Abstract
Background
Heart disease is difficult to detect clinically and it has been suggested that echocardiography should be available to all patients with possible cardiac symptoms or signs.
Aim
To analyse the results of 2 years of open access echocardiography for the frequency of structural heart disease according to request.
Design and setting
Retrospective database analysis in a teaching hospital open access echocardiography service.
Method
Reports of all open access transthoracic echocardiograms between January 2011 and December 2012 were categorised as normal, having minor abnormalities, or significant abnormalities according to the indication.
Results
There were 2343 open access echocardiograms performed and there were significant abnormalities in 29%, predominantly valve disease (n = 304, 13%), LV systolic dysfunction (n = 179, 8%), aortic dilatation (n = 80, 3%), or pulmonary hypertension (n = 91, 4%). If echocardiography had been targeted at a high-risk group, 267 with valve disease would have been detected (compared to 127 with murmur alone) and 139 with LV systolic dysfunction (compared to 91 with suspected heart failure alone). Most GP practices requested fewer than 10 studies, but 6 practices requested over 70 studies.
Conclusion
Open access echocardiograms are often abnormal but structural disease may not be suspected from the clinical request. Uptake by individual practices is patchy. A targeted expansion of echocardiography in patients with a high likelihood of disease is therefore likely to increase the detection of clinically important pathology.
Keywords: echocardiography, general practice, heart valve disease
INTRODUCTION
The population prevalence of heart failure or of valve disease are similar, 2–3% in the general population rising to 10–20% in those aged over 75 years.1,2 Both conditions are underdetected,1,2 leading to unnecessary premature morbidity and deaths. Unrestricted population screening using echocardiography is not an answer since it has a low yield3 and is therefore more likely to cause anxiety4,5 than find clinically significant abnormalities. However it has been suggested6,7 that echocardiography should be more readily available for patients with a high likelihood of cardiac disease based on history, signs or symptoms.
Open access echocardiography was offered by 133 (71%) hospitals replying to a 2007 UK national survey8 and 19 of these used a portable machine in the community. It is likely that the current reorganisation of the NHS will result in a demand for more community services. It would be useful to know whether these changes might be expected to increase the detection of structural heart disease especially valve disease which is the subject of increasing attention7,9 This study analysed the results of 2 years of open access echocardiography to see how often abnormalities particularly of the left ventricle and valves were detected according to the indication for the request.
METHOD
Guy’s and St Thomas’ Hospital Trust acts as a secondary hospital for a catchment area of approximately 500 000, which is mainly served by 98 general practices (51 in Lambeth and 47 in Southwark). Details of practice population sizes were obtained from the Association of Public Health Observatories website (http://www.apho.org.uk/PRACPROF/). The hospitalI also receives tertiary and quaternary cardiac referrals. It performed 29 241 echocardiograms from 1 January 2011 to 31 December 2012 including 19 262 outpatient transthoracic studies of which 2343 (12%) were open access studies (that is echocardiography requested by the GP without direct involvement of a cardiologist). The open access studies were performed at Guy’s and St Thomas’ Hospitals and at a community centre in Streatham. The open access request form includes indications for open access echocardiography and also gives guidance for when echocardiography would be more clinically appropriate at the time of a cardiology outpatient clinic or inpatient admission. Requests for suspected heart failure are only considered if the B-type natriuretic peptide level is elevated. ‘Cardiac history’ included previous heart surgery, abnormalities suggested by echocardiography while on holiday or before migration and previous treatment for heart disease, but was often not explained in detail on the form. Transthoracic echocardiography (TTE) was performed using a Vivid-7, Vivid I system (GE Medical, Milwaukee, WI, USA) or iE33 (Phillips Medical systems, Andover, MA, US).
How this fits in
Structural heart disease is known to be underdetected despite increasing prevalence rates. This report showed that significant left ventricular and valve disease, pulmonary hypertension and aortic dilatation are frequently found on open access echocardiograms but may not be expected from the indication for the request. Uptake by individual practices was patchy. This suggests that echocardiography should be more readily available for clinical groups at high risk of structural disease identified by a murmur, raised BNP level, past cardiac symptom history and atrial fibrillation.
The reports were retrospectively classified into four groups. Group 1 was normal, Group 2 had a minor abnormality not expected to change management, Groups 3 and 4 had a definite abnormality likely to require a change in management either electively (Group 3) or more urgently (Group 4) (Box 1).
Box 1. Examples of abnormalities by group
Group 2
Mild mitral or aortic regurgitation, aortic sclerosis, mitral annulus calcification, mild diastolic dysfunction in the elderly, mild left ventricular (LV) hypertrophy (septal width ≤13 mm with no evidence of diastolic dysfunction or left atrial dilatation)
Group 3
Mild LV systolic dysfunction (LV ejection fraction 40–50%), right ventricular dilatation or impairment, bicuspid aortic valve, mitral prolapse, aortic dilatation >4.0cm, mild mitral or aortic stenosis, moderate aortic or mitral regurgitation, estimated pulmonary artery systolic pressure ≥35mmHg, atrial or ventricular septal defect or, moderate LV hypertrophy (≥14mm)
Group 4
Severe valve disease, pericardial effusion, moderate or severe LV systolic dysfunction (LV ejection fraction <40%).
Analysis
The data were summarised as mean or proportion as appropriate. A χ2 test was used to compare proportions with normal studies between those with suspected heart failure and murmur.
RESULTS
Over the 2-year period 2343 open access echocardiograms were performed. The mean age at the time of echocardiography was 56 (range 17 to 96) years and 43% were men and 57% women. Only 378 were referred to the community centre. This was insufficient for subgroup analysis but there were no obvious differences from the main population.
The most frequent indications were for murmur and suspected heart failure, which together accounted for 56% of requests (Figure 1). In 5% the reason for the test was not entered into the report.
Figure 1.
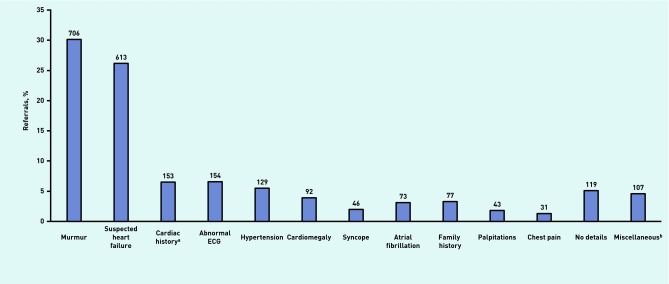
Histogram showing number of requests by clinical indication.aIncluded previous heart surgery, abnormalities suggested by echocardiography while on holiday and previous treatment for heart disease, but was often not explained in detail on the form. bIncluded isolated ankle swelling, stroke, pre-cancer treatment and sickle cell disease.
Requests were made by 118 practices, 84 in Lambeth and Southwark and 34 outside, mainly from Wandsworth, Westminster and Lewisham There were fewer than 10 requests in 65, 10–29 requests in 27, 30–49 requests in 13, 50–69 requests in 7, 70–89 requests in 5 and 100 requests in one practice. Practice populations were accessible for 106 and in these the numbers per 1000 practice population ranged from 0.000072 and 0.012 and are shown in Table 1.
Table 1.
Frequency of requests in 2 years by practice size
| Requests per 1000 practice population | Number of practices |
|---|---|
| <0.001 | 45 |
| 0.001–0.0019 | 11 |
| 0.002–0.0029 | 13 |
| 0.003–0.0039 | 6 |
| 0.004–0.0049 | 9 |
| 0.005–0.0059 | 11 |
| 0.006–0.0069 | 4 |
| 0.007–0.0079 | 2 |
| 0.008–0.0089 | 1 |
| 0.009–0.0099 | 1 |
| >0.01 | 3 |
|
| |
| Total | 106 |
Abnormalities by indication
Figure 2 shows the proportion of requests in each group by indication. For the whole population, there were significant abnormalities in 691, requiring elective management changes in 547 (23%; Group 3) and more urgent changes in 144 (6%; Group 4). The study was normal (Group 1) in 1115 (48%) or had minor abnormalities (Group 2) in 537 (23%). The frequencies were similar for those with a murmur normal in 368 (52%); minor abnormalities in 154 (22%). Those with suspected heart failure were less likely to be normal: normal in 218 (36%); minor abnormalities in 141 (23%). The proportion of normal studies in patients with murmur and suspected heart failure were significantly different (χ2 11; P<0.001). Most studies were normal when requested for screening as a result of family history of heart disease or for palpitation.
Figure 2.
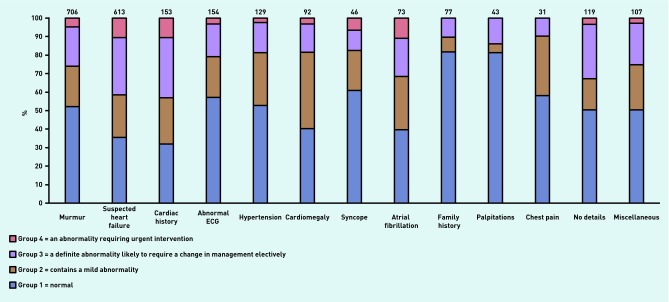
Histogram showing Group 1–4 as a percentage of the total by indication
Valve abnormalities
Figure 3 shows the incidence of minor (Group 2) and significant (Group 3 and 4) valve disease. Significant valve disease occurred in 127 (18%) with a murmur and 304 (13%) in the whole population. In patients with suspected heart failure the valve disease was primary (organic) in 58 (67%) and secondary (functional) in 28 (33%). Mild valve disease (Group 2) occurred in 81 (11%) with murmur, but in 212 (9%) in the whole population. Most with valve disease, 87%, were aged >60 years and all were >45 years.
Figure 3.
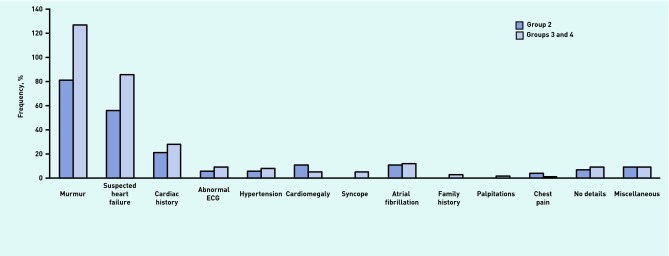
Histogram showing frequency of mild (Group 2) and significant (Group 3 and 4) abnormalities of left ventricular geometry and function according to clinical request.
To improve the detection of valve disease, it has been suggested3 that community-based echocardiography should be available to patients with murmur, atrial fibrillation or any cardiac symptom. Using these criteria, 267 (15%) of 1745 studies showed significant valve disease.
Left ventricular hypertrophy or left ventricular dysfunction
Significant LV hypertrophy occurred in only 36 (1.8%) and was uncommon even if the echocardiogram was requested because of hypertension (Table 2). However mild LV hypertrophy (Group 2) occurred in 145 (7%). Isolated abnormal diastolic filling occurred in 66 (3%). LV systolic impairment occurred in 91 (15%) patients with suspected heart failure, but also in 8 (11%) with atrial fibrillation and 19 (12%) with a cardiac history. LV systolic dysfunction occurred in 139 (13%) of 1089 at high-risk because of cardiac history, murmur, atrial fibrillation, raised B-type natriuretic peptide or cardiac symptom.
Table 2.
Left ventricular (LV) abnormalities of geometry and function by clinical indication
| LV hypertrophy | LV systolic | LV diastolic | ||
|---|---|---|---|---|
|
| ||||
| Group 2 n (%) | Group 3/4 n (%) | impairment n (%) | dysfunction n (%) | |
| Murmur | 25 (3.5) | 19 (2.6) | 10 (1) | 18 (2.5) |
| Suspected heart failure | 41 (7) | 12 (2) | 91 (15) | 25 (4) |
| Cardiac history | 3 (2) | 4 (2.6) | 19 (12) | 2 (1) |
| Abnormal ECG | 15 (10) | 5 (3) | 11 (7) | 3 (2) |
| Hypertension | 23 (18) | 8 (6) | 5 (4) | 3 (2) |
| Cardiomegaly | 11 (12) | 3 (3.2) | 5 (5) | 5 (5) |
| Syncope | 3 (6.5) | 1 (2.0) | 1 (2) | 1 (2) |
| Atrial fibrillation | 3 (4) | 0 | 8 (11) | 2 (3) |
| Family history | 4 (5) | 2 (3) | 1 (1) | 1 (1) |
| Palpitations | 0 | 0 | 3 (7) | 0 |
| Chest pain | 4 (13) | 0 | 2 (7) | 0 |
| No details | 4 (3) | 5 (4.2) | 14 (12) | 3 (2.5) |
| Miscellaneous | 9 (8) | 0 | 9 (8) | 3 (3) |
Other pathology
The most frequent non valve or LV pathologies were minor aortic dilatation of ≤40 mm (n = 64) and major dilatation >40 mm (n = 16), pulmonary hypertension with systolic pressure <35 mmHg (n = 21) or ≥35 mmHg (n = 70) and right ventricular impairment (n = 31). These were most common in suspected heart failure with 14 (19%) aortic dilatation, 44 (7%) pulmonary hypertension. Right ventricular impairment was most common in those with a cardiac history, four (23%). In those with a murmur there were six with previously undiagnosed atrial septal defects, four ventricular septal defects and one persistent ductus. For the other indications there were six further atrial septal defects, two ventricular septal defects, one Ebstein’s anomaly, one persistent ductus and two pericardial effusions.
DISCUSSION
Summary
Abnormalities likely to change management (Group 3 and 4) were found in 29% of all open access echocardiograms. The rate was significantly higher for suspected heart failure (41%) than for murmur (26%) as the indication. Significant valve disease was found in 18% with a murmur but also in 14% with suspected heart failure and 12% with atrial fibrillation.
Strengths and limitations
This is the largest series of open access echocardiograms analysed and the first occasion that the incidence of structural disease has been assessed according to the indication on the request. However there is no information about referrals for outpatient consultations. This means that it is not possible to test whether practices with low request rates were failing to detect structural heart disease or referring such patients directly to a cardiologist rather than for echocardiography.
Comparison with existing literature
Few previously published reports of open access services exist. Some describe services set up solely for heart failure.10–12 Those few with relatively unrestricted indications13–16 confirm that murmur and possible heart failure are the two most common reasons for referral while, not surprisingly, valve disease and LV systolic dysfunction are the two most common abnormalities detected. Valve disease is reported in 12–42% of cases in unrestricted open access services and LV systolic dysfunction in 9–30%.13,14,16 These incidences are far higher than expected with population screening1,3 and similar to those in hospital-based outpatient clinics15,17 suggesting that GPs are not overusing the service.
There has been recent interest in improving the detection of heart valve disease in the community.7 Judging the significance of a murmur is often difficult18,19 and the study showed the incidence of significant valve disease was comparable for the whole population (15%) as for those with a murmur (18%). Similarly in Holland,13 the incidence of moderate or severe valve disease was 31% with murmur, 23% with breathlessness and 28% with peripheral oedema. In a Scottish study,20 the incidence of all valve disease in patients with suspected heart failure was 46% which was substantially higher than the incidence of LV systolic dysfunction, 8%. The incidence of valve disease was similar to the EuroHeart Failure21 survey, but the study showed that the valve disease was primary in 58 (67%) and secondary in 28 (33%). The incidence of significant valve disease was less, 3–8% in echocardiography services set up for patients with possible heart failure.10–12 However these studies predated the use of B-type natriuretic peptide as a screen and many cases were thought not to have heart failure.
Implications for practice
Population screening has a low yield,1,3 but echocardiographic abnormalities are much more frequently shown in patients with a high likelihood of structural disease (Figure 1). It has been suggested7 that a programme of basic cardiac scans (‘Quick scans’) targeted at those at highest risk could reduce demand on echocardiography services while at the same time maximising the detection of structural disease requiring full standard echocardiography. Those at highest risk are those with acute cardiac symptoms22 a cardiac history, murmur, raised B-type natriuretic peptide level, and abnormal ECG (especially atrial fibrillation). Using this strategy in this study 267 (15%) of 1745 with a symptom or clinical evidence of a possible structural abnormality showed evidence of significant valve disease. Confining echocardiography to those with a murmur alone would have detected only 127 cases with valve disease. Similarly 139 (13%) of 1089 with a symptom or clinical evidence of a possible structural abnormality had LV systolic dysfunction compared to only 91 (15%) with an echocardiogram requested for suspected heart failure.
Some indications could have been triaged more effectively. For example an increased cardiothoracic ratio on the chest X-ray is not a good indication in the absence of other signs or symptoms suggesting heart disease.23 Perceived palpitation without a documented arrhythmia or clinical evidence of structural disease is not an appropriate indication for open access echocardiography.24 The request form available from the authors includes guidance on indications and this might improve the appropriateness of the requests. Most GP practices requested only a small number of studies. It is possible that outpatient appointments were being requested instead of open access echocardiograms for patients with obvious disease. However the current authors suspect that in many of these practices, the detection of structural cardiac disease remains suboptimal. Failure to detect and refer aortic stenosis is thought to be the main cause of the major variation between expected and observed rates of aortic valve replacement in the UK25 and within London. Aortic valve replacement rates are high in Enfield and Camden but low in Ealing and Brent.25
The main objective of early open access services was to allow suitably qualified and interested GPs to manage heart failure in the community.6 However many GPs have difficulty interpreting echocardiography reports6 and a high incidence of abnormalities is found which underlines the need for echocardiography to link with clinical cardiac services. About a half of all reported ‘open access’ services offer advice from a cardiologist26 and are closer to a one stop cardiology outpatient appointment than a true open access echocardiography service.
There are other models of providing this clinical link. The current authors have established a sonographer-led open access murmur clinic which triages patients according to result for hospital or community care. Direct community echocardiography occurs in some UK centres8 and was described in a US study.27 A project in Newcastle has shown that domiciliary echocardiography is feasible for elderly patients.28 It is likely that direct community echocardiography will expand with the current changes within the NHS. It is essential that community services remain within a global clinical framework capable of providing back up echocardiography using high-end machines and access to specialist clinical opinions. Some of the abnormalities detected in the study required immediate clinical action. It is also vital that the echocardiograms are performed to a good standard with appropriately qualified and trained staff, quality assurance, and archiving.29
Open access echocardiograms are often abnormal but structural disease may not be suspected from the clinical request. Uptake by individual practices is patchy. A targeted expansion of echocardiography in patients with a high likelihood of disease is therefore likely to increase the detection of clinically important pathology.
Funding
None
Ethical approval
No ethics committee application was required. The study was approved as a Trust (Guy’s and St Thomas’ NHS Trust) clinical evaluation (3951).
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: www.bjgp.org/letters
REFERENCES
- 1.Nkomo VT, Gardin JM, Skelton TN, et al. Burden of valvular heart diseases: a population-based study. Lancet. 2006;368:1005–1011. doi: 10.1016/S0140-6736(06)69208-8. [DOI] [PubMed] [Google Scholar]
- 2.Dickstein K, Cohen-Solal A, Filippatos G, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008. Europ Heart J. 2008;29(19):2388–2442. doi: 10.1093/eurheartj/ehn309. [DOI] [PubMed] [Google Scholar]
- 3.Lindekleiv H, Lochen M-L, Mathiesen EB, et al. Echocardiographic screening of the general population and long-term survival. A randomized clinical study. JAMA Int Med. 2013 doi: 10.1001/jamaunternmed.2013.8412. [DOI] [PubMed] [Google Scholar]
- 4.McDonald, Daly, Jelinek, et al. Opening Pandora’s box: the unpredictability of reassurance by a normal test result. BMJ. 1996;313:329–332. doi: 10.1136/bmj.313.7053.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stoate HG. Can health screening damage your health? J R Coll Gen Pract. 1989;39:193–195. [PMC free article] [PubMed] [Google Scholar]
- 6.Fuat A, Pali A, Hungin S, Murphy JJ. Barriers to accurate diagnosis and effective management of heart failure in primary care: qualitative study. BMJ. 2003;326:196–201. doi: 10.1136/bmj.326.7382.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arden C, Chambers J, Ray S, et al. Can we improve the detection of heart valve disease? Heart. 2013 doi: 10.1136/heartjnl-2013-304223. [DOI] [PubMed] [Google Scholar]
- 8.Chambers J, Fox K, Senior R, Nihoyannopoulos P. Echocardiography within the British Isles: a national survey. Brit J Cardiol. 2007;14:99–101. [Google Scholar]
- 9.d’Arcy JL, Prendergast BD, Chambers JB, et al. Valvular heart disease: the next cardiac epidemic. Heart. 2011;97:91–93. doi: 10.1136/hrt.2010.205096. [DOI] [PubMed] [Google Scholar]
- 10.Francis CM, Caruana L, Davie AP, et al. Open access echocardiography in management of heart failue in the community. BMJ. 1995;310:634–636. doi: 10.1136/bmj.310.6980.634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Murphy JJ, Frain JP, Ramesh P, et al. Open-access echocardiography to general practitioners for suspected heart failure. Br J Gen Pract. 1996;46:475–476. [PMC free article] [PubMed] [Google Scholar]
- 12.Lindsay MM, Goodfield NE, Hogg KJ, Dunn FG. Optimising direct access echo referral in suspected heart failure. Scot Med J. 2000;45:43–44. doi: 10.1177/003693300004500204. [DOI] [PubMed] [Google Scholar]
- 13.Van Heur LM, Baur LH, Tent M, et al. Evaluation of an open access echocardiography service in the Netherlands: a mixed methods study of indications, outcomes, patient management and trends. BMC Health Serv Res. 2010;10:37. doi: 10.1186/1472-6963-10-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sim MFV, Davies J. Open access echocardiography clinic – Newport experience. Br J Cardiol. 1998;5:286–290. [Google Scholar]
- 15.Mahadevan VS, Earley M, McClements B. Open access echocardiography has diagnostic yield similar to outpatient echocardiography and is highly rated by general practitioners and patients. Int J Cardiol. 2005;99:389–393. doi: 10.1016/j.ijcard.2004.01.042. [DOI] [PubMed] [Google Scholar]
- 16.Rao A, Henton D, Walsh J. Evolving trends in open access echocardiography experience over eight years. http://www.priory.com/med/echo.htm (accessed 6 Jan 2014). [Google Scholar]
- 17.Bridgman PG, Ashrafi AN, Mann S, Whalley GA. Survey of clinical echocardiography in New Zealand (ACANZ) NZ Med J. 2008;121:34–44. [PubMed] [Google Scholar]
- 18.Roldan CA, Shively BK, Crawford MH. Value of cardiovascular physical examination for detecting valvular heart disease in asymptomatic subjects. Am J Cardiol. 1996;77:1327–1331. doi: 10.1016/s0002-9149(96)00200-7. [DOI] [PubMed] [Google Scholar]
- 19.Mangione S, Nieman LZ. Cardiac auscultatory skills of internal medicine and family practice trainees. A comparison of diagnostic proficiency. JAMA. 1997;278:717–722. [PubMed] [Google Scholar]
- 20.Jeyaseelan S, Goudie BM, Pringle SD, et al. A critical re-appraisal of different ways of selecting ambulatory patients with suspected heart failure for echocardiography. Eur J Heart Failure. 2007;9:55–61. doi: 10.1016/j.ejheart.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 21.Cleland JG, Swedberg K, Follath F, et al. The EuroHeart Failure survey programme – a survey on the quality of care among patients with heart failure in Europe. Part 1: patient characteristics and diagnosis. Eur Heart J. 2003;24:442–463. doi: 10.1016/s0195-668x(02)00823-0. [DOI] [PubMed] [Google Scholar]
- 22.Kirkpatrick JN, Davis A, DeCara JM, et al. Hand-carried cardiac ultrasound as a tool to screen for important cardiovascular disease in an underserved minority health care clinic. JASE. 2004;17:399–403. doi: 10.1016/j.echo.2004.01.016. [DOI] [PubMed] [Google Scholar]
- 23.Wingate-Samuels L, Javaid J, Chambers J. Echocardiography is not indicated for an enlarged cardiothoracic ratio. Br J Cardiol. 2013;20:149–150. [Google Scholar]
- 24.Douglas PS, Garcia MJ, Haines DE, et al. ACCF/ASE/AHA/ASNC/HFSA/HRS/SCAI/SCCM/SCCT/SCMR 2011. Appropriate use criteria for echocardiography. JACC. 2011;57:1126–1166. [Google Scholar]
- 25.Bridgewater B, Kinsman R, Walton P, et al. Demonstrating quality: the sixth National Adult Cardiac Surgery database report. Henley-on-Thames, UK: Dendrite Clinical Systems Ltd; 2009. [Google Scholar]
- 26.Khunti K. Systematic review of open access echocardiography for primary care. Europ J Heart Failure. 2004;6:79–83. doi: 10.1016/j.ejheart.2003.10.002. [DOI] [PubMed] [Google Scholar]
- 27.Gilman G, Lutzi CA, Daniels BK, et al. The architecture of a mobile outreach echocardiography service. JASE. 2006;19:1526–1528. doi: 10.1016/j.echo.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 28.Yousaf F, Collerton J, Kingston A, et al. Prevalence of left ventricular dysfunction in a UK community sample of very old people: the Newcastle 85+ study. Heart. 2012;98:1418–1423. doi: 10.1136/heartjnl-2012-302457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Saltissi S, Chambers J. Quality issues for echocardiography in the community. Heart. 1998;80(Suppl 1):S9–S11. doi: 10.1136/hrt.80.2008.9s. [DOI] [PMC free article] [PubMed] [Google Scholar]


