Abstract
Background
Hepatitis C is often asymptomatic, presenting with liver failure and cancer decades after infection. People who inject drugs (PWID) and immigrant populations from countries with a moderate-to-high prevalence of hepatitis C virus (HCV) are the main risk groups. Deaths and hospital admissions due to HCV cirrhosis tripled between 1998 and 2010, but the majority of people with chronic HCV are unaware of it.
Aim
To identify patients at risk of developing hepatitis C using routine GP data, to determine the proportion not tested, and to explore GPs’ views regarding testing.
Design and setting
Mixed-methods service evaluation (density-based selection of PWID) in six NHS practices in Bristol.
Method
Patients at risk of HCV were identified. The Health Protection Agency laboratory (now part of Public Health England) provided test results. Semi-structured interviews with 17 GPs were audiorecorded and thematic analyses conducted on anonymised transcripts.
Results
Of 3765 patients identified as being at risk of developing hepatitis C, 3051 (81%) had no test result, including 53% of PWID and 93% of the ‘ethnicity’ group. All GPs said they usually test PWID. Most GPs test for HIV and hepatitis B in immigrants more often than they test for HCV. Barriers to testing included not questioning patients about risk factors, competing priorities, the chaotic lifestyle of PWID, difficulty extracting information from computerised records, and forgetting to address HCV.
Conclusion
Computer prompts and GP education on whom to test are warranted. Ensuring that country of origin and drug use is included on the new-patient questionnaire might also aid case-finding for HCV.
Keywords: evaluation research, hepatitis C, primary health care, screening
INTRODUCTION
In England, approximately 150 000 people (0.4% of adults aged 15–64 years) have chronic hepatitis C virus (HCV) infection: 85% are people who inject drugs (PWID) and 40% of the remainder are from immigrant populations.1,2 It is estimated that more than half of the people who have chronic HCV infection are unaware of it and that, between 2006 and 2008, less than 10% of those with chronic HCV infection received treatment.3,4
HCV is the most rapidly increasing cause of mortality due to liver disease worldwide.5,6 In the UK, hospital admissions and deaths due to HCV-related cirrhosis tripled between 1998 and 2010,3 and an estimated 15 840 people will have HCV-related cirrhosis or hepatocellular carcinoma by 2020.3 The cost of HCV-related disease is projected at £156 million per year in the UK.7 In Bristol, the prevalence among PWID is over 50%; slightly higher than the national prevalence of 45%.4,8 The next key risk group in the UK is migrants. World Health Organization estimates suggest that 2% of people in India, Bangladesh, and Pakistan are infected with HCV. In the UK, national estimates suggest that the prevalence of HCV among South Asians is nearly 1% compared to 0.05% among white non-injectors.2
Guidance on managing hepatitis B and C from the National Institute for Health and Care Excellence (NICE) recommends:
‘... testing for hepatitis B and C [in] adults and children [who are] at increased risk of infection, particularly immigrants from medium- or high-prevalence countries and people who inject, or have injected, drugs’.
HCV testing among PWID and migrants has been assessed as cost-effective.10,11
It is known that targeted case-finding of at-risk groups increases test uptake and diagnosis of asymptomatic patients, and is more effective than opportunistic testing alone.12–18 Guidance from the Royal College of General Practitioners (RCGP) on HCV management advocates the testing of patients who are at risk within primary care.19
Barriers to testing include:
misinformation about HCV;
fears of treatment side-effects; and
Most studies have explored patients’ perspectives, particularly those of PWID. Previous work with GPs has demonstrated:
low awareness of risk groups, other than PWID;
incomplete knowledge regarding treatment and whom to test; and
a reluctance to test people who currently inject drugs due to a risk of reinfection.27–32
A mixed-methods study was conducted to evaluate HCV testing for patients at high risk of developing the disease, and to determine the feasibility of testing in primary care using routinely recorded data. GPs were interviewed to explore their views of HCV testing.
How this fits in
The National Institute for Health and Care Excellence and the Royal College of General Practitioners provide guidance for GPs on testing for hepatitis C, although it is not known whether this is being followed or whether current practice for case-finding is effective. This study shows that the testing of people who inject drugs and immigrants is poor. Improvements to practice must focus on: questioning all patients (for example, through the new-patient questionnaire) to determine those who are at high risk; testing immigrant patients from countries with a moderate-to-high prevalence of hepatitis C virus; and improved data recording.
METHOD
Setting and timeframe
This mixed-methods study involved six GP practices using the Egton Medical Information Systems (EMIS) within NHS Bristol. Purposive sampling was used to include three practices with a high proportion of PWID and three with a low proportion (based on numbers of PWID involved in the NHS Bristol shared-care pathway). Data were collected from the practices and GPs interviewed between August 2012 and January 2013.
Quantitative
A protocol using Read Codes was developed for searching on EMIS LV and EMIS Web. Risk factors were defined according to NICE and RCGP guidance:9,17
injecting or intranasal drug use;
born or brought up in a country with a moderate or high prevalence of HCV (for which ‘ethnicity’ and ‘country born in’ codes were included);
blood transfusion prior to 1991;
blood products prior to 1986;
transplant prior to 1992;
infection with HIV;
infection with hepatitis B; and
born to a mother who has HCV.
Excluded risk factors were:
having had a tattoo or surgery abroad;
being the partner of a person with HCV (not coded within EMIS); and
abnormal liver function tests (it was not possible to determine from EMIS whether this could be attributed to a risk of HCV).
The protocol included a search for ‘HCV positive’ to determine how many patients were coded as such.
Test results since 2006 were obtained for each practice from the local Health Protection Agency (HPA) laboratory (now part of Public Health England), where all HCV tests for NHS Bristol are processed. The two datasets were compared to determine which patients who were considered to be at risk of hepatitis C had tested positive, negative, or had no test result.
At two practices (one with the highest proportion of PWID and one with a low proportion), an additional method of finding test results was applied to validate the method used: individual patient consultation records were scrutinised for results and whether a test had been offered, and accepted or declined. It was beyond the scope of this study to prospectively test patients at risk.
The number and proportion of patients at high risk of hepatitis C who tested for HCV are described, along with any evidence of variation by practice.
Qualitative
GPs were invited for interview by email. One researcher conducted semi-structured, face-to-face interviews with 17 GPs; these lasted for 15–48 (mean 29) minutes. An interview topic guide (informed by the literature) was developed to explore views of the current practice of testing, barriers to testing, interactions with other services, and training and guidelines for HCV testing.24–34
With written informed consent, interviews were audio-recorded and anonymised transcripts (transcribed by the interviewer) were imported into NVivo (version 9) to aid data analysis. Thematic analyses identified issues of particular salience for participants and across the dataset.35 Analysis was ongoing and iterative, informing further data collection. The interviewer coded the data and a subset of transcripts were independently analysed by a second researcher; any discrepancies in interpretation were resolved to maximise rigour.
RESULTS
Quantitative
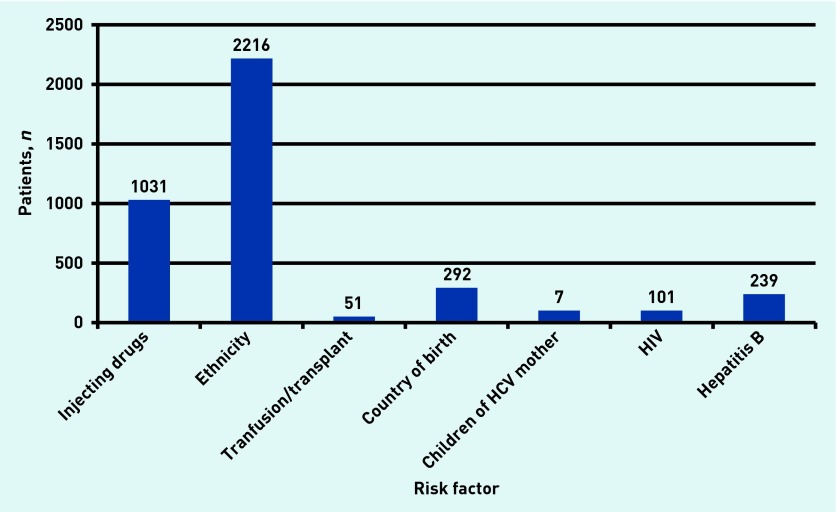
The six practices served 73 814 patients. Of these, 3765 (5%) were identified as being at high risk of HCV. Figure 1 shows the distribution of risk factors; 324 patients had two or more risk factors (data not shown).
Figure 1.
Risk-factor frequency in patients at risk of hepatitis C virus.
Of the 3765 patients at risk, 308 (8%) had tested positive, 406 (11%) negative, and 3051 (81%) had no result. Of the 308 patients who were HCV positive, 235 (76%) were PWID.
There was variation in test uptake by practice for the major risk factors (Table 1). The proportion of PWID and were tested ranged from 29% to 62% (Likelihood Ratio Test [LRT] χ2 [degrees of freedom (df) 5] 81.33 P<0.001). The proportion of people who were tested and from selected minority ethnic groups or countries of birth with a moderate-to-high HCV prevalence ranged from 3% to 20% (LRT χ2 (df 5) 27.46 P<0.001).
Table 1.
Patient testing and major risk factors, by practice
| Risk factor |
Practice 1
|
Practice 2
|
Practice 3
|
Practice 4
|
Practice 5
|
Practice 6
|
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patients with risk factor, n | Patients tested for HCV, % | Patients with risk factor, n | Patients tested for HCV, % | Patients with risk factor, n | Patients tested for HCV, % | Patients with risk factor, n | Patients tested for HCV, % | Patients with risk factor, n | Patients tested for HCV, % | Patients with risk factor, n | Patients tested for HCV, % | |
| Injecting drugs | 424 | 62 | 265 | 29 | 103 | 47 | 157 | 39 | 47 | 45 | 35 | 40 |
| Ethnicity | 274 | 14 | 483 | 7 | 454 | 7 | 588 | 5 | 127 | 6 | 290 | 3 |
| Country of birth | 44 | 14 | 137 | 9 | 17 | 6 | 74 | 7 | 15 | 7 | 5 | 20 |
HCV = hepatitis C virus.
Practices with more than two GPs who had undertaken RCGP training on HCV infection were more likely to test PWID than those with fewer GPs who had undertaken RCGP training (61% of 459 PWID tested versus 36% of 572 PWID respectively (odds ratio 2.7, 95% confidence interval = 2.1 to 3.4). The practices differed in their proportion of PWID (0.4% to 5.7%) and practices’ Index of Multiple Deprivation scores (9.35 to 43.46), but there was too much collinearity in this small study to undertake multivariable analysis.
A comparison of the methods for determining test results is shown in Table 2. The patient-record search revealed more results than using HPA laboratory data alone.
Table 2.
Patients identified for HCV testing using additional methods
| Method | Practice 1 (n) | Practice 5 (n) |
|---|---|---|
| Total tested: HPA laboratory | 144 | 17 |
| Total tested: patient-record search | 229 | 45 |
| From patient record search: test offered and refused | 7 | 3 |
| From patient record search: test offered and no result | 64 | 1 |
| Extra results from patient-record search compared with HPA laboratory alone | 85 | 28 |
HCV = hepatitis C virus. HPA = Health Protection Agency.
Qualitative
In total, 17 GPs were interviewed; years since qualification ranged from 1 to 31 (one GP registrar). Nine were male, seven had an interest in addiction, and nine were from practices with a high proportion of PWID. Analysis of the interview transcripts revealed three key themes:
the motivation for HCV testing;
barriers to HCV testing; and
ideas for improvements to practice.
Reasons to test for HCV
GPs reported that their experience of HCV infection had been mostly with PWID, and this was the group they most frequently tested. Many reported they would test patients who disclosed any drug use, not exclusively those who injected drugs:
‘Anybody who comes to me with a drug problem really. Well, of course, particularly those who are injecting, but, um, even those who say they’re not injecting, they really, they would be the the first people to be tested.’ Dr F
(male, drug and alcohol lead, practice with a high proportion of PWID)
Only two GPs said they would test immigrant patients from countries with a high prevalence of HCV:
‘Well we have an awful lot of African, mostly Somali, um, and they, they tend to all get screened in the … the [named service], the asylum seekers project. Erm, but I think … our consideration of testing would probably be slightly higher in, in those patients. Not particularly because of any good evidence but just because they’re, you, you don’t know [what] their history is.’ Dr D
(female, practice with a high proportion of PWID)
The remaining GPs considered such patients to be at greater risk of hepatitis B and HIV, not HCV:
‘Because of its transmission being primarily through, er, basically through blood, um, there … rather than necessarily, um … er … solely through sexual contact, um, things like HIV tend to be far more potentially transmissible without prior knowledge and, therefore, you know, one would be much more concerned about, sort of, er, somebody being appropriate for screening for HIV rather than necessarily hep C just because of their migrant, er, their immigrant status.’ Dr L
(male, practice with a low proportion of PWID)
Most GPs did not routinely question patients about HCV risk factors:
‘We do ask everyone about alcohol on registration and so there is a school of thought that occasionally bubbles up in practice meetings about, you know, how much should we be asking everybody routinely at registration about, you know, alcohol, drugs, hepatitis, you know. Should we be asking these questions? Um ... we don’t at the moment.’ Dr B
(male, interest in addiction, practice with a high proportion of PWID)
These GPs would, however, ask about risk factors if prompted by the patient’s history. One GP, with an interest in addiction, reported routinely questioning all patients about risk factors for HCV:
‘Yup ... I’m completely cynical … [laughs] Everybody who walks through that door’s using heroin until they tell me otherwise. [laughs] Because that’s just my experience of working at the moment.’ Dr G
(male, interest in addiction, practice with a low proportion of PWID)
A minority of GPs mentioned that patients infected with HIV or hepatitis B should be tested for HCV. Other reported reasons for testing included:
abnormal liver function;
high-risk sexual activity;
‘infertility screening’; and
blood transfusion.
Barriers to testing
The majority of GPs defined their role as identifying cases of HCV, but noted difficulties in raising the subject. Most GPs reported confidence in their knowledge of HCV, but admitted the problem of remembering to test, particularly if patients initially declined testing:
‘I think it’s more usually a sin of omission really, in that we are supposed to invite people every year to have it done, unless you have the template up you might not kind of think to yourself, “actually I haven’t offered this for a while”.’ Dr J
(female, practice with a low proportion of PWID)
‘I remember I was much more aware when we had, whatever this Department of Health thing was, 5 or 6 years ago. I was much more aware then, briefly, er, it probably fell a little bit from the radar, and you see a patient and it heightened your awareness and it falls on the radar a bit.’ Dr K
(female, interest in mental health, practice with a low proportion of PWID)
GPs would be more likely to address HCV infection if it is a priority for them, which, in turn, is influenced by how recently and frequently they see a case of it, whether they have an interest in addiction, and the need to address acutely presenting issues:
‘Because I’m one of the two doctors in the practice who focuses on drug addicts, um, that that is a very standard part of the assessment.’ Dr O
(male, interest in addiction, practice with a low proportion of PWID)
HCV being a slowly progressive infection would get less priority than more immediate issues, given the limited consultation time:
‘It’s not a bottomless pit and time is quite limited, and you have 10-minute appointments and so, if you’re seeing somebody with, say, polycystic ovaries, you’re not gonna start talking about their hep C risks.’ Dr M
(female, practice with a low proportion of PWID)
The importance of building a rapport with patients was highlighted:
‘We have, er, much more ownership of the problem if we have a personal, personal link with … the sense of priority about the problems that partly goes with the, with that kind of more personal knowledge, clinical relationship with the person over a little bit of time. And that’s the, and that’s the underlying thing with a lot of this hep C stuff.’ Dr P
(male, interest in addiction, practice with a low proportion of PWID)
Two GPs mentioned problems in developing rapport with PWID because of infrequent contact with them, making it difficult to broach the subject of HCV:
‘I know those three or four are quite chaotic. So as in I’ve seen them two or three times but they might jump and start and go to different people … Um so you know I wouldn’t say that I’ve got some I’ve that real rapport that I would with other patients that I see really regularly.’ Dr K
(female, interest in mental health, practice with a low proportion of PWID)
GPs also reported difficulties in finding previous (if any) test results from computerised records. One mentioned a computer system used by drug keyworkers (to which not all GPs have access) which mandates input of HCV status. The GP believed this resulted in patients being more comprehensively managed by the drug keyworker. The impact of not knowing a patient’s HCV status is that GPs rely on the patient’s memory, making it challenging to manage patients with an ongoing risk of infection:
‘It’s not, um, often on the computer … whether it’s been done before or not … because it’s not coded on they, er, er, it could be done anywhere and, if the patient says “oh yeah, I’ve already had it done”, but we haven’t got any information on the computer, then we have to accept that they, they have had it done and, you know, er, we don’t chase them up … They’re more likely to be tested I think if they are in shared care with [local drugs service] because ... it’s part of the measurement of the, er, The- do you know Theseus? ... Well that specifically, um, asks about hepatitis C, and the drugs workers are obliged to fill the, the, the minimum data set out on Theseus.’ Dr F
(male, drug and alcohol lead, practice with a high proportion of PWID)
All GPs had a drug keyworker at their practice and most said they would leave it to them to raise the issue of HCV. A few remarked that patients had different expectations of them as ‘prescribers’, compared with the drug keyworker who is seen to address their general wellbeing:
‘We’re seen as the prescribers and so we prescribe, and patients, you know, that’s what you’re there for really as far as they’re concerned, they want something from you. Whereas I think the [local drugs service], you know, health promotion is a key thing and they’re, you know, and it’s, er … so that, that’s a useful format it seems to me for providing people with health information.’ Dr I
(male, practice with a high proportion of PWID)
GPs noted that HCV infection was a difficult issue for patients to address; patients may not be willing to consider testing, or may not be able to cope with the diagnosis:
‘The difficulties I encounter are patients who don’t feel ready to be tested. Um, they suspect they’ve got the disease but prefer to bury their heads in the sand at this time. Or they feel too fragile to take it on board.’ Dr E
(male, drug and alcohol lead, practice with a high proportion of PWID)
Often due to a lack of structure in their lives, patients may be unable to attend appointments or engage with treatment. Most GPs do not consider ongoing substance misuse as a barrier to testing, but they emphasised that patients need stable lives to commit to the demands of treatment:
‘So the main issue is helping life, you know, to get their life sufficiently stable, um, for a period of time, um, so they’re gonna be able to engage with what is a fairly intense long-term process, about 6 months or so, of treatment and regular appointments that they have to keep.’ Dr O
(male, interest in addiction, practice with a low proportion of PWID)
GPs frequently stated that difficult venous access prohibited testing. Many found the dried blood spot test useful, particularly for PWID:
‘I think the, the big, the dried blood spot testing has been a really big advance. I know that’s perhaps old hat now, maybe it’s been about 4 years old or something like that? But ... but before then it was a real pain to get to get people with very poor venous access, um, into treatment.’ Dr F
(male, drug and alcohol lead, practice with a high proportion of PWID)
The dried blood spot test can be used to detect anti-HCV antibody and HCV ribonucleic acid by polymerase chain reaction (PCR). Although a single sample can be used to test for HCV, hepatitis B, and HIV, some GPs believed it cannot be used for HCV PCR or other blood-borne virus tests:
‘The difficulty with dried blood spot is that they can’t normally do PCRs on them so can’t tell you if it’s active.’ Dr G
(male, interest in addiction, practice with a high proportion of PWID)
A minority of GPs said there were no barriers to testing; two were from a practice with a higher proportion of PWID, and two had an interest in addiction.
Improvements to practice
Many GPs felt that raising their awareness of who to test would be the best way forward:
‘I mean, I guess us having greater awareness and just, sort of, being a bit more tuned into the people that we should be offering it to … a lot of the time that we have a knee-jerk response to to screening in certain, you know, very specific clinical situations, but it’s not something that often thought about otherwise really.’ Dr N
(female, area of low deprivation)
One GP (with an interest in addiction) suggested a primary care mini-clinic specifically for PWID. This had been trialled in their practice, but was difficult to implement:
‘Um, because I think it’s complex and it needs time and, really, one would like to work alongside a [local drugs service] colleague and, and, ask advice and, and, change patients. And one would like to have, um, er … one would like to have facilities for testing like on the spot, rather than to get people back for testing and then missed appointments and this that and the other, you know. So I think almost like a one stop-clinic idea, um, would work.’ Dr E
(male, drug and alcohol lead, practice with a high proportion of PWID)
Several GPs felt that better access to test results would be useful:
‘I think the thing that’s, personally, I think the thing that’s most important is to have a, a good accessible record and recall system. Um, er, to have a way of, of quickly being able to see when somebody was tested, what the last result was, and when they next need doing.’ Dr E
(male, drug and alcohol lead, practice with a high proportion of PWID)
One suggestion was giving patients HCV status cards with their test results:
‘Providing people patients with actual cards that say on this date you’re hepatitis C negative or whatever would be useful really … the idea of providing people with their own information with the chaotic group, something like that might actually work.’ Dr I
(male, practice area with high level of deprivation)
DISCUSSION
Summary
The study findings showed that it is possible for GPs to routinely collect data that would help identify patients at risk of HCV infection. Of patients at risk, 81% had no test result. Case-finding for HCV was mainly among PWID. Although all GPs stated that they test PWID, this study found that testing ranged from 29% to 62% (median 42.5%). In the individual practices in this study, 29–62% of people injected drugs; however, the data cannot conclude that practices with a higher population of PWID tested more patients. GPs were more likely to test for HCV if they had greater exposure to PWID. Practices with more GPs who had completed RCGP training on HCV infection performed more tests.
Most GPs incorrectly believed that they did not need to test people from countries with a moderate-to-high prevalence of HCV; this was reflected in the low proportion tested (range 3–20%, median 7% ‘ethnicity’ and 9% ‘country born in’).
It is difficult for GPs to quickly and reliably determine HCV status from EMIS coding alone; they often have to rely on patients’ memories of HCV results. Very few patients refused testing as determined by scrutinising patient records. This method provided more information but was less robust due to large variability in the content of the consultation notes.
These data also highlight barriers to testing (for example, venous access, patients’ chaotic lifestyle, pressure for GPs to address more immediate problems) that have previously been noted.20–31
The results identified new barriers to case-finding: GPs do not always know who is at risk because they do not routinely ask about risk factors; they do not always consider immigrants as a risk group; they often rely on drug keyworkers to address HCV but do not have access to their records. This study confirms that the majority of patients with HCV are PWID, that GPs are most aware of the need to test PWID and less aware of other risk groups.
This study also identified incorrect beliefs about use of the dried blood spot test, which could have resulted in patients with difficult venous access not being tested.
Strengths and limitations
The main strength of this mixed-methods study is the ability to triangulate the quantitative and qualitative data. Inferring that those people without a test result were ‘not tested’ was deliberately avoided. The HPA laboratory could trace results back to the original requestor but patients tested at other practices or institutions would, therefore, be missed.
The use of routinely recorded data may have missed patients whose risk factors were not documented. As a result of this, the proportion of patients with no test recorded is likely to have been underestimated. Furthermore, the results only pertain to patients registered with a GP.
This study included ‘ethnicity’ and ‘country born in’ codes to find patients who were born or brought up in countries with moderate-to-high HCV prevalence rates. ‘Ethnicity’ was more frequently recorded than ‘country born in’ but, as people define ethnicity in different ways, this alone may not accurately identify those people with a genuine risk of HCV infection.
This exploratory study sampled six practices within one primary care trust. A larger study is required to validate the results.
Comparison with existing literature
In total, 1.4% of this study population were PWID; previous estimates of prevalence of PWID were 1.3% for Bristol, 2.0% for Brighton, 1.5% for Liverpool, and 1.7% in inner London.8,36
Barriers to testing, including the non-stable lifestyle of PWID and the time pressures within consultations, have been described by D’Souza et al.27 Of PWID, 53% had no test result; Cullen et al found a similar result in 2003, again demonstrating little change in practice over the past 10 years.37 This is despite the Department of Health campaigns to raise HCV awareness in 2004 and 2009, the RCGP training modules, and the Hepatitis C Trust’s campaigns, particularly among South Asians.
Implications for practice
As HCV infection is usually asymptomatic, case-finding needs to be proactive and based on risk information. Primary-care databases can be used to identify patients who need testing, however difficulties arise due to documentation anomalies. Further GP training needs to emphasise testing patients from countries with moderate-to-high HCV prevalence rates, and encourage GPs to question all patients about risk factors. Financial incentives (for example, linking HCV testing with payment for methadone prescriptions may also be required to improve case-finding, especially in practices with large numbers of migrant populations or PWID.
Acknowledgments
We thank all the practices and GPs who partcipated in this study, the practice managers, and IT support staff at the practices. We also thank Dr Matthew Donati and Paul North at the Health Protection Agency laboratory (now part of Public Health England) for providing hepatitis C virus test results, and Barbara Coleman and John Twigger at Bristol Primary Care Trust for information about the practices.
Funding
Funding for this work was received from the University of Bristol and the Severn Deanery.
Ethical approval
Ethical approval was provided by the Faculty of Medicine and Dentistry Committee for Ethics in 2012 (ref. 121325). Research and development approval was from the University of Bristol (study ref. 1915). The study was registered with the Avon Primary Care Research Collaborative (ref. 2012. E059).
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: www.bjgp.org/letters
REFERENCES
- 1.De Angelis D, Sweeting M, Ades A, et al. An evidence synthesis approach to estimating Hepatitis C prevalence in England and Wales. Stat Methods Med Res. 2009;18:361–379. doi: 10.1177/0962280208094691. [DOI] [PubMed] [Google Scholar]
- 2.Harris RJ, Ramsay M, Hope BD, et al. Hepatitis C prevalence in England remains low and varies by ethnicity: an updated evidence synthesis. Eur J Public Health. 2011;22(2):187–192. doi: 10.1093/eurpub/ckr083. [DOI] [PubMed] [Google Scholar]
- 3.Health Protection Agency Hepatitis C in the UK 2011 Report. http://www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1309969906418 (accessed 11 Dec 2013).
- 4.Department of Health Hepatitis C Action Plan for England. 2004. Jul, http://www.nhs.uk/hepatitisc/SiteCollectionDocuments/pdf/hepatitis-c-action-plan-for-england.pdf (accessed 11 Dec 2013).
- 5.Shepard CW, Finelli L, Alter MJ. Global epidemiology of hepatitis C virus infection. Lancet Infec Dis. 2005;5(9):558–567. doi: 10.1016/S1473-3099(05)70216-4. [DOI] [PubMed] [Google Scholar]
- 6.Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.The University of Southampton Liver Group The UK vs Europe: Ready to fight back? 2006. The Hepatitis C Trust. University of Southampton. http://www.hepctrust.org.uk/Resources/HepC/Migrated%20Resources/Documents/Other/281_Euro%20Report%20final.pdf (accessed 11 Dec 2013).
- 8.Hickman M, Hope V, Coleman B, et al. Assessing IDU prevalence and health consequence (HCV, overdose and drug-related mortality) in a primary care trust: implications for public health action. J Public Health. 2009;31(3):374–382. doi: 10.1093/pubmed/fdp067. [DOI] [PubMed] [Google Scholar]
- 9.National Institute for Health and Care Excellence Hepatitis B and C: ways to promote and offer testing to people at increased risk of infection NICE. 2012. http://guidance.nice.org.uk/PH43 (accessed 11 Dec 2013).
- 10.Martin NK, Hickman M, Miners A, et al. Cost-effectiveness of HCV case-finding for people who inject drugs via dried blood spot testing in specialist addiction services and prisons. BMJ Open. 2013;3(8):e003153. doi: 10.1136/bmjopen-2013-003153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Miners AH, Martin NK, Ghosh A, et al. Assessing the cost-effectiveness of finding cases of hepatitis C infection in UK migrant populations and the value of further research. J Viral Hepat. 2013 doi: 10.1111/jvh.12190. [DOI] [PubMed] [Google Scholar]
- 12.Cullen BL, Hutchinson SJ, Cameron SO, et al. Identifying former injecting drug users infected with hepatitis C: an evaluation of a general practice-based case-finding intervention. J Public Health. 2011;34(1):14–23. doi: 10.1093/pubmed/fdr097. [DOI] [PubMed] [Google Scholar]
- 13.Arnold DT, Bentham LM, Jacob RP, et al. Should patients with abnormal liver function tests in primary care be tested for chronic viral hepatitis: cost minimisation analysis based on a comprehensively tested cohort. BMC Fam Pract. 2011;12:9. doi: 10.1186/1471-2296-12-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lewis H, Burke K, Begum S, et al. What is the best method of case finding for chronic viral hepatitis in migrant communities? Gut. 2011;60:A26. [Google Scholar]
- 15.Kim AY, Nagami EH, Birch CE, et al. A simple strategy to identify acute hepatitis C virus infection among newly incarcerated injection drug users. Hepatology. 2013;57(3):944–952. doi: 10.1002/hep.26113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cullen W, Stanley J, Langton D, et al. Hepatitis C infection among injecting drug users in general practice: a cluster randomised controlled trial of clinical guidelines’ implementation. Br J Gen Pract. 2006;56(532):848–856. [PMC free article] [PubMed] [Google Scholar]
- 17.Foster GR. Injecting drug users with chronic hepatitis C: should they be offered antiviral therapy? Addiction. 2008;103:1412–1413. doi: 10.1111/j.1360-0443.2008.02214.x. [DOI] [PubMed] [Google Scholar]
- 18.Helsper CW. Case finding strategies for hepatitis C infection. 2011. [Thesis]. Julius Center for Health Sciences and Primary Care, University Medical Center Utrecht, University Utrecht, Faculty of medicine. http://igitur-archive.library.uu.nl/dissertations/2011-1201-200339/helsper.pdf (accessed 11 Dec 2013). [Google Scholar]
- 19.Royal College of General Practitioners Guidance for the prevention, testing, treatment and management of hepatitis C in primary care. 2007. RCGP. http://www.smmgp.org.uk/download/guidance/guidance003.pdf (accessed 11 Dec 2013).
- 20.Ellard J. ‘There is no profile it is just everyone’: The challenge of targeting hepatitis C education and prevention messages to the diversity of current and future injecting drug users. Int J Drug Policy. 2007;18:225–234. doi: 10.1016/j.drugpo.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 21.Rhodes T, Treolar C. The social production of hepatitis C risk among injecting drug users: a qualitative synthesis. Addiction. 2008;103(10):1593–1603. doi: 10.1111/j.1360-0443.2008.02306.x. [DOI] [PubMed] [Google Scholar]
- 22.Schackman BR, Teixeira PA, Beeder AB. Offers of hepatitis C care do not lead to treatment. J Urban Health. 2007;84(3):455–458. doi: 10.1007/s11524-007-9180-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tompkins CN, Wright NM, Jones L. Impact of a positive hepatitis C diagnosis on homeless injecting drug users: a qualitative study. Br J Gen Pract. 2005;55(513):263–268. [PMC free article] [PubMed] [Google Scholar]
- 24.Davis M, Rhodes T, Martin A. Preventing hepatitis C: ‘Common sense’, ‘the bug’ and other perspectives from the risk narratives of people who inject drugs. Soc Sci Med. 2004;59:1807–1818. doi: 10.1016/j.socscimed.2004.02.021. [DOI] [PubMed] [Google Scholar]
- 25.Miller ER, McNally S, Wallace J, Schlichthorst M. The ongoing impacts of hepatitis c- a systematic narrative review of the literature. BMC Public Health. 2012;12:672. doi: 10.1186/1471-2458-12-672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Southgate E, Weatherall AM, Day C, Dolan KA. What’s in a virus? Folk understandings of hepatitis C infection and infectiousness among injecting drug users in Kings Cross, Sydney. Int J Equity Health. 2005;4(1):5. doi: 10.1186/1475-9276-4-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.D’Souza RFC, Glynn MJ, Alstead E, et al. Knowledge of chronic hepatitis C among East London primary care physicians following the Department of Health’s educational campaign. Q J Med. 2004;97:331–336. doi: 10.1093/qjmed/hch060. [DOI] [PubMed] [Google Scholar]
- 28.Cozzolongo R, Cuppone R, Petruzzi J, et al. Approach of primary care physicians to hepatitis C: an educational survey from a Southern Italian area. J Infect. 2005;51:396–400. doi: 10.1016/j.jinf.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 29.Leverence RR, Williams RL, Pace W, et al. Context of clinical care: the care of hepatitis C in underserved communities- a report from the Primary Care Multiethnic Network (PRIME Net) Consortium. J Am Board Fam Med. 2009;22(6):638–646. doi: 10.3122/jabfm.2009.06.090020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Perry M, Chew-Graham C. Finding a vein or obtaining consent: a qualitative study of hepatitis C testing in GP methadone clinics. Fam Pract. 2003;20(5):538–544. doi: 10.1093/fampra/cmg508. [DOI] [PubMed] [Google Scholar]
- 31.McGowan CE, Monis A, Bacon BR, et al. A global view of hepatitis C: Physician knowledge, opinions, and perceived barriers to care. Hepatology. 2013;57(4):1325–1332. doi: 10.1002/hep.26246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hellard M, Sacks-Davis R, Gold J. Hepatitis C treatment for injection drug users: a review of the available evidence. Clin Infect Dis. 2009;49:561–573. doi: 10.1086/600304. [DOI] [PubMed] [Google Scholar]
- 33.Wallace J, McNally S, Richmond J, et al. Managing chronic hepatitis B: a qualitative study exploring the perspectives of people living with chronic hepatitis B in Australia. BMC Research Notes. 2011;4:45. doi: 10.1186/1756-0500-4-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Crowe S, Cantrill JA, Tully MP. Chared care arrangements for specialist drugs in the UK: the challenges facing GP adherence. Qual Saf Health Care. 2010;19:54. doi: 10.1136/qshc.2009.035857. [DOI] [PubMed] [Google Scholar]
- 35.Braun V, Braun CV. Using thematic analysis in psychology. Qualitative Research in Psychology. 2006;3:77–101. [Google Scholar]
- 36.Hickman M, Higgins V, Hope V, et al. Injecting drug use in Brighton, Liverpool, and London: best estimates of prevalence and coverage of public health indicators. J Epidemiol Community Health. 2004;58(9):766–771. doi: 10.1136/jech.2003.015164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cullen W, Bury G, Barry J, O’Kelly FD. Hepatitis C infection among drug users attending general practice. Ir J Med Sci. 2003;172(3):123–127. doi: 10.1007/BF02914496. [DOI] [PubMed] [Google Scholar]