Abstract
Objective
To estimate prevalence of urinary incontinence (UI) health care utilization in women from the population to specialty care.
Method
The General Longitudinal Overactive Bladder Evaluation – UI (GLOBE-UI) is a population-based study on the natural history of UI in women ≥ 40 years of age. Prevalence of UI was estimated by using the bladder health survey (BHS). Survey data were linked with electronic health records to build the different steps of the iceberg of disease. Descriptive statistics were used to estimate the prevalence estimates at all levels of the iceberg.
Results
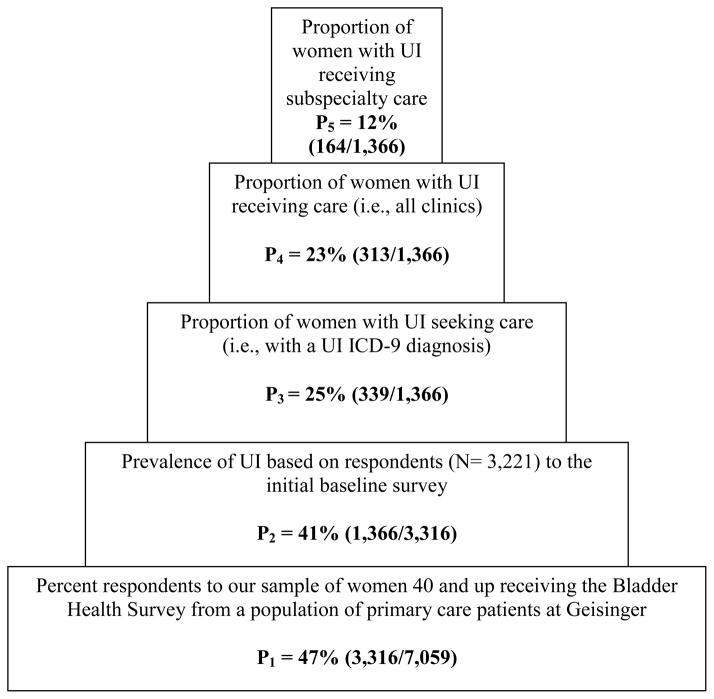
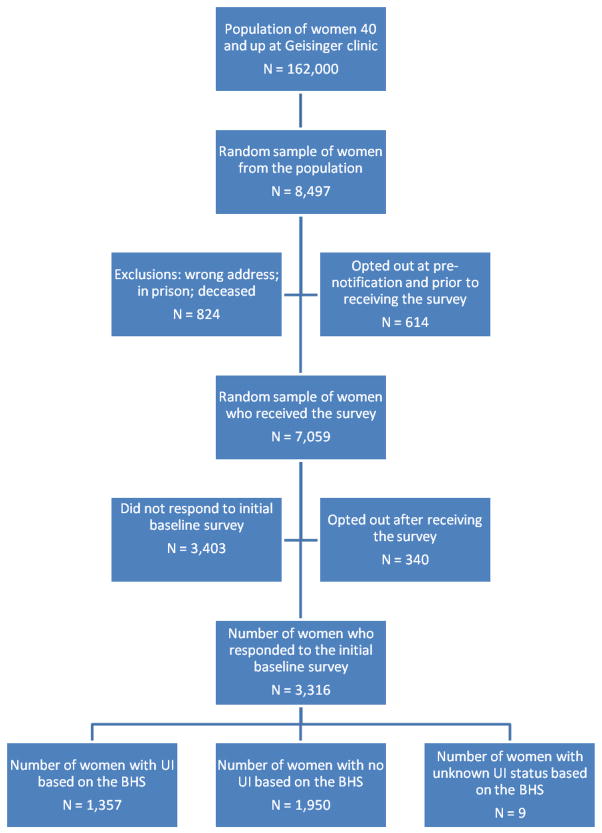
A total sample of 7,059 women received the BHS. Of those, 3,316 (47%) responded. Prevalence of UI was 1,366 (41%). Women with or without UI did not differ by age or marital status. However, women with versus without UI were more parous (91% vs 87%), significantly more overweight or obese (74% vs 61%), and more likely to have a college education or higher (54% vs 46%), P<0.01. Nine-hundred fifty eight (73%) women with UI reported duration of more than two years and 72% reported moderate to severe UI symptoms. Of all 1,366 women with BHS UI diagnosis, only 339 (25%) sought care, 313 (23%) received some care, and 164 (12%) received subspecialty care.
Conclusion
UI is a highly prevalent disease. Only a minority with UI appears to seek care and a fraction sees a pelvic floor specialist. It is important not only to educate women, but also primary care providers about this highly prevalent yet treatable condition.
Keywords: Urinary Incontinence, prevalence, health care seeking
INTRODUCTION
Urinary incontinence (UI) is a condition that affects women of all ages with a major impact on quality of life[1–3]. Its prevalence increases with age, with estimates as high as 50% in the community[4–6]. Little is known about use of health care for UI in the general population. It is estimated that less than 25% of women seek care for UI [7–10], similar to other chronic conditions such as arthritis [11] and migraine [12]. Most UI research is based on women with clinically significant UI with limited data on early stages of UI. Consequently, knowledge of the natural history of UI is limited to the “tip of the iceberg”, a select group of women with advanced UI (i.e., where symptoms have become severe enough to have an impact on quality of life).
One way to better understand the natural history of UI is to study utilization of care. This may reveal health seeking behaviors of women with UI with a perspective on prevalence of meaningful UI versus sporadic symptoms. This in turn can have implications for health costs, distribution and delivery of health care. Previous studies have reported on UI care seeking and delivery using either claims data alone [13] or self reported use of care from surveys [8,9,14]. Such studies show that women with UI who seek care are older, have more severe symptoms of longer duration, and have UI with significant bother and impact on quality of life.
By linking population-based survey data with patients’ electronic health records, our objective was to estimate prevalence estimates of UI and health care utilization in women from the population all the way up to subspecialty care.
METHODS
We used data from the baseline survey of the General Longitudinal Overactive Bladder Evaluation – Urinary Incontinence (GLOBE-UI), a population-based study of the natural history of UI in women ≥ 40 years of age. The original GLOBE study is described in detail elsewhere [15,16]. Here, we summarize the source population, the study cohort, the bladder health survey (BHS), the electronic health records (EHR), and definitions used. We also present in detail how we link data from the BHS to the EHR to estimate different prevalence estimates of UI care seeking and delivery. The Geisinger Health System (GHS) IRB approved the study.
Source Population and Data
GHS is an integrated healthcare system in Pennsylvania. The source population of our study was patients receiving primary care from one of the 38 community practice or hospital-based primary care clinics. These are part of the Geisinger Clinic (GC) serving a 31-county region. The GC based population is stable with census data indicating, with the exception of two counties, out migration rate is less than 1% per year. GC has started using EHR in its ambulatory care sites in 2001, and was fully implemented across all clinic sites with reliable information in 2004. The EHR contains all encounter related data (e.g., clinical notes, orders, labs, procedures, vitals, education, marital status, etc). All orders and visits are linked to one or more ICD9 diagnoses.
GLOBE-UI Cohort
The GLOBE-UI is a second generation longitudinal study initiated in 2009. It is a follow-up to the original GLOBE study conducted from 2006 to 2008. In the current GLOBE-UI study, a new random sample of 8,497 primary care patients was selected from 162,000 eligible patients of the GC, if they were female, ≥40 years of age, assigned to a primary care physician, and had at least one visit in the past 4 years. Before mailing the BHS, patients were mailed a pre-notification letter that invited participation in the survey. Participants were given the chance to opt out of the study by calling a toll free number. Nine-hundred fifty four (11%) patients opted out: 614 opted out before and 340 opted out after receiving the survey. Patients were informed that they would receive a survey every 6-months over a period of four and a half years (total of nine questionnaires). A $2 bill was included in the mailing as nominal compensation. Two weeks after the initial mailing, all non-responders received the same questionnaire as a reminder. To date, the first three waves of the nine 6-month mailings have been completed.
Bladder Health Survey
The BHS is a validated questionnaire with questions on urinary urgency, frequency, nocturia, UI, adaptive behaviors, bother, and impact on quality of life [15,16] [15,16]. Additional areas of inquiry include duration of time with urine loss, Sandvick’s UI severity index [17], age, weight and height, parity, marital status, education, and other possible confounding factors. The BHS was designed to obtain data on lifetime, and previous 6-month and 4-week bladder symptoms. For this analysis, the baseline BHS administered in the fall of 2009 was used as the data source for the denominator of the prevalence estimates.
BHS-based definition of UI
Cases of UI were identified based on responses to the baseline BHS. A non-case individual was defined if any of the following criteria from the survey were met: 1) responded as having no lifetime UI symptoms by answering “no” to two screening UI questions (i.e., “Since age 18, have you ever lost urine, even a small amount at least once a month?” and “Since age 18, did you ever lose more than a few drops or small amount of urine at least once a month?”) (N = 1,346); 2) had a combination of “yes” or “missing answer” to the two screening lifetime UI questions but who, on subsequent questions, also reported UI of no significant duration or severity (N = 584); 3) had one “yes” and one “no” answers to the screening questions and who answered inconsistently to follow-up UI questions (N = 15); or 4) reported that their past UI symptoms were either due to urinary tract infections or pregnancy (N = 5).
Conversely, women who answered affirmatively to both UI screening questions, or those who, on subsequent questions, reported UI of significant duration and severity, or reported change in behavior due to UI symptoms were considered to be cases (N = 1,357). There were 9 patients whose case status could not be determined. For the purpose of this study, these 9 cases were grouped with the cases.
Electronic Health Record Data
Data were extracted from the GC EHR for those originally contacted for the baseline BHS. We used EHR data from January 1, 2004 through October 28, 2010, the date of the data pull. Patient EHRs were queried to identify the number of GLOBE-UI survey participants with a clinical UI diagnosis, or health care related to UI. A patient was defined as having a clinical UI diagnosis if they had any one of the following EHR documentation: 1) the following ICD9 codes associated with two or more encounters or dates: urge UI (788.31, 788.36, 788.39); detrusor instability (596.55); stress UI (788.32, 788.35, 625.6, 599.84); mixed UI (788.33); other UI (788.30, 788.34, 788.37, 788.38, 596.54, 596.55, 596.59); 2) one or more of the following prescription medications associated with a UI diagnosis: oxybutinin, tolterodine, hyoscyamine, solifenacin, darifenacin, fesoterodine, and trospium chloride; 3) one or more of the following CPT surgical codes including collagen injections (51715), implantation of neurostimulator (64581), repair of vesico-vaginal fistula (57320), retropubic urethropexy (51990, 51840, 70051990), and vaginal sling (57288); or 4) a referral order to physical therapy, urogynecology and female urology with one of the UI diagnoses above. Finally, charts of women whose EHR UI diagnoses were not clear were individually reviewed for final case status designation. These were women who either had only one occurrence of a UI ICD9 diagnosis, or were on an anticholinergic medication or were referred to a specialist linked with a non-UI ICD9 diagnosis (e.g., recurrent UTI’s, kidney stones, OAB with no UI, prolapse with no UI).
Analysis
We defined use of health care for UI in a hierarchical manner. First, a random sample was drawn from the population of all GC primary care female patients ≥40 years. Responders (N = 3,316) to the BHS at baseline represented the eligible population. UI cases out of responders were identified from BHS-based UI criteria discussed above, which was the second step. The third step included women with clinical diagnosis of UI who had sought care during the study period from EHR. The fourth step included the proportion of women receiving care for their UI. These women were a subset of the previous step who also had EHR documentation of anti-incontinence prescription order, a referral to physical therapy or subspecialty clinic for UI, or a CPT code for an anti-incontinence procedure. Finally, step five included the proportion of women who were seen in subspecialty clinic for UI. These were a subset of women from step 4 with EHR documentation of urogynecology and a female urology office visit (Figure 1). Descriptive statistics were used to summarize the prevalence estimates at UI cases identified by BHS (Table 1). Baseline characteristics were reported as percentages for categorical variables.
Figure 1.
Iceberg of Disease in Women 40 Years of Age and Over
UI – urinary incontinence
ICD-9 – International Classification of Diseases, Ninth Revision
Table 1.
Demographic characteristics
| All respondents N = 3,316 |
Respondents with UI N = 1,366 |
Respondents with no UI N = 1,950 |
P – value | |
|---|---|---|---|---|
|
| ||||
| Age (years): | ||||
| 40–49 | 772 (24%) | 310 (23%) | 462 (24%) | 0.85 |
| 50–59 | 893 (27%) | 371 (27%) | 522 (27%) | |
| 60–69 | 753 (23%) | 323 (24%) | 430 (22%) | |
| 70–79 | 544 (17%) | 221 (16%) | 323 (17%) | |
| 80+ | 311 (10%) | 127 (9%) | 184 (10%) | |
|
| ||||
| BMI (kg/m2): | ||||
| <25 | 1104 (33%) | 352 (26%) | 752 (39%) | P < 0.001 |
| 25–29.9 | 953 (29%) | 374 (27%) | 579 (30%) | |
| 30–34.9 | 654 (20%) | 308 (23%) | 346 (18%) | |
| 35+ | 598 (18%) | 329 (24%) | 269 (14%) | |
|
| ||||
| Parity: | ||||
| 0 | 360 (11%) | 124 (9%) | 236 (12%) | 0.004 |
| 1+ | 2,842 (89%) | 1,207 (91%) | 1,635 (88%) | |
|
| ||||
| Marital status | ||||
| Married | 2,117 (65%) | 870 (64%) | 1,247 (65%) | 0.09 |
| Widowed | 506 (16%) | 221 (16%) | 285 (15%) | |
| Separated or divorced | 467 (14%) | 202 (15%) | 265 (14%) | |
| Never married | 174 (5%) | 58 (4%) | 116 (6%) | |
|
| ||||
| Education | ||||
| 11th grade or less | 269 (8%) | 104 (8%) | 165 (9%) | <0.001 |
| High school graduate | 1,377 (43%) | 514 (39%) | 863 (45%) | |
| Some college | 789 (25%) | 377 (28%) | 412 (22%) | |
| College graduate | 452 (14%) | 195 (15%) | 257 (14%) | |
| Post-graduate work | 330 (10%) | 143 (11%) | 187 (10%) | |
|
| ||||
Numbers in columns do not add up to total number in each group due to missing values
P value was calculated using Chi-square test.
RESULTS
The estimated available population pool of women ≥ 40-year-old was 162,000. A random sample of 8,497 EHRs was drawn for the survey. After excluding women who refused or opted out, had wrong addresses, or were deceased or in prison, the sample of women receiving the baseline BHS was 7,059. A total of 3,316 (47%) women responded to wave 1 of the baseline survey. Prevalence of survey-based UI was 1,366, or 41% of all respondents (Figure 2). Women with or without UI were similar across all age categories and marital status. Women with UI (74%) were significantly more overweight or obese compared to women with no UI (61%). Moreover, women with UI versus without UI were more likely to be parous (91% versus 87%) and with a college education or higher (54% versus 46%) (Table 1).
Figure 2.
Flow chart of patients
BHS – Bladder Health Survey
UI – urinary incontinence
Of the UI cases, 353 (26%) reported UI symptoms for the first time in the previous 2 years; 365 (27%) reported first UI onset 2 to 4 years ago, and 328 (24%) reported first onset 5 to 10 years ago. Finally, 265 (20%) women reported more than 10 years history of UI. Based on the Sandvick severity score, 28% of women had mild UI, 53% had moderate UI, and 19% had severe UI.
Using the clinical algorithm based on EHR data, 827 women met criteria for clinical UI diagnosis. In addition, review of the individual charts of 30 patients whose UI diagnosis was not clear revealed an additional 9 cases. These were subsequently added to the UI case pool resulting in 838/7,059 (12%) women. Prevalence of clinical UI in responders (443/3,316 (13%)) was higher than that in non-responders (395/3,743 (11%)), (P<0.001) indicating that patients with UI diagnosis may be more likely to respond to the survey. However, of all 1,366 women with survey diagnosis of UI, only 339 (25%) had a clinical UI diagnosis in the EHR, 313 (23%) women were receiving UI related care, and 164 (12%) were referred to or were being seen by urogynecology or female urology subspecialty care (see Figure 1).
Of the 1950 non-cases based on the BHS, there were 104 (5%) false negative cases. Namely, these were women with EHR UI diagnosis and a non-case status based on the survey. Of those, 35 women were considered to be in remission: 27 women had their initial clinical UI diagnosis over 5 years ago, and they reported no UI at baseline, 6- and 12-month follow-up surveys; 8 women had previous surgery or treatment for UI and were also considered to be in remission. There were 5 women whose first EHR UI diagnosis was at the time of survey administration or later and were considered new onset UI cases subsequent to survey administration. Forty-five women were subsequently defined as UI based on their follow-up 6- and 12-months surveys. The status of the remaining 19 potentially false negative cases remained undetermined: 10 with no follow-up survey or incomplete data to ascertain true case status, and 9 continued to have no UI symptoms at follow-up (Table 2).
Table 2.
False Negative cases
| Justification of False Negative cases | Total N = 104 |
|---|---|
| - In remission | 35 (34%) |
| - New onset | 5 (5%) |
| - Identified at 6- or 12- month f/u | 45 (43%) |
| - Incomplete data | 10 (10%) |
| - Unexplained | 9 (9%) |
DISCUSSION
Our findings indicate that about 41% of women ≥ 40 years have UI. Around 30% of all women have moderate to severe UI symptoms, and of those 74% have UI duration of 2 years or more. Most population-based studies of women over the age of 18 show prevalence estimates of UI in the range of 20–30%, and similar estimates in women over 40 years of age [4,18,19]. Although most women with either stress UI alone, or urgency UI alone have milder disease [20][19], women with mixed UI have more severe disease[4,21,22]. Since mixed UI increases with age to become the most prevalent subtype in elderly women, it is evident why most women in our study report moderate to severe UI.
Despite the high prevalence of UI, only 25% of women with UI seek care, 23% receive some type of care, and only 12% receive subspecialty care. These prevalence estimates are possibly even smaller when adjusted for non-responder bias since responders tend to have a higher prevalence of disease. This discrepancy between high prevalence of UI symptoms and low help-seeking behavior is related to: lack of knowledge of available UI treatments; UI considered as a normal part of aging; unavailability of appropriate medical intervention; lack of bidirectional communication between patients and their providers, and others[23]. Conversely, factors associated with care seeking include older age, symptom duration and severity, significant bother and impact on quality of life, and availability of health care [8,9,14].
Our paper establishes the “Iceberg of Disease” in women with UI where the continuum of health care is constructed. This represents the different stages of disease progression from no UI in the population all the way up to women with UI receiving subspecialty care. The iceberg of disease gives information on the distribution of disease at different levels including the population, primary care, and subspecialty care. This offers important information for public health policy makers and health care organizations to allocate appropriate resources to various levels of UI care.
The iceberg (also referred to as pyramid) of disease is not a novel concept in medicine. It has been studied in other disease states such as upper respiratory tract infections (URI) and arthritis[11,24]. Patients with URIs base their decisions about care in the short term secondary to their current symptoms, whereas people with chronic conditions like arthritis develop strategies of care (determined partly by their roles, attitudes, and resources) over months and years, and apply them during flare-ups [11]. We hypothesize that help seeking behavior in UI is more aligned with that of patients with arthritis. Onset and progression of UI in most women is likely to be a slowly progressing condition. Women develop adaptive behavior and strategies that minimize urine loss and its impact on quality of life. Over time, the pelvic floor support mechanisms fail, UI worsens, adaptive behaviors are unable to maintain a positive balance in the quality of life equilibrium, and women start searching for help [19].
By the time patients present to the Urogynecologist or Female Urologist, their UI is at a fairly advanced stage where prevention modalities such as behavioral modification, weight loss, and pelvic floor exercises tend to have little impact [25,26]. The pelvic floor specialist is at the top of the UI health care pyramid. There is generally very little interaction between the pelvic floor specialist and women at high risk of developing UI, or women with early (or mild) manifestations of UI. Like other chronic diseases, UI may at its early stages express reversible symptoms. This tendency to revert back to normal may decrease as the disease state progresses [15,19]. For prevention to work, it is paramount that interventions get implemented before the onset or during the early stages of the disease process.
Our findings indicate that only a small fraction of women with UI receive care by the pelvic floor specialist. These women tend to have more advanced or severe UI where prevention modalities have little impact on reversing the disease status. Therefore, the public health influence of the pelvic floor specialist on the natural history of UI in the population is very limited. Consequently, it behooves the medical community to empower the primary care providers at the frontlines of care delivery with the necessary skill sets, knowledge base, and tools to educate women in healthy behaviors, good habits, and UI prevention modalities. Interventions that increase individuals’ active involvement in their own health care and that encourage greater knowledge of symptoms and outcomes will result in better help-seeking and more efficient service use [10].
Although we used extensive data from the EHR, it was not possible to review progress notes of all patients. We may have missed actual documentation of care delivery to women with UI. For example, a primary care physician could have discussed pelvic floor muscle exercises with a patient but this information was not captured in the data pull. Alternatively, a patient could have presented with UI symptoms, but the clinician did not document, enter the proper UI diagnosis code, or make the appropriate referral. These factors may result in an underestimate of the true prevalence of UI help seeking or delivery. We do not believe that this is a significant source of error since our prevalence estimates of UI help seeking were similar to other population studies where the range varies from 25 to 50% [8,9,14,27,28]. Another weakness is that our response rate was relatively low at 47%. However the response rate is similar to other population-based survey studies [29]. Moreover, since this is part of a longitudinal study, we continue to reach out to the non-responders every 6-months with the BHS to improve our overall response rates. Furthermore, there is evidence from the literature that non-responder bias may not play a significant role in people over the age of 40 in surveys assessing urinary symptoms [30]. Another source of error is the false negative cases. Of the 1,950 women with negative case status by the baseline survey, 104 women had history of EHR diagnosis of UI. We were able to justify 82% (85/104) of the discrepancy. Continued follow-up of our sample over a period of 4 years will help refine case definition criteria and further improve specificity of our survey without affecting its sensitivity.
In summary, it is unquestionable that UI is a highly prevalent condition in women. It appears that most women do not seek or receive care, and those who do so, do not end up with a pelvic floor specialist. Therefore, it is imperative not only to educate women, but also primary care providers about this highly prevalent yet both preventable and treatable condition.
Footnotes
Author Contributions:
VA Minassian: Protocol/project development, Data analysis, Manuscript writing
X Yan: Data analysis, Manuscript writing/editing
MJ Lichtenfeld: Data collection/management, Manuscript writing/editing
H Sun: Data analysis
WF Stewart: Protocol/project development, Manuscript writing/editing
Financial Disclaimer/ Conflict of Interest:
This research was funded by National Institute of Health/ National Institute of Diabetes and Digestive and Kidney Diseases, grant # RO1 DK082551. No author on this paper has a conflict of interest.
References
- 1.Abrams P, Kelleher CJ, Kerr LA, Rogers RG. Overactive bladder significantly affects quality of life. Am J Manag Care. 2000;6:S580–90. [PubMed] [Google Scholar]
- 2.Simeonova Z, Milsom I, Kullendorff AM, Molander U, Bengtsson C. The prevalence of urinary incontinence and its influence on the quality of life in women from an urban Swedish population. Acta Obstet Gynecol Scand. 1999;78:546–51. [PubMed] [Google Scholar]
- 3.Melville JL, Fan MY, Rau H, Nygaard IE, Katon WJ. Major depression and urinary incontinence in women: temporal associations in an epidemiologic sample. Am J Obstet Gynecol. 2009;201:490.e1, 490.e7. doi: 10.1016/j.ajog.2009.05.047. [DOI] [PubMed] [Google Scholar]
- 4.Hannestad YS, Rortveit G, Sandvik H, Hunskaar S Norwegian EPINCONT study. A community-based epidemiological survey of female urinary incontinence: the Norwegian EPINCONT study. Epidemiology of Incontinence in the County of Nord-Trondelag. J Clin Epidemiol. 2000;53:1150–7. doi: 10.1016/s0895-4356(00)00232-8. [DOI] [PubMed] [Google Scholar]
- 5.Thom D. Variation in estimates of urinary incontinence prevalence in the community: effects of differences in definition, population characteristics, and study type. J Am Geriatr Soc. 1998;46:473–80. doi: 10.1111/j.1532-5415.1998.tb02469.x. [DOI] [PubMed] [Google Scholar]
- 6.Milsom I. The prevalence of urinary incontinence. Acta Obstet Gynecol Scand. 2000;79:1056–9. [PubMed] [Google Scholar]
- 7.Minassian VA, Drutz HP, Al-Badr A. Urinary incontinence as a worldwide problem. Int J Gynaecol Obstet. 2003;82:327–38. doi: 10.1016/s0020-7292(03)00220-0. [DOI] [PubMed] [Google Scholar]
- 8.Hannestad YS, Rortveit G, Hunskaar S. Help-seeking and associated factors in female urinary incontinence. The Norwegian EPINCONT Study Epidemiology of Incontinence in the County of Nord-Trondelag Scand. J Prim Health Care. 2002;20:102–7. [PubMed] [Google Scholar]
- 9.Kinchen KS, Burgio K, Diokno AC, Fultz NH, Bump R, Obenchain R. Factors associated with women's decisions to seek treatment for urinary incontinence. J Womens Health (Larchmt) 2003;12:687–98. doi: 10.1089/154099903322404339. [DOI] [PubMed] [Google Scholar]
- 10.Shaw C, Brittain K, Tansey R, Williams K. How people decide to seek health care: a qualitative study. Int J Nurs Stud. 2008;45:1516–24. doi: 10.1016/j.ijnurstu.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 11.Verbrugge LM, Ascione FJ. Exploring the iceberg. Common symptoms and how people care for them. Med Care. 1987;25:539–69. [PubMed] [Google Scholar]
- 12.Lipton RB, Stewart WF, Celentano DD, Reed ML. Undiagnosed migraine headaches. A comparison of symptom-based and reported physician diagnosis. Arch Intern Med. 1992;152:1273–8. doi: 10.1001/archinte.152.6.1273. [DOI] [PubMed] [Google Scholar]
- 13.Hu TW, Wagner TH, Bentkover JD, Leblanc K, Zhou SZ, Hunt T. Costs of urinary incontinence and overactive bladder in the United States: a comparative study. Urology. 2004;63:461–5. doi: 10.1016/j.urology.2003.10.037. [DOI] [PubMed] [Google Scholar]
- 14.O'Donnell M, Lose G, Sykes D, Voss S, Hunskaar S. Help-seeking behaviour and associated factors among women with urinary incontinence in France, Germany, Spain and the United Kingdom. Eur Urol. 2005;47:385, 92. doi: 10.1016/j.eururo.2004.09.014. discussion 392. [DOI] [PubMed] [Google Scholar]
- 15.Stewart WF, Minassian VA, Hirsch AG, Kolodner K, Fitzgerald M, Burgio K, et al. Predictors of variability in urinary incontinence and overactive bladder symptoms. Neurourology & Urodynamics. 2010;29:328–35. doi: 10.1002/nau.20753. [DOI] [PubMed] [Google Scholar]
- 16.Hirsch AG, Minassian VA, Dilley A, Sartorius J, Stewart WF. Parity is not associated with urgency with or without urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2010;21:1095–102. doi: 10.1007/s00192-010-1164-7. [DOI] [PubMed] [Google Scholar]
- 17.Sandvik H, Seim A, Vanvik A, Hunskaar S. A severity index for epidemiological surveys of female urinary incontinence: comparison with 48-hour pad-weighing tests. Neurourol Urodyn. 2000;19:137–45. doi: 10.1002/(sici)1520-6777(2000)19:2<137::aid-nau4>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 18.Melville JL, Katon W, Delaney K, Newton K. Urinary incontinence in US women: a population-based study. Arch Intern Med. 2005;165:537–42. doi: 10.1001/archinte.165.5.537. [DOI] [PubMed] [Google Scholar]
- 19.Minassian VA, Stewart WF, Hirsch AG. Why do stress and urge incontinence co-occur much more often than expected? Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:1429–1440. doi: 10.1007/s00192-008-0647-2. [DOI] [PubMed] [Google Scholar]
- 20.Minassian VA, Stewart WF, Wood CG. Urinary Incontinence in Women: Variation in Prevalence Estimates and Risk Factors. Obstet Gynecol. 2008;2:324–31. doi: 10.1097/01.AOG.0000267220.48987.17. [DOI] [PubMed] [Google Scholar]
- 21.Dooley Y, Lowenstein L, Kenton K, FitzGerald M, Brubaker L. Mixed incontinence is more bothersome than pure incontinence subtypes. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:1359–62. doi: 10.1007/s00192-008-0637-4. [DOI] [PubMed] [Google Scholar]
- 22.Frick AC, Huang AJ, Van den Eeden SK, Knight SK, Creasman JM, Yang J, et al. Mixed urinary incontinence: greater impact on quality of life. J Urol. 2009;182:596–600. doi: 10.1016/j.juro.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shaw C, Tansey R, Jackson C, Hyde C, Allan R. Barriers to help seeking in people with urinary symptoms. Fam Pract. 2001;18:48–52. doi: 10.1093/fampra/18.1.48. [DOI] [PubMed] [Google Scholar]
- 24.Frieden TR. A framework for public health action: the health impact pyramid. Am J Public Health. 2010;100:590–5. doi: 10.2105/AJPH.2009.185652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nygaard IE, Heit M. Stress urinary incontinence. Obstet Gynecol. 2004;104:607–20. doi: 10.1097/01.AOG.0000137874.84862.94. [DOI] [PubMed] [Google Scholar]
- 26.Shamliyan T, Wyman J, Bliss DZ, Kane RL, Wilt TJ. Prevention of urinary and fecal incontinence in adults. Evid Rep Technol Assess (Full Rep) 2007;(161):1–379. [PMC free article] [PubMed] [Google Scholar]
- 27.Irwin DE, Milsom I, Kopp Z, Abrams P EPIC Study Group . Symptom bother and health care-seeking behavior among individuals with overactive bladder. Eur Urol. 2008;53:1029–37. doi: 10.1016/j.eururo.2008.01.027. [DOI] [PubMed] [Google Scholar]
- 28.Hagglund D, Walker-Engstrom ML, Larsson G, Leppert J. Reasons why women with long-term urinary incontinence do not seek professional help: a cross-sectional population-based cohort study. Int Urogynecol J Pelvic Floor Dysfunct. 2003;14:296, 304. doi: 10.1007/s00192-003-1077-9. discussion 304. [DOI] [PubMed] [Google Scholar]
- 29.Eaker S, Bergstrom R, Bergstrom A, Adami HO, Nyren O. Response rate to mailed epidemiologic questionnaires: a population-based randomized trial of variations in design and mailing routines. Am J Epidemiol. 1998;147:74–82. doi: 10.1093/oxfordjournals.aje.a009370. [DOI] [PubMed] [Google Scholar]
- 30.Dallosso HM, Matthews RJ, McGrother CW, Clarke M, Perry SI, Shaw C, et al. An investigation into nonresponse bias in a postal survey on urinary symptoms. BJU Int. 2003;91:631–6. doi: 10.1046/j.1464-410x.2003.04172.x. [DOI] [PubMed] [Google Scholar]