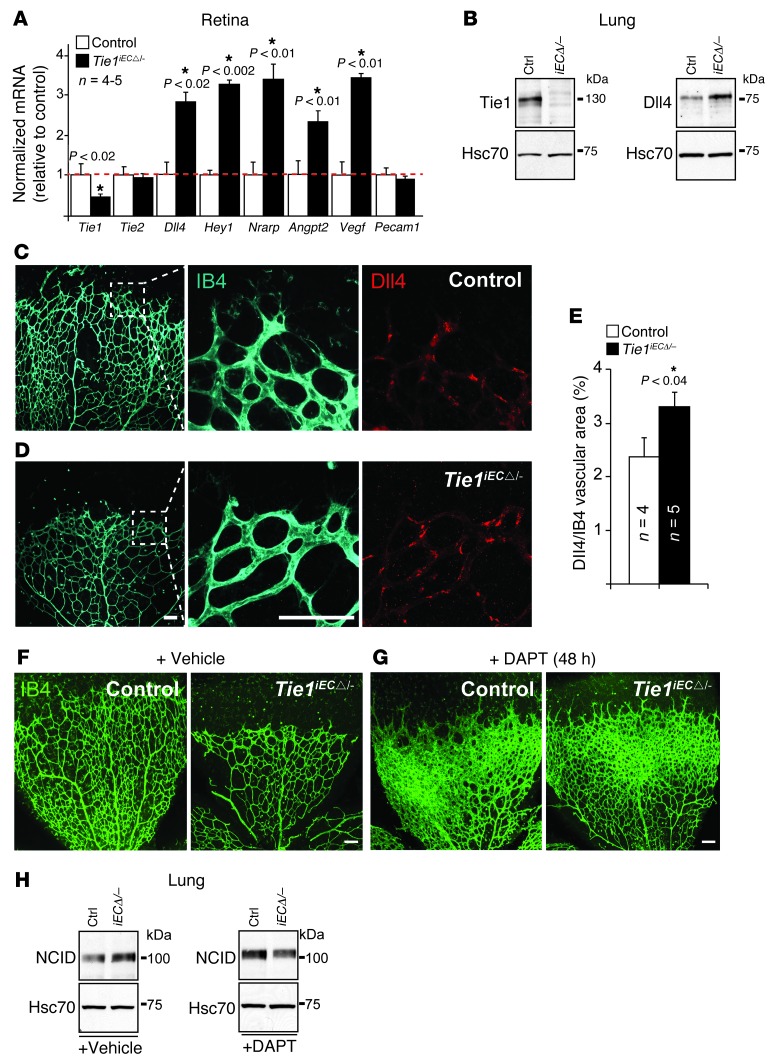
The Notch pathway is activated in Tie1-deficient retinal endothelial cells.
The expression of Tie1 in retinal endothelial tip cells and the retinal phenotype of Tie1-deleted mice prompted us to analyze whether the Tie1 deletion is associated with changes in Notch ligand Delta-like 4 (Dll4) signaling. Dll4 is mainly expressed in the angiogenic tip cells, and it activates Notch signaling in the stalk cells to suppress their migration and sprouting (46, 47). Quantitative RT-PCR using retinal extracts showed that the Tie1iECΔ/Δ and Tie1iECΔ/– retinas expressed significantly increased amounts of mRNA encoding Dll4 and the downstream Notch signaling molecules Hairy enhancer-of-split related with YRPW motif 1 (Hey1) and Notch-regulated ankyrin repeat protein (Nrarp), as well as the hypoxia-regulated angiogenic factors Vegf and Angpt2 (Figure 7A). Dll4 mRNA and protein levels, and the intracellular domain of Notch (NCID), which is cleaved upon its activation, were also significantly upregulated in Tie1iECΔ/Δ and Tie1iECΔ/– lung extracts (Figure 7, B and H, and Supplemental Figure 19). Furthermore, whole-mount staining indicated significantly increased endothelial Dll4 abundance in Tie1iECΔ/– versus control retinas at P6 (Figure 7, C–E). These results indicate that the Notch pathway is activated in the Tie1-deficient retinas, consistent with the suppression of the migratory and sprouting phenotype of the retinal vasculature.
Figure 7. Tie1-deficient retinal phenotype involving upregulation of Dll4/Notch is abolished by Notch inhibitor.
(A) Quantitative RT-PCR analysis of control and Tie1iECΔ/– (Cdh5(PAC)-cre/ERT2 and Pdgfb-icre/ERT2 deletors) retinas at P6. mRNA levels were normalized to Cdh5 to compensate for the decreased vascular area in the Tie1iECΔ/– retinas and expressed relative to control levels (assigned as 1; red dashed line). (B) Representative Western blot analysis of lungs (see Supplemental Figure 19 for quantification). n = 5–8 (control); 6–14 (Tie1iECΔ/–). (C and D) IB4 (cyan) and Dll4 (red) staining of (C) control and (D) Tie1iECΔ/– angiogenic retinal fronts. (E) Quantification of Dll4-positive endothelium (expressed as a percentage). (F and G) IB4 (green) staining of retinas from control and Tie1iECΔ/– (Pdgfb-icre/ERT2 deletor) P6 pups treated with (F) vehicle or (G) DAPT for 48 hours. (H) Representative Western blotting for Notch1 cleaved intracellular domain (NCID) from vehicle- and DAPT-treated lungs. n = 3–4 lungs/genotype. Scale bars: 50 μm. Error bars denote SD (A) or SEM (E). Significant differences are shown by asterisks, with P values indicated.
To further analyze the involvement of the Notch pathway in the Tie1-deficient phenotype, we used the γ-secretase inhibitor DAPT, which inhibits Notch cleavage and signaling (46). Interestingly, Tie1iECΔ/– and control pups had an almost identical retinal hypervascularization phenotype at P6, after a 48-hour treatment with DAPT (Figure 7, F and G). DAPT treatment also prevented the increase of NCID in Tie1iECΔ/– pups (Figure 7H). These results suggest that increased Notch activation contributes to the Tie1-deficient retinal phenotype.
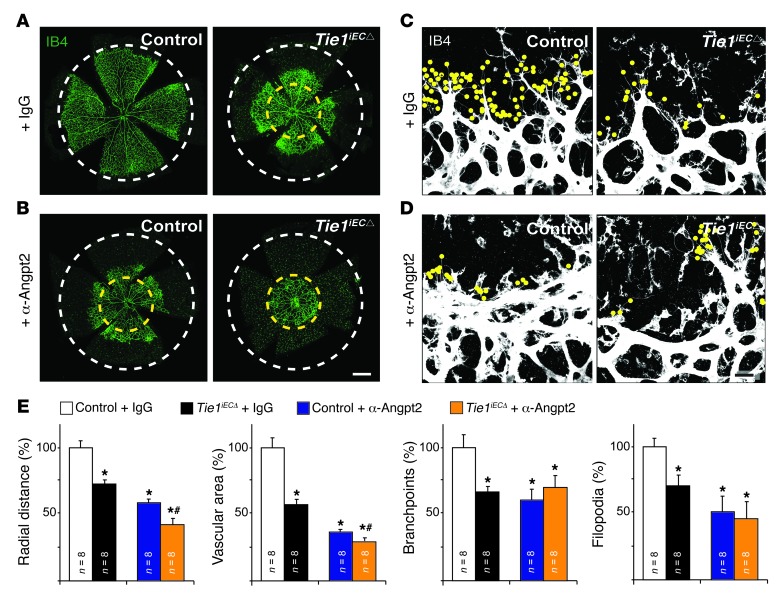
Combinatorial targeting of Tie1 and Angpt2 results in additive inhibition of retinal angiogenesis.
Anti-Angpt2 blocking antibodies inhibit retinal angiogenesis, and Angpt2 expression is highly selective for retinal endothelial tip cells, where we found Tie1 expression, but little or no Tie2 expression (13, 48, 49). We tested whether Tie1 deletion in combination with anti-Angpt2 blocking antibodies could provide additive inhibition of retinal angiogenesis. We deleted Tie1 in pups as described above and simultaneously administered anti-Angpt2 or IgG isotype control antibodies. At P5, as expected, both IgG-treated Tie1iECΔ/Δ pups and anti-Angpt2–treated control pups showed a statistically significant decrease in the distance of the vascular front from the optic nerve compared with IgG-treated controls (Figure 8, A–E). Surprisingly however, significant additive inhibition of vascular front migration was observed when anti-Angpt2 antibodies were used in Tie1iECΔ/Δ pups (Figure 8, B, D, and E). These results showed that the combinatorial treatment with anti-Angpt2 blocking antibodies increases the antiangiogenic effects of Tie1 deletion on retinal sprouting angiogenesis, in line with our results on tumor angiogenesis and growth, in which combinatorial targeting of Tie1 and Angpt2 via soluble murine Tie2-ECD were additive.
Figure 8. Combinatorial targeting of Tie1 and Angpt2 results in greater inhibition of retinal angiogenesis than targeting either alone.
(A and B) IB4-stained retinas from control and either Tie1iECΔ/Δ or Tie1iECΔ/– (Tie1iECΔ) P5 pups treated with (A) human IgG isotype (IgG) or (B) anti-Angpt2 antibodies. White dashed circles denote average control angiogenic front; yellow dashed circles denote average anti-Angpt2–treated Tie1iECΔ angiogenic front. (C and D) High-magnification images of the angiogenic front. Dots denote filopodia. (E) Radial distance from optic nerve, vascular area, branchpoints, and filopodia (expressed as a percentage of IgG-treated control). Scale bars: 100 μm. Error bars denote SEM. *P < 0.05 versus control plus IgG; #P < 0.05 versus control plus anti-Angpt2.
Discussion
Here we report that deleting Tie1 specifically from the vascular endothelium inhibited tumor angiogenesis and growth, to the same extent as blocking antibodies targeted against VEGF or its major signal transducing receptor, VEGFR-2. To our knowledge, this is the first study showing that Tie1, a receptor for which no growth factor ligands have yet been identified, functions as a positive regulator of pathological angiogenesis and that Tie1 targeting has beneficial antitumor effects. Tumors grown in Tie1-deficient mice had decreased vessel density, vascular perfusion, and endothelial cell survival, and this was associated with decreased tumor cell survival. The tumor vessels in Tie1iECΔ/Δ mice showed reduced numbers of angiogenic sprouts and filopodial extensions, resembling the delayed development of the postnatal retinal vasculature in Tie1iECΔ/– mice.
VEGF- and Angpt2-mediated angiogenesis is involved in retinal and choroidal diseases, the most common causes of loss of vision in the developed countries (50). Angpt2 is expressed in the mouse retina between P0 and P7, when the superficial retinal vessels develop; after P7, its expression shifts to the regions of the developing intermediate and deep capillary vascular beds (9, 50, 51). Retinal vascular development is defective in Angpt2-knockout mice, and we and others have recently shown that anti-Angpt2 blocking antibodies inhibit physiological retinal angiogenesis (9, 13, 49). Although the success of the anti-VEGF approach has been remarkable, some concerns exist about the long-term effects of VEGF antagonism in the eye (52). Therefore, new targets and their combinations for safer and more effective therapy are still needed. To our knowledge, our report is the first to show that targeting Tie1 significantly inhibits retinal angiogenesis and that, importantly, combinatorial treatment with anti-Angpt2 blocking antibodies increases this effect.
Notch and VEGF pathway interactions have been thoroughly studied in retinal sprouting angiogenesis, but only 1 study thus far has analyzed the Dll4/Notch crosstalk with angiopoietin/Tie2 signaling (53). We showed here that Dll4/Notch signals were increased in the absence of Tie1, inhibiting retinal angiogenesis even in the presence of increased amounts of the main hypoxia-induced angiogenic drivers, such as VEGF and Angpt2. Furthermore, blocking the Notch pathway abolished the Tie1 deletion phenotype in the developing retina, which suggests that increased Notch signaling is, at least in part, responsible for the inhibition of retinal angiogenesis in the Tie1-deleted mice. This is consistent with previous studies showing that vascular endothelial cells transfected with Dll4 grow poorly even in the presence of VEGF and that upregulation of the Notch pathway in the tumor vessels results in inhibition of tumor neovascularization and growth (54).
The combination of Tie1 inhibition with Angpt antagonists could potentially aid the development of drugs not only for the treatment of ocular diseases, but also for tumor therapy. In line with this, Tie1iECΔ/Δ mice bearing LLC tumors treated with a soluble form of the Tie2 receptor, which blocks Angpt activity, resulted in a stronger antitumor effect than targeting Tie1 or Angpt alone. Considering that the Angpt1/Angpt2 balance in the context of the tumor environment is strongly shifted toward Anpgt2 expression (55, 56), one could argue that the additive antitumor effects are likely due to the combinatorial targeting of Tie1 and Anpgt2. Notably, the Angpt1/Angpt2 blocking peptibody has already entered clinical phase III trials for the treatment of ovarian cancer, and Angpt2 blocking antibodies are tested in phase I/II trials in many different cancers ( www.clinicaltrials.gov). The development of Tie1 inhibitors would be a worthwhile goal, as they would probably synergize with the Angpt blocking agents in tumor therapy.
Tie1 has been shown to interact with Tie2 in endothelial cell-cell and cell-substratum contacts, where Angpt1 mediates activation of the complex (16–18). Although some reports have suggested that Tie1 may inhibit Tie2 activation, we did not find significantly increased Tie2 phosphorylation in lung lysates from the Tie1-deleted mice. Instead, phosphorylation of Tie2 at Y1106 appeared to be reduced in Tie1-deleted versus control mice. The Tie2Y1106 phosphopeptide is known to bind Dok-R, which mediates Angpt1-induced endothelial cell migration (38), suggesting that reduced Tie2 phosphorylation at Y1106 may contribute to the phenotype of the retinal and tumor blood vessels in Tie1-deleted mice. In line with this, Angpt1 was recently found to be required for postnatal retinal vascularization (10). However, as exogenous Angpt2 did not affect Tie2 phosphorylation at Y1106 in our experiments, blocking Angpt2 may inhibit another signaling pathway, for example, one mediated by the integrins (49). It should be noted that endogenous Angpt2 is produced by endothelial cells in hypoxic tissues, and autocrine Angpt2 stimulation of Tie2 may mediate a proangiogenic function in conditions of vascular stress (57, 58).
The current antiangiogenic inhibitors based on targeting VEGF signaling are effective in treating age-related macular degeneration, but thus far, their utility in cancer has been limited to prolonging disease-free survival in patients with a few tumor types (3). Our present results indicate that Tie1 targeting inhibits tumor angiogenesis by decreasing endothelial cell survival and subsequently decreasing vascular density and vessel perfusion, while not affecting the normal vessels in various organs. The overall healthy condition of the Tie1-deleted mice is consistent with the conclusion that their possible vascular changes would have to be relatively subtle. Furthermore, recent experiments have shown that atherosclerosis is inhibited by partial Tie1 deletion (20), which argues that decreased Tie1 function might be beneficial not only in cancer, but also in atherosclerosis patients. Thus, our present findings elucidate a previously unknown regulatory system for angiogenesis and propose Tie1 as a potential new target for anti-angiogenic therapy that potentially holds clinical relevance now, more than 20 years after its isolation (59), when we first suggested — based on its enhanced expression pattern in the tumor vasculature (19) — the possible involvement for this interesting receptor in tumorigenesis and other angiogenesis-dependent diseases, such as diabetic retinopathy, atherosclerosis, and arthritis.
Methods
Further information can be found in Supplemental Methods.
Statistics.
At least 3 mice were analyzed per time point and treatment. 2-tailed paired or equal-variance Student’s t test or 1-way ANOVA was used for statistical analysis. A P value less than 0.05 was considered statistically significant.
Study approval.
Mice were maintained in the Meilahti Experimental Animal Center and in the Laboratory Animal Centre of University of Oulu according to IACUC and IRB guidelines. The National Animal Experiment Board in Finland approved animal experiments used in this study.
Supplementary Material
Acknowledgments
We thank Juha Partanen, Tatiana Petrova, and Maija Bry for critical comments on the manuscript; Yvan Lallemand and Marcus Fruttiger for transgenic mice; Sirpa Jalkanen and Petri Salven for tumor cells; Ching Ching Leow and MedImmune and Gerhard Christofori for 3.19.3 and DC101 antibodies, respectively; Seppo Kaijalainen for AAV constructs; Michael Jeltsch for VEGF protein; and Hannu Sariola for advice on histopathology. We acknowledge Alun Parsons, Laura Raitanen, Kirsi Lintula, Tanja Laakkonen, Katja Salo, Tapio Tainola, Jaana Träskelin, Jussi Kenkkilä, and Biocenter Oulu and Biomedicum Imaging Unit staff for technical assistance and microscopy services. This work was funded by the EU-ERC Program (TX-Factors, AdG_20100317), the Marie Curie ITN (Vessel, FP7-PEOPLE-2012-ITN), the Sigrid Juselius Foundation, the Finnish Cancer Organizations, the Finnish Foundation for Cardiovascular Research, and the Academy of Finland (140723 and 262976 to K. Alitalo; 130446 to P. Saharinen; 136880 and Centre of Excellence Program 2012-2017 to L. Eklund). G. D’Amico was supported by University of Helsinki funds. F. Kiefer was supported by the DFG (SFB629 and SFB656). T. Holopainen was supported by the K. Albin Johansson Foundation and Finska Läkaresällskapet.
Footnotes
Conflict of interest: The authors have declared that no conflict of interest exists.
Citation for this article: J Clin Invest. 2014;124(2):824–834. doi:10.1172/JCI68897.
References
- 1.Chung AS, Ferrara N. Developmental and pathological angiogenesis. Annu Rev Cell Dev Biol. 2011;27:563–584. doi: 10.1146/annurev-cellbio-092910-154002. [DOI] [PubMed] [Google Scholar]
- 2.Welti J, Loges S, Dimmeler S, Carmeliet P. Recent molecular discoveries in angiogenesis and antiangiogenic therapies in cancer. J Clin Invest. 2013;123(8):3190–3200. doi: 10.1172/JCI70212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Singh M, Ferrara N. Modeling and predicting clinical efficacy for drugs targeting the tumor milieu. Nat Biotechnol. 2012;30(7):648–657. doi: 10.1038/nbt.2286. [DOI] [PubMed] [Google Scholar]
- 4.Augustin HG, Koh GY, Thurston G, Alitalo K. Control of vascular morphogenesis and homeostasis through the angiopoietin-Tie system. Nat Rev Mol Cell Biol. 2009;10(3):165–177. doi: 10.1038/nrm2639. [DOI] [PubMed] [Google Scholar]
- 5.Puri MC, Rossant J, Alitalo K, Bernstein A, Partanen J. The receptor tyrosine kinase TIE is required for integrity and survival of vascular endothelial cells. EMBO J. 1995;14(23):5884–5891. doi: 10.1002/j.1460-2075.1995.tb00276.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dumont DJ, et al. Dominant-negative and targeted null mutations in the endothelial receptor tyrosine kinase, tek, reveal a critical role in vasculogenesis of the embryo. Genes Dev. 1994;8(16):1897–1909. doi: 10.1101/gad.8.16.1897. [DOI] [PubMed] [Google Scholar]
- 7.Suri C, et al. Requisite role of angiopoietin-1, a ligand for the TIE2 receptor, during embryonic angiogenesis. Cell. 1996;87(7):1171–1180. doi: 10.1016/S0092-8674(00)81813-9. [DOI] [PubMed] [Google Scholar]
- 8.Jeansson M, et al. Angiopoietin-1 is essential in mouse vasculature during development and in response to injury. J Clin Invest. 2011;121(6):2278–2289. doi: 10.1172/JCI46322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gale NW, et al. Angiopoietin-2 is required for postnatal angiogenesis and lymphatic patterning, and only the latter role is rescued by Angiopoietin-1. Dev Cell. 2002;3(3):411–423. doi: 10.1016/S1534-5807(02)00217-4. [DOI] [PubMed] [Google Scholar]
- 10.Lee J, et al. Angiopoietin-1 guides directional angiogenesis through integrin αvβ5 signaling for recovery of ischemic retinopathy. Sci Transl Med. 2013;5(203):203ra127. doi: 10.1126/scitranslmed.3006666. [DOI] [PubMed] [Google Scholar]
- 11.Korhonen J, et al. Enhanced expression of the tie receptor tyrosine kinase in endothelial cells during neovascularization. Blood. 1992;80(10):2548–2555. [PubMed] [Google Scholar]
- 12.Saharinen P, Eklund L, Pulkki K, Bono P, Alitalo K. VEGF and angiopoietin signaling in tumor angiogenesis and metastasis. Trends Mol Med. 2011;17(7):347–362. doi: 10.1016/j.molmed.2011.01.015. [DOI] [PubMed] [Google Scholar]
- 13.Holopainen T, et al. Effects of angiopoietin-2-blocking antibody on endothelial cell-cell junctions and lung metastasis. J Natl Cancer Inst. 2012;104(6):461–475. doi: 10.1093/jnci/djs009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Eklund L, Saharinen P. Angiopoietin signaling in the vasculature. Exp Cell Res. 2013;319(9):1271–1280. doi: 10.1016/j.yexcr.2013.03.011. [DOI] [PubMed] [Google Scholar]
- 15.Schulz P, et al. Angiopoietin-2 drives lymphatic metastasis of pancreatic cancer. FASEB J. 2011;25(10):3325–3335. doi: 10.1096/fj.11-182287. [DOI] [PubMed] [Google Scholar]
- 16.Saharinen P, et al. Multiple angiopoietin recombinant proteins activate the Tie1 receptor tyrosine kinase and promote its interaction with Tie2. J Cell Biol. 2005;169(2):239–243. doi: 10.1083/jcb.200411105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saharinen P, et al. Angiopoietins assemble distinct Tie2 signalling complexes in endothelial cell-cell and cell-matrix contacts. Nat Cell Biol. 2008;10(5):527–537. doi: 10.1038/ncb1715. [DOI] [PubMed] [Google Scholar]
- 18.Fukuhara S, et al. Differential function of Tie2 at cell-cell contacts and cell-substratum contacts regulated by angiopoietin-1. Nat Cell Biol. 2008;10(5):513–526. doi: 10.1038/ncb1714. [DOI] [PubMed] [Google Scholar]
- 19.Kaipainen A, et al. Enhanced expression of the tie receptor tyrosine kinase mesenger RNA in the vascular endothelium of metastatic melanomas. Cancer Res. 1994;54(24):6571–6577. [PubMed] [Google Scholar]
- 20.Woo KV, et al. Tie1 attenuation reduces murine atherosclerosis in a dose-dependent and shear stress-specific manner. J Clin Invest. 2011;121(4):1624–1635. doi: 10.1172/JCI42040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Partanen J, Puri MC, Schwartz L, Fischer KD, Bernstein A, Rossant J. Cell autonomous functions of the receptor tyrosine kinase TIE in a late phase of angiogenic capillary growth and endothelial cell survival during murine development. Development. 1996;122(10):3013–3021. doi: 10.1242/dev.122.10.3013. [DOI] [PubMed] [Google Scholar]
- 22.D’Amico G, Korhonen EA, Waltari M, Saharinen P, Laakkonen P, Alitalo K. Loss of endothelial Tie1 receptor impairs lymphatic vessel development-brief report. Arterioscler Thromb Vasc Biol. 2010;30(2):207–209. doi: 10.1161/ATVBAHA.109.196618. [DOI] [PubMed] [Google Scholar]
- 23.Lallemand Y, Luria V, Haffner-Krausz R, Lonai P. Maternally expressed PGK-Cre transgene as a tool for early and uniform activation of the Cre site-specific recombinase. Transgenic Res. 1998;7(2):105–112. doi: 10.1023/A:1008868325009. [DOI] [PubMed] [Google Scholar]
- 24.Hagerling R, et al. A novel multistep mechanism for initial lymphangiogenesis in mouse embryos based on ultramicroscopy. EMBO J. 2013;32(5):629–644. doi: 10.1038/emboj.2012.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hatva E, et al. Expression of endothelial cell-specific receptor tyrosine kinases and growth factors in human brain tumors. Am J Pathol. 1995;146(2):368–378. [PMC free article] [PubMed] [Google Scholar]
- 26.Chan B, Sukhatme VP. Suppression of Tie-1 in endothelial cells in vitro induces a change in the genome-wide expression profile reflecting an inflammatory function. FEBS Lett. 2009;583(6):1023–1028. doi: 10.1016/j.febslet.2009.02.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kamba T, et al. VEGF-dependent plasticity of fenestrated capillaries in the normal adult microvasculature. Am J Physiol Heart Circ Physiol. 2006;290(2):H560–H576. doi: 10.1152/ajpheart.00133.2005. [DOI] [PubMed] [Google Scholar]
- 28.Yang Y, et al. Anti-VEGF- and anti-VEGF receptor-induced vascular alteration in mouse healthy tissues. Proc Natl Acad Sci U S A. 2013;110(29):12018–12023. doi: 10.1073/pnas.1301331110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vooijs M, Jonkers J, Berns A. A highly efficient ligand-regulated Cre recombinase mouse line shows that LoxP recombination is position dependent. EMBO Rep. 2001;2(4):292–297. doi: 10.1093/embo-reports/kve064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brown JL, et al. A human monoclonal anti-ANG2 antibody leads to broad antitumor activity in combination with VEGF inhibitors and chemotherapy agents in preclinical models. Mol Cancer Ther. 2010;9(1):145–156. doi: 10.1158/1535-7163.MCT-09-0554. [DOI] [PubMed] [Google Scholar]
- 31.Hashizume H, et al. Complementary actions of inhibitors of angiopoietin-2 and VEGF on tumor angiogenesis and growth. Cancer Res. 2010;70(6):2213–2223. doi: 10.1158/0008-5472.CAN-09-1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Koh YJ, et al. Double antiangiogenic protein, DAAP, targeting VEGF-A and angiopoietins in tumor angiogenesis, metastasis, and vascular leakage. Cancer Cell. 2010;18(2):171–184. doi: 10.1016/j.ccr.2010.07.001. [DOI] [PubMed] [Google Scholar]
- 33.Prewett M, et al. Antivascular endothelial growth factor receptor (fetal liver kinase 1) monoclonal antibody inhibits tumor angiogenesis and growth of several mouse and human tumors. Cancer Res. 1999;59(20):5209–5218. [PubMed] [Google Scholar]
- 34.Sullivan LA, et al. r84, a novel therapeutic antibody against mouse and human VEGF with potent anti-tumor activity and limited toxicity induction. PLoS One. 2010;5(8):e12031. doi: 10.1371/journal.pone.0012031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gerber HP, et al. Mice expressing a humanized form of VEGF-A may provide insights into the safety and efficacy of anti-VEGF antibodies. Proc Natl Acad Sci U S A. 2007;104(9):3478–3483. doi: 10.1073/pnas.0611492104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Singh H, Hansen TM, Patel N, Brindle NP. The molecular balance between receptor tyrosine kinases Tie1 and Tie2 is dynamically controlled by VEGF and TNFα and regulates angiopoietin signalling. PLoS One. 2012;7(1):e29319. doi: 10.1371/journal.pone.0029319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Seegar TC, et al. Tie1-Tie2 interactions mediate functional differences between angiopoietin ligands. Mol Cell. 2010;37(5):643–655. doi: 10.1016/j.molcel.2010.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jones N, et al. A unique autophosphorylation site on Tie2/Tek mediates Dok-R phosphotyrosine binding domain binding and function. Mol Cell Biol. 2003;23(8):2658–2668. doi: 10.1128/MCB.23.8.2658-2668.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Maisonpierre PC, et al. Angiopoietin-2, a natural antagonist for Tie2 that disrupts in vivo angiogenesis. Science. 1997;277(5322):55–60. doi: 10.1126/science.277.5322.55. [DOI] [PubMed] [Google Scholar]
- 40.Holash J, et al. Vessel cooption, regression, and growth in tumors mediated by angiopoietins and VEGF. Science. 1999;284(5422):1994–1998. doi: 10.1126/science.284.5422.1994. [DOI] [PubMed] [Google Scholar]
- 41.Lin P, et al. Antiangiogenic gene therapy targeting the endothelium-specific receptor tyrosine kinase Tie2. Proc Natl Acad Sci U S A. 1998;95(15):8829–8834. doi: 10.1073/pnas.95.15.8829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Phng LK, Gerhardt H. Angiogenesis: a team effort coordinated by notch. Dev Cell. 2009;16(2):196–208. doi: 10.1016/j.devcel.2009.01.015. [DOI] [PubMed] [Google Scholar]
- 43.Tammela T, et al. VEGFR-3 controls tip to stalk conversion at vessel fusion sites by reinforcing Notch signalling. Nat Cell Biol. 2011;13(10):1202–1213. doi: 10.1038/ncb2331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Claxton S, Kostourou V, Jadeja S, Chambon P, Hodivala-Dilke K, Fruttiger M. Efficient, inducible Cre-recombinase activation in vascular endothelium. Genesis. 2008;46(2):74–80. doi: 10.1002/dvg.20367. [DOI] [PubMed] [Google Scholar]
- 45.Soriano P. Generalized lacZ expression with the ROSA26 Cre reporter strain. Nat Genet. 1999;21(1):70–71. doi: 10.1038/5007. [DOI] [PubMed] [Google Scholar]
- 46.Hellstrom M, et al. Dll4 signalling through Notch1 regulates formation of tip cells during angiogenesis. Nature. 2007;445(7129):776–780. doi: 10.1038/nature05571. [DOI] [PubMed] [Google Scholar]
- 47.Suchting S, et al. The Notch ligand Delta-like 4 negatively regulates endothelial tip cell formation and vessel branching. Proc Natl Acad Sci U S A. 2007;104(9):3225–3230. doi: 10.1073/pnas.0611177104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.del Toro R, et al. Identification and functional analysis of endothelial tip cell-enriched genes. Blood. 2010;116(19):4025–4033. doi: 10.1182/blood-2010-02-270819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Felcht M, et al. Angiopoietin-2 differentially regulates angiogenesis through TIE2 and integrin signaling. J Clin Invest. 2012;122(6):1991–2005. doi: 10.1172/JCI58832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Campochiaro PA. Ocular neovascularization. J Mol Med (Berl). 2013;91(3):311–321. doi: 10.1007/s00109-013-0993-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hackett SF, Wiegand S, Yancopoulos G, Campochiaro PA. Angiopoietin-2 plays an important role in retinal angiogenesis. J Cell Physiol. 2002;192(2):182–187. doi: 10.1002/jcp.10128. [DOI] [PubMed] [Google Scholar]
- 52.Kurihara T, Westenskow PD, Bravo S, Aguilar E, Friedlander M. Targeted deletion of Vegfa in adult mice induces vision loss. J Clin Invest. 2012;122(11):4213–4217. doi: 10.1172/JCI65157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zhang J, et al. Angiopoietin-1/Tie2 signal augments basal Notch signal controlling vascular quiescence by inducing δ-like 4 expression through AKT-mediated activation of β-catenin. J Biol Chem. 2011;286(10):8055–8066. doi: 10.1074/jbc.M110.192641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Williams CK, Li JL, Murga M, Harris AL, Tosato G. Up-regulation of the Notch ligand δ-like 4 inhibits VEGF-induced endothelial cell function. Blood. 2006;107(3):931–939. doi: 10.1182/blood-2005-03-1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Helfrich I, et al. Angiopoietin-2 levels are associated with disease progression in metastatic malignant melanoma. Clin Cancer Res. 2009;15(4):1384–1392. doi: 10.1158/1078-0432.CCR-08-1615. [DOI] [PubMed] [Google Scholar]
- 56.Goede V, et al. Identification of serum angiopoietin-2 as a biomarker for clinical outcome of colorectal cancer patients treated with bevacizumab-containing therapy. Br J Cancer. 2010;103(9):1407–1414. doi: 10.1038/sj.bjc.6605925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yuan HT, Khankin EV, Karumanchi SA, Parikh SM. Angiopoietin 2 is a partial agonist/antagonist of Tie2 signaling in the endothelium. Mol Cell Biol. 2009;29(8):2011–2022. doi: 10.1128/MCB.01472-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Daly C, et al. Angiopoietin-2 functions as a Tie2 agonist in tumor models, where it limits the effects of VEGF inhibition. Cancer Res. 2013;73(1):108–118. doi: 10.1158/0008-5472.CAN-12-2064. [DOI] [PubMed] [Google Scholar]
- 59.Partanen J, et al. A novel endothelial cell surface receptor tyrosine kinase with extracellular epidermal growth factor homology domains. Mol Cell Biol. 1992;12(4):1698–1707. doi: 10.1128/mcb.12.4.1698. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.