Abstract
Primary splenic cyst is a relatively rare entity; they comprise only about 10% of benign non-parasitic cysts. Most of these are asymptomatic and are observed incidentally during abdominal ultrasonography. The number of diagnosed splenic cyst cases seems to have risen because of the increasing use of abdominal imaging techniques. However, definite diagnosis is possible only after splenectomy when epithelial lining is confirmed histologically. We report a case of a 14-year-old child who presented with fullness of abdomen and pain in the left hypochondrium since last few months. First impression made was in favor of a splenic lymphangioma of size 8 × 8 cm which was based on a Computerized tomography scan and the sonographic findings. Splenectomy was performed and was sent for histopathological examination which in combination with immunohistochemistry revealed findings suggestive of primary epithelial cyst. A large cystic mass with a relatively thin wall localized in the spleen is likely to be a primary or secondary cyst. The diagnosis of false cyst should be favored if there is a clear history of trauma, if the patient is older than fourth decade, if there is a hematoma elsewhere in spleen, or if cyst wall is calcified. This rare entity should be considered in the differential diagnosis in a patient presenting with left hypochondrial pain.
Keywords: Epithelial cyst, primary cyst, spleen
INTRODUCTION
Splenic cysts are unusual in everyday surgical practice. Prenatal findings of cystic lesions of spleen are rare, but possible usually during the third trimester. Conversely, splenic cysts are usually seen in late childhood. Splenic cysts found prenatally tend to disappear later in pregnancy or after birth.[1] The first case of splenic cyst was reported by Berthelot in the year 1790.[2] Primary splenic cyst comprises only about 10% of benign non-parasitic cysts. These cysts are encountered more commonly in children and young adults.[3] Most of these are asymptomatic and are incidental findings during abdominal ultrasonography (USG). The number of diagnosed splenic cysts seems to have risen because of the increased use of abdominal imaging techniques.[4] Here, we present a case of splenic cyst which was diagnosed before surgery as lymphangioma on computerized tomography (CT) scan and USG and we also review the literature herein. This case is presented due to the diagnostic dilemma it can create.
CASE REPORT
A 14-year-old boy was admitted with complaint of progressively enlarging mass and pain in left hypochondrium since last few months. There was no history of abdominal trauma and no symptoms like vomiting and constipation pertaining to gastrointestinal tract. History was negative for infection by malaria or any hematological disorder. Physical examination showed good general condition. In the area of left hypochondrium, a smooth firm, non-tender mass was palpable. The liver was not enlarged. The laboratory investigations were within normal limits. On USG, a well-defined intrasplenic hypoechoic lesion was seen measuring 8 cm × 6 cm with internal septations; CT scan also revealed similar findings. Keeping in view the above findings, a clinical diagnosis of lymphangioma was made. Therapeutic procedure in the form of splenectomy was performed due to the large size of the tumor and tissue was sent for histopathologic examination.
We received a specimen of spleen measuring 15 cm × 10 cm × 7 cm. On serial sectioning, a large cyst of size 8 cm × 8 cm was identified at one end [Figure 1]. Wall of the cyst showed trabeculations and the cyst contained an opaque dark-colored fluid. Rest of spleen showed congestion. Microsections examined revealed a cyst wall lined by pseudo-stratified epithelium. Focally, the lining epithelium was flattened, and the cyst wall was composed of fibrocollagenous tissue and congested blood vessels. Rest of the splenic tissue showed congestion [Figure 2]. Immunohistochemical panel for epithelial and vascular markers were performed. The lining cells were positive for pancytokeratin and were negative for CD-34 [Figures 3a and b]. The cyst was diagnosed as epithelial cyst rather than lymphangioma.
Figure 1.

Specimen of spleen with a cyst measuring 8 cm × 8 cm, with cyst wall showing trabeculations
Figure 2.
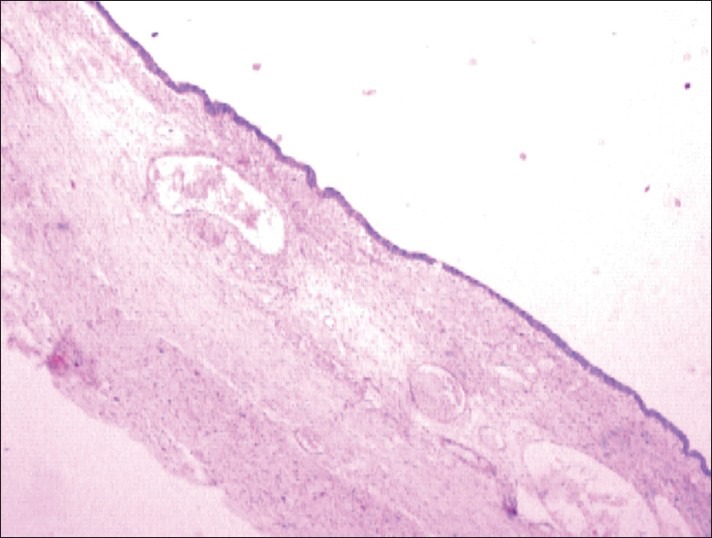
Cyst wall lined by flattened epithelium with fibrocollagenous tissue and congested blood vessels (H and E; ×100)
Figure 3.
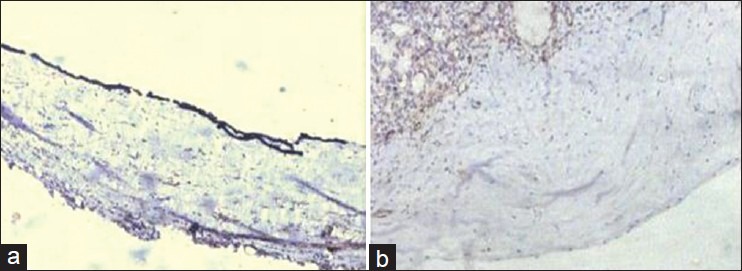
(a) The cells lining the cyst showed positivity for cytokeratin (b) and were negative for CD 34
DISCUSSION
Cysts of the spleen are rare and usually found incidentally. They have been classified in various ways based on their lining, etiology, pathogenesis, etc. Splenic cysts have been classified by Martin as follows: Type 1 cysts are primary (true) cysts with a cellular lining, parasitic or non-parasitic in nature. Non-parasitic type 1 cysts are either congenital or neoplastic. Type 2 cysts are secondary (false) cysts without cellular lining.[5] According to etiology, the splenic cysts can be of two types: Parasitic or non-parasitic. Based on the presence of surface epithelium, the non-parasitic cyst are divided as true or false (pseudocyst).[6] A new classification based on the true pathogenesis of cyst divides non-parasitic splenic cysts as congenital, neoplastic, traumatic, and degenerative.[7]
Parasitic cysts develop only in endemic areas and are usually caused by Taenia echinococcus. Most true primary cysts are epithelial in origin and have embryonic inclusion of epithelial cells from adjacent structures.[8] False or secondary cysts, which usually constitute 75% of all non-parasitic cysts, are mostly of traumatic origin, and may also be of infectious and degenerative origin. Primary cysts are also known as epithelial cysts in British literature and epidermoid cysts in American literature.[2]
A review study has observed the prevalence of non-parasitic splenic cysts to be congenital in 82%, traumatic in 15%, and of hamartomatous origin in 3% cases. Male to female ratio was one. Median age of presentation was 11 years. Abdominal pain was the main complaint in 46% cases. Forty seven of the cysts were diagnosed incidentally.[9]
Histologically, most of these primary non-parasitic cysts are lined by stratified squamous epithelium. However, the lining may be flattened or completely lost in some areas and sometimes the cyst may be lined by transitional lining.[10] Secondary (false) cysts have an inner lining of connective tissue and are usually secondary to blunt trauma or hemorrhage in the splenic parenchyma, but they may also be of infectious or degenerative origin.[11]
Either type of cysts usually does not produce any specific symptoms, until they reach a significant size. Large cysts may produce pain and heaviness in left hypochondriac region, due to distension of capsule or space occupying mechanisms within the abdominal cavity; or they may present as a palpable mass. Symptoms secondary to pressure on surrounding organs such as nausea, vomiting, flatulence, pleuritic pain, and dyspnea may appear. Splenic cysts may also present with complications such as infection, rupture, and hemorrhage.[4,10,11] Indeed, in our case, the symptomatology included a progressively enlarging mass and pain in left hypochondrium.
A comprehensive differential diagnoses for a cystic lesion in spleen include parasitic echinococcal disease, congenital cyst, pseudo-cyst from splenic trauma, infarction, infection, pyogenic splenic abscess, pancreatic pseudo-cyst, metastatic disease, and cystic neoplasms like hemangioma/lymphangioma. False cysts typically have a smooth, fibrous non-cellular lining, which can lead to hemorrhage and may calcify.[3]
Clinical diagnosis requires an early suspicion and recognition of the differential diagnosis of left hypochondriac pain. USG is a good non-invasive tool for screening and confirming the cystic nature of the mass. CT and magnetic resonance imaging may be superior to USG as they provide additional information regarding septation and trabeculation within the cysts and calcification of cyst wall. However, although CT and USG are preferred modalities for diagnosing the splenic lesions, it is often difficult to distinguish between false cyst and true cyst using these tests. Other techniques such as 99m Technetium sulfur colloid scintigraphy and 67-Gallium citrate are being employed. Recent reports demonstrate preoperative elevations of serum carbohydrate antigen 19-9(CA 19-9) that decrease after splenectomy.[12] In this case, USG and CT had preoperatively suggested the diagnosis of lymphangioma of spleen.
There are different approaches to the surgical treatment depending on the patient's age, size, location, and nature of the cyst. The classic approach to splenic cyst has been an open laparotomy, complete splenectomy. Recently, there are trends toward more conservative surgery, because of the development of overwhelming life-threatening septicemia, especially in children who underwent splenectomy. Indeed, spleen plays an important role in hematopoiesis, immune function, and protection against infection and malignancy. Today, the optimal treatment options are partial splenectomy, total cystectomy, marsupialization, or cyst decapsulation, which are accessed either by an open laparotomy or laparoscopy.[4]
Although the literature offers the possibility of providing conservative or semi-conservative treatment, in our case, considering the large size of the cyst and its location (intra-splenic), conservative procedure was difficult to perform. So, an open, total splenectomy was performed.
CONCLUSION
In conclusion, the epithelial splenic cysts are rare. Clinical symptoms may not be obvious unless cysts are large or associated with complications. This rare entity must be considered in the differential diagnoses of left hypochondriac pain. Whenever possible, early employment of CT and USG for detection of splenic lesions is justified. Definitive diagnosis requires a histological confirmation.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Cuillier F, Lemaire P, Bideault J, Bertha A. Congenital splenic cysts: Report of four cases. Fetus. 2007;8:13–19. [Google Scholar]
- 2.Desai MB, Kamdar MS, Bapat RR, Modhe JM, Medhekar ST, Kokal KC, et al. Splenic cysts: Report of 2 cases and review of the literature. J Postgrad Med. 1981;27:251–2. [PubMed] [Google Scholar]
- 3.Belekar D, Desai A, Dewoolkar A, Bhutala U. Splenic epithelial cyst: A rare entity. Int J Surg. 2010;22:1–18. [Google Scholar]
- 4.Macheras A, Misiakos E, Liakakos T, Mpistarakis D, Fotiadis C, Karatzas G. Non-parasitic splenic cysts: A report of three cases. World J Gastroenterol. 2005;11:6884–7. doi: 10.3748/wjg.v11.i43.6884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martin JW. Congenital splenic cysts. Am J Surg. 1958;96:302–8. doi: 10.1016/0002-9610(58)90916-4. [DOI] [PubMed] [Google Scholar]
- 6.Kalinova K. Giant pseudocyst of the spleen: A case report and review of the literature. J Indian Assoc Pediatr Surg. 2005;10:176–8. [Google Scholar]
- 7.Morgenstern L. Nonparasitic splenic cysts: Pathogenesis, classification, and treatment. J Am Coll Surg. 2002;194:306–14. doi: 10.1016/s1072-7515(01)01178-4. [DOI] [PubMed] [Google Scholar]
- 8.Lippitt WH, Akhavan T, Caplan GE. Epidermoid cyst of the spleen with rupture and inflammation. Arch Surg. 1967;95:74–8. doi: 10.1001/archsurg.1967.01330130076015. [DOI] [PubMed] [Google Scholar]
- 9.Sinha CK, Agrawal M. Nonparasitic splenic cysts in children: Current status. Surgeon. 2011;9:49–53. doi: 10.1016/j.surge.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 10.Reddi VR, Reddy MK, Srinivas B, Sekhar CC, Ramesh O. Mesothelial splenic cyst: A case report. Ann Acad Med Singapore. 1998;27:880–2. [PubMed] [Google Scholar]
- 11.Trompetas V, Panagopoulos E, Priovolou-Papaevangelou M, Ramantanis G. Giant benign true cyst of the spleen with high serum level of CA 19-9. Eur J Gastroenterol Hepatol. 2002;14:85–8. doi: 10.1097/00042737-200201000-00015. [DOI] [PubMed] [Google Scholar]
- 12.Chen SC, Gao HW, Liu MY, Hsieh CB. Infected splenic epidermoid cyst. J Med Sci. 2004;24:43–6. [Google Scholar]


