Abstract
Background
Inattention to symptoms of mental disorders and substance abuse in patients with HIV/AIDS and other at-risk groups, may lead to irreversible damages. The purpose of this study was to compare the psychopathological dimensions in substance abusers with and without HIV/AIDS and healthy matched groups.
Methods
In a cross-sectional and analytical study, selected samples (by available, consecutive, and objective methods) were 43 HIV-positive substance abusers, 49 HIV negative substance abusers under methadone maintenance therapy (MMT) in the counseling clinic of Behavioral Diseases and Addiction Abandonment, and 45 ordinary individuals. All of them were evaluated by matched confounding variables via Symptom Checklist-90-Revised (SCL-90-R).
Findings
Results indicated a significant difference between these groups in the Global Severity Index (GSI), Positive Symptom Distress Index (PSDI), and Positive Symptom Total (PST) (P < 0.001). Two by two the comparison of the three groups from psychopathological dimensions revealed that substance abusers with HIV/AIDS persistently suffer more mental problems in all dimensions compared with healthy individuals (P < 0.05). In addition, in comparison with HIV negative substance abusers, they also suffer more mental problems in other dimensions, including somatization, interpersonal sensitivity, depression, anxiety, phobia, and psychoticism (P < 0.05). Yet, the difference in paranoid ideation, hostility, and obsessive-compulsive cases was insignificant. Two by two, the comparison between healthy individuals and substance abusers without HIV/AIDS showed higher levels of depression and psychoticism in substance abusers (P < 0.05), but no difference in other dimensions.
Conclusion
Comorbidity of substance abuse and HIV diagnosis intensify mental disorder symptoms. Moreover, lack of prevention and implementation of appropriate psychological and psychiatric interventions after substance abuse and HIV lead to extended establishment of mental disorder symptoms.
Keywords: Substance abuse, HIV/AIDS, Psychopathology, SCL-90-R
Introduction
Despite the remarkable advances in medicine, AIDS is still killing millions of people every day and HIV is increasingly spreading worldwide. This biopsychosocial phenomenon rapidly affects social structures and individual entity.1 HIV and AIDS should not be considered as a simple health problem, since social and economic complications of the disease has such a wide range of dimensions that make it difficult to compare with other present epidemic diseases.
AIDS is beyond just clinical manifestations (e.g. skin infections, tuberculosis, bacterial pneumonia, thrombophlebitis, hepatitis B and C, and etcetera), which co-occur with the progression of HIV infection and damage to cellular immune system.2 Evidences have shown that these patients are affected by a wide range of mental disorders, and nearly 20% to 59% of HIV-infected people suffer from one or more mental disorders, which is 2 or 3 times general population.3-9
In this regard, substance use disorder is the most common comorbid in mental disorders of HIV-infected patients.5,10 Prior researches have associated substance use, especially in the form of injection, with some HIV epidemics around the world. The prevalence and frequency of medical and mental disorders are higher in HIV-infected substance users. Consequently, due to the large number and wide range of these dual disorders, diagnosis and treatment in these patients become more complicated, and result in a large number of challenges for a thorough care.10 For instance, in some studies, the rate of substance use disorder was 70% or more and the it prevalence considering age and gender may be at least 3 times higher than expected.11,12 Moreover, some studies revealed that the onset of mood and substance use disorders was prior to the possible time of acquiring HIV infection.13,14 Moreover, mental disorders in HIV-infected individuals is accompanied with a drop in quality of life score and reduction of adherence or compliance to antiretroviral therapy.15-18
The influence of HIV on the young population of Iran is becoming obvious, especially during recent years. According to the latest report by the Ministry of Health and Medical Education (Iran), the number of HIV-infected people is 23,125 (22/June/2011). 4311 people diagnosed with AIDS have died, 46.5% were between 25-34 years of age.19 Therefore, like other countries, HIV infection involves the young population of Iran in respect to their reproduction and economical activities, and social communication.
However, without exact the diagnosis and efficient treatment for mental disorders one should not expect a reduction in the disastrous outcome of HIV/AIDS and its transmission to other people or substance users. Promoting public awareness leaning on local researches may help therapists, who first visit these patients, to offer successful care. Besides, there are a limited number of data on recognition of mental disorders in substance users with and without HIV/AIDS and their healthy matched group for quick reference and treatment. Thus, the main goal of this research is to identify the difference between the 3 groups in respect to the diverse dimensions of psychopathology. Therefore, understanding psychopathology in at-risk groups may show the necessity for revealing fundamental data in this regard, prioritizing the symptoms of mental disorder, and precise program planning to offer health and mental services.
Methods
Research plan
This was a cross-sectional study. The medical ethics and the plan were approved by the Research Council of Guilan University of Medical Sciences (GUMS), Iran [NO. P/3/132/10617 approved on 8/June/2010]. The subjects were the following groups: A) confirmed HIV-infected substance users under highly active antiretroviral therapy (HAART) B) substance users without HIV/AIDS C) healthy matched group for both A and B groups with no special morbidity. All participants of group A were under supervision of the Research Council of GUMS in 2010 and had record files. Furthermore, group B with substance abuse history referred to the same behavioral Disease Counseling Clinic, a Drop in Center (DIC), and two other drug abandonment centers in Rasht, Iran. Group C consisted of healthy individuals who were relatives of patients in A and B groups and the staff who worked with these patients.
Participants
The sample size was 43 individuals in each group and 129 subjects in total for 3 groups with 99% confidence interval (CI) and considering 95% statistical power based on sample size determination table for variance analysis by Bratcher et al.20 In the sampling procedure, from June to September 2010, first substance users with HIV/AIDS were included in the project by convenience sampling method, and then, substance users without HIV/AIDS by consecutive method. All patients were referred the medical centers due to a history of risky behavior (e.g. drug injection, sharing syringe, unsafe sexual behavior, and etcetera), or for a free voluntary counseling and testing (VCT) and Methadone Maintenance Therapy (MMT). Shortly before starting, and during the project, damage reduction and care program (pre-test counseling, giving condom and syringe, and etcetera) were performed. Before HIV diagnostic test, they were assured that the test is safe and free. Blood samples (2cc) were sent to Guilan Blood Transfusion Organization for enzyme-linked immunosorbent assay (ELIZA) by Bio-Rad kit with confirmatory western blot assay by Innogenetic kit. Finally, those who were HIV-positive were tested for CD4 count of T-helper lymphocytes in GUMS. The number of CD4 is a good index to determine the severity of disease progression and plays a key role in cellular defense system; the less the count, the more vulnerable the body to other infections.21 The healthy group were selected by purposive sampling method out of patients' acquaintances, staff, and service workers of hygiene and drug abandonment centers. The reason for using non-random sampling method in substance abusers without HIV/AIDS and the healthy group was to match HIV/AIDS substance abusers more accurately according to age, gender, marital status, education level, and place of living (urban, rural).
The inclusion criteria for the HIV/AIDS group were two positive ELISA serum tests and a positive western blot assay plus AIDS symptoms determined and recorded in their file by a specialist and other experts. In the non-HIV/AIDS substance abusers group, their HIV tests were negative and were added to their record file. For the healthy matched group "no history of substance abuse" was considered as a criterion. Moreover, inclusion criteria for all 3 groups were being above 18 years of age, acceptable understanding of the procedure, and no acute psychiatric disease (e.g. schizophrenia) and developmental-neuronal disorders (e.g. retardation, brain damage, dementia, and other cognitive disorders). A written consent form was obtained from each participant. The exclusion criteria were identified by examining and interviewing patients, and reviewing their files by a doctor and specialist in behavioral diseases in the center.
Measures
Symptom checklist-90-Revised (SCL-90-R): This test is a powerful self-report tool for psychopathological assessment specifically intended for those physical and psychological disorders recently experienced by respondents. The 90 items of this test describe symptoms most experienced and reported by medical and psychiatric patients. The first version of this test was introduced by Derogatis et al. in 1973, followed by a revision based on clinical experiences and psychometric analysis that created the final version.22,23 The 90 items of this test include 9 dimensions; somatization, obsessive-compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobia, paranoid ideation, and psychoticism. All given answers to the items are placed in a 5-degree scale (0 = none, 1 = a little, 2 = to some extent, 3 = very much, and 4 = extremely).24 It takes about 10-15 minutes to answer this questionnaire.
Grading and interpretation of the results are done based on the Global Severity Index (GSI), Positive Symptom Distress Index (PSDI), and Positive symptom Total (PST).24 Derogatis has utilized the internal reliability and retest reliability to assess the reliability of the 9 dimensions of this test. Internal reliability of SCL-90-R for 9 dimensions was satisfying and the most internal consistency was about depression with 0.90 and the least was about psychoticism with 0.77. Retest reliability varied between 0.78 to 0.90.25 Similarly, Bagheri Yazdi et al. reported a 0.97 reliability coefficient and 0.94, 0.98, and 0.96 for sensitivity, specificity, and efficiency, respectively.26 They suggested SCL-90-R to be used as a diagnostic screening tool in epidemiologic studies of mental disorders. In the current project, based on a survey by Noorbala et al., who calculated cut-off point of SCL-90-R test to be 0.7 in Iran based on GSI coefficient, individuals with GSI > 0.7 are considered as having mental disorder.27 Previously, SCL-90-R was successfully applied in researches related to mental symptoms assessment and in patients with HIV/AIDS.9,28-31 Mohseni and Hedayati-Moghadam et al. used the same cut-off point (0.7) to determine the extent of mental disorders in HIV/AIDS infected patients in Iran.9,28
Furthermore, a researcher-made questionnaire was used to record demographic characteristics for all 3 groups, and some clinical information such as present status of drug use, HIV infection status of spouse, history of syringe addiction, and number of CD4 lymphocytes in substance abusers with and without HIV/AIDS.
Project procedure
The interviews were performed by two MA psychologists; after getting to know the participants in the sampling setting they explained the general aim of the research to them. Considering the low literacy of some subjects, all questions were read and their verbal responses registered to equalize the test completion method. They were also assured that all information would be confidential and published as the total result. They were also informed that they could quit the study whenever they decided and it would not negatively affect the diagnostic and treatment procedure.
Statistical Analysis
After scoring, data of the 3 subject groups were analyzed by SPSS 16.0 statistical package (SPSS Inc., Chicago, IL., USA) using descriptive statistic indices, Student’s independent t-test for two-group comparisons, χ2 to compare the observed frequency of suspected cases for mental disorders, and one way Analysis Of Variance (ANOVA) to exhibit the main effects of group membership (substance abusers with HIV/AIDS, substance abusers without HIV/AIDS, and their matched group). Gabriel post-hoc test was also utilized to determine the significant difference between the mean of the 3 groups' scores.
Results
Out of the 150 distributed questionnaires, data of 43 HIV/AIDS substance abusers, 49 non-HIV/AIDS substance abusers, and 45 healthy matched individuals were collected. As is shown in table 1, the results of ANOVA and χ2 show no significant difference between likely confounding variables (P > 0.05).
Table 1.
Demographic characteristics of participants based on matched variables (n = 137)
| Quantitative matched variables* | HIV positive | HIV negative | Healthy matched | P |
|---|---|---|---|---|
|
| ||||
| (n = 43) | (n = 49) | (n = 45) | ||
| Age (year) | 33.81 ± 7.76 | 34.96 ± 9.80 | 32.18 ± 10.54 | NS |
| Education (years) | 8.04 ± 2.92 | 7.40 ± 1.88 | 9.93 ± 2.34 | NS |
|
| ||||
| Qualitative matched variables† | n (%) | n (%) | n (%) | |
|
| ||||
| Gender | ||||
| Male | 38 (88.3) | 44 (89.8) | 36 (80.0) | NS |
| Female | 5 (11.7) | 5 (10.2) | 9 (20.0) | |
| Marital status | ||||
| Single | 20 (46.5) | 27 (55.1) | 20 (44.4) | |
| Married | 17 (39.5) | 18 (36.7) | 25 (55.6) | NS |
| Divorced | 4 (9.3) | 3 (6.1) | 0 (0) | |
| Widow | 2 (4.7) | 1 (2.1) | 0 (0) | |
| Living place | ||||
| Rural | 37 (86.1) | 41 (83.7) | 42 (93.4) | NS |
| Urban | 6 (13.9) | 8 (16.3) | 3 (6.6) | |
ANOVA test
χ2 test; NS: Not significant
The mean of CD4 lymphocyte count in confirmed HIV+ substance abusers was 377.74 ± 202 (from 36 to 830). Muma et al. indicated lymphocyte count (in 1 mm2 of blood sample) < 200 CD4 as inclusion criterion for AIDS phase.21 In our study, 7 patients (16.3%) had entered this phase. Mean of positive HIV period was 20 ± 24 months based on medical records. 37 (86.0%) of the 43 HIV/AIDS substance abusers were under MMT and 34 (79.1%) reported drug injection history. In addition, 46 (93.9%) of the 49 non- HIV/AIDS substance abusers were under MMT, and 29 (59.2%) reported drug injection history. The results of χ2 revealed that HIV/AIDS substance abusers and non- HIV/AIDS substance abusers were significantly different in drug injection history (χ2 = 4.20, df = 1, P = 0.041). HIV/AIDS substance abusers had significantly higher rate of drug injection history (79.1% vs. 59.2 %).
The results of this study showed that there is no significant difference in Methadone consumption period between HIV and non-HIV substance abusers (t = 1.09, df = 90, P = 0.280). However, there is a significant difference in the results of independent t-test about imprisonment period. In other words, HIV/AIDS infected substance abusers are on average imprisoned twice more than the other group (t = 2.57, df = 90, P = 0.012).
As shown in table 2, in comparison analysis of mental disorder prevalence in studied groups based on cut-off point, general symptom index (GSI) has been considered as 0.7. 88.4% of HIV/AIDS substance abusers, 75.5% of non-HIV/AIDS substance abusers, and 53.0% of their healthy matched group that showed mental disorder symptoms are significant based on χ2 (χ2 = 13.87, df = 2, P < 0.001).
Table 2.
Mental disorders in the 3 groups of substance abusers with and without HIV/AIDS and healthy matched group
| Mental disorder status | Yes | No | χ2 | P | |
|---|---|---|---|---|---|
| Groups |
|
||||
| n (%) | n (%) | ||||
| HIV positive (n = 43) | 38 (88.4) | 5 (11.6) | 13.87 | < 0.001 | |
| HIV negative (n = 49) | 37 (75.5) | 37 (24.5) | |||
| Healthy matched (n = 45) | 24 (53.3) | 24 (46.7) | |||
Table 3 shows the number distribution (Mean ± SD) and results of ANOVA of subscales of the SCL-90-R test, representing diverse mental aspects of the psychopathology of HIV/AIDS and non-HIV/AIDS groups, and their healthy matched group.
Table 3.
Results of Analysis of Variance (ANOVA) of psychopathology dimensions in the 3 groups
| Groups | HIV positive | HIV negative | Healthy matched | F (134,2) | P | |
|---|---|---|---|---|---|---|
|
|
||||||
| (n = 43) | (n = 49) | (n = 45) | ||||
| SCL-90-R dimensions |
|
|||||
| Mean ± SD | Mean ± SD | Mean ± SD | ||||
| Somatization | 17.76 ± 11.11 | 10.65 ± 8.36 | 9.18 ± 5.19 | 12.79 | < 0.001 | |
| Obsessive-compulsive | 16.32 ± 8.55 | 10.65 ± 8.36 | 9.22 ± 6.31 | 9.82 | < 0.001 | |
| Interpersonal sensitivity | 16.32 ± 8.55 | 11.94 ± 7.67 | 8.58 ± 5.42 | 14.83 | < 0.001 | |
| Depression | 25.23 ± 12.70 | 16.92 ± 10.31 | 10.98 ± 7.41 | 21.09 | < 0.001 | |
| Anxiety | 15.18 ± 9.06 | 10.33 ± 7.02 | 7.29 ± 5.60 | 12.97 | < 0.001 | |
| Hostility | 7.74 ± 6.11 | 5.94 ± 4.35 | 4.98 ± 4.17 | 3.57 | < 0.031 | |
| Phobia | 7.77 ± 5.63 | 4.69 ± 4.14 | 3.11 ± 2.81 | 13.16 | < 0.001 | |
| Paranoid ideation | 11.72 ± 5.43 | 9.28 ± 5.62 | 7.04 ± 4.93 | 8.41 | < 0.001 | |
| Psychoticism | 15.56 ± 8.42 | 10.71 ± 6.72 | 4.95 ± 5.74 | 25.21 | < 0.001 | |
| Global Severity Index (GSI) | 1.62 ± 0.76 | 1.13 ± 0.61 | 0.81 ± 0.47 | 19.12 | < 0.001 | |
| Positive Symptom Total (PST) | 58.09 ± 19.10 | 46.69 ± 17.61 | 41.58 ± 18.25 | 9.37 | < 0.001 | |
| Positive Symptom Distress Index (PSDI) | 2.42 ± 0.59 | 2.08 ± 0.50 | 1.71 ± 0.43 | 21.20 | < 0.001 | |
As seen in table 3, there is a significant difference between these 3 groups in all psychopathological dimensions (i.e. the ratio of calculated F by free grades is 2 and 134) and all subscales of SCL-90-R test (P < 0.05). Table 4 also presents the results of two-by-two mean comparison of groups using Gabriel post-hoc test, the power of which is good particularly in discriminating unequal groups with different sample sizes.32
Table 4.
Results of two-by-two mean comparison of groups by Gabriel post-hoc test in different dimensions of psychopathology
| Groups | Mean difference |
Mean | ||
|---|---|---|---|---|
| Variables SCL-90-R dimensions | A | B | ||
| Somatization | A: HIV positive | - | - | 17.76 |
| B: HIV negative | 7.11*** | - | 10.65 | |
| C: Healthy matched | 8.59*** | 1.47 | 9.18 | |
| Obsessive-compulsive | A: HIV positive | - | - | 16.32 |
| B: HIV negative | 3.75* | - | 12.57 | |
| C: Healthy matched | 7.10*** | 3.35 | 9.22 | |
| Interpersonal sensitivity | A: HIV positive | - | - | 16.91 |
| B: HIV negative | 4.97* | - | 11.94 | |
| C: Healthy matched | 8.33*** | 3.36 | 8.58 | |
| Depression | A: HIV positive | - | - | 25.23 |
| B: HIV negative | 8.31** | - | 16.92 | |
| C: Healthy matched | 14.25*** | 5.94* | 10.98 | |
| Anxiety | A: HIV positive | - | - | 15.18 |
| B: HIV negative | 4.86** | - | 10.33 | |
| C: Healthy matched | 7.90*** | 3.04** | 7.29 | |
| Hostility | A: HIV positive | - | - | 7.74 |
| B: HIV negative | 1.81 | - | 5.94 | |
| C: Healthy matched | 2.77* | 0.96 | 4.98 | |
| Phobia | A: HIV positive | - | - | 7.77 |
| B: HIV negative | 3.07** | - | 4.69 | |
| C: Healthy matched | 4.66*** | 1.58 | 3.11 | |
| Paranoid ideation | A: HIV positive | - | - | 11.72 |
| B: HIV negative | 2.43 | - | 9.28 | |
| C: Healthy matched | 4.68*** | 2.24 | 7.04 | |
| Psychoticism | A: HIV positive | - | - | 15.56 |
| B: HIV negative | 4.84** | - | 10.71 | |
| C: Healthy matched | 10.60*** | 5.76*** | 4.95 | |
| Global Severity Index (GSI) | A: HIV positive | - | - | 1.62 |
| B: HIV negative | 0.49** | - | 1.13 | |
| C: Healthy matched | 0.82** | 0.32* | 0.81 | |
| Positive Symptom Total (PST) | A: HIV positive | - | - | 58.09 |
| B: HIV negative | 11.40** | - | 46.69 | |
| C: Healthy matched | 16.51*** | 5.12 | 41.58 | |
| Positive Symptom Distress Index (PSDI) | A: HIV positive | - | - | 2.42 |
| B: HIV negative | 0.33** | - | 2.08 | |
| C: Healthy matched | 0.71*** | 0.38** | 1.71 | |
P < 0.05
P < 0.01
P < 0.001
Gabriel post-hoc test showed that HIV/AIDS substance abusers report significantly more symptoms and show a more acute mental status in all dimensions compared to their healthy matched group. This is also true in all psychopathological dimensions, except hostility and paranoid ideation, compared to non-HIV/AIDS substance abusers. There was also a significant difference in depression, anxiety, psychoticism, GSI, and PSDI between substance abusers without HIV/AIDS and the healthy matched group.
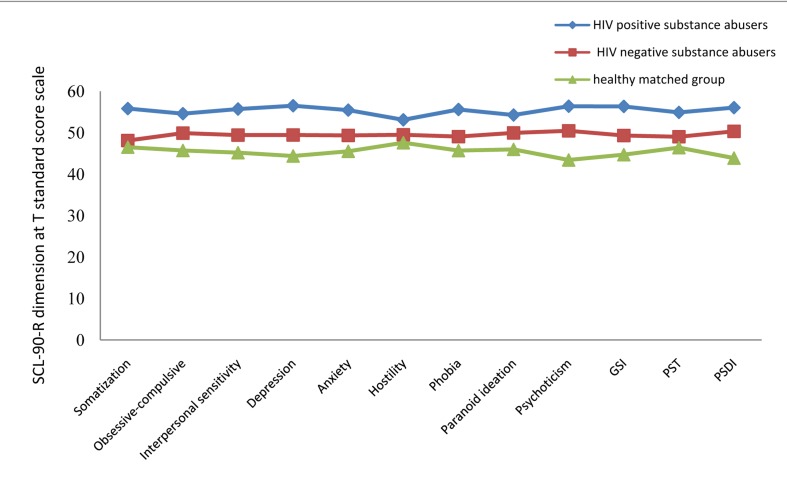
Figure 1 by T standard score for all subscales of SCL-90-R is the best method to demonstrate the difference and order of mental disorder symptoms, and distribution of psychopathological profile of the 3 groups in this study.
Figure 1.
Comparison of distribution of psychopathological profile of the 3 groups GSI: Global severity index; PST: Positive symptom total; PSDI: Positive symptom distress index
Discussion
This research aimed to compare psychopathological dimensions in substance abusers with and without HIV/AIDS and their matched group. Finding a clear discrimination between and a sample of mental disorder symptoms in these groups is an important step in promotion of medical outcomes and prognosis of multiple chronic, mental, and medical diseases (addiction with HIV/AIDS).
Data showed that the population of substance abusers with HIV/AIDS report significantly higher rates of drug injection history (P = 0.041) and imprisonment (P < 0.012) compared to substance abusers without this infection. Findings have shown sharing contaminated needles and syringes is the major risk factor in HIV transmission and other blood borne infections.10,33 The results of this project and the findings of the study by Hammett uncovered that group imprisonment of substance abusers leads to a raise in HIV/AIDS infection compared to other routes. Nevertheless, different studies proved that imprisonment increases HIV infection rates via factors such as social support cessation, multiple sex partners, or risky sexual behaviors.34-36 These findings indicate that longer imprisonment in congregate and crowded settings, for instance in prisons, plus continuous injection of drugs can make the HIV infection more prevalent. Therefore, watchful follow-up and performance such as mandatory programs to prevent transmission of HIV/AIDS, includes: creating more awareness of homosexual behavior and sharing contaminated syringes in prisons, also damage-reduction interventions in DICs and self-proclaimed addicts, and distributing new syringes and collecting used ones.
Findings of this study indicate that substance abusers with HIV/AIDS show significantly more frequency of mental disorders based on GSI in SCL-90-R test (88.4%) compared to substance abusers without HIV/AIDS (75.5%), and the healthy matched group (53.3%) (Table 2). Moreover, the majority of studies have claimed a close relationship between mental comorbidities and substance use disorders in HIV-infected individuals.5,6,8,10,12,17,30 Similarly, some studies have demonstrated that individuals with this triple comorbidity (mental disorder, substance abuse, and HIV infection) are more likely to exhibit risky behaviors and have an active role in fueling the HIV epidemic when not under therapy.37
Results of the present effort clarified that substance abusers with HIV/AIDS, in all psychopathological dimensions, have significantly more symptoms compared with their healthy matched group (P < 0.001). In addition, substance abusers without HIV/AIDS show higher levels of symptoms (P < 0.05) in comorbidity dimensions of somatization, interpersonal sensitivity, depression, anxiety, phobia, and psychoticism, GSI, PST, and PSDI. However, there was no significant difference between them in paranoid ideation and hostility (Table 4). These findings suggest the existence of important qualitative differences in psychopathological dimensions between these groups. On the other hand, multiplicity of significant differences among substance abusers with and without HIV/AIDS support the idea that HIV infection is not related to any special symptomatology. Moreover, Koutsilieri et al. have mentioned the development of a wide continuum of mental illnesses in HIV-infected substance abusers.37 However, we may interpret increased levels of comorbidity symptoms in substance abusers with HIV/AIDS compared to other groups of this study as below:
Effective psychopathological factors in HIV/AIDS: HIV-infected individuals may develop some mental disorders before HIV infection which in turn can predispose individuals to HIV. Furthermore, Baillargeon et al. showed that major depression, dysthymia, bipolar disorder, schizophrenia, schizoaffective disorder, and non-schizophrenic psychotic disorder, which can be placed among chronic mental disorders, are more prevalent in patients with HIV.7 Meade et al., also found that recent manic episode, lower psychiatric symptom severity, and greater drug usage are predictors of HIV infection in patients with multiple bipolar and drug use disorders.38 In addition, according to findings of Atkinson et al. those with HIV infection reported more depression in their lifetime, the onset of which was before HIV infection in one third of the cases, in comparison to those without HIV. Furthermore, HIV-infected group, in comparison to the non-infected group, showed more substance use in their lifetime. Finally, Koutsilieri et al. postulated that substance abuse accelerates HIV encephalopathy progression. These substances activate mesocortical/mesolimbic dopaminergic pathways which in turn can lead to psychosis that is difficult to differentiate from schizophrenia.
The outcome of psychopathology resulting from HIV/AIDS: As soon as the first positive test and the first symptoms of HIV/AIDS are manifested, the mental profile of the patient will shift to maladjustment. Denial and reluctant behaviors of friends, spouse, and family members cause acute depressive reactions. Moreover, the feeling of an epidemic factor growing in their body makes HIV patients feel rejected. Due to prejudgments and concerns about infection, these individuals are discriminated against in matters of their house, job, health care, and public support. Illogical fear and negative reaction of society is among the problems the patients, their families, and supportive groups still face.21 Results of previous studies and the present survey have found a considerable range of psychopathological dimensions in these patients including mood and anxiety disorders, PTSD, psychosis, suicidal thinking, and simultaneity of several mental disorders especially substance use disorders.3-8,12,31
Results of the present study should be generalized with regard to its limitations. In this project, self-report method was used to evaluate psychopathological dimensions. Despite its sensitivity and good feature of mental disorder diagnosis, SCL-90-R cannot help us in descriptive and navigating researches to discover and compare the prevalence of mental disorders of different groups based on DSM-IV-TR.26 Furthermore, SCL-90-R has not been extensively validated in a population with HIV/AIDS. Therefore, it is suggested that structured diagnosis interviews be used instead of screening diagnosis tools. The association between HIV/AIDS infection and manifestation of mental disorder symptoms can be bilateral; thus, the results of this study with a cross-sectional design are not adequate. We should consider that conducting a study in a specific area cannot be indicative of the behaviors in all individuals with and without HIV/AIDS. Thus, it is proposed that future studies be carried out with respect to multi-center sampling and the dimensions of personality disorders. Here, the point to note is that simultaneous medical and mental disorders and substance use make it difficult to care for these patients. Thus, resolving these limitations is proposed for future efforts which should insist on the necessity of designing a model with the most effective medical services, and social and psychological work so these patients obtain a normal status of health.
Conclusion
Overall, it can be stated that symptoms of mental disorders in substance abusers with HIV/AIDS is significantly more than substance abusers without it, and less than the matched group in all dimensions. Comorbidity of substance abuse and HIV diagnosis accentuates mental disorder symptoms. In addition, not preventing and performing appropriate psychological interventions following substance abuse and HIV infection leads to widespread establishment of mental disorder symptoms.
Acknowledgments
The present research is funded by the Research Deputy of Guilan University of Medical Sciences (NO. P/3/132/10617 approved on 8/June/2010). The author would like to offer his special thanks to the Research Counseling of GUMS and Dr. Tousi, the supervisor of the Behavioral Disorder Counseling Clinic in Rasht, Dr. Tavakolifard, expert in prevention programs in the Welfare Organization of Guilan province, Ms. Nedaie, the clinical psychologist of the Drop in Center of (disabled and elderly) Nursing Home (Ma'lolin) of Rasht for their sincere cooperation.
Footnotes
Conflicts of Interest
The Authors have no conflict of interest.
REFERENCES
- 1.Ratigan B. Counseling people affected by HIV and AIDS. In: Palmer S, MacMahon G, editors. Handbook of Counselling. London, UK: Routledge; 1997. [Google Scholar]
- 2.Sayad B, Hatami H, Janbakhsh AR, Vaziri S, Afsharian M, Rezabeigi M. Survey of Clinical Syndromes leading to Hospitalization in HIV Infected Patients According to CD4 count in Sina Hospital (Kermanshah). Sci J Hamdan Univ Med Sci. 2006;13(3):51–6. [Google Scholar]
- 3.Nebhinani N, Mattoo SK, Wanchu A. Psychiatric morbidity in HIV-positive subjects: a study from India. J Psychosom Res. 2011;70(5):449–54. doi: 10.1016/j.jpsychores.2010.09.021. [DOI] [PubMed] [Google Scholar]
- 4.Peng EY, Lee MB, Morisky DE, Yeh CY, Farabee D, Lan YC, et al. Psychiatric morbidity in HIV-infected male prisoners. J Formos Med Assoc. 2010;109(3):177–84. doi: 10.1016/S0929-6646(10)60040-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zahari MM, Hwan BW, Zainal NZ, Habil H, Kamarulzaman A, Altice FL. Psychiatric and substance abuse comorbidity among HIV seropositive and HIV seronegative prisoners in Malaysia. Am J Drug Alcohol Abuse. 2010;36(1):31–8. doi: 10.3109/00952990903544828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adewuya AO, Afolabi MO, Ola BA, Ogundele OA, Ajibare AO, Oladipo BF. Psychiatric disorders among the HIV-positive population in Nigeria: a control study. J Psychosom Res. 2007;63(2):203–6. doi: 10.1016/j.jpsychores.2007.03.006. [DOI] [PubMed] [Google Scholar]
- 7.Baillargeon J, Ducate S, Pulvino J, Bradshaw P, Murray O, Olvera R. The association of psychiatric disorders and HIV infection in the correctional setting. Ann Epidemiol. 2003;13(9):606–12. doi: 10.1016/S1047-2797(03)00061-9. [DOI] [PubMed] [Google Scholar]
- 8.Olley BO, Seedat S, Stein DJ. Persistence of psychiatric disorders in a cohort of HIV/AIDS patients in South Africa: a 6-month follow-up study. J Psychosom Res. 2006;61(4):479–84. doi: 10.1016/j.jpsychores.2006.03.010. [DOI] [PubMed] [Google Scholar]
- 9.Mohseni F. The rate of mental disorders in patients HIV + / AIDS in Zahedan and Saravan city. Zahedan, Iran: Zahedan University of Medical Sciences; 2005. [Google Scholar]
- 10.Altice FL, Kamarulzaman A, Soriano VV, Schechter M, Friedland GH. Treatment of medical, psychiatric, and substance-use comorbidities in people infected with HIV who use drugs. Lancet. 2010;376(9738):367–87. doi: 10.1016/S0140-6736(10)60829-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bing EG, Burnam MA, Longshore D, Fleishman JA, Sherbourne CD, London AS, et al. Psychiatric disorders and drug use among human immunodeficiency virus-infected adults in the United States. Arch Gen Psychiatry. 2001;58(8):721–8. doi: 10.1001/archpsyc.58.8.721. [DOI] [PubMed] [Google Scholar]
- 12.Sayad B, Shakeri J, Hoseini M, Janbakhsh A, Aminijavid F, Omidniakan Z. Correlation of psychiatric disorders with CD4 counts in HIV/AIDS patients in Sina hospital, Kermanshah. Pejouhesh. 2007;31(3):247–54. [Google Scholar]
- 13.Atkinson JH, Higgins JA, Vigil O, Dubrow R, Remien RH, Steward WT, et al. Psychiatric context of acute/early HIV infection. The NIMH Multisite Acute HIV Infection Study: IV. AIDS Behav. 2009;13(6):1061–7. doi: 10.1007/s10461-009-9585-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rabkin JG. HIV and depression: 2008 review and update. Curr HIV/AIDS Rep. 2008;5(4):163–71. doi: 10.1007/s11904-008-0025-1. [DOI] [PubMed] [Google Scholar]
- 15.Atkinson JH, Jin H, Shi C, Yu X, Duarte NA, Casey CY, et al. Psychiatric context of human immunodeficiency virus infection among former plasma donors in rural China. J Affect Disord. 2011;130(3):421–8. doi: 10.1016/j.jad.2010.10.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marcellin F, Preau M, Ravaux I, Dellamonica P, Spire B, Carrieri MP. Self-reported fatigue and depressive symptoms as main indicators of the quality of life (QOL) of patients living with HIV and Hepatitis C: implications for clinical management and future research. HIV Clin Trials. 2007;8(5):320–7. doi: 10.1310/hct0805-320. [DOI] [PubMed] [Google Scholar]
- 17.Katibaei J , Hamidi H, Yarian S, Ghanbari S, Seyed Mousavi PS. Comparison of quality of life, stress and mental health of addicts and non-addicts affected by HIV and healthy individuals. J Res Behav Sci. 2010;4(2):135–9. [Google Scholar]
- 18.Kemppainen JK, Levine R, Buffum M, Holzemer W, Finley P, Jensen P. Antiretroviral adherence in persons with HIV/AIDS and severe mental illness. J Nerv Ment Dis. 2004;192(6):395–404. doi: 10.1097/01.nmd.0000130132.55146.04. [DOI] [PubMed] [Google Scholar]
- 19.Management of Diseases Center. Latest report related to HIV/AIDS infection in Islamic republic of Iran. Tehran, Iran: Ministry of Health and Medical Education; 2011. pp. 1–6. [Google Scholar]
- 20.Bratcher TL, Moran MA, Zimmer WJ. Tables of Sample Size in the Analysis of Variance. Journal of Quality Technology. 1970;2(3):156–64. [Google Scholar]
- 21.Muma RD, Pollard RB, Lyons BA. HIV manual for health care professionals. New York, NY: Appleton & Lange; 1997. [Google Scholar]
- 22.Derogatis LR, Lipman RS, Covi L. SCL-90: an outpatient psychiatric rating scale--preliminary report. Psychopharmacol Bull. 1973;9(1):13–28. [PubMed] [Google Scholar]
- 23.Derogatis LR, Rickels K, Rock AF. The SCL-90 and the MMPI: a step in the validation of a new self-report scale. Br J Psychiatry. 1976;128:280–9. doi: 10.1192/bjp.128.3.280. [DOI] [PubMed] [Google Scholar]
- 24.Groth-Marnat G. Handbook of Psychological Assessment. New Jersey, NJ: John Wiley & Sons; 2009. [Google Scholar]
- 25.Derogatis LR. Misuse of the symptom checklist 90. Arch Gen Psychiatry. 1983;40(10):1152–3. doi: 10.1001/archpsyc.1983.01790090114025. [DOI] [PubMed] [Google Scholar]
- 26.Bagheri Yazdi SA, Bolhari J, Shah Mohammadi D. Epidemiology of mental disorders in sub rural areas of Meybod in Yazd state. Iran J Psychiatry Clin Psychol. 1992;1:32–42. [Google Scholar]
- 27.Noorbala AA, Kazam M, Bageri Yazdi SA. The Survey of prevalence psychiatric disorder in Tehran. Hakim Res J. 1999;2(4):212–23. [Google Scholar]
- 28.Hedayati-Moghaddam MR, Eftekharzadeh Mashhadi I, Zibaee R, Hosseinpoor AM, Fathi-Moghaddam F, Bidkhori H. Assessment of Psychiatric Symptoms Using SCL-90-R among HIV/AIDS Individuals in Razavi Khorasan Province, Iran. Iran Red Crescent Med J. 2011;13(1):58–9. [PMC free article] [PubMed] [Google Scholar]
- 29.Latas M, Kostic M, Glomazic O. P01-281- Psychopathological features in somatic asymptomatic HIV positive patients. European Psychiatry. 2010;25(Supplement 1):494. [Google Scholar]
- 30.Nnadi CU, Better W, Tate K, Herning RI, Cadet JL. Contribution of substance abuse and HIV infection to psychiatric distress in an inner-city African-American population. J Natl Med Assoc. 2002;94(5):336–43. [PMC free article] [PubMed] [Google Scholar]
- 31.Habibpoor K, Safari R. Comprehensive manual for using SPSS in survey researches. Tehran, Iran: Looyeh and Motefakkeran Publication; 2010. p. 565. [Google Scholar]
- 32.Hammett TM. HIV/AIDS and other infectious diseases among correctional inmates: transmission, burden, and an appropriate response. Am J Public Health. 2006;96(6):974–8. doi: 10.2105/AJPH.2005.066993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Thomas JC. From slavery to incarceration: social forces affecting the epidemiology of sexually transmitted diseases in the rural South. Sex Transm Dis. 2006;33(7 Suppl):S6–10. doi: 10.1097/01.olq.0000221025.17158.26. [DOI] [PubMed] [Google Scholar]
- 34.Wallace R. Social disintegration and the spread of AIDS-II. Meltdown of sociogeographic structure in urban minority neighborhoods. Soc Sci Med. 1993;37(7):887–96. doi: 10.1016/0277-9536(93)90143-r. [DOI] [PubMed] [Google Scholar]
- 35.Harrison LD. The Revolving Prison Door for Drug-Involved Offenders: Challenges and Opportunities. Crime & Delinquency. 2001;47(3):462–85. [Google Scholar]
- 36.Kalichman SC, Rompa D. HIV treatment adherence and unprotected sex practices in people receiving antiretroviral therapy. Sex Transm Infect. 2003;79(1):59–61. doi: 10.1136/sti.79.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Koutsilieri E, Scheller C, Sopper S, ter Meulen V, Riederer P. Psychiatric complications in human immunodeficiency virus infection. J Neurovirol. 2002;8(Suppl 2):129–33. doi: 10.1080/13550280290167948. [DOI] [PubMed] [Google Scholar]
- 38.Meade CS, Graff FS, Griffin ML, Weiss RD. HIV risk behavior among patients with co-occurring bipolar and substance use disorders: associations with mania and drug abuse. Drug Alcohol Depend. 2008;92(1-3):296–300. doi: 10.1016/j.drugalcdep.2007.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]