Abstract
We investigated geographical variations of three sexually transmitted infections (STIs) namely chlamydia, gonorrhea and syphilis in the greater Durban area, so as to optimize intervention strategies. The study population was a cohort of sexually active women who consented to be screened in one of three biomedical studies conducted in Durban. A total of nine local regions collectively formed three clusters at screening, five of which were previously defined as HIV hot-spots. STI cases were geo-coded at the census level based on residence at the time of screening. Spatial SaTScan Statistics software was employed to identify the areas with a disproportionate prevalence and incidence of STI infection when compared to the neighboring areas under study. Both prevalence and incidence of STIs were collectively clustered in several localized areas, and the majority of these locations overlapped with high HIV clusters and shared the same characteristics: younger age, not married/cohabitating and multiple sex partners.
Keywords: Sexual transmitted infections and risk behaviours, Spatial clustering, South Africa
Resumen
Se investigaron las variaciones geográficas de los tres infecciones de transmisión sexual (ITS), es decir, la clamidia, la gonorrea y la sífilis en el área metropolitana de Durban, con el fin de optimizar las estrategias de intervención. La población de estudio fue una cohorte de mujeres sexualmente activas que dieron su consentimiento para someterse a las pruebas en uno de los tres estudios biomédicos realizados en Durban. Un total de nueve regiones locales forman colectivamente tres grupos de investigación, cinco de los cuales fueron definidos previamente como VIH puntos calientes. Casos de ITS fueron geo-codificados a nivel censal basada en la residencia en el momento de la detección. Software Espacial Scan Estadísticas (SaTScan) fue empleado para identificar las zonas con una prevalencia desproporcionada e incidencia de ITS en comparación con las zonas vecinas en estudio. y la incidencia. ITS se agrupan colectivamente en varias zonas localizadas, y la mayoría de estos lugares se superponen con los clústeres de alta de VIH y comparte las mismas características: la edad más joven, no está casado/cohabitan y múltiples parejas sexuales.
Introduction
South Africa has the highest burden of human immunodeficiency virus (HIV) infection in the world with an estimated 5.6 million people infected in 2011 [1]. Other sexually transmitted infections (STIs), particularly chlamydia, gonorrhea and syphilis are also reported to cause morbidity in the region and have been linked to HIV transmission [2–5]. Unprotected heterosexual exposure has been reported to be the primary mode of HIV and STI transmission in this region with young sexually active adults being the most vulnerable population prone to these infections [6]. Additionally, recent epidemiological studies indicate a high incidence of both HIV and STIs among women, with low condom use being a contributing factor to transmission of infections [7, 8].
We have previously highlighted the importance of geographic clustering in the potential transmission of HIV infection [9, 10]. The current study represents a continuation of our previous work focusing on the identification of “high STI” in specific geographical areas.
We hypothesized that geographical clusters of STIs would potentially represent sexual networks that could overlap with the areas identified as hot-spots for HIV infections. We also investigated if demographic or sexual behavioural data could further differentiate the geographically distinct STI clusters in this region. If detected, these clusters may potentially represent relatively homogenous individuals, by splitting a large sexual network into smaller communities.
Methods
Study Areas and Geographical Data
Data from 5,753 sexually active women who consented to screening for three studies from six clinics and 158 census locations were combined for this study. The studies were as follows: the methods for improving reproductive health in Africa (MIRA) trial of the vaginal diaphragm for HIV prevention, took place at two sites between September 2002 and September 2005 (rural Umkomaas, 44 km south of Durban, and Botha’s Hill, 31 km west of Durban) [11]; the Microbicides Development Programme (MDP) feasibility study in preparation for Phase III microbicide trials, took place at two sites between August 2002 and September 2004 (semi-rural Tongaat, 31 km north of Durban, and Verulam, 22 km north of Durban) [12]; and the HIV Prevention Trials Network (HPTN 055) site-preparedness study for future implementation of Phase II/IIb/III clinical trials, took place at two sites between May 2003 and January 2005 (rural district of Hlabisa and urban Durban)[13].
Study Procedures
For the MIRA and HPTN 055 studies, HIV diagnostic testing was achieved using two rapid tests on whole blood sourced from either finger-prick or venepuncture (Determine HIV-1/2, Abbot Laboratories, Tokyo, Japan and Oraquick, Orasure Technologies, Bethlehem, PA, USA). For the MDP feasibility study, the Abbot IMX ELISA test (Abbot Diagnostics, Africa Division), in combination with the Vironostika HIV1/2 ELISA for positive and equivocal results, was used on whole blood sourced from venepuncture. In the MIRA trial, a first catch urine sample was collected for DNA PCR testing for chlamydia and gonorrhoea (Roche Pharmaceuticals, Branchberg, NJ, USA) at screening, while a blood sample was collected for syphilis [rapid plasma regain (RPR) and confirmatory TPHA (Omega Diagnostics, Alva, UK)]. In the HPTN 055 study, urine samples were collected for diagnosis of gonorrhoea and chlamydia using the BD Probe Tec ET assay (Becton–Dickinson, Sparks, MD). Syphilis was tested using RPR (BD Macro-Vue) and confirmed using TPHA (Serodia Fujirebio). The MDP feasibility study tested for chlamydia and gonorrhoea using PCR (COBAS Amplicor, Roche Molecular Diagnostics, Pleasanton, CA, USA); syphilis was tested by RPR and confirmatory TPHA (Omega Diagnostics, Alva, UK). Only women who had test results and geographical data were included in the study. At all visits, all participants received a comprehensive HIV prevention package consisting of HIV pre- and post-test counseling, intensive STI/HIV risk reduction counseling and treatment of curable, laboratory-diagnosed STIs. The studies were all approved by the local biomedical research ethics committee of the University of KwaZulu-Natal, Durban.
Detecting and Characterizing Clusters
The spatial scan statistics (SaTScan) [14–16] software (version 9.1, www.satscan.org) was used to detect the potential excess of STIs [17, 18]. Briefly, scan statistics were calculated at each geographical location to assess the number of excess STIs in the target population. Geographic data such as latitude and longitude for location were used as a proxy for residential area of women.
Stata (Version 12.0, CS, TX) software was also used to compare the characteristics of each cluster area with a non-cluster area. Chi square and Fisher’s exact tests were used to compare differences in proportions.
Results
Characteristics of Study Subjects
As described previously [9], the current study included data from the six clinical sites and 158 census locations where the predominantly black population was estimated to be approximately 2,400,000 (http://www.statssa.gov.za/publications/populationstats.asp). The geographical data of a total of 728 women who tested positive for any one of the STIs namely, chlamydia, gonorrhea and syphilis, at screening or enrolment were used to identify areas of high STI prevalence. Additionally, 680 women who were STI negative at screening but who tested positive during study follow-up were included in the analysis.
Hot-Spots of Increased STI Prevalence
The SaTScan analysis for significant spatial clustering for excess STI prevalence, after adjusting for the size of the study population and women’s age, is represented in Table 1. The analysis identified three clusters of high prevalence when compared to other study sites. These clusters included 175 cases (24 % of all cases) recruited from two study sites: a less urbanized clinic in Botha’s Hill and a peri-urban clinic in Umkomaas. The first cluster, which was within a 2.47 km radius in the south of Durban, had 78 cases from four residential areas: Umkomaas, Naidooville, Mkomazi and Saiccor (relative risk, RR = 10, p = 0.001). The second cluster involved 86 cases (RR = 8, p = 0.001) centered within 9.76 km radius and located exclusively west of Durban from four residential areas: Inchanga, Hammarsdale, Botha’s Hill and Cato-Ridge. The final cluster was made up by one residential area north-west of Durban, Molweni, which had 11 STI cases (RR = 51, p = 0.001).
Table 1.
Distribution of STI infection cases by districts at screening (age and population adjusted)
| Clusters | Radius (km) | Observed STI cases | Relative risk of excess STI cases | Test statisticsa | p value | Total locations |
|---|---|---|---|---|---|---|
| Cluster 1 | 2.47 | 78 | 10 | 212.11 | 0.001 | 3 |
| Cluster 2 | 9.76 | 86 | 8 | 29.38 | 0.001 | 4 |
| Cluster 3 | 0 | 11 | 51 | 19.23 | 0.001 | 1 |
1. Umkomaas, Naidooville, Mkomazi Drift and Saiccor; 2. Inchanga, Hammersdale, Botha’s Hill, Cato-Ridge; 3. Molweni
aFrom likelihood-ratio test
Hot-Spots of STI Incidence
A total of 2,523 HIV negative and STI negative (or treated) women enrolled in the three studies with a median duration of 12 months follow-up. Of these, 680 had tested positive at least once during the follow-up period (incidence rate of 20 per 100 person years). Using the SaTScan programme, and adjusting for the size of the population and women’s age, a total of 126 (19 % of the all STIs) of the women who tested positive for at least one STI during the follow-up period were geographically clustered into five hot-spots (Table 2). The highest incidence of STIs was observed in a cluster that comprised two census areas south of Durban, namely Umkomaas and Mkomazi, encompassing a radius of 2.64 km (RR = 12, p < 0.001). The second cluster was centred within ~6.5 km radius and included Inchanga, Hammarsdale (RR = 24, p < 0.001); Cato-Ridge, Molweni and Botha’s Hill were all identified to be the third, fourth and fifth clusters respectively.
Table 2.
Distribution of STI incidence by districts during the follow-up
| Clusters | Radius (km) | Observed STI incidence cases | Relative risk of excess HIV cases | Test statisticsa | p value | Total locations |
|---|---|---|---|---|---|---|
| Cluster 1 | 2.64 | 68 | 12 | 51.86 | 0.001 | 2 |
| Cluster 2 | 6.48 | 32 | 24 | 37.54 | 0.001 | 2 |
| Cluster 3 | 0 | 11 | 18 | 27.16 | 0.001 | 1 |
| Cluster 4 | 0 | 7 | 51 | 17.41 | 0.001 | 1 |
| Cluster 5 | 0 | 8 | 9 | 8.03 | 0.002 | 1 |
1. Umkomaas, Mkomazi; 2. Inchanga, Hammersdale; 3. Cato-Ridge; 4. Molweni; 5. Botha’s Hill
aFrom likelihood-ratio test
STI Hot-Spots in Relation to HIV Hot-Spots
Both previously reported HIV and the current STI studies consistently determined to be geographical locations in “west of Durban” and “south of Durban” with excess HIV and STI cases which broadly overlapped. Demographic characteristics and sexual risk behaviour of women who were living in the cluster areas (i.e. hot-spots) were compared with those who did not (Table 3).
Table 3.
Selected characteristics of the hot-spots
| Characteristics | Percentage (%) | HIV/STI hot-spots (%) | Rest of the study sites (%) | Test statisticsa | p value |
|---|---|---|---|---|---|
| Age groups (years) | 41.41 | <0.001 | |||
| <25 | 41 | 59 | 40 | ||
| 25–34 | 37 | 31 | 37 | ||
| 34+ | 22 | 10 | 23 | ||
| Language spoken | 68.41 | <0.001 | |||
| English | 12 | 19 | 9 | ||
| Zulu and other | 88 | 81 | 91 | ||
| Religious | 0.0192 | 0.890 | |||
| Christian | 91 | 91 | 91 | ||
| Other | 9 | 9 | 9 | ||
| Age at sexual debut | 2.02 | 0.155 | |||
| <16 | 21 | 20 | 22 | ||
| 16+ | 79 | 80 | 78 | ||
| Marital status | 10.95 | 0.001 | |||
| Not married | 85 | 92 | 84 | ||
| Married | 15 | 8 | 16 | ||
| Living with a regular partner | 22.52 | <0.001 | |||
| No | 70 | 82 | 69 | ||
| Yes | 30 | 18 | 31 | ||
| Lifetime number of sexual partners | 9.74 | 0.002 | |||
| Less than three | 53 | 43 | 53 | ||
| Three or more | 47 | 57 | 47 | ||
| Current contraceptive use | 2.08 | 0.198 | |||
| Injectables/pills | 42 | 42 | 42 | ||
| Male/female condoms | 26 | 27 | 25 | ||
| Others (e.g. none, traditional) | 32 | 30 | 33 |
aFrom Chi square test
Compared to those who were living outside the HIV/STI geographical hot-spots, women who were living in HIV/STI hot-spots were significantly younger (age <25, 59 vs. 40 %, p < 0.001), not married (92 vs. 84 %, p = 0.001), not cohabiting with their regular sex partners (82 vs. 69 %, p < 0.001) and they also reported a higher number of lifetime sexual partners (3+, 57 vs. 47 %, p = 0.002). A higher number of women in the HIV/STI hot-spots reported English as their preferred language (19 vs. 9 %, p < 0.001). Women were similar in terms of religion, age at sexual debut and type of contraceptive use regardless of whether they were living in one of the hot-spots or not.
Figure 1 shows the location of the excess STI and HIV cases. A total of nine local regions collectively formed three clusters, of which five of them were also previously defined as HIV hot-spots [9].
Fig. 1.
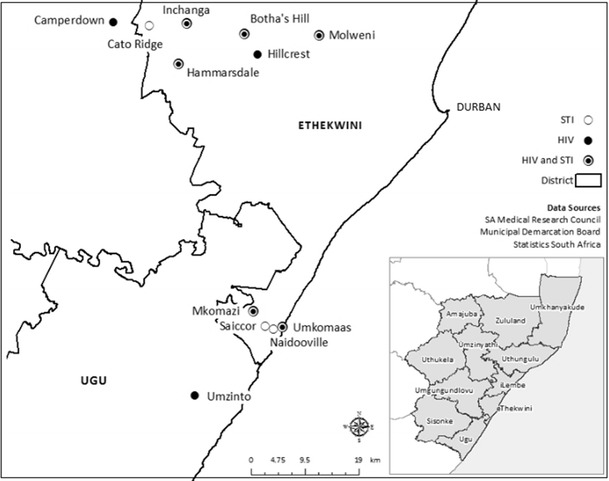
HIV/STI hot-spots
Discussion
Building on our previous data of identifying geographic excesses of HIV infections at rates among the highest in the world in certain rural communities of Durban, we have now identified excess cases for STIs with overlapping areas of excessive HIV infection. Additionally, the current study has identified three statistically significant areas of excess STI prevalence and incidence rates around the Umkomaas clinic (44 km south of Durban) and Botha’s Hill clinic (31 km west of Durban) with the inference that risks for chlamydia, gonorrhea and syphilis are associated with statistically definable socio-geographic locations. In terms of spatial persistence, these cluster areas were overlapped with the high HIV clusters (prevalence and incidence).
Determining the geographical variations of HIV and STIs is critical for targeting areas most in need of prevention interventions. Our study confirmed that “high transmission areas” overlap with high prevalence and incidence of HIV and STI cases. These high transmission areas are located predominantly in areas where HIV prevalence is higher than in neighbouring areas.
Our finding suggesting that the clusters for STIs overlap with HIV clusters is hardly surprising. Others have reported overlap of HIV/STI prevalence previously [19]. Finding overlapping areas of HIV and STI’s is not unusual as both these sexually transmitted infections share common demographic, social and sexual behavioural risk factors [20]. Furthermore it has been well documented that curable STIs are risk factors for HIV [21, 22]. For this reason, STI diagnosis and treatment is always included as part of HIV prevention package.
Our study has several limitations that need to be acknowledged. Due to the nature of the research conducted in these clinical trials, the study population selected could potentially be at higher risk for infection with HIV and other STIs. Therefore, the study population may not be representative of all women in the KwaZulu-Natal province. Furthermore, only six study sites were included in this analysis, which may not be fully representative of the region itself. We also cannot rule out the possibility that the findings could be due in part to unmeasured characteristics, such as commercial sex work or population migration.
Conclusion
Our studies of spatial and demographic variation in prevalence and incidence of STI infection suggested areas of high sexual networking, with poor condom use among young women in these communities. Data from our previous studies suggested that young women are particularly at high risk of both HIV and STI acquisition. Although South Africa has a generalised epidemic, there are pockets in communities which demonstrate concentrated epidemics. Identification of these pockets of “hot-spots” is critical for targeted biomedical behavioural and structural intervention to reduce the burden of HIV/STI in the communities.
Acknowledgments
We gratefully acknowledge the women who participated in the studies. We acknowledge the assistance of Dr. Nathlee Abbai, Dr. Brodie Daniels and Ms. Ramona Moodley for assistance in the preparation of the final manuscript. We acknowledge funding and support for the various studies from the UK Department for International Development and the Medical Research Council (MDP Feasibility Study: Grant number G0100137); the Bill & Melinda Gates Foundation (MIRA: Grant number 21082); and the Division of AIDS, NIH (HPTN055: Grant U01 AI048008). We would also like to thank the principal investigators/protocol chairs of the studies: Dr. Sheena McCormack, Dr. Nancy Padian, Prof Saidi Kapiga and Prof Stephen Weiss. Dr. Wand was funded by the Australian Government Department of Health and Ageing. The views expressed in this publication do not necessarily represent the position of the Australian Government.
Conflict of interest
The authors declare that they have no competing interests.
Compliance with ethical requirements
The study received ethical approval from the Biomedical Research Ethics Committee of the University of KwaZulu-Natal. This study is registered with ClinicalTrials.gov, number NCT00121459.
References
- 1.UNAIDS. UNAIDS report on the global AIDS epidemic 2011. Geneva: UNAIDS; 2012.
- 2.Chen L, Jha P, Stirling B, et al. Sexual risk factors for HIV infection in early and advanced HIV epidemics in sub-Saharan Africa: systematic overview of 68 epidemiological studies. PLoS One. 2007;2(10):e1001. doi: 10.1371/journal.pone.0001001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Taha T, Hoover D, Dallabetta G, et al. Bacterial vaginosis and disturbances of vaginal flora: association with increased acquisition of HIV. AIDS. 1998;12:1699–1706. doi: 10.1097/00002030-199813000-00019. [DOI] [PubMed] [Google Scholar]
- 4.Van Der Pol B, Kwok C, Pierre-Louis B, et al. Trichomonas vaginalis infection and Human Immunodeficiency Virus acquisition in African women. J Infect Dis. 2008;197:548–554. doi: 10.1086/526496. [DOI] [PubMed] [Google Scholar]
- 5.van de Wijgert J, Morrison C, Cornelisse P, et al. Bacterial vaginosis and vaginal yeast, but not vaginal cleansing, increase HIV-1 acquisition in African women. J Acquir Immune Defic Syndr. 2008;48:203–210. doi: 10.1097/QAI.0b013e3181743936. [DOI] [PubMed] [Google Scholar]
- 6.Ramjee G, Wand H, Whitaker C, et al. HIV incidence among non-pregnant women living in selected rural, semi-rural and urban areas in Kwazulu-Natal, South Africa. AIDS Behav. 2012;16(7):2062–71. [DOI] [PMC free article] [PubMed]
- 7.Wand H, Ramjee G. The effects of injectable hormonal contraceptives on HIV seroconversion and on sexually transmitted infections. AIDS. 2012;26(3):375–380. doi: 10.1097/QAD.0b013e32834f990f. [DOI] [PubMed] [Google Scholar]
- 8.Ramjee G, Wand H. Population-level impact of hormonal contraception on incidence of HIV infection and pregnancy in women in Durban, South Africa. Bull World Health Organ. 2012;90(10):748–755. doi: 10.2471/BLT.12.105700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wand H, Ramjee G. Targeting the hotspots: investigating spatial and demographic variations in HIV infection in small communities in South Africa. J Int AIDS Soc. 2010;13(1):41. doi: 10.1186/1758-2652-13-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wand H, Whitaker C, Ramjee G. Geoadditive models to assess spatial variation of HIV infections among women in local communities of Durban, South Africa. Int J Health Geogr. 2011 doi: 10.1186/1476-072X-10-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Padian N, van der Straten A, Ramjee G, et al. Diaphragm and lubricant gel for prevention of HIV acquisition in southern African women: a randomised controlled trial. Lancet. 2007;370(9583):251–261. doi: 10.1016/S0140-6736(07)60950-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nunn A, McCormack S, Crook A, Pool R, Rutterford C, Hayes R. Microbicides development programme: design of a phase III trial to measure the efficacy of the vaginal microbicide PRO 2000/5 for HIV prevention. Trials. 2009;10(1):99. doi: 10.1186/1745-6215-10-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ramjee G, Kapiga S, Weiss S, et al. The value of site preparedness studies for future implementation of phase 2/IIb/III HIV prevention trials: experience from the HPTN 055 study. J Acquired Immune Defic Syndr. 2008;47(1):93. doi: 10.1097/QAI.0b013e31815c71f7. [DOI] [PubMed] [Google Scholar]
- 14.Kulldorff M, Song C, Gregorio D, Samociuk H, DeChello L. Cancer map patterns: are they random or not? Am J Prev Med. 2006;30(2 Suppl):S37. doi: 10.1016/j.amepre.2005.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kulldorff M. Information Management Services, Inc: SaTScan version 7.0: software for the spatial and space-time scan statistics 2007.
- 16.Kulldorff M. Commentary: geographical distribution of sporadic Creutzfeldt-Jakob disease in France. Int J Epidemiol. 2002;31(2):495–496. doi: 10.1093/ije/31.2.495. [DOI] [PubMed] [Google Scholar]
- 17.Nunes C. Tuberculosis incidence in Portugal: spatiotemporal clustering. Int J Health Geogr. 2007;6(1):30. doi: 10.1186/1476-072X-6-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Risley CL, Ward H, Choudhury B, et al. Geographical and demographic clustering of gonorrhoea in London. Sexually Transm Infect. 2007;83(6):481–487. doi: 10.1136/sti.2007.026021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hayes R, Watson-Jones D, Celum C, van de Wijgert J, Wasserheit J. Treatment of sexually transmitted infections for HIV prevention: end of the road or new beginning? AIDS. 2010;24:S15. doi: 10.1097/01.aids.0000390704.35642.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zuma K, Lurie M, Williams B, Mkaya-Mwamburi D, Garnett G, Sturm A. Risk factors of sexually transmitted infections among migrant and non-migrant sexual partnerships from rural South Africa. Epidemiol Infect. 2005;133(3):421–428. doi: 10.1017/S0950268804003607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kalichman SC, Pellowski J, Turner C. Prevalence of sexually transmitted co-infections in people living with HIV/AIDS: systematic review with implications for using HIV treatments for prevention. Sexually Transm Infect. 2011;87(3):183–190. doi: 10.1136/sti.2010.047514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mavedzenge SN, Pol BVD, Cheng H, et al. Epidemiological synergy of trichomonas vaginalis and HIV in Zimbabwean and South African women. Sex Transm Dis. 2010;37(7):460. doi: 10.1097/OLQ.0b013e3181cfcc4b. [DOI] [PubMed] [Google Scholar]


