INTRODUCTION
Premature mortality in people with intellectual disability (ID; also referred to as learning disability) is significant and to some extent, avoidable. In the 2013 report Confidential Inquiry into Premature Deaths of People with Learning Disabilities people with ID tended to die from causes potentially amenable to change by improvement of quality of health care:
‘All aspects of care provision, planning, coordination and documentation were significantly less good… than for comparators.’1
A recent article in the BJGP addresses acute care in this group of vulnerable patients.2 This article addresses how primary care teams may improve maintenance care to reduce the health inequality gap that these patients may experience.
Over the past decade, GP practices have taken on increasing responsibilities for the care of people with ID. Two principal reasons are the closure of long-stay ID institutions and relocation of their patients to the community. Many patients are now settled in residential care homes and others in supervised tenancies. Also, with recent medical technological advances more people with intellectual disabilities are living longer. This means the total prevalence for ID in the general population, including those with mild ID is 2.5%, but the prevalence for those likely to have been identified on GP practice registers (those with moderate, severe and profound ID) is now 0.45%. Should this mean a change in the role of the specialist nursing and psychiatric services? Closer working relationships and collaboration could improve communications and reduce duplication of clinical monitoring.
By definition people with ID have impaired social functioning and limited cognitive ability that has developed before the age of 18 years.3 It follows that, in addition to socioeconomic determinants of health inequality, people with ID are likely to be at additional disadvantage competing for primary care services. This is due to a mixture of other health inequality determinants such as access, physiological differences, and comprehension difficulties, which are likely to include cognitive and communication problems.
WHY REDUCING THE HEALTH INEQUALITY GAP IS IMPORTANT
There may be accessibility problems for people with ID, for example they may be unable to phone to make appointments unaided; be unable to read appointment letters and other correspondence; be dependent on helpers for transport to the surgery; and may be wheelchair dependent. About one-quarter of this population have Down’s syndrome (DS), which may have a number of physiological associated conditions, such as short stature, congenital heart problems, undiagnosed diabetes, early onset dementia, thyroid problems, and early menopause. Patients with DS also often have indistinct speech and hearing impairment which is sometimes associated with impacted ear wax. People with other syndromes are likely to have particular problems; for example, patients with Fragile X syndrome are often restless in the waiting room due to social anxiety; a feature of the condition. They may have difficulties with patient call systems and therefore appreciate being personally invited into the consulting room by the clinician. Along with comprehension difficulties, many people with ID may be unable to read or understand standard advice leaflets about various conditions, and they are particularly likely not to trust doctors or other clinicians they have not met before.
Some of these factors, or potential factors, may increase health inequality, if allowance (reasonable adjustment) is not made for the additional needs of people with intellectual disabilities. Some of the above considerations may apply to other disadvantaged and/or minority groups of patients.
Figure 1 shows how widening of the health inequality gap might occur, and as a generalisation (other things being equal) more able individuals could be more likely to have their clinical needs met from their primary care service than those who have a limited intellectual ability. The slope of the playing field (so to speak) is inclined to the disadvantage of those with ID.
Figure 1.
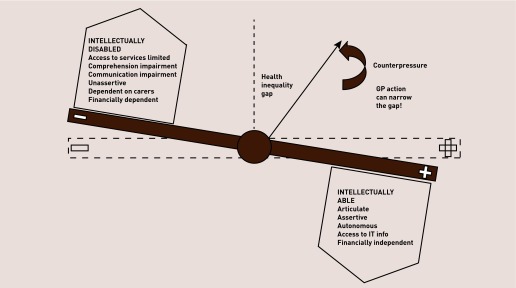
Consulting room dynamics; possible different attributes between patients with high and low intellectual ability that may widen the health inequality gap. Note: this presumes various empowerments and/or advantages on the intellectual ability side of the fulcrum (+), which may or may not apply. On the intellectual disability side (–) patients with intellectual disabilities have considerably less choice in reducing their disadvantages.
HOW GPs CAN NARROW THE GAP
Reasonable adjustments include planning additional time to spend with these patients. Flagging allows reception staff to offer double appointments. Appropriate advice and information for a range of conditions is available via easyhealth, (www.easyhealth.org.uk; general medical conditions), Contact a Family, (www.cafamily.org.uk/medical-information; underlying aetiology and syndromes), and several other organisations.
Of all interventions, an annual check is probably the most important, and the first, which may be at transition, should be the most thorough with abnormal findings on enquiry and physical examination recorded as baseline findings. Annually, such a structured comprehensive ‘MOT’ in protected time is known to identify twice as many clinical needs as standard GP care for a whole year.4 The actual leading clinical needs that require addressing in people with ID are different from a comparable population with no disability, and tend to be about physical function, particularly sensory, gastrointestinal, and seizure control.5,6 Participant’s experience of primary care services generally, and health checks in particular, are positive.7 It is believed to be relatively inexpensive,8 and the main costs of GP and nurse time are largely offset by reimbursement through the Directed Enhanced Service (DES) for adults. It may be possible to arrange for specialist learning disability nurse input, which will improve continuity and communication for the benefit of all.
Currently only just over one-half of those entitled receive an annual health check. The results of uptake for 2012–2013 (the last annual cycle under the aegis of primary care trusts in England) shows that 52.0% received health checks. The overall number of checks rose from 86 134 in 2011–2012 to 92 329 in 2012–2013 due to an increase in the numbers identified as eligible. In 2011–2012, on the revised figures, 52.8% of those then eligible had a health check. There is considerable variation in uptake. For example, only 4 out of 10 eligible people in the West Midlands SHA had checks, whereas 6 out of 10 had checks in the East Midlands. Variations are more pronounced at PCT levels.9
Why has there been consistently low uptake in some localities? Did the patients actively choose not to attend? Did their carers decide for them? Or did they not receive an invitation in the first place? Or was their GP not persuaded of the benefits to the patient of health checks, or unwilling to receive training and organise the appointments, as the returns to the practice were too small? This might apply if the practice had comparatively few adults with intellectual disabilities. Where low uptake, and therefore comparative inequality, is identified, clinical commissioning groups need to address the situation in line with public sector equality duty (Equality Act 2010).
So the first thing from a general practice perspective that would narrow the health inequality gap, and improve the uptake towards the target of 90%, would be for more GPs to sign up to the DES and more of the eligible population to have high quality health checks. These should identify opportunities for health improvement to be captured in a health action plan.
CONCLUSION
Further advice by GPs about the care of people with ID are to be found in two recent RCGP publications.10,11 In offering health checks to this vulnerable group of patients, the authors are convinced that we, GPs, will make a difference in improving health and reducing unnecessary mortality for people with ID.
In addition to signing up and committing to annual health checks for their patients, a number of GP practices have also put their names to the Mencap ‘Getting it right Charter’ (www.mencap.org.uk/campaigns/take-action/getting-it-right). You are invited to join them, if you haven’t already.
Provenance
Commissioned; not externally peer reviewed.
REFERENCES
- 1.Heslop P, Blair P, Fleming P, et al. Confidential Inquiry into premature deaths of people with learning disabilities (CIPOLD). Final Report. Bristol: Norah Fry Research Centre; 2013. http://www.bris.ac.uk/cipold/fullfinalreport.pdf (accessed 7 Jan 2013). [Google Scholar]
- 2.Heslop P, Hoghton M, Blair P, et al. The need for FASTER CARE in the diagnosis of illness in people with intellectual disabilities. Br J Gen Pract. 2013;63:661–662. doi: 10.3399/bjgp13X675593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Department of Health . Valuing people; a new strategy for learning disability for the 21st Century. London: DH; 2001. Cm 5086. [PMC free article] [PubMed] [Google Scholar]
- 4.Cooper S-A, Morrison J, Melville C, et al. Improving the health of people with intellectual disabilities: outcomes of health screening programme after 1 year. J Intellect Disabil Res. 2006;50(9):667–677. doi: 10.1111/j.1365-2788.2006.00824.x. [DOI] [PubMed] [Google Scholar]
- 5.Cooper S-A, Melville C, Morrison J. People with intellectual disabilities; their health needs differ and need to be recognised and met. BMJ. 2004;329:414. doi: 10.1136/bmj.329.7463.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chauhan U, Kontapolis E, Campbell S, et al. Health checks in primary care for adults with intellectual disabilities: how extensive should they be? J Intellect Disabil Res. 2010;54(6):479–486. doi: 10.1111/j.1365-2788.2010.01263.x. [DOI] [PubMed] [Google Scholar]
- 7.Perry J, Felce D, Kerr M, et al. Contact with primary care: the experiences of people with intellectual disabilities. J Appl Res Intellect Disabil. 2013 doi: 10.1111/jar.12072. [DOI] [PubMed] [Google Scholar]
- 8.Romeo R, Knapp M, Morrison J, et al. Cost estimation of a health check intervention for adults with intellectual disabilities in the UK. J Intellect Disabil Res. 2009;53(5):426–39. doi: 10.1111/j.1365-2788.2009.01159.x. [DOI] [PubMed] [Google Scholar]
- 9.Glover G, Niggebrugge A. The uptake of health checks for adults with learning disabilities 2008/9 to 2012/13. http://www.ihal.org.uk/gsf.php5?f=17761 (accessed 7 Jan 2013) [Google Scholar]
- 10.Hoghton M, the RCGP learning disability group . A step by step guide for GP practices: annual health checks for people with a learning disability. London: RCGP; 2010. [Google Scholar]
- 11.Martin G. Caring for patients with intellectual disabilities. In: Gill P, Wright N, Brew I, editors. Working with vulnerable groups: a clinical handbook for GPs. London: RCGP; 2014. in press. [Google Scholar]


