Abstract
Background:
There are concerns on the efficacy and safety of endoscopic papillary balloon dilatation (EPBD) as an alternative to endoscopic sphincterotomy (EST) in the treatment of choledocholithiasis. We compared the efficacy and safety of EPBD and EST for removing large common bile duct (CBD) stones.
Materials and Methods:
One hundred sixty patients with CBD stones of 10-20 mm were randomized to undergo EPBD or EST. A 15-mm dilatation balloon was used for EPBD. Cotton's criteria were used to determine the incidence of post-EPBD or post-EST complications. CBD stone removal and complications were compared between the two methods.
Results:
CBD stones were completely removed in 97.5% of the EPBD and 96.2% of the EST group (P = 0.5). The incidence of postoperative pancreatitis (11.2% vs 8.7%) and bleeding (1.2% vs 1.2%) were similar between the EPBD and EST groups (P > 0.05). Perforation did not occur in any patient.
Conclusions:
EPBD with 15-mm dilator balloon appears to be equally safe and effective compared with EST for removal of large CBD stones. So because of low complication and high success rate we recommend EPBD as the preferred method for removal of large (10-20 mm) CBD stones.
Keywords: Choledocholithiasis, endoscopic papillary balloon dilatation, endoscopic sphincterotomy, pancreatitis
INTRODUCTION
With the introduction of endoscopic retrograde cholangiopancreatography (ERCP) in the late 1970s, endoscopic treatment has become a preferred method over surgery for the management of common bile duct (CBD) stones, and endoscopic sphincterotomy (EST) is the most frequently used technique with success rate of over 90%.[1] However, besides bleeding, perforation, infection, and dysfunction of the papillary sphincter, pancreatitis is the most frequent and most important complication of EST, which occurs in up to 5% of the patients.[2] Because of concerns regarding both short-term and long-term complications related to EST, another less invasive technique, endoscopic papillary balloon dilation (EPBD), has been investigated.[3] With EPBD, the extraction of CBD stones becomes possible while preserving the biliary sphincter. There are reports on some advantages of EPBD over EST regarding stone removal and complications.[3,4] Because the bile duct orifice is extended by balloon inflation and is anatomically preserved, complications such as bleeding and perforation are expected to occur less frequently than in EST. Evidence also have shown that with EPBD, the function of sphincter of Oddi can be preserved more successfully than with EST.[5]
Despite several advantages reported for EPBD over EST, many endoscopists still hesitate to consider it as a standard procedure for treatment, and its safety has been yet under question. There are concerns on the higher frequency of postoperative pancreatitis reported by EPBD. The incidence of pancreatitis associated with EPBD is reported in separated studies from 4.8% to 11%.[6,7,8,9] This is while the reported incidence for EST ranges from 1.9% to 5.4%.[2,10] Some prospective randomized trial also reported the higher incidence of postoperative pancreatitis with EPBD compared with EST.[11,12,13] The results of the other studies have been conflicting and there are limited data from prospective randomized trials in this regard.[14] The aim of the present study was to investigate and compare the efficacy and safety of EPBD and EST in the treatment of large CBD stones.
MATERIALS AND METHODS
Patients and settings
This randomized comparative trial was conducted at the Department of Gastroenterology of Alzahra University Hospital from 2008 to 2011.
We performed diagnostic ERCP for the patients in whom CBD stones were diagnosed by ultrasonography, computed tomography (CT), magnetic resonance cholangiopancreatography (MRCP), or endoscopic ultrasonography (EUS) previously. The study protocol was approved by the Ethics committee of Isfahan University of Medical Sciences, and informed consent was obtained from all the patients.
Intervention
All the patients received a standard method of sedation by an anesthesiologist with a combination of propofol, midazolam, and fentanyl. Intravenous ceftriaxone 1 g/day was administered for 3 days after the procedure to prevent postoperative biliary infection.
ERCP was performed with a sideview endoscope (TJF-145, Olympus Co, Japan). After guide wire-assisted selective cannulation of the CBD, using a cholangiography catheter (ERCP cannula; Boston Scientific Co, USA), confirmation of the correct site of the catheter in CBD was performed by fluoroscopic imaging.
After contrast injection, the patients who had 10-20 mm size CBD stone were included in our study and then using a random table of numbers generated by Random Allocation Software, patients were randomized to receive either EPBD or EST. Patients who needed precut sphincterotomy or needle knife sphincterotomy for CBD cannulation were excluded. Also, patients with active acute pancreatitis, intrahepatic stones, benign or malignant CBD strictures, and prior sphincterotomy were excluded from the trial.
For EPBD, a triple-sized dilator balloon (CRE-wire-guided esophageal/pyloric balloon dilation catheter; Boston Scientifics, Ireland) was inserted into the bile duct, for dilating the papilla. The balloon was inflated in 3 steps: 12, 13.5, and then 15 mm with saline solution, each for 1 min. Stones were removed with a multiple-sized extractor balloon (fusion; Wilson-Cock Co, USA), which were 12-20 mm in size (according to CBD stone size and CBD diameter). For EST, a papillary incision was made using a pull-type, 25 mm cutting wire sphincterotome (fusion, Wilson-Cock Co, USA), then CBD stones were removed with the extractor balloon.
Assessments
After performing the procedure and full recovery from anesthesia, the patients were transferred to the ward and were observed for any complications, including bleeding and pancreatitis. The diagnosis of pancreatitis was based on the criteria of Cotton et al.;[15] with abdominal pain and the serum level of amylase three or more times the normal level, which have been used in several studies.[2,7,16,17,18] Bleeding was defined as early bleeding, during the procedure or within 5 min after the procedure, and was controlled by local injection and APC or hemoclip, if needed and delayed bleeding within 48 h after the procedure, suspected by unexplained tachycardia, orthostatic change in blood pressure, melena, or hematemesis and confirmed by endoscopy. Perforation was evaluated with initiation of abdominal symptoms and imaging findings. The physician who monitored the patients for complications and collected the data (RR) was blinded to the type of the procedure used for each patient.
Statistical analyses
After collecting the data about efficacy and complications in all patients, data were analyzed using the SPSS software for windows version 16.0. Binary variables were compared using the Chi-square test and differences were considered significant when P was <0.05.
RESULTS
During the study period, 79 female and 81 male patients with mean age of 56.4 ± 15.3 years were included; 42 male and 38 female patients in the EST group and 39 male and 41 female patients in the EPBD group. The two groups were similar with respect to gender (P = 0.376) and age (P = 0.508).
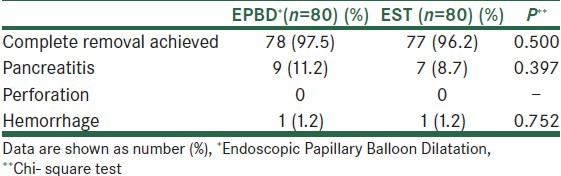
The treatment outcome and related complications are presented in table 1. The CBD stones were removed successfully in 97.5% (78/80) and 96.2% (77/80) of the patients who received EPBD and EST, respectively (P = 0.500). Pancreatitis occurred in 11.2% of the EPBD group compared with 8.7% in the EST group (P = 0.397). Severe acute pancreatitis occurred in 2 patients in the EPBD group and 1 patient in the EST group (P = 0.14). Severity of acute pancreatitis was determined using the criteria of Cotton et al.[15] All patients who developed acute pancreatitis were managed successfully with conservative measures, including intravenous hydration, avoidance of oral intake, and analgesics. The mean time for hospital stay was (3.2 ± 1.8 days). There was no major complication, organ failure, or mortality from acute pancreatitis in any patient. Perforation did not occur in any patients and only 1 patient in each group experienced major bleeding needing transfusion and endoscopic therapy. There were 6 (7.5%) minor bleedings during or immediately after the procedure in EST group compared with 8 (10%) minor bleedings in EPBD group (P = 0.28). All minor bleedings stopped spontaneously except one in the EPBD group in which the endoscopist decided to treat it with injection of diluted epinephrine into the bleeding site. In patients whose stones could not been extracted with balloon, we used lithotripter basket, which was successful in 2 patients in each group. Only 1 patient in the EST group was referred to surgeon for stone retrieval.
Table 1.
Comparison of outcome and complications between the two groups
DISCUSSION
Since the introduction of EPBD as an alternative method for EST, several studies reported that it has some advantageous effects over the EST with regard to outcomes and short- and long-term complications.[3,4,5] EPBD is relatively easier to perform than EST, with less possibility of shorter complications of bleeding and perforation. It also allows functional preservation of the papillary sphincter, one of the major advantages of EPBD over EST, which in turn may result in a decrease in long-term complications.[3] However, after more data became available, several concerns raised with EPBD, such as the difficulty of removing larger stones because of the smaller biliary opening, the more frequent need for endoscopic mechanical lithotripsy (EML), and the higher incidence of postoperative pancreatitis.[3,4,14] In the present study, we achieved the rate of successful removal of large bile duct stones as 97.5% versus 96.2% in the EPBD and EST groups, respectively, that are in agreement with previously reported data indicating a success rate of 79%-100% with EPBD and 85%-100% with EST method, and shows that EPBD, as well as EST, appears to be a useful therapeutic procedure for removal of 10-20 mm CBD stones.[19] In contrast to some previous reports, we did not find an increase in the rate of complications with EPBD compared with EST. In our study, pancreatitis occurred in 11.2% and 8.7% of those who underwent EPBD and EST, respectively. The most recent meta-analysis by Liu et al. presented data of 10 randomized comparative trials of EPBD versus EST and found that although the overall complications are similar between EPBD and EST, there is a higher incidence of postoperative pancreatitis with EPBD (9.4% vs 3.3%), but less hemorrhage (0.1% vs 4.2%) compared with EST. The study also showed that, with EPBD, more EML is needed.[19] The small differences of our study with the previous ones may have technical reasons, such as avoidance of needle knife sphincterotomy and dye injection into the pancreatic duct and also using cautious guide wire–assisted cannulation of bile duct. We also used a large-sized dilator balloon (15 mm esophageal TTS balloon instead of the routine 8-10 mm biliary dilator balloons), which may explain the higher success rate of stone extraction in our study. The difference between studies might be related to several factors, including patients and disease characteristics, endoscopist experience, and available facilities. Most of the previous studies have been done in patients with stones smaller than 10 mm, while our study included patients with stones 10-20 mm. Our study also showed that using a large dilator balloon can facilitate removal of large CBD stones without increasing the rate of complications. Although limited data are available, the study by Tsujino and colleagues found an association between smaller stone size and higher risk of pancreatitis.[20] Also, previous studies mostly used the criteria of Cotton et al.[15] for diagnosis of postoperative pancreatitis, which, according to the study by Watanabe et al., a modification to the criteria in which mild pancreatitis is also included as a complication made it more sensitive and showed higher incidence of pancreatitis in the EPBD group compared with the EST group (10.0% vs 2.2%), although severe pancreatitis has been uncommon with EPBD in several studies.[6,8,11,21]
Also, we didn’t encounter perforation in any group, which was similar to other studies.[19] Although the meta-analysis by Liu et al. showed a significantly higher incidence of bleeding with EST compared with EPBD,[19] we found low incidence (1.2%) in both the groups, which is similar to some other studies.[11] Considering the lower incidence of hemorrhage reported with EPBD, and high mortality rate in patients with cirrhosis who undergo EST,[22,23] EPBD is probably the optimal choice for patients with liver cirrhosis, or other coagulopathies,[24] although, more studies are required in this regard.
There are some limitations for our study. As mentioned above, by using more sensitive criteria for definition of pancreatitis provide better information for comparison of EPBD and EST in this regard. More studies are also required to evaluate the contributory role of the numbers of stones and maximal stone size on the efficacy and safety of EPBD and EST; stone removal, need for EML, and recurrence of stones. Another attractive suggestion for further studies can be a combination of a minimal sphincterotomy, followed by EPBD to see if we can decrease the rate of complications of a generous EST.
CONCLUSION
EPBD, by using a large esophageal dilator balloon, is as safe and effective as EST for removal of large CBD stone. So because of low complication and high success rate, we suggest EPBD as an alternative for EST in the management of large CBD stones.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Yoo KS, Lehman GA. Endoscopic management of biliary ductal stones. Gastroenterol Clin North Am. 2010;39:209–27. doi: 10.1016/j.gtc.2010.02.008. viii, [doi: 10. 1016/j.gtc.2010.02.008] [DOI] [PubMed] [Google Scholar]
- 2.Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, et al. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335:909–18. doi: 10.1056/NEJM199609263351301. [DOI] [PubMed] [Google Scholar]
- 3.Aiura K, Kitagawa Y. Current status of endoscopic papillary balloon dilation for the treatment of bile duct stones. J Hepatobiliary Pancreat Sci. 2011;18:339–45. doi: 10.1007/s00534-010-0362-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baron TH, Harewood GC. Endoscopic balloon dilation of the biliary sphincter compared to endoscopic biliary sphincterotomy for removal of common bile duct stones during ERCP: A metaanalysis of randomized, controlled trials. Am J Gastroenterol. 2004;99:1455–60. doi: 10.1111/j.1572-0241.2004.30151.x. [DOI] [PubMed] [Google Scholar]
- 5.Yasuda I, Tomita E, Enya M, Kato T, Moriwaki H. Can endoscopic papillary balloon dilation really preserve sphincter of Oddi function? Gut. 2001;49:686–91. doi: 10.1136/gut.49.5.686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tsujino T, Kawabe T, Komatsu Y, Yoshida H, Isayama H, Sasaki T, et al. Endoscopic papillary balloon dilation for bile duct stone: Immediate and long-term outcomes in 1000 patients. Clin Gastroenterol Hepatol. 2007;5:130–7. doi: 10.1016/j.cgh.2006.10.013. [DOI] [PubMed] [Google Scholar]
- 7.Sugiyama M, Izumisato Y, Abe N, Masaki T, Mori T, Atomi Y. Predictive factors for acute pancreatitis and hyperamylasemia after endoscopic papillary balloon dilation. Gastrointest Endosc. 2003;57:531–5. doi: 10.1067/mge.2003.143. [DOI] [PubMed] [Google Scholar]
- 8.Komatsu Y, Kawabe T, Toda N, Ohashi M, Isayama M, Tateishi K, et al. Endoscopic papillary balloon dilation for the management of common bile duct stones: Experience of 226 cases. Endoscopy. 1998;30:12–7. doi: 10.1055/s-2007-993721. [DOI] [PubMed] [Google Scholar]
- 9.Sugiyama M, Abe N, Izumisato Y, Masaki T, Mori T, Atomi Y. Risk factors for acute pancreatitis after endoscopic papillary balloon dilation. Hepatogastroenterology. 2003;50:1796–8. [PubMed] [Google Scholar]
- 10.Hong WD, Zhu QH, Huang QK. Endoscopic sphincterotomy plus endoprostheses in the treatment of large or multiple common bile duct stones. Dig Endosc. 2011;23:240–3. doi: 10.1111/j.1443-1661.2010.01100.x. [DOI] [PubMed] [Google Scholar]
- 11.Watanabe H, Yoneda M, Tominaga K, Monma T, Kanke K, Shimada T, et al. Comparison between endoscopic papillary balloon dilatation and endoscopic sphincterotomy for the treatment of common bile duct stones. J Gastroenterol. 2007;42:56–62. doi: 10.1007/s00535-006-1969-9. [DOI] [PubMed] [Google Scholar]
- 12.Fujita N, Maguchi H, Komatsu Y, Yasuda I, Hasebe O, Igarashi Y, et al. Endoscopic sphincterotomy and endoscopic papillary balloon dilatation for bile duct stones: A prospective randomized controlled multicenter trial. Gastrointest Endosc. 2003;57:151–5. doi: 10.1067/mge.2003.56. [DOI] [PubMed] [Google Scholar]
- 13.Disario JA, Freeman ML, Bjorkman DJ, Macmathuna P, Petersen BT, Jaffe PE, et al. Endoscopic balloon dilation compared with sphincterotomy for extraction of bile duct stones. Gastroenterology. 2004;127:1291–9. doi: 10.1053/j.gastro.2004.07.017. [DOI] [PubMed] [Google Scholar]
- 14.Gerke H, Baillie J. To cut or stretch? Am J Gastroenterol. 2004;99:1461–3. doi: 10.1111/j.1572-0241.2004.40358.x. [DOI] [PubMed] [Google Scholar]
- 15.Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, et al. Endoscopic sphincterotomy complications and their management: An attempt at consensus. Gastrointest Endosc. 1991;37:383–93. doi: 10.1016/s0016-5107(91)70740-2. [DOI] [PubMed] [Google Scholar]
- 16.Sato H, Kodama T, Takaaki J, Tatsumi Y, Maeda T, Fujita S, et al. Endoscopic papillary balloon dilatation may preserve sphincter of Oddi function after common bile duct stone management: Evaluation from the viewpoint of endoscopic manometry. Gut. 1997;41:541–4. doi: 10.1136/gut.41.4.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yasuda I, Fujita N, Maguchi H, Hasebe O, Igarashi Y, Murakami A, et al. Long-term outcomes after endoscopic sphincterotomy versus endoscopic papillary balloon dilation for bile duct stones. Gastrointest Endosc. 2010;72:1185–91. doi: 10.1016/j.gie.2010.07.006. [DOI] [PubMed] [Google Scholar]
- 18.Tanaka S, Sawayama T, Yoshioka T. Endoscopic papillary balloon dilation and endoscopic sphincterotomy for bile duct stones: Long-term outcomes in a prospective randomized controlled trial. Gastrointest Endosc. 2004;59:614–8. doi: 10.1016/s0016-5107(04)00157-9. [DOI] [PubMed] [Google Scholar]
- 19.Liu Y, Su P, Lin S, Xiao K, Chen P, An S, et al. Endoscopic papillary balloon dilatation vs endoscopic sphincterotomy in the treatment for choledocholithiasis: A meta-analysis. J Gastroenterol Hepatol. 2012;27:464–71. doi: 10.1111/j.1440-1746.2011.06912.x. [DOI] [PubMed] [Google Scholar]
- 20.Tsujino T, Isayama H, Komatsu Y, Ito Y, Tada M, Minagawa N, et al. Risk factors for pancreatitis in patients with common bile duct stones managed by endoscopic papillary balloon dilation. Am J Gastroenterol. 2005;100:38–42. doi: 10.1111/j.1572-0241.2005.40638.x. [DOI] [PubMed] [Google Scholar]
- 21.Ueno N, Ozawa Y. Pancreatitis induced by endoscopic balloon sphincter dilation and changes in serum amylase levels after the procedure. Gastrointest Endosc. 1999;49:472–6. doi: 10.1016/s0016-5107(99)70045-3. [DOI] [PubMed] [Google Scholar]
- 22.Sugiyama M, Atomi Y, Kuroda A, Muto T. Treatment of choledocholithiasis in patients with liver cirrhosis. Surgical treatment or endoscopic sphincterotomy? Ann Surg. 1993;218:68–73. doi: 10.1097/00000658-199307000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moreira VF, Arribas R, Sanroman AL, Meroño E, Larena C, Garcia M, et al. Choledocholithiasis in cirrhotic patients: Is endoscopic sphincterotomy the safest choice? Am J Gastroenterol. 1991;86:1006–10. [PubMed] [Google Scholar]
- 24.Park DH, Kim MH, Lee SK, Lee SS, Choi JS, Song MH, et al. Endoscopic sphincterotomy vs. endoscopic papillary balloon dilation for choledocholithiasis in patients with liver cirrhosis and coagulopathy. Gastrointest Endosc. 2004;60:180–5. doi: 10.1016/s0016-5107(04)01554-8. [DOI] [PubMed] [Google Scholar]


