Abstract
Objective
To describe a systematic assessment of patient educational materials for the Growing Right Onto Wellness (GROW) trial, a childhood obesity prevention study targeting a low health literate population.
Methods
Process included: (1) expert review of educational content, (2) assessment of the quality of materials including use of the Suitability Assessment of Materials (SAM) tool, and (3) material review and revision with target population.
Results
12 core modules were developed and assessed in an iterative process. Average readability was at the 6th grade reading level (SMOG Index 5.63 ± 0.76, and Fry graph 6.0 ± 0.85). SAM evaluation resulted in adjustments to literacy demand, layout & typography, and learning stimulation & motivation. Cognitive interviews with target population revealed additional changes incorporated to enhance participant's perception of acceptability and feasibility for behavior change.
Conclusion
The GROW modules are a collection of evidence-based materials appropriate for parents with low health literacy and their preschool aged children, that target the prevention of childhood overweight/obesity.
Practice implications
Most trials addressing the treatment or prevention of childhood obesity use written materials. Due to the ubiquitous prevalence of limited health literacy, our described methods may assist researchers in ensuring their content is both understood and actionable.
Keywords: Health literacy, Childhood obesity, Intervention development, Education, Evaluation
1. Introduction
Over the past several decades, the prevalence of overweight and obesity has increased dramatically in U.S. children and adolescents with notable disparate trends among African-American and Hispanic youth [1,2]. Current estimates indicate that nearly 32% of children ages 2–19 are overweight or obese [1], and although trends may be stabilizing, the long-term health impact of overweight and obesity remains significant. The etiologic factors that have contributed to this public health problem include significant decreases in physical activity, effective marketing of calorie dense foods to children, and increased portion size and calorie consumption. Additionally, evidence continues to grow linking childhood overweight and obesity to increased future risk for cardiovascular disease and diabetes [3,4]. Unless, effective and sustainable interventions are developed to reverse these trends, future generations will face significant health challenges. Overweight and obesity patterns often cluster in families and evidence supports parental influence as a contributing factor to rates of overweight and obesity among children [5–7]. It is imperative then that efforts to improve behaviors associated with obesity target both adults and children of the same household.
Individual limitations in health literacy are often a barrier faced in public health efforts to effectively convey information that is both accessible and meaningful to the public. Over 90 million Americans have limited health literacy skills in that they struggle to understand and apply health information. These limitations have been shown to influence a variety of health outcomes [8]. Deficits in health literacy include the misapplication and/or non-application of written and quantitative information to daily decisions and activities that affect health. In the context of overweight and obesity prevention, examples include comparing and choosing healthy foods [9], understanding food labels and estimating appropriate portion sizes [10–13], engaging in physical activity [14], and assessing how weight can affect health [15]. There is some evidence in the literature to support improvements in parental knowledge and behaviors that impact upon child health when specific efforts are taken to address health literacy deficits; however, none of these studies have specifically targeted obesity prevention among preschoolers. To address this need, we describe a systematic process to assess the quality of educational materials for a behavioral intervention aimed at obesity prevention within a low health literate population.
2. Methods
The behavioral intervention entitled Growing Right Onto Wellness (GROW) includes an approach that incorporates plain language principles [16–18] into all study-related written materials to meet the health literacy needs of our target population. Our systematic process included: (1) expert review of core content for core materials; (2) material mock-ups that were graded utilizing the Suitability Assessment of Materials; and (3) target population review and revisions. We review each of these steps in detail below.
GROW study team members with expertise in pediatric medicine, overweight and obesity, behavioral health, healthy literacy, and health communication developed a list of core modules and the instructional content therein for a planned educational intervention (Table 1). To best serve the target population, which from previous work was known to have limited health literacy skills [19–22], we undertook a multi-step process for each module to ensure that materials were appropriate for a low health literate audience. We concurrently developed a Spanish version of our materials but report here the assessment for the English materials only. Initial base mock-ups for each module were created using content from our previously developed materials [19,23] that had been adapted from sources available through the American Academy of Pediatrics and Bright Futures™, as well as from a publically available childhood obesity pamphlet entitled, We Can!®, produced by the National Heart, Lung, and Blood Institute. Initial module format, structure, and literacy approach were also informed by the GREENLIGHT toolkit that targets health behaviors of parents of young children (≤24 months) [24]. Specific module content was revised by GROW team experts in an iterative process and finalized prior to quality assessment.
Table 1.
12 core modules.
| (1) | Community building |
| (2) | Behavior change/goal setting |
| (3) | Parenting styles |
| (4) | Community center |
| (5) | Family physical activity |
| (6) | Snacks and drinks |
| (7) | Mindful eating |
| (8) | Sleep |
| (9) | Choosing foods |
| (10) | Meal planning |
| (11) | Eating together |
| (12) | Media time |
Quality assessment for each module began with an initial cursory evaluation of content and style according to several principles of clear health communication [16,18]. Specifically, we structured each module to contain no more than three key messages which appear prominently on the face page of each booklet. Headers and other directional statements were emboldened, and short phrases using active voice were made to appear throughout so as to better guide the reader through the text. Second, to maximize readability, we optimized the use of white space and graphics, avoided the use of medical and other complex jargon, and minimized subheadings and lists to only a few bulleted points of text, clearly grouped by theme. Thirdly, we placed the text font at 12 point or higher and simplified sentence structure. At the end of each module, we incorporate a section that encourages participants to set a goal by selecting an activity they and their child will implement toward improving their health in the coming week [25,26]. Finally, each module underwent a more thorough evaluation of content and structure using the Suitability Assessment of Materials (SAM) process described by Doak and Doak [18].
The SAM process was initially developed to move beyond simple formula-based methods of readability assessment and toward a more systematic, rigorous, and quantified evaluation of health-related materials. It includes assessment in the areas of material content, literacy demand, graphics, layout & typography, learning stimulation & motivation, and cultural appropriateness with subtopics contained within each category. Content refers to whether or not the materials contain a clearly stated purpose and provide instructional rather than simply factual information that can be learned in the allotted time (i.e. 60 min educational sessions). Literacy demand includes the assessment of reading level, writing style, sentence construction, choice of vocabulary, and how well topics are organized to promote learning. Graphics refers to the use and quality of drawings, illustrations, and images and how easily the intended information is communicated to the reader. Layout & typography refer to the size of printed text and the framing of messages so as to promote readability and logical flow of thought. Learning stimulation & motivation assess whether or not materials provide information that encourages the reader to apply and act upon the information given. Finally, cultural appropriateness refers to whether or not the presented information matches the language and experience of the targeted audience.
In conducting a SAM evaluation, users are encouraged to first familiarize themselves with the instrument and evaluation criteria. After reading the materials to be assessed, the user then evaluates the materials according to each sub-category and assigns a score for each factor. Scores ranging from 0 to 2 are assigned according to whether that factor is deemed not suitable, adequate, or superior respectively. Scores are then summed across all factors with a maximum score of 44. Finally, scores are converted to a percentage with ranges of 70–100%, 40–69%, and 0–39% distinguishing materials that are superior, adequate, or not suitable. GROW study team members established an a priori internal standard of 88% on SAM scoring before allowing materials to progress through the final steps of development. Modules scoring less than 88% were revised accordingly in an iterative process until each module received a rating of 88% or above. GROW experts were then asked to conduct a final review to ensure that the core content and educational intent of each module were preserved following the adaptation process. To assess the readability of the materials, unformatted text from each module was transcribed verbatim into a separate document and analyzed using two separate, validated readability assessment tools, the SMOG Index and Fry graph. Each method is derived from different formulas that calculate the reading grade level based on the number of sentences and polysyllables contained within the text.
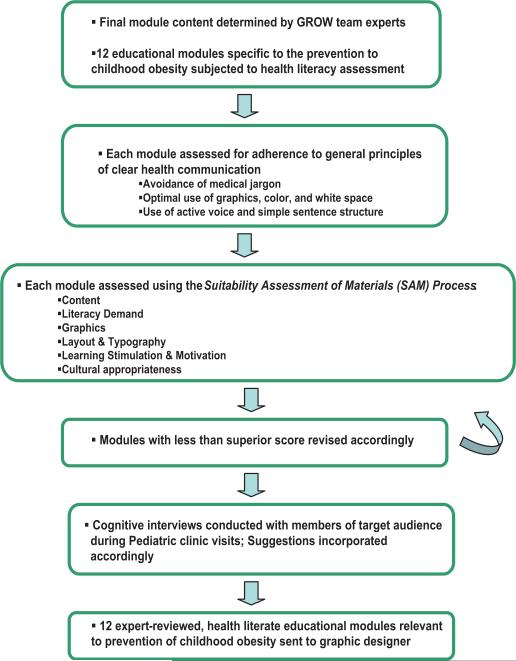
Next, cognitive interviews were conducted with parents of 3–5 year old children (i.e. target audience) to verify topic relevancy and ease of understanding. Individual cognitive interviews were selected as the method for this feedback to reduce the social desirability that can be found in group settings [27]. After obtaining approval from the Vanderbilt IRB, sixty cognitive interviews took place from June to July 2011 in the General Pediatrics clinic at Vanderbilt Children's Hospital. The General Pediatrics clinic serves as a primary recruitment source for GROW intervention participants, which made it an ideal choice to maintain demographic and socioeconomic similarities between the interviewed participants and those in the subsequent study. Study staff members scheduled blocks of time when large numbers of parents with 3–5 year old children would be available at the clinic. In addition to having a preschool age child, participants were selected based on their ability to speak English, their availability in the waiting room, and their willingness to participate. Each parent approached in the waiting room was asked if he or she would like to provide feedback on one of the 12 modules. Questions included: initial reaction to the material, ease of understanding the content, relevance of the content, esthetics of the format, and the practical usability of the material. The length of the interview was driven by the participant and took 10–15 min on average. For their participation, families received an incentive of $10 for their time. When conducting the cognitive interviews, study staff arrived in the clinic with two copies of each module to be reviewed per potential participant. As the study staff member spoke to a participant, he or she noted comments directly on one copy of the module, while the participant reviewed the other copy. This process allowed the study staff to note, as he or she followed through the protocol, exact suggestions by circling or writing comments next to the language or graphical pieces relevant to a response. After reviewing the results from the first mock-up interviews, a saturation point was found to be reached at approximately 5 interviews per mock-up, and this pattern continued for the remaining 11 content areas. Two study staff members independently reviewed each of the 5 comment-filled booklets per topic and then compared notes to develop themes as well as specific directions for improving each module. Fig. 1 outlines and summarizes the steps taken for the entire health literacy-sensitive adaptation process, which was repeated for all 12 modules. The resulting final versions contained relevant, expert-reviewed, and health literate information that was appropriate for families with preschool age children. These modules represent the written, educational component of the behavioral intervention for the GROW trial. Each finalized module was subjected to an additional SAM assessment by two independent reviewers that had experience using the SAM, knowledge of the educational goals of the trial, but were blinded to the first reviewer's assessment. This was done to evaluate in a general sense the inter-rater agreement on the quality of materials using the SAM process.
Fig. 1.
Systematic approach to health literacy assessment of materials.
3. Results
3.1. SAM evaluation
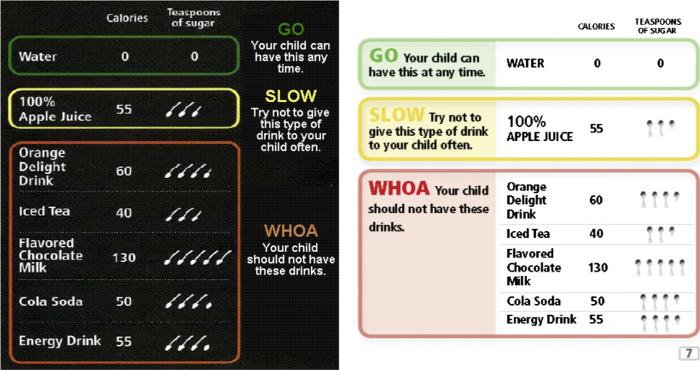
Each finalized GROW module is a self-contained, 8-pagebound pamphlet that is easily transportable. Table 2 provides a summary of the initial and repeat health literacy-sensitive assessment conducted by the first reviewer and examples of changes made to the materials. On average, the readability for the final 12 educational modules was at the 6th grade level (SMOG Index 5.63 ± 0.76, Fry graph 6.0 ± 0.85). Initial SAM scores indicated that 11 out of the 12 modules were in the superior range; however, only 3 of the 12 modules met our a priori internal standard of 88%. Some of the most common areas that required revision were literacy demand, layout & typography, and learning stimulation & motivation. Specifically regarding literacy demand, our writing style was often passive and was occasionally found to contain jargon despite concerted efforts to minimize the latter. Improvements in layout & typography included enhancements in the color scheme and contrast of certain tables and graphics as well as the reframing of health information to better coincide with typical reading patterns and logical flow of thought. For example, in module 6 “Snacks and Drinks”, readers are informed about smart snacking and challenged to reduce the sugar content of liquids provided to their child. The original version of this module contained a graphic (Fig. 2) in which participants were required to read from left to right to interpret the health message, and the process of interpreting the message was neither natural nor logical. The final version of this graphic had improved color contrast and the educational content was reframed to ease understanding of the intended message. Enhancements in learning stimulation & motivation consisted of improvements in the perceived level of interaction between the reader and our materials, including examples that better modeled behavior and improved the perception of the feasibility of recommended behavior change. In module 11 “Eating Together”, participants are instructed on the benefits of shared meal times and are encouraged to involve their children in the food selection and preparation process as a means of educating them about healthier choices. In the final version of this module, an easy-to-do, healthy recipe was added to enhance behavior change. Similarly, in module 9 “Choosing Foods” we model for parents how to ensure they are helping their child receive the recommended 5 daily servings of fruits and vegetables using an example that walks them through a typical day's meal selections. Finally, in module 6 “Snacks and Drinks” we originally provided the option for parents to remove juice consumption all together from their child's diet, but this was changed to a more reasonable recommendation to offer one less serving of juice each day in the upcoming week. Each of the 12 modules required a single repeat SAM evaluation by the first reviewer after the recommended edits were addressed in order to meet or surpass the internal standard of 88% on SAM scoring. The two independent reviewers who additionally utilized the SAM on the final revised modules were in 100% agreement with the “superior” ratings of the first reviewer using criteria established by Doak and Doak. There was less agreement, however, between all three reviewers as to which of the revised modules met the a priori internal standard of 88% or higher. One rater had low agreement with the other two (25%) while the other two raters had 100% agreement (Table 3).
Table 2.
GROW intervention SAM assessment and revision.
| Module | SMOG Index | Fry graph | Primary SAM evaluation | Final SAM evaluation | General changes required |
|---|---|---|---|---|---|
| (1) Community building | 6.1 | 7 | 38/44 (86%) | 40/44 (91%) | Simplified language (e.g. “contagious” Δ to “spread”), reframing of messages, active voice |
| (2) Behavior change/goal setting | 6 | 5 | 38/44 (86%) | 40/44 (91%) | Improved writing style |
| (3) Parenting styles | 6 | 6 | 36/44 (82%) | 41/44 (93%) | Improved literacy demand, improved graphics |
| (4) Community center | 6.1 | 7 | 40/44 (90%) | N/A | Simplified language (e.g. “etiquette” removed), reframing of messages |
| (5) Family physical activity | 6.6 | 7 | 36/44 (82%) | 39/44 (88%) | Simplified sentence structure and language (“weight-bearing exercises” Δ to “walking/playing tag”), active voice |
| (6) Snacks and drinks | 5 | 6 | 32/40 (80%) | 37/40 (92%) | Simplified language, reframing of messages |
| (7) Mindful eating | 4.2 | 5 | 38/44 (86%) | 40/44 (91%) | Simplified language, improved graphics |
| (8) Sleep | 5.4 | 6 | 41/44 (93%) | N/A | Active voice |
| (9) Choosing foods | 6.1 | 7 | 39/44 (88%) | 41/44 (93%) | Improved literacy demand, modeling of behavior |
| (10) Meal planning | 4.8 | 6 | 40/44 (90%) | N/A | Improved interaction during problem solving and graphical layout |
| (11) Eating together | 4.8 | 5 | 28/42 (66%) | 39/42 (93%) | Reduction of jargon, simplified language (“control portion sizes” Δ to “control your plate”), active voice, reduce prose burden, reframing of messages |
| (12) Media time | 6.4 | 5 | 38/44 (86%) | 41/44 (93%) | Simplified language, active voice, removed unfamiliar jargon (“game boys” Δ to “hand-held video games”), improved subheadings |
| Average score ± SD | 5.63 ± 0.76 | 6.00 ± 0.85 | 85% ± 7 | 91.5 ± 1.62 |
Fig. 2.
Sample improvements in layout and typography; Module 6 “Health Snacks and Drink.”
Table 3.
Inter-rater agreement for SAM assessment of revised, finalized materials.
| GROW modules | Reviewer #1 | Reviewer #2 | Reviewer #3 |
|---|---|---|---|
| Community building | 40/44 (91%) | 36/44 (82%) | 43/44 (98%) |
| Behavior change/goal setting | 40/44 (91%) | 37/44 (84%) | 42.5/44 (97%) |
| Parenting styles | 41/44 (93%) | 34/44 (77%) | 44/44 (100%) |
| Community center | 40/44 (90%) | 36/44 (82%) | 44/44 (100%) |
| Family physical activity | 39/44 (88%) | 36/44 (82%) | 41.5/44 (94%) |
| Snacks and drinks | 37/40 (92%) | 38/44 (86%) | 44/44 (100%) |
| Mindful eating | 40/44 (91%) | 38/44 (86%) | 42.5/44 (97%) |
| Sleep | 41/44 (93%) | 37/44 (84%) | 43/44 (98%) |
| Choosing foods | 41/44 (93%) | 40/44 (91%) | 44/44 (100%) |
| Meal planning | 40/44 (90%) | 39/44 (89%) | 41.5/44 (94%) |
| Eating together | 39/42 (93%) | 40/44 (91%) | 43/44 (98%) |
| Media time | 41/44 (93%) | 37/44 (84%) | 43/44 (98%) |
3.2. Cognitive interviews
As the cognitive interview participants only reviewed one module booklet each, much of the feedback was module specific. However, in general the comments fell into one of 8 themes. Themes 1 and 2 involve concerns raised that would either require clarification in a later session or further elaboration during the facilitation of the session. These themes did not require changes in the educational modules but instead proved helpful in the process of developing the corresponding facilitator's guides, which included all interactive and didactic instructions for the inter-ventionist. The remaining themes did require changes to the modules themselves for a variety of reasons. Themes 3 and 4 reflected upon the idea that participants did not like to feel pushed or pigeon-holed into a specific behavior. In response, we reduced any sweeping generalizations that participants felt had a negative connotation, and likewise, we removed any language participants deemed too forceful or unrealistic in regards to healthy behaviors. This included, for example, the addition of phrases like “tend to” or “are more likely to” when discussing behavioral changes or the resulting health benefits thereof. For themes 5 and 6, participants raised concerns about word choice and wordiness, which caused us to eliminate phrases participants felt were difficult to understand and to decrease the number of words in phrases to amplify the ease of understanding. Theme 7 included items that participants brought up in regards to practicality and making sure all suggestions and supplemental materials fit their needs. Finally, theme 8 contained suggestions generated by participants that added helpful information to the module that our team had not previously considered (Table 4).
Table 4.
Feedback from cognitive interviews.
| Theme | Change required | Module | Example issue | Example solution |
|---|---|---|---|---|
| Clarify messages in the facilitator's guide | No | Behavior change/goal setting | Participants found the idea of setting SMART goals difficult to understand | In response, we developed session content and a poster to highlight each of the elements of SMART goals |
| Requested information found in another session | No | Community building | Participants did not know how to “Work with others to set goals you can reach and find answers when problems occur” | No change occurred since this topic is found in a different session |
| Reduce sweeping generalizations that may negatively implicate behaviors | Yes | Community building | Participants stated that the phrase “Parents who are connected with others have less stress and are healthier” was too over-generalized | Added ‘tend to’ into the phase: “Parents who are connected with others tend to have less stress and are healthier” |
| Reduce language that seems to be overly forcing certain behaviors | Yes | Snacks and drinks | Participants felt the phrase “I will not offer juice at all to my child this week” was unrealistic | Changed phrase to: “I will offer my child one less serving of juice each day this week” |
| Clarify/remove unfamiliar terminology | Yes | Family physical activity | Participants felt that “weight-bearing activities” was not a commonly used phrase | Removed the phrase from the module |
| Reduce wordiness/be clear and concise | Yes | Community center | Participants felt the phrase “Families with a place for recreation tend to be more active. A local community center is a great option for your family's recreational home!” was too wordy | Changed phrase to: “A local community center is a great place to be active with your family!” which greatly reduced wordiness |
| Ensure tools included are practical | Yes | Goal setting | Participants felt that a large number of rows suggested they needed to develop a large number of goals | Reduced the number of rows on the goal tracking sheet |
| Add participant suggestions when relevant | Yes | Meal planning | A participant suggested adding an item regarding expiration date to a statement about stocking up on sale items | Added the statement into the module content |
4. Discussion and conclusion
4.1. Discussion
We have described a systematic approach to evaluating the quality of an educational and behavioral intervention that targets the prevention of overweight and obesity among parents with limited health literacy skills and their preschool-aged children (3–5 years old). We found this process to be both feasible to our study staff and acceptable to potential participants who represented our target population. Our materials are written at a 6th grade reading level which is appropriate for our audience based on data from the 2003 National Assessment of Adult Literacy in which the “average” adult had literacy skills correlating roughly between the 6th and 9th grade reading level [28]. Given the known health literacy needs of our audience then, a health literate approach to intervention development has the potential to enhance the efficacy of our program's educational and behavioral goals among participants randomized to this condition.
Previous studies that have developed enhanced educational materials for low health literate populations have demonstrated moderate improvements in parental behaviors that impact upon child health. For example, Yin et al. compared the use of standard print instructions for the dosing of infant acetaminophen to the use of the same instructions plus a pictogram guide on parental medication dosing errors [29]. They not only observed significant overall reductions in error rates with the inclusion of the pictogram, but there was significant variation in error rates by literacy status in that lower health literate parents experienced greater benefit from the visual cues. Oettinger et al. similarly assessed parental understanding of BMI and BMI percentiles using standard versus color-coded BMI charts. They found that understanding in general was improved with use of the color-coded charts, and that greater benefit again was gained by those parents with lower numeracy skills [15].
Kumar et al. assessed parental ability to perform tasks such as mixing infant formula and interpreting the results from a digital thermometer reading and identified significant deficits in these numeracy-related skills [30]. In a similar study, Yin et al. observed that a significant proportion of Spanish-speaking caregivers of young children (<30 months) struggled to determine accurately if a food label met Women, Infants, and Children (WIC) nutrition guidelines [31]. Again, the majority of parents in this sample had poor numeracy skills. In the context of obesity-related behaviors, Garrett identified a small association between low parental health literacy and inaccurate weight perceptions by parents of preschool aged children [32]. In that study, parents were given credit for accurately labeling their child's weight as “appropriate” if the BMI in fact fell between the 5th and 95th percentiles. This suggests a potential underestimation of the magnitude of the reported association if one were to assign parental accuracy using the CDC guidelines for overweight and obesity cut-points in children (i.e. ≥85% for overweight, ≥95% for obese). Finally, there have been a handful of studies that discuss the importance of parental understanding and engagement in addressing the growing epidemic of childhood obesity [33–36].
4.2. Conclusion
Overall, these studies collectively highlight the potential role of parental health literacy in addressing childhood overweight and obesity and support approaches that target both parent and child psychosocial factors related to obesogenic behaviors. There are some limitations to the described approach to our intervention development. Content for our educational program was in part derived from previous work with our local community that experiences many socio-demographic challenges and hence may not be fully generalizable to other populations. Nonetheless, our materials are evidenced-based, informed by expert opinion and experience, and congruent with current national guidelines where applicable. Lastly, despite demonstrating relative agreement between independent reviewers using the SAM process, assessment of the quality of materials using the SAM may still be vulnerable to some subjectivity.
4.3. Practice implications
Currently, many behavioral interventions are underway that address the topic of pediatric obesity [37–40]. The majority of these require written materials to deliver some core content. Therefore, considering a systematic process that allows for the development of materials sensitive to the health literacy needs of the intended audience becomes critical (refer to Fig. 1). We have presented a clear, replicable approach to use in other programs that utilize written materials to impart core content knowledge and behavior change. Given the ubiquitous prevalence of limited health literacy in our nation, the approach we have described has the potential to ensure that efforts to address childhood overweight and obesity are understood, accepted, and actionable by the majority of those we aim to reach.
Acknowledgements
The project described was supported by Award Number 5U01HL103620-03 from the National Heart, Lung, and Blood Institute, the Eunice Kennedy Shriver National Institute of Child Health and Development and the Office of Behavioral and Social Sciences Research. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute or the National Institutes of Health. Support also came in part from the Effective Health Communication Core of the Vanderbilt CTSA (NIH/NCATS UL54TR000123), the Vanderbilt Institute for Clinical and Translational Research (Ul1TR000445), and the Vanderbilt Center for Diabetes Translation Research (P30DK092986). ROW is supported by an NIDDK Career Development Award (5K23DK092470-04). ROW and JRT were lead authors of the manuscript. ROW, AMS, and WJH independently conducted the SAM assessment. ECS provided statistical input. RLR and SLB provided health literacy expertise and mentorship to ROW. SLB provided substantive editing and data assessment. All authors approved the final version of the manuscript.
Funding
Approval for manuscript submission was obtained from the Childhood Obesity Prevention and Treatment Research (COPTR) publications committee.
Footnotes
Conflicts of interest
No author has any conflicts of interest to report. ROW is supported by an NIDDK Career Development Award (5K23DK092470-04). AMS is supported by an NIH/NCATS award (UL54TR000123).
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. J Am Med Assoc. 2013;307:483–90. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rendall MS, Weden MM, Fernandes M, Vaynman I. Hispanic and black US children's paths to high adolescent obesity prevalence. Pediatr Obes. 2012;7:423–35. doi: 10.1111/j.2047-6310.2012.00080.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Halfon N, Verhoef PA, Kuo AA. Childhood antecedents to adult cardiovascular disease. Pediatr Rev. 2012;33:51–60. doi: 10.1542/pir.33-2-51. [DOI] [PubMed] [Google Scholar]
- 4.Nadeau KJ, Maahs DM, Daniels SR, Eckel RH. Childhood obesity and cardiovascular disease: links and prevention strategies. Nat Rev Cardiol. 2011;8:513–25. doi: 10.1038/nrcardio.2011.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kuhl ES, Clifford LM, Stark LJ. Obesity in preschoolers: behavioral correlates and directions for treatment. Obesity. 2012;20:3–29. doi: 10.1038/oby.2011.201. [DOI] [PubMed] [Google Scholar]
- 6.Patrick H, Nicklas TA. A review of family and social determinants of children's eating patterns and diet quality. J Am Coll Nutr. 2005;24:83–92. doi: 10.1080/07315724.2005.10719448. [DOI] [PubMed] [Google Scholar]
- 7.van Stralen MM, te Velde SJ, van Nassau F, Brug J, Grammatikaki E, Maes L, et al. Weight status of European preschool children and associations with family demographics and energy balance-related behaviours: a pooled analysis of six European studies. Obes Rev. 2012;13:29–41. doi: 10.1111/j.1467-789X.2011.00959.x. [DOI] [PubMed] [Google Scholar]
- 8.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155:97–107. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- 9.Pieper JR, Whaley SE. Healthy eating behaviors and the cognitive environment are positively associated in low-income households with young children. Appetite. 2011;57:59–64. doi: 10.1016/j.appet.2011.03.016. [DOI] [PubMed] [Google Scholar]
- 10.Rothman RL, Housam R, Weiss H, Davis D, Gregory R, Gebretsadik T, et al. Patient understanding of food labels: the role of literacy and numeracy. Am J Prev Med. 2006;31:391–8. doi: 10.1016/j.amepre.2006.07.025. [DOI] [PubMed] [Google Scholar]
- 11.Small L, Lane H, Vaughan L, Melnyk B, McBurnett D. A systematic review of the evidence: the effects of portion size manipulation with children and portion education/training interventions on dietary intake with adults. Worldviews Evid Based Nurs. 2012;10:69–81. doi: 10.1111/j.1741-6787.2012.00257.x. [DOI] [PubMed] [Google Scholar]
- 12.Young LR, Nestle M. Reducing portion sizes to prevent obesity: a call to action. Am J Prev Med. 2012;43:565–8. doi: 10.1016/j.amepre.2012.07.024. [DOI] [PubMed] [Google Scholar]
- 13.Huizinga MM, Carlisle AJ, Cavanaugh KL, Davis DL, Gregory RP, Schlundt DG, et al. Literacy, numeracy, and portion-size estimation skills. Am J Prev Med. 2009;36:324–8. doi: 10.1016/j.amepre.2008.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Osborn CY, Paasche-Orlow MK, Bailey SC, Wolf MS. The mechanisms linking health literacy to behavior health status. Am J Health Behav. 2011;35:118–28. doi: 10.5993/ajhb.35.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Oettinger MD, Finkle JP, Esserman D, Whitehead L, Spain TK, Pattishall SR, et al. Color-coding improves parental understanding of body mass index charting. Acad Pediatr. 2009;9:330–8. doi: 10.1016/j.acap.2009.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kripalani S, Weiss BD. Teaching about health literacy and clear communication. J Gen Intern Med. 2006;21:888–90. doi: 10.1111/j.1525-1497.2006.00543.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rudd RE, Comings JP, Hyde JN. Leave no one behind: improving health and risk communication through attention to literacy. J Health Commun. 2003;8:104–15. doi: 10.1080/713851983. [DOI] [PubMed] [Google Scholar]
- 18.Doak CC, Doak LG, Root JH. Teaching patients with low literacy skills. 2nd ed. J. B. Lippincott; Philadelphia: 1996. [Google Scholar]
- 19.Barkin SL, Gesell SB, Po'e EK, Escarfuller J, Tempesti T. Culturally tailored, family-centered, behavioral obesity intervention for Latino-American pre-school-aged children. Pediatrics. 2012;130:445–56. doi: 10.1542/peds.2011-3762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ciampa PJ, White RO, Perrin EM, Yin HS, Sanders LM, Gayle EA, et al. The association of acculturation and health literacy, numeracy and health-related skills in Spanish-speaking caregivers of young children. J Immigr Minor Health. 2013;15:492–8. doi: 10.1007/s10903-012-9613-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Huizinga MM, Pont S, Rothman RL, Perrin E, Sanders L, Beech B. ABC's and 123's: parental literacy, numeracy, and childhood obesity. Obes Manag. 2008;4:98–103. doi: 10.1089/obe.2008.0163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.White RO, 3rd, Osborn CY, Gebretsadik T, Kripalani S, Rothman RL. Development and validation of a Spanish diabetes-specific numeracy measure: DNT-15 Latino. Diabetes Technol Ther. 2011;13:893–8. doi: 10.1089/dia.2011.0070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rothman RL, Perrin E, Yin HS, Patino-Fernandez A, Bachus A, Sanders L. GreenLight: a randomized trial addressing health literacy and communication to prevent paediatric obesity.. International Conference on Communication in Health.; St. Andrews. 2012. [Google Scholar]
- 24.National Institute of Child Health and Human Development; Vanderbilt University . ClinicalTrials.gov [Internet] National Library of Medicine (US); Bethesda (MD): [2013 Jun 11]. Addressing Health Literacy and Numeracy to Prevent Childhood Obesity. 2009. Available from: http//clinicaltrials.-gov/ct2/show/NCT01040897 NLM Identifier: NCT01040897. [Google Scholar]
- 25.Cullen KW, Baranowski T, Smith SP. Using goal setting as a strategy for dietary behavior change. J Am Diet Assoc. 2001;101:562–6. doi: 10.1016/S0002-8223(01)00140-7. [DOI] [PubMed] [Google Scholar]
- 26.Pearson ES. Goal setting as a health behavior change strategy in overweight and obese adults: a systematic literature review examining intervention components. Patient Educ Couns. 2012;87:32–42. doi: 10.1016/j.pec.2011.07.018. [DOI] [PubMed] [Google Scholar]
- 27.Hollander J. The social contexts of focus groups. J Contemp Ethnogr. 2004;33:602–37. [Google Scholar]
- 28.Kutner MA, United States Department of Education, National Center for Education Statistics . The health literacy of America's adults: results from the 2003 National Assessment of Adult Literacy. United States Department of Education; National Center for Education Statistics; Washington, DC: 2006. [Google Scholar]
- 29.Yin HS, Dreyer BP, van Schaick L, Foltin GL, Dinglas C, Mendelsohn AL. Randomized controlled trial of a pictogram-based intervention to reduce liquid medication dosing errors and improve adherence among caregivers of young children. Arch Pediatr Adolesc Med. 2008;162:814–22. doi: 10.1001/archpedi.162.9.814. [DOI] [PubMed] [Google Scholar]
- 30.Kumar D, Sanders L, Perrin EM, Lokker N, Patterson B, Gunn V, et al. Parental understanding of infant health information: health literacy, numeracy, and the Parental Health Literacy Activities Test (PHLAT). Acad Pediatr. 2010;10:309–16. doi: 10.1016/j.acap.2010.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yin HS, Sanders LM, Rothman RL, Mendelsohn AL, Dreyer BP, White RO, et al. Assessment of health literacy and numeracy among Spanish-Speaking parents of young children: validation of the Spanish Parental Health Literacy Activities Test (PHLAT Spanish). Acad Pediatr. 2012;12:68–74. doi: 10.1016/j.acap.2011.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Garrett-Wright D. Parental perception of preschool child body weight. J Pediatr Nurs. 2011;26:435–45. doi: 10.1016/j.pedn.2010.07.009. [DOI] [PubMed] [Google Scholar]
- 33.Abrams MA, Klass P, Dreyer BP. Health literacy and children: recommendations for action. Pediatrics. 2009;124:S327–31. doi: 10.1542/peds.2009-1162I. [DOI] [PubMed] [Google Scholar]
- 34.Yin HS, Johnson M, Mendelsohn AL, Abrams MA, Sanders LM, Dreyer BP. The health literacy of parents in the United States: a nationally representative study. Pediatrics. 2009;124:S289–98. doi: 10.1542/peds.2009-1162E. [DOI] [PubMed] [Google Scholar]
- 35.Golan M. Parents as agents of change in childhood obesity – from research to practice. Int J Pediatr Obes. 2006;1:66–76. doi: 10.1080/17477160600644272. [DOI] [PubMed] [Google Scholar]
- 36.Golan M, Kaufman V, Shahar DR. Childhood obesity treatment: targeting parents exclusively v. parents children. Br J Nutr. 2006;95:1008–15. doi: 10.1079/bjn20061757. [DOI] [PubMed] [Google Scholar]
- 37.National Heart L, and Blood Institute; Case Western Reserve University . Clinical-Trials.gov [Internet] National Library of Medicine (US); Bethesda (MD): [2013 Jun 11]. Ideas Moving Parents and Adolescents to Change together (IMPACT). 2011. Available from: http://clinicaltrials.gov/ct2/show/ NCT01514279. NLM Identifier: NCT01514279. [Google Scholar]
- 38.National Heart L, and Blood Institute; Vanderbilt University . ClinicalTrials.gov [Internet] National Library of Medicine (US); Bethesda (MD): [2013 Jun 11]. Growing Right Onto Wellness (GROW): Changing Early Childhood Body Mass Index (BMI) Trajectories. 2011. Available from: http://clinicaltrials.gov/ct2/show/NCT01316653 NLM Identifier: NCT01 316653. [Google Scholar]
- 39.National Heart L, and Blood Institute; Stanford University . ClinicalTrials.gov [Internet] National Library of Medicine (US); Bethesda (MD): [2013 Jun 11]. Clinic, Family & community Collaboration to Treat Overweight and Obese Children (Stanford GOALS). 2012. Available from: http://clinicaltrials.-gov/ct2/show/NCT01642836 NLM Identifier: NCT01642836. [Google Scholar]
- 40.National Heart L, and Blood Institute; University of Minnesota . ClinicalTrials.gov [Internet] National Library of Medicine (US); Bethesda (MD): [2013 Jun 11]. NET-Works: Community Preschooler Obesity Prevention. 2012. Available from: http://clinicaltrials.gov/ct2/show/NCT01606891 NLM Identifier: NCT01606891. [Google Scholar]