Abstract
Rare exonic, non-truncating variants in known cancer susceptibility genes such as BRCA1 and BRCA2 are problematic for genetic counseling and clinical management of relevant families. This study used multifactorial likelihood analysis and/or bioinformatically-directed mRNA assays to assess pathogenicity of 19 BRCA1 or BRCA2 variants identified following patient referral to clinical genetic services. Two variants were considered to be pathogenic (Class 5). BRCA1:c.4484G> C(p.Arg1495Thr) was shown to result in aberrant mRNA transcripts predicted to encode truncated proteins. The BRCA1:c.122A>G(p.His41Arg) RING-domain variant was found from multifactorial likelihood analysis to have a posterior probability of pathogenicity of 0.995, a result consistent with existing protein functional assay data indicating lost BARD1 binding and ubiquitin ligase activity. Of the remaining variants, seven were determined to be not clinically significant (Class 1), nine were likely not pathogenic (Class 2), and one was uncertain (Class 3).These results have implications for genetic counseling and medical management of families carrying these specific variants. They also provide additional multifactorial likelihood variant classifications as reference to evaluate the sensitivity and specificity of bioinformatic prediction tools and/or functional assay data in future studies.
Introduction
Identification of missense BRCA1 and BRCA2 unclassified variants during clinical testing poses a problem for clinicians and affected families, given their unclear role in disease risk and tumorigenesis. The multifactorial likelihood model for variant classification has been proposed as a gold standard for variant classification. The method utilizes statistical methods incorporating a prior probability of pathogenicity based on bioinformatic predictions, combined with clinical data from tumor pathology, segregation of the variant with disease, family history and co-occurrence with a deleterious mutation data to assign clinical significance [1], [2]. The model derives a posterior probability of pathogenicity for individual variants, and this posterior probability was used as the basis for a 5-tier classification system with associated clinical recommendations [3].
Refinement of the model is an ongoing process with the potential to improve its accuracy through the inclusion of new findings. These may include results that improve the bioinformatically-based estimation of prior probability of pathogenicity, impact the underlying assumptions for estimation of likelihood ratios, revise existing likelihood ratios based on analysis of larger sample sets, and/or estimate likelihood ratios for new components of the model that represent independent data sources.
For instance, the prior probability for an exonic variant is currently based on bioinformatic prediction of the consequences of the amino acid change and does not take into account the potential for a splicing aberration – an important consideration particularly for exonic variants that occur near to the intron-exon boundary or silent variants predicted to create splicing aberrations [4]. It is now feasible to bioinformatically predict whether such variants create de novo splice sites with reasonable confidence [5], [6], and rigorous calibration of such predictions against in vitro or clinical data will ultimately allow such information to be incorporated into estimates of the prior probability of pathogenicity to improve prediction of pathogenicity for missense variants. As another example, a recent report describing an ovarian cancer patient carrying a pathogenic missense mutation co-occurring in trans with a truncating mutation in BRCA1 [7] indicates inheritance of two pathogenic BRCA1 mutations may not be lethal as first assumed [8], and that the likelihood ratio developed for co-occurrence of BRCA1 variants should be amended to reflect this.
Recent studies have assessed the sensitivity and specificity of BRCA1 BRCT domain and BRCA2 DNA-binding domain functional assays to reflect pathogenicity of variants in these domains [9]–[11]. These studies compared functional assay results to pathogenicity assigned on the basis of clinical data alone, and have established the baseline to incorporate data from these specific functional assays into the multifactorial likelihood model. It is acknowledged that other domains of BRCA1 and BRCA2 are important for function, including the RING, transcriptional activation and BRCA1 c-terminal domains. However, to date, there have been no comprehensive studies calibrating level of function of variants in these domains against clinical information, to assess sensitivity and specificity of relevant assays to indirectly measure cancer risk. In addition, the development and calibration of quantitative splicing assays against direct measures of risk will be important to drive improvements in bioinformatic prediction tools, enhance estimation of bioinformatically-determined prior probabilities, and allow incorporation of mRNA assay data as a likelihood component of the multifactorial model.
In this study, we report the results from multifactorial likelihood modeling and/or bioinformatically-directed splicing assays for 19 BRCA1 and BRCA2 exonic variants to provide variant classifications of direct clinical utility. The combined bioinformatic, splicing and multifactorial likelihood results contribute to the pool of variants with appropriate clinical classification and assay data that can be used as a calibration set of variants for future studies updating the bioinformatically estimated prior probability of pathogenicity for variants, and also incorporating splicing and functional assays into the multifactorial model.
Materials and Methods
Ethics Statement
All families were ascertained as eligible for research by kConFab (http://www.kconfab.org/Index.shtml) [12], apart from two families for which the proband was identified directly by clinical testing in Familial Cancer Clinics. BRCA1:c.4484G>C(p.Arg1495Thr) was identified by BRCA1 mutation screening and referred to the Genetics Department of the Canberra Hospital, Canberra, Australia. Another family carrying the BRCA1:c.122A>G(p.His41Arg) variant was recruited by the Familial Service, Westmead Hospital, Westmead, NSW, Australia. De novo lymphoblastoid cell lines (LCLs) were established for this study by kConFab, with approval by the Peter Mac Institutional Review Board. Written, informed consent was obtained for all patient samples used and approval was gained from the QIMR Berghofer Human Research Ethics Committee and the Peter Mac Human Research Ethics Committee. All research was conducted in Australia.
Nucleotide numbering reflects cDNA numbering with +1 corresponding to the A of the ATG translation initiation codon in the reference sequence of BRCA1 (GenBank accession #NM_007294.3) and BRCA2 (GenBank accession #NM_000059.3). All 19 exonic variants investigated were considered to be of uncertain clinical significance by the kConFab mutation review committee, or by the investigators (BRCA1:c.4484G>C(p.Arg1495Thr)) at the time of selection for the study.
Bioinformatic Splice Predictions
For all 19 variants investigated, three bioinformatic splice prediction programs (HSF matrices, MaxEntScan and NNsplice) were used to predict whether de novo splice sites may be created by variants or whether the variant has an effect on the intron-exon boundary. One program (ESEfinder) was used to assess the effect of a variant on potential exonic splice enhancers. Human Splicing Finder version 2.4 (www.umd.be/HSF/) combines HSF matrices, MaxEnt Scan and ESEfinder in one web interface [13]–[15], and variant nomenclature was input into HSF as in standard HGVS format. Sequences of 25 nucleotides flanking each side of the variant were entered into NNsplice (http://www.fruitfly.org/seq_tools/splice.html) [16]). The difference between variant and wild-type output scores was expressed as a proportion of wild-type scores for HSF matrices and MaxEntScan. Scores for the proximal consensus splice site for all programs were derived by entering the exact sequence at the intron-exon boundary. mRNA assays were prioritized for all variants with existing LCLs, and also for two additional variants where bioinformatic prediction suggested that mRNA splicing might be altered by the variant, namely BRCA1:c.4484G>C(p.Arg1495Thr) and BRCA2 c.7828G>A (p.Val2610Met) (Table 1).
Table 1. Bioinformatic splice prediction scores* and in-vitro splicing assay results.
| Variant | Human Splicing Finder | MaxEntScan | NNsplice | ESEfinder | In-vitro splicing assay result | ||||
| Variant | Proximal consensus site | Variant | Proximal consensus site | Variant | Proximal consensus site | ||||
| BRCA1 | c.4484G>C p.Arg1495Thr) | Donor 85.7 (−11.4%) | 96.71 | Donor 7.69 (−27.2%) | 10.57 | Donor 0.97 | 1.00 | No enhancer motif | Δexon 14 and Δexon 14/15 |
| c.4991T>C(p.Leu1664Pro) | Acceptor 71.97 (−2.5%) | 87.03 | NSC | 6.69 | NSC | 0.61 | SF2/ASF: 71.23 (+11.40%) | no aberration | |
| BRCA2 | c.440A>G(p.Gln147Arg) | Donor 64.23 (−1.24%) | 88.86 | NSC | 9.46 | NSC | 0.99 | SC35: new site SRp40: site broken | no aberration |
| c.1514T>C (p.Ile505Thr) | Acceptor 85.55 (+0.49%) | 85.7 | NSC | 9.62 | NSC | 0.90 | No enhancer motif | no aberration | |
| c.7521A>G (p. = ) | Acceptor 75.63 (−0.09%) | 82.1 | Donor 6.52 (+3.82%) | 6.97 | NSC | 0.90 | SF2/ASF (IgM-BRCA1): 88.38 (+20.16%) SF2/ASF: 88.53 (+20.35%) | no aberration | |
| c.7828G>A (p.Val2610Met) | Donor 89.26 (+1.32%) | 73.16 | Donor 9.99 (+57.57%) | 3.1 | Donor 1.00 | NSC | SRp55∶74.69 (+4.97%) | no aberration | |
| c.8734G>A (p.Ala2912Thr) | Acceptor 75.26 (+0.09%) | 82.1 | NSC | 6.97 | NSC | 0.98 | SF2/ASF (IgM-BRCA1): site broken SF2/ASF: site broken | no aberration | |
Bracketed percentages refer to the difference between variant and wild-type scores as a proportion of the wild-type score. NSC, no sites created (no scores provided by bioinformatic program output). Positive values for HSF matrices and MaxEntScan represent an increased likelihood of creating a de novo site when compared with the wild-type sequence where the variant occurs. Negative values represent a decreased likelihood. Positive values for ESEfinder represent an increase in strength for the enhancer motif as a result of the variant. The proximal consensus site is taken as the donor or acceptor site of the exon in which the variant occurs. Variant scores for NNsplice are for splice sites created by the variant, except for BRCA1:c.4484G>C (p.Arg1495Thr) for which the variant score is for the consensus splice junction in the presence of the variant.
mRNA Splicing Assays
For BRCA1:c.4484G>C(p.Arg1495Thr), a blood sample was taken from the variant carrier using an RNA stabilising, PaxGene tube and RNA extracted within 24 hrs using the PAXgene Blood RNA Kit (Qiagen, Doncaster, Victoria, Australia). A blood sample was collected from one female healthy control using the same sample collection and RNA extraction protocol, for comparison in the splicing assay. For the remaining variants assessed, culture of LCLs was conducted without and with cycloheximide, where treated LCLs were grown in the presence of cycloheximide (100 mg/ml) for 4 hours to stabilize transcripts against nonsense mediated decay (NMD) to assist detection of aberrant mRNA products [17]. RNA was extracted from cycloheximide untreated and treated cell lines using the RNeasy Mini Kit (Qiagen), according to the manufacturer’s instructions. Each RNA sample was treated with DNase to minimize DNA contamination using DNA-free Kit (Ambion, Austin, TX, USA). cDNA was synthesised using Superscript III First Strand Synthesis System (Invitrogen). PCR amplification was performed using Amplitaq Gold (Applied Biosystems, Mulgrave, Victoria, Australia) under the following conditions: 95°C for 7 minutes followed by 35 cycles of 94°C for 30 seconds, 55°C for 30 seconds and 72°C for 1–2 minutes and a final extension step at 72°C for 7 minutes (See Table S1 for details of primers). PCR products from the BRCA1:c.4484G> C(p.Arg1495Thr) carrier were purified using QIAquick PCR Purification Kit (Qiagen), cloned using pGEM-T Vector (Promega, Auburn, Victoria, Australia) and sequenced using Big-Dye Terminator version 3.1 sequencing chemistry and the ABI 377 sequencer (Applied Biosystems). The interpretation of the clinical significance of variants based on splicing data was as described in Walker et al [18].
Multifactorial Likelihood Analysis
Data relevant for multifactorial analysis was available for all variants except BRCA1:c.4484G>C(p.Arg1495Thr). Information on segregation was available for all families, and likelihood ratios (LRs) based on tumor pathology (ER and grade for BRCA1 and tubule formation for BRCA2) [19], co-occurrence and family history was available for a subset the variants (Table 2). Multifactorial analysis was conducted using the methods described in Walker et al [20] which incorporates likehoods for segregation [21], tumor pathology [21], [22], co-occurrence [23] and family history [24]. Family History and co-occurrence LRs were derived by querying a Myriad Genetics Laboratories dataset of 70,000 BRCA1 and BRCA2 tests [24]. However, in recognition of the recent report describing a patient with developmental delay and early onset ovarian cancer found to carry two pathogenic BRCA1 mutations [25], for BRCA1 variants we applied the same co-occurrence likelihood ratio formulation derived for BRCA2 variants [8] which takes into consideration presentation of a Fanconi Anemia clinical phenotype in carriers of two pathogenic BRCA2 mutations. Variant classifications follow the IARC criteria outlined in Plon et al. [3], namely: Class 1 not pathogenic posterior probability (pp)<0.001; class 2 likely not pathogenic pp 0.001–0.049; Class 3 uncertain pp 0.05–0.949; Class 4 likely pathogenic pp 0.95–0.99; Class 5 pathogenic pp>0.99. The classification system assigns recommendations related to surveillance and patient management guidelines [3].
Table 2. Classification of BRCA1 and BRCA2 variants on the basis of multifactorial and splicing information.
| Variant | A-GVGD | A-GVGD prior probability | Segreg-ation | Tumor Patho-logy | Co-occurrence | Family History | Odds for Causality | Posterior Probability of Pathogenicity | IARC Class | Splicing class | |
| BRCA1 | c.122A>G(p.His41Arg) | C25 | 0.29 | 159.17 | 2.95 | – | – | 469.56 | 0.995 | Class 5 | – |
| c.2759T>C (p.Val920Ala) | C0 | 0.01 | 0.002 | – | – | – | 0.002 | 1.52×10−5 | Class 1 | – | |
| c.4484G>C(Arg1495Thr) | C0 | 0.01 | – | – | – | – | – | – | – | Class 5 | |
| c.4991T>C (p.Leu1664Pro) | C0 | 0.01 | 0.01 | – | 1.29 | 0.03 | 0.0003 | 3.89×10−6 | Class 1 | Class 1 | |
| BRCA2 | c.1354C>A (p.Leu452Ile) | C0 | 0.01 | 0.03 | – | – | – | 0.03 | 0.0003 | Class 1 | – |
| c.440A>G (p.Gln147Arg) | C0 | 0.01 | 1.38 | 1.20 | 1.07 | 0.78 | 1.37 | 0.014 | Class 2 | Class 1 | |
| c.1514T>C (p.Ile505Thr) | C0 | 0.01 | 0.16 | 1.20 | – | – | 0.191 | 0.002 | Class 2 | Class 1 | |
| c.4609G>A (p.Glu1537Lys) | C0 | 0.01 | 0.004 | – | – | – | 0.004 | 4.24×10−5 | Class 1 | – | |
| c.5070A>C (p.Lys1690Asn) | C0 | 0.01 | 0.48 | – | 0.30 | 3.23×10−5 | 4.55×10−6 | 4.59×10−8 | Class 1 | – | |
| c.5278T>G (p.Ser1760Ala) | C0 | 0.01 | 1.38 | 0.14 | – | – | 0.1977 | 0.002 | Class 2 | – | |
| c.5714A>G (p.His1905Arg) | C0 | 0.01 | 0.16 | – | – | – | 0.16 | 0.0016 | Class 2 | – | |
| c.6172T>A (p.Phe2058Ile) | C15 | 0.29 | 0.04 | – | 1.12 | 0.20 | 0.008 | 0.003 | Class 2 | – | |
| c.6322C>T (p.Arg2108Cys) | C0 | 0.01 | 0.06 | – | – | – | 0.06 | 0.0006 | Class 1 | – | |
| c.7521A>G (p. = ) | SYN | 0.01 | 0.01 | – | – | – | 0.01 | 9.89×10−5 | Class 1 | Class 1 | |
| c.7534C>T (p.Leu2512Phe) | C0 | 0.01 | 0.11 | – | – | – | 0.11 | 0.0011 | Class 2 | – | |
| c.7828G>A (p.Val2610Met) | C15 | 0.29 | 0.83 | – | – | – | 0.8288 | 0.25 | Class 3 | Class 1 | |
| c.8734G>A (p.Ala2912Thr) | C0 | 0.01 | 0.14 | – | – | – | 0.14 | 0.0014 | Class 2 | Class 1 | |
| c.9038C>T (p.Thr3013Ile) | C0 | 0.01 | 0.23 | – | – | – | 0.23 | 0.002 | Class 2 | – | |
| c.9364G>A (p.Ala3122Thr) | C0 | 0.01 | 0.34 | – | – | – | 0.34 | 0.0034 | Class 2 | – | |
Classifications for multifactorial likelihood as described in Plon et al. (3) and splicing as described in Spurdle et al. (32). Frequency data from 1000 Genomes and EVS datasets is available for a subset of the variants studied (Table S2). Information used to determine tumor pathology LRs was as follows: BRCA1c.122A>G(p.His41Arg) - one ER-positive Grade 3 tumor; BRCA2 variants c.440A>G (p.Gln147Arg) and c.1514T>C (p.Ile505Thr) - tubule formation present in <10% of tumor; BRCA2:c.5278T>G (p.Ser1760Ala) – tubule formation in >75% tumor.
Data Access
After peer-review and publication, the variants analysed and findings from this study will be submitted to several public databases: the LOVD literature unclassified variant database (http://chromium.liacs.nl/LOVD2/cancer/home.php?select_db=BRCA1); the LOVD-IARC ex-UV database (http://brca.iarc.fr/LOVD/home.php?select_db=BRCA1) which shows results from multifactorial likelihood analyses of BRCA variants; the BIC database (http://research.nhgri.nih.gov/bic/) which collates information from these databases and the scientific literature to derive a curated, publicly available classification source.
Results
Bioinformatic Analysis of Variants
HSF, MaxEntScan and NNsplice predicted a reduction in splice site strength at the intron-exon boundary for BRCA1:c.4484G> C(Arg1495Thr), which occurs in the last nucleotide of exon 14 and a strongly increased de novo splice site attributable to BRCA2:c.7828G>A(p.Val2610Met) (Table 1). Changes to normal splicing for the other 17 variants were very modest (<25% difference between wildtype and variant values) and/or variant score was considerably lower than expected for donor/acceptor sites at the consensus sequence at intron-exon boundaries. Of the variants investigated using mRNA assays (Table 1), ESEfinder predicted potential disruption of binding of splice regulatory proteins for BRCA2c.440A>G(p.Gln147Arg) and c.8734G>A (p.Ala2912Thr), and a new site or increase in binding for BRCA2c.440A>G(p.Gln147Arg) and three other variants.
mRNA Analysis Reveals that BRCA1:c.4484G>C(Arg1495Thr) Produces Two Aberrant Transcripts with Whole Exon Deletions
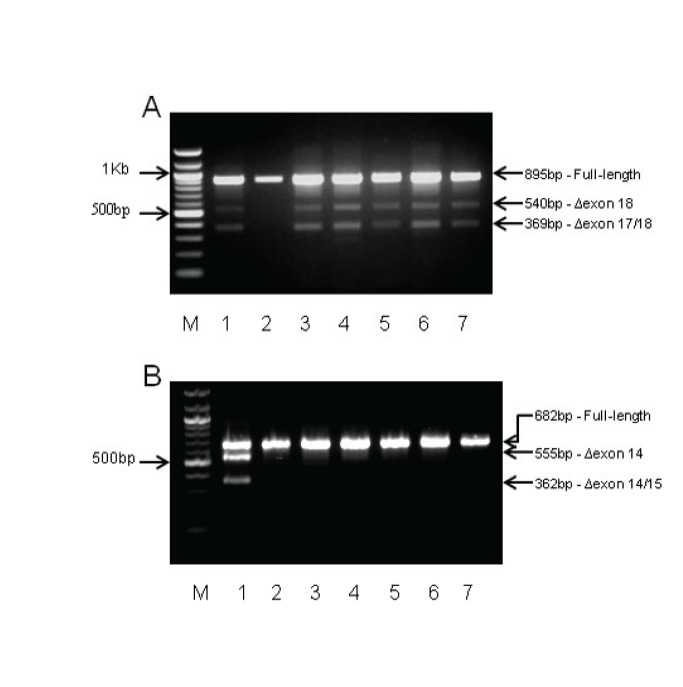
As described in the methods, mRNA splicing assays were performed for a subset of 7 variants selected according to existing availability of material, and bioinformatic predictions that justify performing mRNA assays (Table 1). Despite predictions of an increased likelihood of creating a de novo donor site by MaxEntScan for BRCA2:c.7828G>A(p.Val2610Met), there was no evidence for the predicted aberration from RT-PCR analysis (Figure 1A).
Figure 1. RT-PCR results for BRCA1 c.4484G>C(p.Arg1495Thr) and BRCA2:c.7828G>A (p.Val2610Met).
M - 100bp DNA marker (New England Biolabs). A) BRCA2:c.7828G>A (p.Val2610Met). Lane 1: RT-PCR products from variant carrier derived cycloheximide treated LCL. Lane 2–7: Cycloheximide treated LCLs from unaffected female controls. There is no evidence for a predicted loss of 149bp from exon 17 as a result of a de novo donor site. The Δexon 18 (540bp) and Δexon 17/18 (369bp) are detected in the variant carrier and all but one control samples. B) BRCA1 c.4484G>C(p.Arg1495Thr). Lane 1: RT-PCR products from whole blood derived RNA from the variant carrier showing the Δexon 14 and Δexon 14/15 splicing aberration. Lane 2: RT-PCR carried out on whole blood derived RNA from an unaffected female control (collection and extraction methods as per the variant carrier). Lane 3–7: Cycloheximide treated LCLs from unaffected female controls.
Aberrant mRNA splicing was detected experimentally for the other variant for which there was a bioinformatic prediction of an effect on splicing: BRCA1: c.4484G>C(p.Arg1495Thr) variant located at the last base of exon 14. Consistent with the prediction by HSF and MaxEntScan of loss of a donor site, two aberrant splice products were detected by gel electrophoresis of RT-PCR products in the variant carrier but not in controls (Figure 1B). Sub-cloning and sequencing of the PCR products confirmed that the 555 bp splice product contains an out-of-frame deletion of exon 14 predicted to encode a truncating protein, although the presence of the stop codon will likely result in degradation by nonsense-mediated decay (NMD). The 362 bp product was shown to represent a transcript with an in-frame deletion of exon 14/15, covering the BRCA1 transactivation domain. The full-length product was extracted from the agarose gel following electrophoresis and sequenced. Only wild-type sequence was evident in the chromatogram data suggesting that the variant allele does not produce full-length transcript.
Multifactorial Likelihood Analysis
As shown in Table 2, classifications after multifactorial analysis of the 18 of the 19 exonic variants assessed were: class 1 (not pathogenic) for 7 variants, class 2 (likely not pathogenic) for 9 variants, class 3 (uncertain) for 1 variant, and class 5 (Pathogenic) for 1 variant. The posterior probability of pathogenicity for BRCA1:c.122A>G(p.His41Arg) was 0.995, driven predominantly by a strong co-segregation score (159.17) calculation from two families. BRCA1:c.2759T>C(p.Val920Ala) and BRCA2:c.5278T>G(p.Ser1760Ala) were previously analyzed by multifactorial likelihood analysis and were determined to be Class 3 and Class 2 respectively, based on the data available at that time [22]. The Bayes odds for BRCA1:c.2759T>C (p.Val920Ala) was 0.9811 in the initial study [22] and genotyping of additional family members in this study lowered the Bayes segregation odds to 0.002, resulting in a revised posterior probability of 1.52×10−5 (Class 1). For BRCA2:c.5278T>G(p.Ser1760Ala), additional genotyping of six individuals changed the Bayes segregation odds from 1.17 in the initial study to 1.38 in this study but did not alter the Class 2 classification.
Discussion
Results from this study provide evidence of pathogenicity for the two variants BRCA1:c.4484G>C(p.Arg1495Thr) and BRCA1:c.122A>G(p.His41Arg), and indicate that another 16 variants are not associated with high risk of cancer (Class 1 or 2). These findings are of direct relevance for counselling and management of individuals found to carry these variants. They also highlight the need for ongoing collection of clinical data to facilitate classification, as recommended for variants that fall into IARC Class 2, 3 or 4 [3]. Specifically, the inclusion of additional genotypes into the Bayes segregation analysis for BRCA1:c.2759T>C(p.Val920Ala) was a major factor which led to reclassification of this variant from Class 2 to Class 1.
The BRCA2:c.7828G>A(p.Val2610Met) variant which fell into Class 3 on the basis of multifactorial likelihood modelling was also investigated using mRNA assays since bioinformatic analysis using HSF, MaxEntScan and NNsplice predicted a splice donor. The lack of splicing aberration indicates the variant is in fact not deleterious due to effect on splicing. Given only modest likelihood of an effect on protein function (prior probability of 0.29 based on missense effect, conservation and location), further clinical information will be most helpful to resolve the clinical significance of this variant.
Bioinformatic splice prediction of a de novo donor for BRCA2:c.7828G>A(p.Val2610Met) was not confirmed experimentally, with no evidence observed for a splicing aberration caused by this variant. The sequence at the next downstream intron-exon boundary is CAGgcaagt, which contains a gc dinucleotide rarely observed at the intron-exon boundary. NNsplice did not predict a splice junction, and the score for the donor sequence at this motif was 3.1 for MaxEntScan and 73.16 for HSF. This compared to 9.99 (MaxEntScan) and 89.26 (HSF) for the de novo donor predicted for the variant. That is, the higher bioinformatic scores for the variant suggest that the de novo motif should out-compete the motif at the intron-exon boundary, and the normal splicing profile observed for this variant is thus surprising. This finding raises the possibility that splicing regulation in this region may be strongly dependent on cis-acting regulatory motifs and accessibility for the polypeptides and small nuclear RNAs that coordinate splicing [20], [26]. While we cannot exclude the possibility that the discrepancy between prediction and assay result reflects tissue-specific splicing events that are restricted to breast epithelium, there is much evidence demonstrating validity of mRNA assays using blood-derived tissue sources. Specifically, 12 of 13 reported naturally-occurring BRCA1 splice variants detected in breast tissue also occur in lymphocytes [27], and we have recently demonstrated the validity of LCLs as a tissue source for routine mRNA assays of gene variants leading to major aberrations [28].
The BRCA1 c.4484G>C(p.Arg1495Thr) variant was shown by our analysis to create aberrant splice products encoding loss-of-function proteins. This variant is located at the last base of exon 14, with increased bioinformatic likelihood to disrupt normal donor function. The exon 14 splicing defect observed in mRNA analysis of BRCA1c.4484G>C(p.Arg1495Thr) was also previously reported for a different variant (BRCA1:c.4484G>T) at the same nucleotide [29], [30]. While RT-PCR is not quantitative and may not reflect the true ratio of full-length to aberrant transcript, the variant allele appears to produce only exon 14 deletion and exon 14/15 deletion transcripts. The exon 14 deletion leads to an out-of-frame transcript, so impact on the protein can be unambiguously inferred from the sequence information. Interpreting the effect of the exon 14/15 in-frame deletion on protein function is not as simple. This deletion falls within a broad TAD region c.3879 to c.5592 defined by BRCA interaction with transcription partners LMO4, JunB and HDACs [31]–[33], but does not incorporate the BRCT regions essential for TAD function [34] and might thus be considered to lie within auxillary activating regions. Further, while there is an example of a variant in exon 13 (BRCA1 p.Leu1407Pro) resulting in loss of transactivation activity [35], the exon14/15 deletion itself would appear to be a poor candidate for loss of transactivation function: it is not well conserved evolutionarily, it is not predicted bioinformatically to alter stability (data not shown), and to our knowledge has not been tested for effect on TAD activity. Nevertheless, the BRCA1 del exon14–15 splicing variant has been demonstrated to impair DNA double-strand break repair and also to interfere with the activity of wildtype BRCA1 in a dominant-negative fashion [36], via loss of non-homologous end-joining activity. Thus, it is appropriate to consider that both aberrant transcripts caused by the BRCA1:c.4484G>T substitution are deleterious to protein function, and to place this variant in Class 5 on the basis of the mRNA assay data. Although, the exercise of interpreting the functional importance of the exon14/15 deletion has highlighted the need to standardize definitions of functional domains in BRCA1 or BRCA2 that consider differences in effects of missense versus in-frame deletions, this interpretation as Class 5 is consistent with the IARC Unclassified Genetic Variants Working Group recommendations [37] recently revised for clarity [18], namely: “variant allele produces only transcript(s) carrying a premature stop codon or an in-frame deletion disrupting known functional domain(s)”.
Together, the results from our mRNA assays highlight the importance of considering potential splice defects for exonic variants, but also the need to improve bioinformatic prediction tools by incorporating information about other motifs and factors important for splicing. The data presented in this study will add to a pool of information that may be used, in the future, to calibrate bioinformatic predictions and/or splicing assay results against cancer risk as measured using clinical data. Such calibration is important, since although mRNA assays are commonly used in clinical testing to detect splicing aberrations and infer pathogenicity, the interpretation of assay data is challenging where the variant allele produces multiple transcripts e.g. a combination of full-length, naturally occurring isoforms, and aberrant transcripts. The ENIGMA Splicing Working group has highlighted the need to move to quantitative assays for future calibration analyses [18], and it is encouraging that appropriate technologies are becoming available, including a pyrosequencing approach allowing accurate measure allelic ratios of splice isoforms in patient RNA [38].
While there are a range of functional assays used to elucidate protein interactions and cellular mechanisms affected by BRCA1 and BRCA2 missense variants, incorporation of functional assay data in the model is at present limited. Firstly, the execution and interpretation of such results is generally limited to specialists in the field. Secondly, functional assays are not a direct measure of cancer risk, and therefore need to be calibrated for sensitivity and specificity against appropriate variants of known clinical significance i.e. “high-risk” pathogenic or clearly not pathogenic variants, located in domains relevant to the functional assay being assessed. The BRCA1:c.122A>G(p.His41Arg) variant classified here as pathogenic by multifactorial analysis is located in the RING domain. The RING-domain spans amino acids 8–96, and includes a binding site for the BARD1 protein [39], which in turn enables the E3 ubiquitin ligase activity of BRCA1 observed at sites of DNA repair [40], [41]. Further, structural changes to the protein involving co-ordination of zinc ions can result in loss of homologous recombination activity [42], [43]. Results from our study add to the body of evidence on the relationship between loss of each of these functions and cancer risk.
As summarized in Table 3, there are 26 variants in the BRCA1 RING-domain that have been tested for BARD1 binding activity and Ubiquitin ligase activity and/or, classified using the multifactorial approach. Several of these variants have also been assessed for loss of function using a homology-directed recombination assay. The p.His41Arg protein has been reported to show weak BARD1 binding capacity and abrogated E3 ubiquitin ligase activity [43]. Considering the remaining 20 variants assessed for BARD1 binding and ubiquitin ligase function, results reported indicate that 6 variants lost both BARD1 binding capacity and ubiquitin ligase activity, 12 variants lost ubiquitin ligase activity with no or inconclusive BARD1 binding (2 variants), one variant lost only BARD1 binding capacity, and another exhibited inconclusive ligase activity.
Table 3. BRCA1 RING-domain variants with reported loss of function on the basis of in-vitro functional assays and/or (likely) clinically significant from multifactorial likelihood analysis.
| BRCA1 Mutation | BARD1Binding | UbiquitinLigase Activity | HomologyDirected Repair | Posteriorprobability | Classification | Ref. |
| p.Val11Ala | Lost | Retained | – | [46] | ||
| p.Ile15Thr | Retained | Abrogated | – | [43] | ||
| p.Met18Lys | Lost | Abrogated | – | [46] | ||
| p.Met18Thr* | Retained | Abrogated | Abrogated | 0.984 | Class 4- Likely pathogenic | [24], [42], [43], [46] |
| p.Leu22Ser | – | – | – | 0.994 | Class 5 - Pathogenic | [47] |
| p.Cys24Arg | Lost | Abrogated | Abrogated | [42], [43], [48] | ||
| p.Ile26Ala | Lost | Abrogated | – | [43] | ||
| p.Leu28Pro | Retained | Inconclusive | – | [43] | ||
| p.Thr37Arg | Lost | Abrogated | Abrogated | [42], [43], [48] | ||
| p.Thr37Lys | – | – | – | 0.999 | Class 5 - Pathogenic | [47] |
| p.Cys39Arg | Retained | Abrogated | – | 0.993 | Class 5 - Pathogenic | [43], [47] |
| p.Cys39Tyr | Lost | – | – | [42] | ||
| p.His41Arg | Weak Binding | Abrogated | Abrogated | 0.995 | Class 5 - Pathogenic | [42], [43], present study |
| p.Cys44Phe | Lost | Abrogated | Abrogated | [42], [43] | ||
| p.Cys44Ser | – | – | – | 0.998 | Class 5 - Pathogenic | [47] |
| p.Cys44Tyr | – | – | – | 0.997 | Class 5 - Pathogenic | [47] |
| p.Lys45Thr | Retained | Abrogated | – | [43] | ||
| p.Lys45Asn | Retained | Abrogated | – | [43] | ||
| p.Cys47Gly | Retained | Abrogated | Abrogated | [42], [43] | ||
| p.Leu52Phe | Inconclusive | Abrogated | No impact | [42], [43], | ||
| p.Cys61Gly* | Lost | Abrogated | Abrogated | 0.999 | Class 5 - Pathogenic | [42], [43], [47] |
| p.Leu63Phe | Retained | Abrogated | – | [43] | ||
| p.Cys64Gly* | Inconclusive | Abrogated | Abrogated | [42], [43] | ||
| p.Ile68Lys | Retained | Abrogated | – | [43] | ||
| p.Ser72Arg | Retained | Abrogated | – | [43] | ||
| p.Thr77Met | Retained | Abrogated | – | [43] |
In all eight instances of abrogated homology directed repair function, abrogated ubiquitin ligase activity function by was also observed, although the reverse is not always the case. For example, there is one variant (p.Leu52Phe) that despite abrogated function by ubiquitin ligase activity had no impact on function in the homology directed repair assay. Of the eight variants, where both ubiquitin ligase activity and homology directed repair showed abrogated function, five also lost or had weak BARD1 binding, one showed inconclusive binding and two retained BARD1 binding (p.Met18Thr and p.Cys47Gly). Taken together, this indicates that different variants may have different effects on the function of the RING domain, and that no single assay should be used to infer loss of function at this point in time. Alternatively, it may be preferable to consider as an alternative assays such as the mouse embryonic stem cell assay [44] with cell proliferation as outcome measure, which can be used to indirectly measure the functional capacity of variants in the RING finger and also other protein domains.
Comparing functional assay results with clinical classification of pathogenicity variants using multifactorial analysis (Class 4 and 5), four variants show variously: abrogated ubiquitin ligase and retained BARD1 binding (p.Met18Thr and p.Cys39Arg); abrogated ubiquitin ligase and weak BARD1 binding activity (p.His41Arg); abrogated ubiquitin ligase activity and lost BARD1 binding (p.Cys61Gly). Each of these four variants also showed abrogated function in the homology directed repair assay except p.Cys39Arg which remains untested. These observations are notable, given the conclusion by Shakya et al. that E3 ubiquitin ligase activity is not required for tumor suppression [45]. Of the remaining variants classified using the multifactorial approach, all Class 5, none have been tested in functional assays. It would be of interest, in order to improve our understanding of the relationship of function to risk, for further studies to assess RING domain functions for these 4 variants, and yet other studies to determine the clinical significance using multifactorial analysis for the 17 variants with existing functional assay data. Such studies will pave the way to incorporation of assays measuring the various functions of the RING finger domain into future multifactorial models.
In summary, our investigations have provided information of clinical utility for 18 of 19 BRCA1 or BRCA2 variants identified by clinical germline testing of breast cancer patients. Our results also provide further evidence that bioinformatic predictions of altered splicing should be incorporated into clinical assessment of variants to prioritize mRNA assays, and used to improve bioinformatic splicing prediction tools and the estimation of the prior probability of pathogenicity for assumed missense alterations. Lastly, the classifications arising from our study will be useful for future studies that correlate functional or splicing assay results against risk.
Supporting Information
Primers for mRNA splicing assays.
(DOCX)
Frequency of variant occurrence in 1000 Genomes and EVS snp datasets.
(DOCX)
Acknowledgments
We thank the many families who participated in this study. We wish to thank Heather Thorne, Eveline Niedermayr, all the kConFab research nurses and staff, the heads and staff of the Family Cancer Clinics, and the Clinical Follow Up Study for their contributions to this resource, and the many families who contribute to kConFab.
Funding Statement
The Clinical Follow Up Study was funded 2001–2009 by NHMRC (www.nhmrc.gov.au) and currently by the National Breast Cancer Foundation (www.nbcf.org.au) and Cancer Australia (www.canceraustralia.gov.au) #628333. kConFab is supported by grants from the National Breast Cancer Foundation, the National Health and Medical Research Council (NHMRC) and by the Queensland Cancer Fund, the Cancer Councils of New South Wales, Victoria, Tasmania and South Australia, and the Cancer Foundation of Western Australia. This work was supported in part by project grants from The National Health and Medical Research Council (NHMRC, ID442970 & ID1010719) to Amanda B. Spurdle who is supported by an NHMRC Senior Research Fellowship. David E. Goldgar was supported by National Institutes of Health (NIH) (www.nih.gov) grant CA116167, an NIH Recovery Act supplement (CA116167Z) and an NIH Specialized Program of Research Excellence (SPORE) in Breast Cancer (CA116201). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Goldgar DE, Easton DF, Byrnes GB, Spurdle AB, Iversen ES, et al. (2008) Genetic evidence and integration of various data sources for classifying uncertain variants into a single model. Hum Mutat 29: 1265–1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Spurdle AB (2010) Clinical relevance of rare germline sequence variants in cancer genes: evolution and application of classification models. Curr Opin Genet Dev 20: 315–323. [DOI] [PubMed] [Google Scholar]
- 3. Plon SE, Eccles DM, Easton D, Foulkes WD, Genuardi M, et al. (2008) Sequence variant classification and reporting: recommendations for improving the interpretation of cancer susceptibility genetic test results. Hum Mutat 29: 1282–1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Raponi M, Douglas AG, Tammaro C, Wilson DI, Baralle D (2012) Evolutionary constraint helps unmask a splicing regulatory region in BRCA1 exon 11. PLoS One 7: e37255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Thery JC, Krieger S, Gaildrat P, Revillion F, Buisine MP, et al. (2011) Contribution of bioinformatics predictions and functional splicing assays to the interpretation of unclassified variants of the BRCA genes. Eur J Hum Genet 19: 1052–1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Vallee MP, Francy TC, Judkins MK, Babikyan D, Lesueur F, et al. (2012) Classification of missense substitutions in the BRCA genes: a database dedicated to Ex-UVs. Hum Mutat 33: 22–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Domchek SM, Tang J, Stopfer J, Lilli DR, Hamel N, et al. (2013) Biallelic deleterious BRCA1 mutations in a woman with early-onset ovarian cancer. Cancer Discov 3: 399–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Goldgar DE, Easton DF, Deffenbaugh AM, Monteiro ANA, Tavtigian SV, et al. (2004) Integrated evaluation of DNA sequence variants of unknown clinical significance: application to BRCA1 and BRCA2. American Journal Of Human Genetics 75: 535–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lee MS, Green R, Marsillac SM, Coquelle N, Williams RS, et al. (2010) Comprehensive analysis of missense variations in the BRCT domain of BRCA1 by structural and functional assays. Cancer Res 70: 4880–4890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Millot GA, Carvalho MA, Caputo SM, Vreeswijk MP, Brown MA, et al. (2012) A guide for functional analysis of BRCA1 variants of uncertain significance. Hum Mutat 33: 1526–1537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Guidugli L, Pankratz VS, Singh N, Thompson J, Erding CA, et al. (2013) A Classification Model for BRCA2 DNA Binding Domain Missense Variants Based on Homology-Directed Repair Activity. Cancer Res 73: 265–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mann GJ, Thorne H, Balleine RL, Butow PN, Clarke CL, et al. (2006) Analysis of cancer risk and BRCA1 and BRCA2 mutation prevalence in the kConFab familial breast cancer resource. Breast Cancer Res 8: R12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cartegni L, Wang J, Zhu Z, Zhang MQ, Krainer AR (2003) ESEfinder: A web resource to identify exonic splicing enhancers. Nucleic Acids Res 31: 3568–3571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Desmet FO, Hamroun D, Lalande M, Collod-Beroud G, Claustres M, et al. (2009) Human Splicing Finder: an online bioinformatics tool to predict splicing signals. Nucleic Acids Res 37: e67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Yeo G, Burge CB (2004) Maximum entropy modeling of short sequence motifs with applications to RNA splicing signals. J Comput Biol 11: 377–394. [DOI] [PubMed] [Google Scholar]
- 16. Reese MG, Eeckman FH, Kulp D, Haussler D (1997) Improved splice site detection in Genie. J Comput Biol 4: 311–323. [DOI] [PubMed] [Google Scholar]
- 17. Bateman JF, Freddi S, Lamande SR, Byers P, Nasioulas S, et al. (1999) Reliable and sensitive detection of premature termination mutations using a protein truncation test designed to overcome problems of nonsense-mediated mRNA instability. Hum Mutat 13: 311–317. [DOI] [PubMed] [Google Scholar]
- 18. Walker LC, Whiley PJ, Houdayer C, Hansen TV, Vega A, et al. (2013) Evaluation of a 5-tier scheme proposed for classification of sequence variants using bioinformatic and splicing assay data: inter-reviewer variability and promotion of minimum reporting guidelines. Hum Mutat 34: 1424–1431. [DOI] [PubMed] [Google Scholar]
- 19. Lakhani SR, Gusterson BA, Jacquemier J, Sloane JP, Anderson TJ, et al. (2000) The pathology of familial breast cancer: histological features of cancers in families not attributable to mutations in BRCA1 or BRCA2. Clin Cancer Res 6: 782–789. [PubMed] [Google Scholar]
- 20. Walker LC, Whiley PJ, Couch FJ, Farrugia DJ, Healey S, et al. (2010) Detection of splicing aberrations caused by BRCA1 and BRCA2 sequence variants encoding missense substitutions: implications for prediction of pathogenicity. Hum Mutat 31: E1484–1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Chenevix-Trench G, Healey S, Lakhani S, Waring P, Cummings M, et al. (2006) Genetic and histopathologic evaluation of BRCA1 and BRCA2 DNA sequence variants of unknown clinical significance. Cancer Res 66: 2019–2027. [DOI] [PubMed] [Google Scholar]
- 22. Spurdle AB, Lakhani SR, Healey S, Parry S, Da Silva LM, et al. (2008) Clinical classification of BRCA1 and BRCA2 DNA sequence variants: the value of cytokeratin profiles and evolutionary analysis–a report from the kConFab Investigators. J Clin Oncol 26: 1657–1663. [DOI] [PubMed] [Google Scholar]
- 23. Goldgar DE, Easton DF, Deffenbaugh AM, Monteiro AN, Tavtigian SV, et al. (2004) Integrated evaluation of DNA sequence variants of unknown clinical significance: application to BRCA1 and BRCA2. Am J Hum Genet 75: 535–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Easton DF, Deffenbaugh AM, Pruss D, Frye C, Wenstrup RJ, et al. (2007) A systematic genetic assessment of 1,433 sequence variants of unknown clinical significance in the BRCA1 and BRCA2 breast cancer-predisposition genes. Am J Hum Genet 81: 873–883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Domchek SM, Tang JB, Stopfer J, Lilli DR, Hamel N, et al.. (2012) Biallelic Deleterious BRCA1 Mutations in a Woman with Early-Onset Ovarian Cancer. Cancer Discov. [DOI] [PMC free article] [PubMed]
- 26. Cartegni L, Chew SL, Krainer AR (2002) Listening to silence and understanding nonsense: exonic mutations that affect splicing. Nature Reviews Genetics 3: 285–298. [DOI] [PubMed] [Google Scholar]
- 27. Orban TI, Olah E (2003) Emerging roles of BRCA1 alternative splicing. Mol Pathol 56: 191–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Whiley P, de la Hoya M, Thomassen M, Becker A, Brandao R, et al.. (2013) Comparison of mRNA Splicing Assay Protocols across Multiple Laboratories: Recommendations for Best Practice in Standardized Clinical Testing. Clin Chem. [DOI] [PMC free article] [PubMed]
- 29. Ozcelik H, Nedelcu R, Chan VW, Shi XH, Murphy J, et al. (1999) Mutation in the coding region of the BRCA1 gene leads to aberrant splicing of the transcript. Hum Mutat 14: 540–541. [DOI] [PubMed] [Google Scholar]
- 30. Yang Y, Swaminathan S, Martin BK, Sharan SK (2003) Aberrant splicing induced by missense mutations in BRCA1: clues from a humanized mouse model. Human Molecular Genetics 12: 2121–2131. [DOI] [PubMed] [Google Scholar]
- 31. Hu YF, Li R (2002) JunB potentiates function of BRCA1 activation domain 1 (AD1) through a coiled-coil-mediated interaction. Genes Dev 16: 1509–1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Sum EY, Peng B, Yu X, Chen J, Byrne J, et al. (2002) The LIM domain protein LMO4 interacts with the cofactor CtIP and the tumor suppressor BRCA1 and inhibits BRCA1 activity. J Biol Chem 277: 7849–7856. [DOI] [PubMed] [Google Scholar]
- 33. Yarden RI, Brody LC (1999) BRCA1 interacts with components of the histone deacetylase complex. Proc Natl Acad Sci U S A 96: 4983–4988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hu YF, Miyake T, Ye Q, Li R (2000) Characterization of a novel trans-activation domain of BRCA1 that functions in concert with the BRCA1 C-terminal (BRCT) domain. J Biol Chem 275: 40910–40915. [DOI] [PubMed] [Google Scholar]
- 35. Phelan CM, Dapic V, Tice B, Favis R, Kwan E, et al. (2005) Classification of BRCA1 missense variants of unknown clinical significance. J Med Genet 42: 138–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Sevcik J, Falk M, Kleiblova P, Lhota F, Stefancikova L, et al. (2012) The BRCA1 alternative splicing variant Delta14–15 with an in-frame deletion of part of the regulatory serine-containing domain (SCD) impairs the DNA repair capacity in MCF-7 cells. Cell Signal 24: 1023–1030. [DOI] [PubMed] [Google Scholar]
- 37. Spurdle AB, Couch FJ, Hogervorst FB, Radice P, Sinilnikova OM (2008) Prediction and assessment of splicing alterations: implications for clinical testing. Hum Mutat 29: 1304–1313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Gaildrat P, Krieger S, Di Giacomo D, Abdat J, Revillion F, et al. (2012) Multiple sequence variants of BRCA2 exon 7 alter splicing regulation. J Med Genet 49: 609–617. [DOI] [PubMed] [Google Scholar]
- 39. Brzovic PS, Rajagopal P, Hoyt DW, King MC, Klevit RE (2001) Structure of a BRCA1-BARD1 heterodimeric RING-RING complex. Nat Struct Biol 8: 833–837. [DOI] [PubMed] [Google Scholar]
- 40. Chen A, Kleiman FE, Manley JL, Ouchi T, Pan ZQ (2002) Autoubiquitination of the BRCA1*BARD1 RING ubiquitin ligase. J Biol Chem 277: 22085–22092. [DOI] [PubMed] [Google Scholar]
- 41. Xia Y, Pao GM, Chen HW, Verma IM, Hunter T (2003) Enhancement of BRCA1 E3 ubiquitin ligase activity through direct interaction with the BARD1 protein. J Biol Chem 278: 5255–5263. [DOI] [PubMed] [Google Scholar]
- 42. Ransburgh DJ, Chiba N, Ishioka C, Toland AE, Parvin JD (2010) Identification of breast tumor mutations in BRCA1 that abolish its function in homologous DNA recombination. Cancer Res 70: 988–995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Morris JR, Pangon L, Boutell C, Katagiri T, Keep NH, et al. (2006) Genetic analysis of BRCA1 ubiquitin ligase activity and its relationship to breast cancer susceptibility. Hum Mol Genet 15: 599–606. [DOI] [PubMed] [Google Scholar]
- 44.Bouwman P, van der Gulden H, van der Heijden I, Drost R, Klijn CN, et al.. (2013) A high-throughput functional complementation assay for classification of BRCA1 missense variants. Cancer Discov. [DOI] [PubMed]
- 45. Shakya R, Reid LJ, Reczek CR, Cole F, Egli D, et al. (2011) BRCA1 tumor suppression depends on BRCT phosphoprotein binding, but not its E3 ligase activity. Science 334: 525–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Sarkar M, Magliery TJ (2008) Re-engineering a split-GFP reassembly screen to examine RING-domain interactions between BARD1 and BRCA1 mutants observed in cancer patients. Mol Biosyst 4: 599–605. [DOI] [PubMed] [Google Scholar]
- 47. Sweet K, Senter L, Pilarski R, Wei L, Toland AE (2010) Characterization of BRCA1 ring finger variants of uncertain significance. Breast Cancer Res Treat 119: 737–743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Ruffner H, Joazeiro CA, Hemmati D, Hunter T, Verma IM (2001) Cancer-predisposing mutations within the RING domain of BRCA1: loss of ubiquitin protein ligase activity and protection from radiation hypersensitivity. Proc Natl Acad Sci U S A 98: 5134–5139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Chang S, Biswas K, Martin BK, Stauffer S, Sharan SK (2009) Expression of human BRCA1 variants in mouse ES cells allows functional analysis of BRCA1 mutations. J Clin Invest 119: 3160–3171. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Primers for mRNA splicing assays.
(DOCX)
Frequency of variant occurrence in 1000 Genomes and EVS snp datasets.
(DOCX)