Abstract
Music is an ideal intervention to reduce anxiety and promote relaxation in critically ill patients. This article reviews the research studies on music-listening interventions to manage distressful symptoms in this population, and describes the development and implementation of the Music Assessment Tool (MAT) to assist professionals in ascertaining patients’ music preferences in the challenging, dynamic clinical environment of the intensive care unit (ICU). The MAT is easy to use with these patients who experience profound communication challenges due to fatigue and inability to speak because of endotracheal tube placement. The music therapist and ICU nursing staff are encouraged to work collaboratively to implement music in a personalized manner to ensure the greatest benefit for mechanically ventilated patients.
Every year, one million patients receive mechanical ventilation to treat respiratory insufficiency from a variety of causes (MacIntyre, 1998). Mechanical ventilation involves the application of an artificial airway (endotracheal tube or tracheostomy) and a mechanical ventilator to support a patient’s respiratory system. A majority of the patients admitted to ICUs need mechanical ventilation. While mechanical ventilation is a life-saving modality, patients report numerous distressing symptoms such as feeling fearful, alone, and anxious, and experiencing discomfort (Rotondi et al., 2002).
Because of the placement of the artificial airway, patients are unable to speak. Communication difficulties are profound, causing great distress for patients as they attempt to convey their thoughts and feelings. A primary challenge in working with a mechanically ventilated patient is finding an efficient way to communicate with the patient. Strategies to foster communication may include using a communication board, using head nods, using eye blinks or movements, or squeezing the hand to indicate a “yes/no” response. A patient who is mechanically ventilated may also be receiving sedative and/or analgesic medications that affect alertness, adding to difficulty obtaining sustained responses from a patient in this critical state.
Despite the challenge, nonpharmacologic, adjunctive interventions, such as music, can provide the mechanically ventilated patient with alternative, meaningful stimuli while promoting relaxation. Music listening interventions are useful for ICU patients receiving mechanical ventilatory support for many reasons. First, the intervention is not demanding of a patient and it does not require focused concentration on a stimulus as imagery or biofeedback do. This is important for mechanically ventilated patients since they are critically ill and have low energy states with limited concentration ability. Also, music is a comforting stimulus that patients can use to distract and calm them during this stressful ICU experience.
Previous research has shown that as little as 30 minutes of listening to preferred music can induce relaxation and reduce anxiety in ICU patients receiving mechanical ventilatory support (Chlan, 1995; Chlan, 1998; Wong, Lopez-Nahas, & Molassiotis, 2001). Music is safe for these patients and no untoward side effects have been reported in any participants who listened to music. However, not all of the investigations provided participants with choice or control over the type of music used.
In order for music to be effective, it should be meaningful and familiar to the individual (Janelli, Kanski, & Wu, 2004). Involving patients in music intervention provides them with some control, and this is key because the ICU environment often allows for little or no patient control or involvement in the plan of care. Traditionally, the music used in music listening intervention studies was selected by the researchers and deemed “relaxing” or referred to as “anxiolytic” music (Pelletier, 2004). Further, “patient selected or self-selected” music often was selected from a predetermined collection or set of music genres, ranging from three options (Burns et al., 2002; Heiser, Chiles, Fudge, & Gray, 1997) to up to seven categories or genres (Allen et al., 2001; Cooke, Chaboyer, Schluter, & Hiratos, 2005).
More recently, studies have allowed patients to select the music (Janelli, Kanski, & Wu, 2004/2005; Smolen, Topp, & Singer, 2002). Researchers reported that self-selected music significantly reduces anxiety and promotes tolerance during distressful medical procedures (Bampton & Draper, 1997; Palankis et al., 1994; Wang, Kulkari, Dolev, & Kain, 2002), and familiarity and control over the selection serve as better predictors of physiological response to the music (Allen et al., 2001).
To adequately assess patient music preferences requires knowledge of music, including its various applications and desired outcomes, for which the music therapist is uniquely qualified. When a specific musical genre is identified, it does not mean that the patient will like all groups or artists from that genre. For example, if a patient likes classic rock, the music therapist needs to narrow down the numerous groups or artists within that genre. Does this include Pink Floyd, Jimi Hendrix, The Doors, The Grateful Dead, The Rolling Stones, Credence Clearwater Rival, and Crosby, Steals, Nash and Young? The list could go on and on. The music therapist can “fine tune” the assessment process to discover what music from a specific genre is preferred. Finally, individuals may classify music under different genres; therefore it is important to get specifics about groups and artists.
An assessment of music preference by a professional music therapist is crucial for determining what type of music to offer. However, a strategy for assessing music preference in a simple yet comprehensive format is needed for patients with energy limitations and communication challenges. This article describes a tool to assess music preferences in patients receiving mechanical ventilatory support, a population with a number of unique needs and communication challenges, who can benefit greatly from music listening intervention. The tool is currently being used in a multi-site clinical research study to test the effect of patient-directed music listening interventions on anxiety self-management in critically ill patients receiving mechanical ventilatory support. Examples from interactions with study subjects and a case-based scenario detailing a step-by-step protocol for the application of the music preference assessment tool are presented to guide music therapists in working with mechanically ventilated patients or other patient populations with profound communication challenges.
Development of the Music Assessment Tool for Mechanically Ventilated Patients
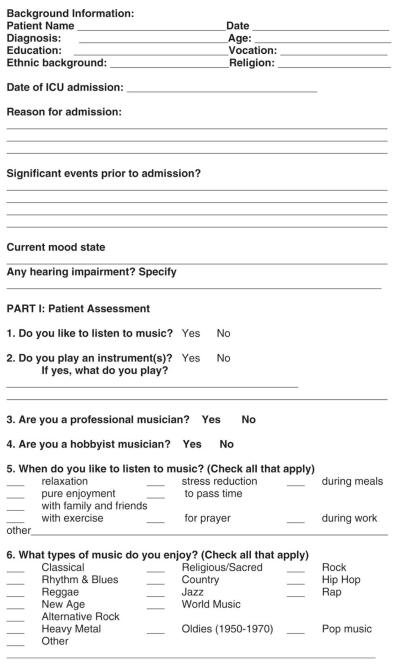
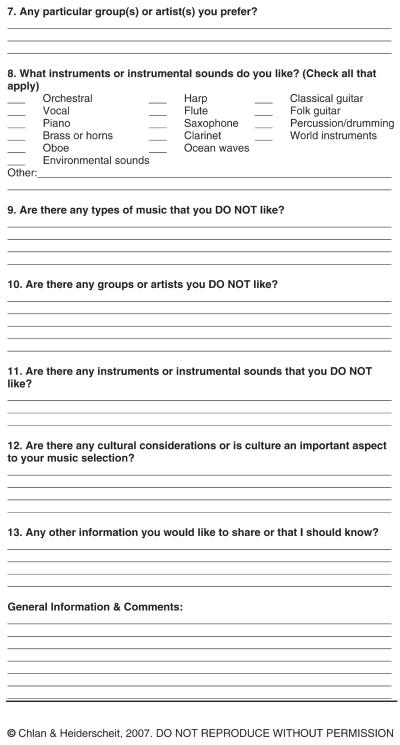
The Music Assessment Tool (MAT) presented here is based on the Music Assessment and Intervention Tool (MAIT), originally developed for nurses to use as a step-by-step guide for music listening intervention for patients in the ICU
The Music Assessment Tool (MAT) presented here is based on the Music Assessment and Intervention Tool (MAIT), originally developed for nurses to use as a step-by-step guide for music listening intervention for patients in the ICU. Details on the MAIT have been published elsewhere (Chlan & Tracy, 1999). While the MAIT is useful to ICU nurses, it does not contain enough detail for a thorough music preference assessment. Therefore, the original MAIT has been modified by a board-certified, PHD trained music therapist in consultation with an experienced ICU nurse researcher and is now referred to as the Music Assessment Tool or MAT. The MAT is currently being used to ensure standard assessment of music preference among subjects in a study of music interventions for mechanically ventilated patients. The MAT is a 3-page tool which consists of yes/no questions, checklists, and open-ended questions.
The MAT includes background information about the patient, such as age, education, profession/vocation, ethnic background, religion, reason for ICU admission, and medical diagnosis, which are all known to influence personal music preference (McCown, Keiser, Mulhearn, & Williamson, 1997; Pelletier, 2004). The information on reason for admission and diagnosis provides insight into what the patient has experienced prior to the music therapist’s initial assessment visit. It is also helpful to know if any significant events occurred prior to the admission. For example, did a traumatic experience precipitate this admission? The frame of mind the patient is in will influence the interactions with the music therapist. If a patient is feeling overwhelmed or depressed, she/he may be less forthcoming in sharing information.
The MAT also asks whether a patient plays an instrument, because if so, the patient may have a favorite artist, pieces of music or recordings. It is important to also assess the patient’s level of musicianship because this can have an impact on the music, artists, and specific recordings the patient prefers. For example, a patient may like to listen to the Pachebel Cannon in D, but there are hundreds of recordings of this piece on various instruments. Does a patient like the traditional version on the harpsichord, the contemporary version on electric keyboard, or a brass quartet version?
The MAT has expanded the question on genres of music to include an option for “other.” Additionally, a question on instruments and sounds has been added to further refine the music preference assessment process.
Three questions ask about types of music and/or instruments the patient does not like which is important when working with patients who are nonverbal due to placement of the artificial airway. For example, a patient may share a preference for easy listening music and may name some preferred artists. But when you ask about music or artists the patient does not like, he or she may tell you, “I don’t like Rod Stewart.” This is important information in order to avoid unknowingly including music the patient does not like, which can have a detrimental effect.
Guidelines for Administration of the MAT with Mechanically Ventilated Patients
When patients enter the hospital, they are treated and cared for by a team of experts. Working together as a team also applies to the use of music as an intervention in the ICU.
When the music therapist receives a referral to work with a patient in the ICU, it is important to check in with the nurse prior to meeting the patient to determine if it is an appropriate time and gather any important information the nurse may be able to share about the patient. For example, is the patient able to communicate verbally, write messages, or respond via eye blinks or head nods? Is the patient’s hearing impaired? Is there information the patient has already shared that would be helpful to the music therapist? Asking the nurses avoids asking the patient to convey information already communicated. A patient recently enrolled in our study was hearing impaired and heard best in his left ear. The patient’s nurse shared this information with the music therapist, which was vital for communicating with the subject. The nurse may also have significant knowledge of the patient’s likes, dislikes, habits, or mood state.
The MAT is designed to facilitate gathering comprehensive information concerning the patient’s music preferences. Focusing on preferred music can facilitate the patient experiencing significantly less anxiety (Burns et al., 2002; Wang, Kulkari, Dolev, & Kain, 2002), decreased blood pressure and heart rate (Allen & Blasovich, 1994), and can dramatically diminish the perception of stress (Allen et al., 2001).
For gathering information from patients in the ICU who may have limited energy for communicating, it is imperative to focus on questions that can be answered accurately only by the patient. While the MAT contains many questions, not all areas need to be addressed at once; the music therapist needs to determine what is essential information and what can be obtained at a later time or from others. General information can be obtained from the research staff, family members, or nursing staff. Family members may be able to provide information on music preferences. If they are unsure about preferences, the music therapist can ask a family member to inventory the patient’s home music collection and write down names of groups or artists in the collection. Also, family members may have brought recordings to the hospital and these can be helpful in generating insight into the patient’s preferences.
Using the MAT in the ICU
It is important for the music therapist to keep in mind some aspects of the ICU setting that make it unique. When patients are in the ICU, they experience a lack of choice and little, if any, control or involvement with their care. Often they have no opportunities to express their desires or make choices. In the complex, high-tech environment of the ICU, patients can feel depersonalized. Further, ICU patients can have long lengths of stay, up to 28 days or more, which can feel confining. They can watch and listen to television but to do so for many hours a day, day in and day out, becomes monotonous. For mechanically ventilated patients with long stays, the music therapist will need to provide more varied music. It is important for the music therapist to check in with the patient regularly to determine if there are other artists, groups, or genres of music that the patient might like. Patients’ music preferences can change based on their mood state and how they feel physically.
Application of the MAT: A Case Scenario
Scott was a 57 year old Caucasian male admitted to the ICU for mechanical ventilatory support due to shortness of breath and pulmonary edema. IRB approval and patient consent were obtained for use of his data. He had a lengthy medical history, including hypertension, anemia, and coronary artery disease. He was a paraplegic and prior to his hospitalization was residing in a group home. Prior to the initial music preference assessment, he had been hospitalized for two days. He communicated that he had been hospitalized many times previously due to complications as a result of being a paraplegic.
When the music therapist first met with Scott, he communicated that he enjoyed listening to a wide array of music, and he mentioned both classical music and classic rock. He specified the music of Mozart, The Beatles, and The Who, and he said he preferred orchestral music, violins, and classical guitar. He also liked to listen to National Public Radio and a local Christian music station.
The MAT assists the music therapist in determining when a client prefers listening to music and the purpose(s) for which the client uses music. Reviewing these with a patient is helpful since the client may not immediately recall all of the moments of listening to music or a patient may not be consciously aware of the fact that one listens to music at various times. The questions on the MAT can make patients aware of specific times for music listening. For Scott, the question prompted him to share that he was encountering difficulty sleeping.
Following this initial assessment, the music therapist created five disks for Scott: three disks of the music of Mozart, including primarily adagio and largo movements; a disk of early Beatles music; music from The Who; and a compilation of contemporary or new age music that was between 40–60 beats per minute to help him achieve deeper sleep states. This music was designed to take Scott’s thoughts away from the environment and from anxious or stressful feelings onto the music and to provide the body with slow rhythms for entrainment to occur, resulting in relaxation. As Scott listened to the music, his body rhythms became synchronized with the rhythm of the music, achieving a more restful state and promoting sleep.
When the music was presented to Scott, he was appreciative that someone would take the time to bring him the music he preferred. The next morning he reported that he listened to the music the previous day and entered into a deep sleep, with several consecutive hours of sleep for the first time since being admitted to the ICU; he felt more relaxed when he awoke from this sleep.
When the music therapist came to see Scott the next day, he thanked her profusely for the music and commented that he would like to purchase music like this to use when he left the hospital. During each encounter with Scott, the music therapist assessed preferences, using the questions 6 through 10 on the MAT. Scott often recalled other musicians and groups he liked as he listened to music. While he initially identified some genres that he did not like, he later identified a small number of artists in some of these genres that he did enjoy. This shows how in a dynamic, on-going assessment process, additional information is gained with each interaction. As his preferences were further assessed, Scott mentioned various artists including Jim Morrison, Bob Dylan, Rod Stewart, The Doors, music by Johann Sebastian Bach and music of the 1960’s in general. Additional disks were created and provided to Scott incorporating these various artists and composers.
Scott continued to report improved sleep, even sleeping for 5 consecutive hours one night, an achievement almost unheard of in the ICU. He also noted that when he listened to the music, he was reminded of people and moments in his life. During visits with the music therapist, he would become tearful when discussing these feelings. It was evident that the music was facilitating reminiscence and the expression of emotions long withheld. When he was able to process through the emotions, he said that this was motivating him to reconnect with important people in his life.
In the daily assessment process with Scott, the MAT served as a springboard for helping him recall the times in his life when he incorporated music and also prompted him to share his difficulty in sleeping. Previously, he had not considered using music to address this problem.
Reviewing the various genres of music helped to prompt Scott’s thoughts about his likes and dislikes in music and reviewing instruments contained in question 8; questions 9, 10 and 11 allowed for additional follow up. The MAT also explores an individual’s background and whether this is an important consideration to their music preferences (question 12). Question 13 of the MAT concludes with a broad question to allow patients to discuss anything they feel is important for the therapist to know. This may be related to music preferences or it may inform the music therapist about difficulties or discomforts being experienced that might be amenable to music intervention. The information is important when the music therapist is customizing CDs for patient-directed music listening.
Directions for Practice and Research
It is important to work within the copyright laws when providing customized CDs. The music therapist should ensure that the music is either downloaded through a reputable site with downloads purchased or purchase original CDs. For our research study, music is purchased from a reputable internet download service (www.MyMusicInc.com) and CDs are commercially purchased and maintained in a study music library by the music therapist, all adhering to copyright laws. It is recommended that when providing music to patients for a music listening intervention, the music therapist should be knowledgeable of the these copyright laws (www.copyright.gov). While patients may ask to keep CDs, the music therapist should not engage in distributing copied or downloaded music because this violates copyright laws.
The MAT is presented in Table 1 as previously shown. Other areas or questions may need to be added to the instrument, but this will only become clear through application of the tool in clinical practice. While the MAT is designed for a music therapist to efficiently obtain information from ICU patients receiving mechanical ventilatory support, we believe the tool has applicability to other clinical settings. Any music therapist working with patients who have communication challenges or energy limitations, such as those in oncology, rehabilitation or palliative care settings, may find the MAT useful for music preference assessments. Likewise, music therapists and multi-disciplinary colleagues could use the MAT when designing music listening interventions to ameliorate symptoms such as pain and distress in postoperative patients. The MAT could also be used to guide the establishment of clinical practice guidelines based on the most current evidence available.
Table 1.
MUSIC ASSESSMENT TOOL (MAT)
|
|
Using a tool such as the MAT provides researchers with a structure or template to afford patients the opportunity to communicate their choices and then to provide them the music that is preferred, rather than using researcher-selected or a limited, predetermined collection of music
A multi-disciplinary team is needed to care for complex patients such as those who are critically ill and receiving mechanical ventilatory support. Using a tool such as the MAT provides researchers with a structure or template to afford patients the opportunity to communicate their choices and then to provide them the music that is preferred, rather than using researcher-selected or a limited, predetermined collection of music. The MAT can ensure that all patients are assessed in a standardized manner. The MAT serves as a template and organizer for the music therapist, particularly if a patient is in the ICU for a lengthy period of time. Furthermore, the assessment process guided by the MAT accommodates information from members of the healthcare team as well as family members. The efficacy of using the MAT to implement music intervention in clinical settings warrants further exploration.
Acknowledgments
This project was supported by Grant Number R01NR009295 from the National Institute of Nursing Research. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Nursing Research or the National Institutes of Health.
Footnotes
This article is based on a current multi-site trail testing music for anxiety self-management in critically ill patients receiving mechanical ventilator support.
Contributor Information
LINDA CHLAN, School of Nursing at the University of Minnesota, Minneapolis..
ANNIE HEIDERSCHEIT, Center for Spirituality and Healing at the University of Minnesota..
REFERENCES
- Allen K, Blasovich J. Effects of music on cardiovascular reactivity among surgeons. Journal of the American Medical Association. 1994;272:882–884. [PubMed] [Google Scholar]
- Allen K, Golden L, Izzo J, Ching M, Forrest A, Niles C, et al. Normalization of hypertension responses during ambulatory surgical stress by perioperative music. Psychosomatic Medicine. 2001;63:487–492. doi: 10.1097/00006842-200105000-00019. [DOI] [PubMed] [Google Scholar]
- Bamptom P, Draper B. Effect of relaxation music on patient tolerance of gastrointestinal endoscopic procedures. Journal of Clinical Gastroenterology. 1997;25(1):343–345. doi: 10.1097/00004836-199707000-00010. [DOI] [PubMed] [Google Scholar]
- Burns J, Labbe E, Williams K, McCall J. Perceived and physiological indicators of relaxation: As different as Mozart and Alice in chains. Applied Psychophysiology and Biofeedback. 1999;24(3):197–202. doi: 10.1023/a:1023488614364. [DOI] [PubMed] [Google Scholar]
- Burns J, Labbe’ E, Arke B, Capless K, Cooksey B, Steadman A, et al. The effects of different types of music on perceived and physiological measures of stress. Journal of Music Therapy. 2002;35(2):101–116. doi: 10.1093/jmt/39.2.101. [DOI] [PubMed] [Google Scholar]
- Chlan L. Psychophysiologic responses of mechanically ventilated patients to music: A pilot study. American Journal of Critical Care. 1995;4(3):233–238. [PubMed] [Google Scholar]
- Chlan L. Effectiveness of a music therapy intervention on relaxation and anxiety for patients receiving ventilatory assistance. Heart and Lung: The Journal of Acute and Critical Care. 1998;27(3):169–176. doi: 10.1016/s0147-9563(98)90004-8. [DOI] [PubMed] [Google Scholar]
- Chlan L, Tracy MF. Music therapy in critical care: Indications and guidelines for intervention. Critical Care Nurse. 1999;19(3):35–41. [PubMed] [Google Scholar]
- Cooke M, Chaboyer W, Schluter P, Hiratos M. The effect of music on preoperative anxiety in day surgery. Journal of Advanced Nursing. 2005;52(1):1133–40. doi: 10.1111/j.1365-2648.2005.03563.x. [DOI] [PubMed] [Google Scholar]
- Copyright Law of the United States and Related Laws Contained in Title 17 of the United States Code. [retrieved March 24, 2008]. http://www.copyright.gov.title17/
- Heiser R, Chiles K, Fudge M, Gray S. The use of music during immediate postoperative period. AORN Journal. 1997;65:777–85. doi: 10.1016/s0001-2092(06)62999-2. [DOI] [PubMed] [Google Scholar]
- Janelli L, Kanski G, Wu Y. The influence of individualized music on patients in physical restraints: A pilot study. Journal of New York State Nurses Association. 2004/2005;35(2):22–27. [PubMed] [Google Scholar]
- MacIntyre N. Mechanical ventilation: The next 50 years. Respiratory Care. 1998;43(3):46–61. [Google Scholar]
- McCown W, Keiser R, Mulhearn S, Williamson D. The role of personality and gender on preference for exaggerated bass in music. Personality and Individual Differences. 1997;4:543–47. [Google Scholar]
- Palankis K, DeNobile J, Sweeney W, Blakenship C. Effect of music therapy on state anxiety in patients undergoing flexible sigmoidoscopy. Diseases of the Colon and Rectum. 1994;37:478–481. doi: 10.1007/BF02076195. [DOI] [PubMed] [Google Scholar]
- Pelletier CL. The effect of music on decreasing arousal due to stress: A meta-analysis. Journal of Music Therapy. 2004;41(3):192–214. doi: 10.1093/jmt/41.3.192. [DOI] [PubMed] [Google Scholar]
- Rotondi A, Chelluri L, Sirio C, Mendelsohn A, Schulz R, Belle S, et al. Patients’ recollections of stressful experiences while receiving prolonged mechanical ventilation in an intensive care unit. Critical Care Medicine. 2002;30(4):746–752. doi: 10.1097/00003246-200204000-00004. [DOI] [PubMed] [Google Scholar]
- Smolen D, Topp R, Singer L. The effect of self-selected music during colonoscopy on anxiety, heart rate, and blood pressure. Applied Nursing Research. 2002;15(3):126–36. doi: 10.1053/apnr.2002.34140. [DOI] [PubMed] [Google Scholar]
- Wang S, Kulkarni L, Dolev J, Kain Z. Music and preoperative anxiety: A randomized, controlled study. Anesthesia and Analgesia. 2002;94:1489–94. doi: 10.1097/00000539-200206000-00021. [DOI] [PubMed] [Google Scholar]
- Wong H, Lopez-Nahas V, Molassiotis A. Effects of music therapy on anxiety in ventilator-dependent patients. Heart and Lung: The Journal of Acute and Critical Care. 2001;30(5):376–387. doi: 10.1067/mhl.2001.118302. [DOI] [PubMed] [Google Scholar]


