Abstract
Background
Lipedema is a rare female disorder with a characteristic distribution of adipose tissue hypertrophy on the extremities, with pain and bruising. In advanced stages, reduction of adipose tissue is the only available effective treatment. In elderly patients with advanced lipedema, correction of increased skin laxity has to be considered for an optimal outcome.
Methods
We report on a tailored combined approach to improve advanced lipedema in elderly females with multiple comorbidities. Microcannular laser-assisted liposuction of the upper legs and knees is performed under tumescent anesthesia. Medial thigh lift and partial lower abdominoplasty with minimal undermining are used to correct skin laxity and prevent intertrigo. Postsurgical care with nonelastic flat knitted compression garments and manual lymph drainage are used.
Results
We report on three women aged 55–77 years with advanced lipedema of the legs and multiple comorbidities. Using this step-by-step approach, a short operation time and early mobilization were possible. Minor adverse effects were temporary methemoglobinemia after tumescent anesthesia and postsurgical pain. No severe adverse effects were seen. Patient satisfaction was high.
Conclusion
A tailored approach may be useful in advanced lipedema and is applicable even in elderly patients with multiple comorbidities.
Keywords: lipedema, tumescent anesthesia, liposuction, subdermal diode laser, medial thigh lift, lower abdominoplasty
Introduction
Lipedema is a disfiguring inherited disease affecting women. The disease is characterized by proximal attenuated lipohypertrophy of the extremities, in particular the upper legs and knees. Patients often complain about pain and bruising after minor trauma.1 Although the underlying pathogenesis is poorly understood, recruitment of adipose-derived stem cells has been observed.2 The severity of the disease can be classified into three grades according to Meier-Vollrath and Schmeller, with grade 3 being the most advanced and disabling.3
Microcannular liposuction has been shown to be the most effective treatment for advanced cases.4–8 The pathologic adipose tissue on the upper legs is typically localized to the anterior aspects, proximal thigh, and medioposterior knees. This leads not only to disfigurement, but may hamper gait and knee bending and promote knee problems.3,7 Although microcannular liposuction improves body contour and function, tightening of the skin is limited. Laser-assisted liposuction seems to be superior to other types of liposuction under this view. This technique offers a comfortable combination of body contouring and skin tightening in younger nonobese patients.9,10
When treating patients with lipedema, in particular elderly patients with advanced lipedema, the situation is different. Extensive autonomous subcutaneous adipose tissue growth and skin laxity are a challenge. Because of the multimorbidity seen in such patients with the concomitant presence of metabolic and cardiovascular disease, the procedures have to be designed for increased safety as well.4
Although the functional outcome after repeated liposuction is good, the esthetic outcome may be poor. Since these patients are often intolerant of extensive surgical procedures, a different approach is necessary. Here we describe combination of laser-assisted liposuction and a modified medial thigh lift with lower partial abdominoplasty to obtain satisfying results in this specific group of patients.
Anatomic considerations
The trunk and thigh represent an esthetic unit. In elderly patients with lipedema, central obesity and laxity of the abdominal tissue influence this esthetic unit in a negative way. In many elderly patients with lipedema, anteromedial thigh laxity is worsened by descent of the lower abdominal tissues.
The medial thigh usually has a relatively thin dermal compartment separated by lamina profunda strati subcutanei from two separate layers of adipose tissue. Colles’ fascia defines the border between the adipose layers attached to the ischiopubic area of the pelvic bone, anteriorly to Scarpa’s fascia and posteriorly to the urogenital diaphragm. The Scarpa’s triangle contains major vascular structures like the vena femoralis, vena saphena, vena pudenda, vena circumflexa iliaca, femoral artery, and lymphatic vessels. This area needs to be protected during surgery to avoid complications during surgery, such as secondary lymphedema and major bleeding.11
Procedures
We begin with removal of the excess adipose tissue by microcannular laser-assisted liposuction under tumescent anesthesia. For safety reasons, we limit the tumescent solution to a maximum of 5 liters per session. Liposuction is performed in 4–5 sessions. The laser equipment consists of a 980 nm diode laser with the bare fiber integrated into the liposuction cannula. Details of the technique have been described elsewhere.5,7
Medial thigh lift
Patients with advanced lipedema after liposuction usually have a vertical tissue excess propagated by the looser adherence of skin and adipose layers of the medial thigh. The major aim of the thigh lift is an esthetic leg shape. We wait at least 4 months after liposuction before performing a medial thigh lift.
The incision lines are marked preoperatively in a standing position. Surgery is performed under general anesthesia in the supine position with the legs bent. We start with a proximal line incision below the crease between the thigh and perineum. In contrast with the Lockwood technique, the incision line does not cross the ligamentum inguinale lateroapically.12 These patients are not searching for a “bikini” look, which makes the surgery easier. It also circumvents displacement of the labia major as a possible risk of Lockwood’s technique. Skin and adipose tissue are resected en bloc in an anterior-posterior direction respecting the Scarpa’s triangle. Careful blood vessel coagulation is done by bipolar diathermy. A bottle-neck incision is performed in the vertical direction from the upper thigh to the medial knee. The tissue around the major saphenous vein has to be protected since major lymphatics follow the vein. We perform only minimal undermining for the horizontal and vertical incisions using the technique described by del Pino Roxo et al.13 The wounds are closed starting from the horizontal incision by suturing the upper and lower skin flap with Colles’ fascia using 0 Vicryl or 0 PDS, in this way, the tension on superficial scars is reduced. The vertical incision is sutured in three layers with absorbable 2-0 PDS and 3-0 PDS. We do not use drains because there is little undermined tissue. The upper legs are taped and a compression garment is worn for 6 months.
Lower partial abdominoplasty
The major aim of this procedure is to remove large skin/fat folds from the lower abdomen. Surgical planning is performed in a standing position. Since the trunk and thighs form one esthetic unit, improvement of the lower trunk will also improve the thighs. The procedure is performed under general anesthesia with the patient in a supine position. The incision usually begins in the pubis area with a median horizontal incision followed by lateroapical incisions to the spinae iliacae anteriores superiores completed by the upper horizontal incision. The upper horizontal line is below the umbilicus. Preparation of the skin-adipose tissue flap goes along Scarpa’s fascia. We perform the dermatolipectomy en bloc. Bleeding vessels need careful coagulation by diathermy. The wounds are sutured in three layers with 2-0 and 3-0 PDS. Sutures are taped. Patients wear a compression girdle for about 12 weeks.14 The procedure can be combined with correction of pubis ptosis and bulging. We perform the procedure in the same session as lower abdominoplasty. After Y-sized incision and removal of adipose tissue and flaccid skin, a dermal-fascial suspension is performed according to the method described by El-Khatib and the defect is sutured in the three-layer technique outlined above.15
Safety concerns
Because we are not dealing with young and healthy patients, the risk of complications is higher. Interdisciplinary team work with colleagues from internal medicine, anesthesiology, and rehabilitative medicine is important to reduce the surgical and postsurgical risks as far as possible. Patients should refrain from smoking for at least 2 weeks before and until 4 weeks after surgery. Antiplatelet drugs should also be stopped. Tumescent anesthesia reduces the risk of thromboembolic complications after liposuction by immediate mobilization after surgery. The other procedures performed under general anesthesia warrant low molecular heparin/heparinoids after surgery.
We prefer tumescent anesthesia with prilocaine because of the lower cardiotoxicity compared with lidocaine. Prilocaine requires monitoring of methemoglobin levels for 24 hours. In the event of symptomatic methemoglobinemia or methemoglobin levels ≥20%, intravenous toluidine blue solution is used as an antidote.
Chemoprophylaxis is not usually necessary during liposuction, but may be useful in patients with diabetes for abdominoplasty and thigh lift. Early mobilization of patients and rehabilitation is important for the final outcome. Manual lymph drainage and compression garments reduce the time to healing and ensure an uneventful healing process.16
Patients
The combined procedure was performed in three female patients with lipedema grade 3 according to Meier-Vollrath and Schmeller3 and multiple comorbidities (Table 1). The women were aged 55, 72, and 77 years and their body mass index was 33, 35, and 42, respectively. Their surgical risk was assessed by American Society of Anesthesiology physical status classification.17 All patients were scored class 3, ie, as having severe systemic disease (Table 1). Satisfaction with the outcome was classified as –1 (dissatisfied), 0 (no improvement), 1 (partly satisfied), 2 (satisfied), or 3 (very satisfied).
Table 1.
Patient characteristics
| Patient | Age (years) | BMI | Comorbidities |
|---|---|---|---|
| 1 | 55 | 33 | Coxarthrosis and gonarthrosis, diabetes mellitus, arterial hypertension, multiple drug and contact allergies |
| 2 | 72 | 35 | Arterial hypertension, atopic dermatitis, osteoarthritis, venous insufficiency |
| 3 | 77 | 42 | Dilated cardiomyopathy, diabetes mellitus with renal insufficiency, pulmonary hypertension, coxarthrosis and gonarthrosis |
Abbreviation: BMI, body mass index.
Results
Laser-assisted liposuction was performed in 3–5 sessions under tumescent anesthesia with an overnight stay in hospital for methemoglobinemia monitoring. In total, 4–6 liters of lipoaspirate was harvested. All patients developed methemoglobinemia within the 12 hours following liposuction that was treated by intravenous toluidine blue solution and normalized within 20 minutes. Patients received individual nonelastic flat knitted compression garments for a postsurgical period of 6 months. Mobilization was started on the day of liposuction. Manual lymph drainage was done in an outpatient setting on a regular basis, starting 2 weeks after liposuction. The procedures were well tolerated. No major adverse effects were seen.
All other procedures were performed under general anesthesia with close monitoring by the anesthesiologist. Pain control was undertaken in collaboration with the anesthesiology department. Early mobilization was started between 2 and 4 days after surgery. No wound infection or bleeding was observed, but bruising was evident in all patients. Again, a flat knitted compression garment (pressure 46 mmHg) was recommended in the follow-up period (12 hours a day for the first 2 months and at least 8 hours a day for a minimum of 4 months). Moisturizers were recommended for skin and scar care. There was no major reduction in body mass index (33 to 31.8, 35 to 33, and 42 to 39.5). Loss of body weight was 5–10 kg by the multiple-step approach. Clothing size was reduced by 2 to 3 sizes. No procedure-induced secondary lymphedema was seen and there was no recurrence of lipedema during a follow-up period of 2–4 years. Patients were satisfied with the final outcome (Figures 1–3), which was grade 3 (for patients 1 and 3) or grade 2 (for patient 2). All patients continue to use the compression garment during the day.
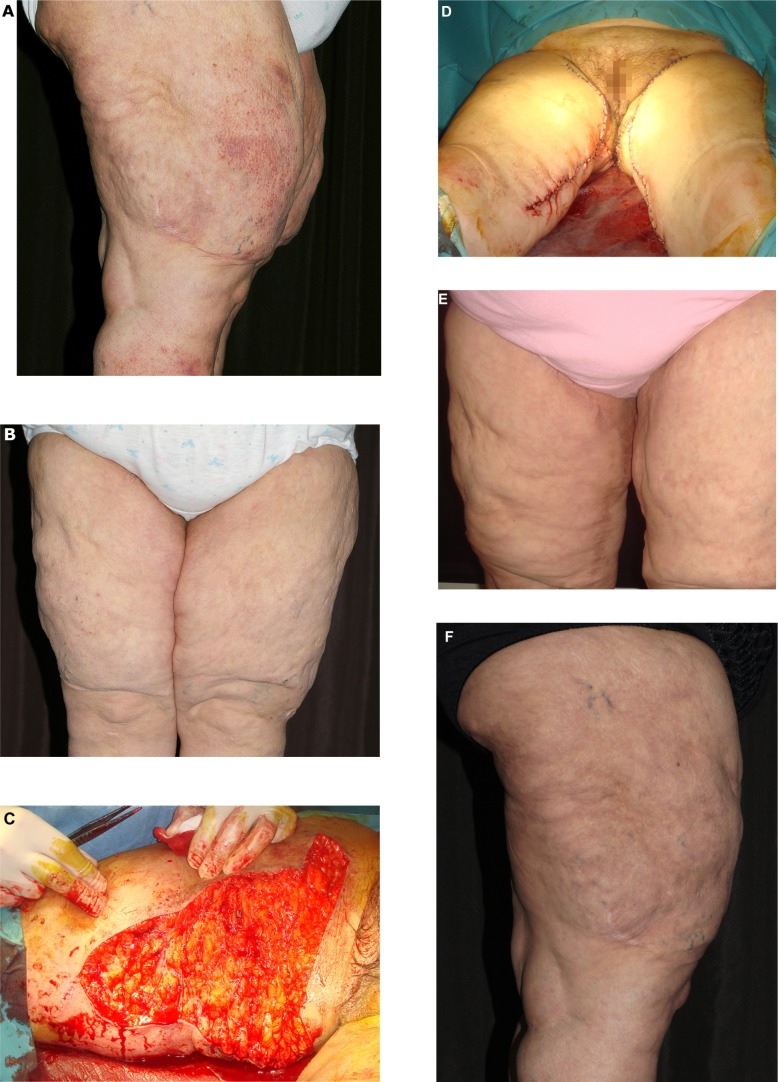
Figure 1.

A 72-year-old woman with lipedema grade 3 according to the Meier-Vollrath and Schmeller classification.3 She had had an unsuccessful lipectomy of the upper legs a couple of years earlier (see suprapatellar scars). (A) and (B) Initial presentation with side and front view. (B) Operation site of medial thigh lift. (C) Operation site of medial thigh lift. (D) After suturing. (E) About 4 weeks later. (F) and (G) Outcome of the thigh lift with improved tissue laxity about 8 weeks later.
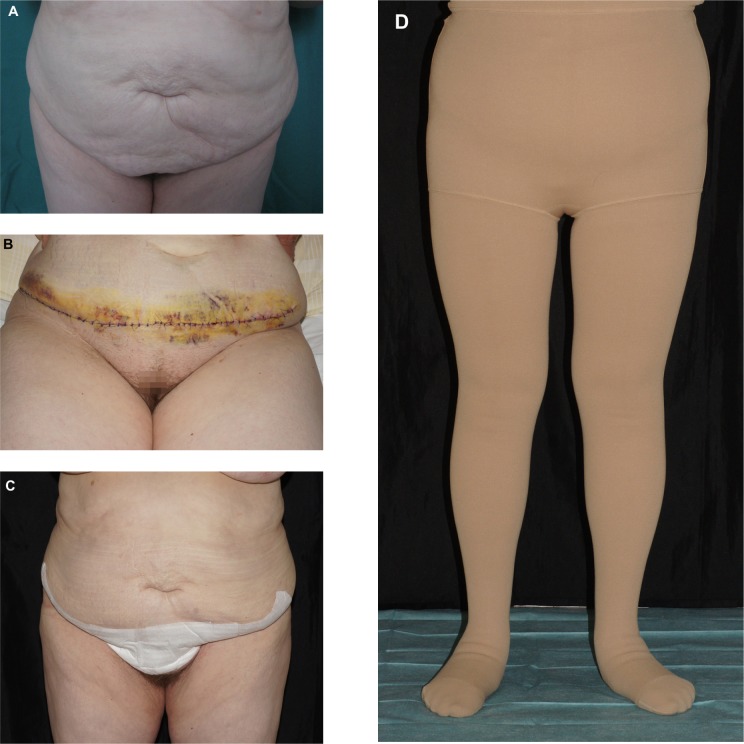
Figure 3.
A 55-year-old woman with lipedema grade 3 according to the Meier-Vollrath and Schmeller classification.3 (A) Before lower abdominal lipoplasty. (B) Four days after surgery, with minor bruising. (C) Two weeks after lower abdominoplasty, showing markedly improved body contour. (D) Patient with tailored compression garment.
Discussion
Lipedema is a disabling disease with a negative impact on quality of life.1,4 No casual treatment is available. On the other hand, stable improvement has been achieved with liposuction,4–8 and is greater in advanced stages of the disease.4
Patients with advanced lipedema often suffer from comorbidities that have to be considered in the treatment plan.7 Therefore, selection of surgical procedures and anesthesia has to balance the risks and benefits very carefully. This has an impact not only on liposuction, where tumescent anesthesia should not exceed 5 liters per session, but on the other surgical techniques described here as well.4–7 For tumescent anesthesia, we used prilocaine instead of lidocaine given that prilocaine has the lowest potential of all amide anesthetics to fluidize the bilayer membranes and therefore has the least cardiotoxicity.18 The major adverse effect is methemoglobinemia, which needs to be monitored for. Treatment with toluidine blue is very effective.19,20
Although there is evidence of improvement in skin laxity by subdermal laser application in nonobese patients, elderly patients with advanced lipedema require further attempts to achieve a good functional and esthetic outcome.9,10 Here we described a modified surgical approach combining medial thigh lift and lower abdominoplasty to meet the special needs of these multimorbid elderly patients. For medial thigh lift, a simple procedure with a short operation time (<2 hours) was chosen. The horizontal scars were placed more distally compared with the Lockwood technique, circumventing possible displacement of the labia major.11,12 Displacement of the labia major can be a severe problem in elderly women with pelvic floor weakness.
The lower partial abdominoplasty performed here is capable of preventing skin problems like intertrigo with mycotic or bacterial infection of the abdominal folds, which would be aggravated by a compression garment.21 We used an en bloc dermatolipectomy which can be combined with correction of pubic bulging and ptosis in the same session if necessary. Minimal undermining was preferred for both medial thigh lift and lower partial abdominoplasty to reduce the risk of postsurgical bleeding and development of seroma. Using this approach, the time to complete healing can be shortened.13,14
Recent investigations provide evidence of stable reduction of adipose tissue using liposuction and abdominoplasty.4,7,22 This is in line with our experience in this case series. In addition, elevated triglyceride levels and leukocyte counts have been shown to decrease after liposuction and abdominoplasty.23 Our patients were satisfied with their combined individually tailored approach and the procedures used were safe but monitored carefully. Early rehabilitation with a compression garment is important after surgery to avoid postoperative complications.24
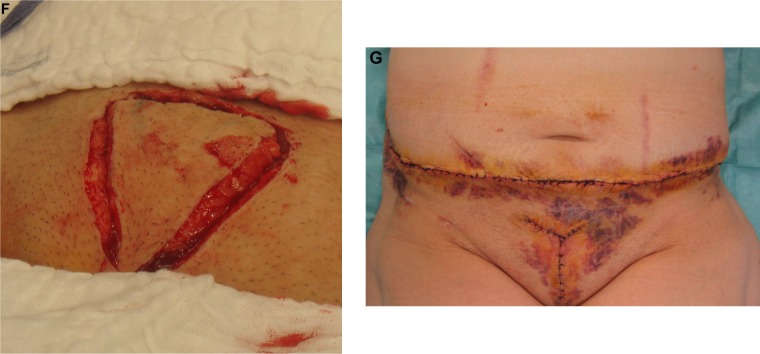
Figure 2.
A 77-year-old woman with lipedema grade 3 according to the Meier-Vollrath and Schmeller classification.3 (A) Asymmetric proximal lipedema of the legs, laxity of the abdominal skin, and ptosis and bulging of the pubic area. (B) After laser-assisted liposuction and correction of thigh laxity by medial thigh lift 6 days after surgery. (C) Medial thigh lift. (D) Lower abdominoplasty with skin and adipose tissue resection. Scarpa’s fascia is exposed. (E) Cross view of resection specimen demonstrating the massive enlarged fat lobules of the deeper layer of adipose tissue. (F) Puboplasty. (G) Result 3 days after surgery. Some minor bruising is still evident but contours has been markedly improved.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Child AH, Gordon KD, Sharpe P, et al. Lipedema: an inherited condition. Am J Med Genet A. 2010;152A(4):970–976. doi: 10.1002/ajmg.a.33313. [DOI] [PubMed] [Google Scholar]
- 2.Suga H, Araki J, Aoi N, Kato H, Higashino T, Yoshimura K. Adipose tissue remodeling in lipedema: adipocyte death and concurrent regeneration. J Cutan Pathol. 2009;36(12):1293–1238. doi: 10.1111/j.1600-0560.2009.01256.x. [DOI] [PubMed] [Google Scholar]
- 3.Meier-Vollrath I, Schmeller W. Lipoedema – current status, new perspectives. J Dtsch Dermatol Ges. 2004;2(3):181–186. doi: 10.1046/j.1439-0353.2004.04051.x. [DOI] [PubMed] [Google Scholar]
- 4.Schmeller W, Hueppe M, Meier-Vollrath I. Tumescent liposuction in lipeodema yields good long-term results. Br J Dermatol. 2012;166(1):161–168. doi: 10.1111/j.1365-2133.2011.10566.x. [DOI] [PubMed] [Google Scholar]
- 5.Wollina U, Goldman A, Heinig B. Microcannular tumescent liposuction in advanced lipedema and Dercum’s disease. G Ital Dermatol Venereol. 2010;145(2):151–159. [PubMed] [Google Scholar]
- 6.Rapprich S, Dingler A, Podda M. Liposuction is an effective treatment for lipedema – results of a study with 25 patients. J Dtsch Dermatol Ges. 2011;9(1):33–40. doi: 10.1111/j.1610-0387.2010.07504.x. [DOI] [PubMed] [Google Scholar]
- 7.Wollina U, Heinig B. Tumescent microcannular (laser-assisted) liposuction in painful lipedema. Eur J Aesthet Med Dermatol. 2012;2(2):56–69. [Google Scholar]
- 8.Peled AW, Slavin SA, Brorson H. Long-term outcome after surgical treatment of lipedema. Ann Plast Surg. 2012;68(3):303–307. doi: 10.1097/SAP.0b013e318215791e. [DOI] [PubMed] [Google Scholar]
- 9.DiBernardo BE. Randomized, blinded split abdomen study evaluating skin shrinkage and skin tightening in laser-assisted liposuction versus liposuction control. Aesthet Surg J. 2010;30(4):593–602. doi: 10.1177/1090820X10380707. [DOI] [PubMed] [Google Scholar]
- 10.Goldman A, Wollina U, de Mundstock EC. Evaluation of tissue tightening by the subdermal Nd: YAG laser-assisted liposuction versus liposuction alone. J Cutan Aesthet Surg. 2011;4(2):122–128. doi: 10.4103/0974-2077.85035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Labardi L, Gentile P, Gigliotti S, et al. Medial thighplasty: horizontal and vertical procedures after massive weight loss. J Cutan Aesthet Surg. 2012;5(1):20–25. doi: 10.4103/0974-2077.94330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lockwood T. Lower body lift with superficial fascial system suspension. Plast Reconstr Surg. 1993;92(6):1112–1122. [PubMed] [Google Scholar]
- 13.Del Pino Roxo, Wenck Roxo, AC Varela V. [Thigh lift with minimal undermining] In: Von Heimburg D, Lemperle G, editors. [Aesthetic Surgery, 27th Complementary] 1–9. XI-3a. Landsberg/Lech: ecomed Medizin; 2012. German. [Google Scholar]
- 14.Del Pino Roxo C, Weck Roxo AC. [Bodylift with minimal undermining] In: Von Heimburg D, Lemperle G, editors. [Aesthetic Surgery, 27th Complementary] 1–12. X-2c. Landsberg/Lech: ecomed Medizin; 2012. German. [Google Scholar]
- 15.El-Khatib HA. Mons pubis ptosis: classification and strategy for treatment. Aesthetic Plast Surg. 2011;35(1):24–30. doi: 10.1007/s00266-010-9552-4. [DOI] [PubMed] [Google Scholar]
- 16.Langer V, Singh A, Aly AS, Cram AE. Body contouring following massive weight loss. Indian J Plast Surg. 2011;44(1):14–20. doi: 10.4103/0970-0358.81439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chand M, Armstrong T, Britton G, Nash G. How and why do we measure surgical risk? J Royal Soc Med. 2007;100:508–512. doi: 10.1258/jrsm.100.11.508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tsuchiya H, Ueno T, Mizogami M, Takakura K. Local anesthetics structure-dependently interact with anionic phospholipid membranes to modify the fluidity. Chem Biol Interact. 2010;183(1):19–24. doi: 10.1016/j.cbi.2009.10.006. [DOI] [PubMed] [Google Scholar]
- 19.Guay J. Methemoglobinemia related to local anesthetics: a summary of 242 episodes. Anesth Analg. 2009;108(3):837–845. doi: 10.1213/ane.0b013e318187c4b1. [DOI] [PubMed] [Google Scholar]
- 20.Kiese M, Lörcher W, Weger N, Zierer A. Comparative studies of toluidine blue and methylen blue on the reduction of ferrihaemoglobin in man and dog. Eur J Clin Pharmacol. 1972;4(2):115–118. doi: 10.1007/BF00562507. [DOI] [PubMed] [Google Scholar]
- 21.Mistiaen P, van Halm-Walters M. Prevention and treatment of intertrigo in large skin folds of adults: a systematic review. BMC Nurs. 2010;9:12. doi: 10.1186/1472-6955-9-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Swanson E. Photographic measurements in 301 cases of liposuction and abdominoplasty reveal fat reduction without redistribution. Plast Reconstr Surg. 2012;130(2):311e–322e. doi: 10.1097/PRS.0b013e3182589ef7. [DOI] [PubMed] [Google Scholar]
- 23.Swanson E. Prospective clinical study reveals significant reduction in triglyceride levels and white blood cell count after liposuction and abdominoplasty and no change in cholesterol levels. Plast Reconstr Surg. 2011;128(3):182e–197e. doi: 10.1097/PRS.0b013e31822213c6. [DOI] [PubMed] [Google Scholar]
- 24.Wagner S. Lymphedema and lipedema – an overview of conservative treatment. Vasa. 2011;40(4):271–279. doi: 10.1024/0301-1526/a000115. [DOI] [PubMed] [Google Scholar]