Abstract
New generation DES are effectively used in all spectrum of coronary artery diseases (CAD) and are replacing earlier DES and BMS. Biolimus A9™-eluting stent is a new generation DES containing the anti-proliferative drug biolimus A9™ incorporating a biodegradable abluminal coating that leaves a polymer-free stent after drug release enhancing strut coverage while preventing neointimal hyperplasia. A retrospective data analysis was done in patients treated with DES, with a major share of Biolimus A9™ (BA9™) drug-eluting stents (DES) at Bombay Hospital, Mumbai. A total of 158 patients with 219 lesions were treated with DES, comprising Biolimus A9-eluting stent and others and the major adverse cardiac events (MACE) rate and stent thrombosis (ST) at 1, 6, 12 months and 24 months were analyzed. Mace rate was 3.16 % for average follow-up of 19 months. There were 3 cases of ST (2 of acute and 1 of subacute onset) and one non-cardiac death reported during this time. This retrospective data demonstrates good one- and two-year clinical safety and efficacy of DES, especially of BioMatrix stents in real world setting.
Keywords: BioMatrix, Biodegradable polymer, Biolimus A9, Abluminal, Major adverse cardiac events
1. Introduction
Even though the clinical efficacy and safety in terms lower adverse event rates and target lesion revascularization of second generation polymer-based drug-eluting stents (DES) such as Everolimus [(EES), Xience®] and Zotarolimus [(ZES), Endeavor®] over bare-metal stents (BMS) has been shown,1–4 a lot of focus is still on development of newer generations of DES. This is because DESs still have late-stage disadvantages that might be attributable to the polymer. The newer generation DES platforms aim to address concerns of safety and improved efficacy. Biodegradable polymers and polymer-free drug delivery have shown to minimize vascular injury and delayed stent endothelialization. Newer generation DES with biodegradable polymers provide controlled drug release with subsequent degradation of the polymer rendering the stent surface more closely to a BMS after the period of biodegradation. The efficacy of biodegradable polymer coated DES has been shown to have non-inferior performance in terms of clinical and angiographic outcomes.5–7 Couple of other randomized trials have also supported these established results.8,9
DES have also demonstrated low rates of stent thrombosis (ST), especially the limus derivatives delivered from a durable polymer platform as compared to paclitaxel in several clinical trials.10–14 Interest in biodegradable polymer technology had emerged as a result of concerns over very late ST that is believed to result from the vascular inflammation and consequential delayed endothelialization associated with the polymers used in DES designs. DES involving biodegradable polymers offer early benefits of reducing neointimal proliferation while reducing the risk of very late ST.
BioMatrix stents have a stainless steel stent platform that is combined with the anti-proliferative drug Biolimus A9™, a lipophilic sirolimus analog that is bound to the stent platform via a poly-lactic acid, a biodegradable polymer that biodegrades within 6–9 months. The BioMatrix stent design was compared with the Cypher SES with permanent polymer in the randomized, all-comers LEADERS trial and was shown to be non-inferior for MACE (composite of cardiac death, myocardial infarction, and ischemia-driven revascularization) and 80% relative risk reduction of very late stent thrombosis (1–4 years).15,16 Biolimus eluting stents have also demonstrated good safety and efficacy profile in other randomized trials.17,18 The market approval of various DESs was based on data generated from various clinical trials5,15–17 which included low- to moderate-risk patients but majority of patients treated in routine clinical practice fall outside the approved indications of DES. A couple of post marketing registry studies involving DESs are also being done, which will further add to extrapolate the clinical outcomes and long term safety of these devices in real world setting.
Newer generation DESs are also being used in clinical practice if available by cardiologist to treat patients with STEMI undergoing Percutaneous Coronary Intervention (PCI). This report includes the safety and clinical outcomes of patients in terms of MACE rate and ST for a period of around 2 years who received DES with a major share of Biolimus A9™-eluting stents during PCI at Bombay Hospital, Mumbai.
2. Methodology
This is a retrospective analysis of data from patients who underwent angioplasty at Bombay Hospital, Mumbai in India between January 2009 and March 2012. The primary objective of this analysis was to determine device oriented major adverse cardiac events (MACE) defined as composite of cardiac death, myocardial infarction [MI], or target vessel revascularization [TVR], and stent thrombosis (ST).
The criteria for inclusion of data for analysis were patients who had undergone PCI with lesions suitable for stent implantation with Biolimus A9™-eluting stent and/or other DES and presence of ≥1 coronary artery stenoses in a native coronary artery and saphenous bypass graft or radial vein graft that can be covered with one or multiple stents with no limitation to the number of treated lesions, number of treated vessels or lesion length.
Implantation of DES in each target lesion during the index procedure was done as per the standard procedure. All post-operative medical management, including dual antiplatelet therapy, was prescribed according to usual local practice at the discretion of the cardiologist. The available data collected as part of standard medical care including demographic information, lesion and stent characteristics, and on events, if any, were analyzed. The follow up data of the patients were recorded as and when patients attended the clinic and was considered for analysis. Review and analysis of all MACE and ST were done from available hospital records including electrocardiograms, and angiograms, when necessary.
All statistical analyses were performed with SPSS (Version 16.0). Standard descriptive statistics were used for baseline, lesion, and procedural characteristics and for clinical results for all patients. Continuous variables were presented as mean ± SD and range, and categorical variables were presented as numbers and percentages. Descriptive data of the patient population and serious adverse events were compiled as per protocol specified time intervals.
3. Overall results
The study population included a total of 158 consecutive patients at Bombay Hospital, Mumbai who underwent single or multi-vessel revascularization between January 2009 and March 2012 with 219 lesions treated with Biolimus A9™-eluting stents and other DES. Patients' baseline demographics are summarized in Table 1 and Fig. 1. Lesion characteristics and lesion stent characteristics are shown in Tables 2 and 3, respectively. The mean age was 57.57 ± 12 years. A total of 242 biolimus eluting stents were implanted during the index procedure. In more than half of the patients, 63.3% had lesions that were ≤2.75 mm in diameter and 39.9% patients had long length lesions (stent length ranged between 8 and 28 mm). Almost three fourths of the patients (74.5%) had single vessel disease and most of the lesions were located in the left anterior descending artery (75.31%). On average, 1.53 stents were used to treat 1.38 lesions per patient. Hybrid stenting (additional stent implantation other than Biolimus A9™-eluting stent) was done in a total of 23 patients.
Table 1.
Baseline characteristics.
| Baseline characteristics | N (%) |
|---|---|
| Age group (years) | |
| 20–39 | 11 (8.14) |
| 40–59 | 69 (51.11) |
| 60–79 | 50 (37.03) |
| ≥80 | 05 (3.7) |
| Gender | |
| Female | 18 (11.4) |
| Male | 140 (88.6) |
Fig. 1.
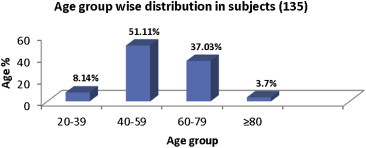
Age group wise comparison.
Table 2.
Characteristics of lesions treated in 158 subjects.
| Lesion characteristics | |
| Single Vessel Disease (SVD) | 117 (74.5) |
| Multi Vessel Disease (MVD) | 36 (22.78) |
| Triple Vessel Disease (TVD) | 05 (3.16) |
| Lesion segments | |
| Total no. of lesion segment | N (219) (%) |
| RCA | 42 (26.58) |
| LAD | 119 (75.31) |
| LCX | 51 (32.27) |
| Left main | 05 (3.16) |
| Ramus | 02 (1.27) |
Table 3.
Characteristics of lesion stent in 158 subjects.
| Parameters | N (%) |
|---|---|
| Total no. of lesion segments | 219 |
| Lesions per patient | 1.38 |
| Total no. of stents used | 242 |
| No. of stents used per patient | 1.53 |
| Long lesion stent length (28 mm) | 63 (39.87) |
| Small vessel (≤2.75 mm) | 100 (63.29) |
This analysis includes average clinical follow up of 1 year and 7 months (588 days) in 158 patients. The cumulative rates of adverse clinical events and overall ST classification are presented in Table 4. MACE rate was 3.16 if calculated for average follow up of 1 year and 7 months. There were 3 cardiac deaths and 2 cases of TVR reported. Of 3 patients who developed ST, two presented with acute onset and one with sub-acute onset. All the patients who had stent thrombosis were having elevated creatinine value and eGFR less than 30. There was only one case of non-cardiac death reported.
Table 4.
Cumulative rates of adverse clinical events up to 1 year.
| MACE (major adverse cardiac event) | N | Total MACE | Rate |
|---|---|---|---|
| Cardiac death | 3 | 5 | 3.16 |
| Myocardial infarction | 0 | ||
| TVR | 2 |
| Stent thrombosis | Acute | Sub-acute | Late | Very late |
|---|---|---|---|---|
| Definite | 2 | 0 | 0 | |
| Probable | 0 | 1 | 0 | 0 |
| Possible | 0 | 0 | 0 | 0 |
*Major Adverse Cardiac Events (MACE) within the study population, defined as composite of cardiac death, myocardial infarction (Q-wave and non-Q-wave), or justified target vessel revascularization at 12 months.
4. Discussion
The safety and efficacy of BioMatrix been established in several large randomized controlled trials including LEADERS trial.8 Biolimus eluting stents also performed well in unselected patient registry trial19 and randomized BES trial compared to PES.11
The Biolimus A9™-eluting stent system has shown good results in terms of low rates of MACE (cardiac death, TVR and MI) in this retrospective analysis. The results may be considered as significant attesting favorable clinical outcome of Biolimus A9™-eluting stents in real world setting. In this analysis, considering small sample size of patients who received BES stents, MACE rate (Cardiac death, MI, TVR) (3.16 if calculated for average follow up of 1 year and 7 months.) and ST were significantly lower. There were only 3 reported cases of ST and there was not a single case of late onset ST. These results are comparable to the recent real world registry trials20–22 of newer generation DESs. This 2-year clinical outcome data which showed apparent clinical benefit was primarily attributable to reduced risk of very late definite ST and this is quite supportive of an indication of long term benefit of BA9-eluting stent. The findings from this analysis thus supports favorable outcome from randomized and post marketing registry trials of BioMatrix stent involving patients with STEMI undergoing PCI in real world setting.
5. Market challenges
The introduction of drug-eluting stent (DES) technology with significant reductions in the rates of target lesion revascularization (TLR) and major adverse cardiac events (MACE) has dramatically altered the landscape of coronary artery disease (CAD) revascularization. Innovation is occurring rapidly in the coronary stents industry with technology advancing at a fast pace. The prevalence of CAD and associated co-morbid conditions such as hypertension, diabetes and obesity is likely to increase and stimulate the demand for coronary stents. Despite the progress achieved with the first-generation DES, Cypher® and Taxus®, rates of MACE at 5 years remain high.23 Hence, newer generation DES such as stents with biodegradable polymers, are projected to increase the use of stents in interventional cardiology as the current data suggests that biodegradable polymer stents have the potential to reduce the safety concerns of durable polymer stents. Drug, Biolimus A9 is ten times lipophilic than its analogs, the property that ensures very much targeted action of it. Apart from having biodegradable polymer, BioMatrix stent has a coating on the outer surface (abluminal) thereby reducing systemic exposure of drug and risk of stent thrombosis to a great extent.
6. Limitations
The results from this analysis reflect a minority of the patients treated at only one hospital with Biolimus A9™-eluting and other stents. Secondly, the analysis was single-arm with no control arm for direct comparison. Also, this being a retrospective analysis, a few variables might have been missed for analysis.
7. Conclusion
In conclusion, MACE rate and ST in this small cohort of general patients treated with Biolimus A9™-eluting stents were comparable to previously published data of clinical trials as well as post marketing surveillance registry studies. This retrospective data demonstrates that Biolimus A9™ DES, BioMatrix has a favorable clinical outcome compared to any other DES available in the market.
8. Recommendation
Trial like LEADERS has shown that a combination of Biodegradable polymer PLA, highly lipophilic Biolimus A9™ drug and its abluminal coating over a Juno platform is safe and effective as compared to a permanent polymer limus eluting stent. Our experience in Bombay Hospital confirms this. We strongly recommend BioMatrix and BioMatrix Flex Biolimus A9™-eluting stent in the treatment of CAD. This new generation stent not only treats de novo lesions but is helping complex patients and is effective in the management of STEMI also.
Conflicts of interest
Dr. Bhushan Khemnar and Dr. Hrishikesh Rangnekar are employees of Biosensors International.
References
- 1.Serruys P., Ong A., Piek J.J. A randomized comparison of a durable polymer everolimus-eluting stent with a bare metal coronary stent: the SPIRIT first trial. EuroIntervention. 2005;1:58–65. [PubMed] [Google Scholar]
- 2.Tsuchida K., Garcia-Garcia H.M., Ong A.T. Revisiting late loss and neointimal volumetric measurements in a drug-eluting stent trial: analysis from the SPIRIT FIRST trial. Catheter Cardiovasc Interv. 2006;67:188–197. doi: 10.1002/ccd.20581. [DOI] [PubMed] [Google Scholar]
- 3.Fajadet J., Wijns W., Laarman G.J. Long-term follow-up of the randomised controlled trial to evaluate the safety and efficacy of the zotarolimus-eluting driver coronary stent in de novo native coronary artery lesions: five year outcomes in the ENDEAVOR II study. EuroIntervention. 2010;6:562–567. doi: 10.4244/EIJV6I5A95. [DOI] [PubMed] [Google Scholar]
- 4.Meredith I., Rothman M., Erglis A., E-Five Investigators Extended follow-up safety and effectiveness of the Endeavor zotarolimus-eluting stent in real-world clinical practice: two-year follow-up from the E-Five Registry. Catheter Cardiovasc Interv. 2011;77:993–1000. doi: 10.1002/ccd.22803. [DOI] [PubMed] [Google Scholar]
- 5.Windecker S., Serruys P.W., Wandel S. Biolimus-eluting stent with biodegradable polymer versus sirolimus-eluting stent with durable polymer for coronary revascularisation (LEADERS): a randomised non-inferiority trial. Lancet. 2008;372:1163–1173. doi: 10.1016/S0140-6736(08)61244-1. [DOI] [PubMed] [Google Scholar]
- 6.Ahmed T.A., Bergheanu S.C., Stijnen T., Plevier J.W., Quax P.H., Jukema J.W. Clinical performance of drug-eluting stents with biodegradable polymeric coating: a meta-analysis and systematic review. EuroIntervention. 2011 Aug;7:505–516. doi: 10.4244/EIJV7I4A81. [DOI] [PubMed] [Google Scholar]
- 7.Van der Giessen W.J., Lincoff A.M., Schwartz R.S. Marked inflammatory sequelae to implantation of biodegradable and nonbiodegradable polymers in porcine coronary arteries. Circulation. 1996;94:1690–1697. doi: 10.1161/01.cir.94.7.1690. [DOI] [PubMed] [Google Scholar]
- 8.Mehilli J., Byrne R.A., Wieczorek A. Randomized trial of three rapamycin-eluting stents with different coating strategies for the reduction of coronary restenosis. Eur Heart J. 2008;29:1975–1982. doi: 10.1093/eurheartj/ehn253. [DOI] [PubMed] [Google Scholar]
- 9.Byrne R.A., Kastrati A., Kufner S. Randomized, non-inferiority trial of three limus agent-eluting stents with different polymer coatings: the Intracoronary Stenting and Angiographic Results: Test Efficacy of 3 Limus-Eluting Stents (ISAR-TEST-4) Trial. Eur Heart J. 2009;30:2441–2449. doi: 10.1093/eurheartj/ehp352. [DOI] [PubMed] [Google Scholar]
- 10.Wenaweser P., Daemen J., Zwahlen M. Incidence and correlates of drug-eluting stent thrombosis in routine clinical practice. 4-year results from a large 2-institutional cohort study. J Am Coll Cardiol. 2008;52:1134–1140. doi: 10.1016/j.jacc.2008.07.006. [DOI] [PubMed] [Google Scholar]
- 11.Caixeta A., Leon M.B., Lansky A.J. 5-year clinical outcomes after sirolimus-eluting stent implantation. Insights from a patient-level pooled analysis of 4 randomized trials comparing sirolimus-eluting stents with bare-metal stents. J Am Coll Cardiol. 2009;54:894–902. doi: 10.1016/j.jacc.2009.04.077. [DOI] [PubMed] [Google Scholar]
- 12.Stone G.W., Midei M., Newman W. Randomized comparison of everolimus-eluting and paclitaxel-eluting stents: two-year clinical follow-up from the Clinical Evaluation of the Xience V Everolimus Eluting Coronary Stent System in the Treatment of Patients with de novo Native Coronary Artery Lesions (SPIRIT) III trial. Circulation. 2009;119:680–686. doi: 10.1161/CIRCULATIONAHA.108.803528. [DOI] [PubMed] [Google Scholar]
- 13.Kedhi E., Joesoef K.S., McFadden E. Second-generation everolimus-eluting and paclitaxel-eluting stents in real-life practice (COMPARE): a randomised trial. Lancet. 2010;375:201–209. doi: 10.1016/S0140-6736(09)62127-9. [DOI] [PubMed] [Google Scholar]
- 14.Smits P., Kedhi E., Royaards K.-J. 2-year follow-up of a randomized controlled trial of everolimus- and paclitaxel-eluting stents for coronary revascularization in daily practice. COMPARE (Comparison of the everolimus eluting XIENCE-V stent with the paclitaxel eluting TAXUS LIBERTÉ stent in all-comers: a randomized open label trial) J Am Coll Cardiol. 2011;58:11–18. doi: 10.1016/j.jacc.2011.02.023. [DOI] [PubMed] [Google Scholar]
- 15.Garg S., Sarno G., Serruys P.W. The twelve-month outcomes of a biolimus eluting stent with a biodegradable polymer compared with a sirolimus eluting stent with a durable polymer. EuroIntervention. 2010;6:233–239. [PubMed] [Google Scholar]
- 16.Stefanini G.G., Kalesan B., Serruys P.W. Long-term clinical outcomes of bio-degradable polymer biolimus-eluting stents versus durable polymer sirolimus-eluting stents in patients with coronary artery disease (LEADERS): 4 year follow-up of a randomised non-inferiority trial. Lancet. 2011 Dec 3;378:1940–1948. doi: 10.1016/S0140-6736(11)61672-3. [DOI] [PubMed] [Google Scholar]
- 17.Kadota K., Muramatsu T., Iwabuchi M. Randomized comparison of the Nobori biolimus A9-eluting stent with the sirolimus-eluting stent in patients with stenosis in native coronary arteries. Catheter Cardiovasc Interv. 2011 Jul 29 doi: 10.1002/ccd.23280. [DOI] [PubMed] [Google Scholar]
- 18.Danzi G.B., Chevalier B., Ostojic M., Hamilos M., Wijns W. Nobori drug eluting stent system: clinical evidence update. Minerva Cardioangiol. 2010;58:599–610. [PubMed] [Google Scholar]
- 19.Danzi G.B., Chevalier B., Urban P. Clinical performance of a drug-eluting stent with a biodegradable polymer in an unselected patient population: the NOBORI 2 study. EuroIntervention. 2012 May 15;8:109–116. doi: 10.4244/EIJV8I1A17. [DOI] [PubMed] [Google Scholar]
- 20.Von Birgelen C., Basalus M.W., Tandjung K. A randomized controlled trial in second-generation zotarolimus-eluting Resolute stents versus everolimus-eluting Xience V stents in real-world patients: the TWENTE trial. J Am Coll Cardiol. 2012 Apr 10;59:1350–1361. doi: 10.1016/j.jacc.2012.01.008. [DOI] [PubMed] [Google Scholar]
- 21.Seth A. XIENCE V India single arm study: 2-year clinical follow-up. Heart. 2011;97:479. [PubMed] [Google Scholar]
- 22.Meredith I.T., Verheye S., Dubois C.L. Primary endpoint results of the EVOLVE trial: a randomized evaluation of a novel bioabsorbable polymer-coated, everolimus-eluting coronary stent. J Am Coll Cardiol. 2012 Apr 10;59:1362–1370. doi: 10.1016/j.jacc.2011.12.016. [DOI] [PubMed] [Google Scholar]
- 23.Räber L., Wohlwend L., Wigger M. Five-year clinical and angiographic outcomes of a randomized comparison of sirolimus-eluting and paclitaxel-eluting stents: results of the Sirolimus-Eluting Versus Paclitaxel-Eluting Stents for Coronary Revascularization LATE trial. Circulation. 2011;123:2819–2828. doi: 10.1161/CIRCULATIONAHA.110.004762. [DOI] [PubMed] [Google Scholar]


