Abstract
Blister formation in skin and mucous membranes results from a loss of cell-cell or cell-matrix adhesion and is a common outcome of pathological events in a variety of conditions, including autoimmune and genetic diseases, viral and bacterial infections, or injury by physical and chemical factors. Autoantibodies against structural components maintaining cell-cell and cell-matrix adhesion induce tissue damage in autoimmune blistering diseases. Detection of these autoantibodies either tissue-bound or circulating in serum is essential to diagnose the autoimmune nature of disease. Various immunofluorescence methods as well as molecular immunoassays, including enzyme-linked immunosorbent assay and immunoblotting, belong to the modern diagnostic algorithms for these disorders. There is still a considerable need to increase awareness of the rare autoimmune blistering diseases, which often show a severe, chronic-relapsing course, among physicians and the public. This review article describes the immunopathological features of autoimmune bullous diseases and the molecular immunoassays currently available for their diagnosis and monitoring.
Keywords: Autoantibodies, autoantigens, basement membrane, desmosome, ELISA, extracellular matrix, hemidesmosome, immunoassay, immunoblotting, immunofluorescence microscopy.
INTRODUCTION
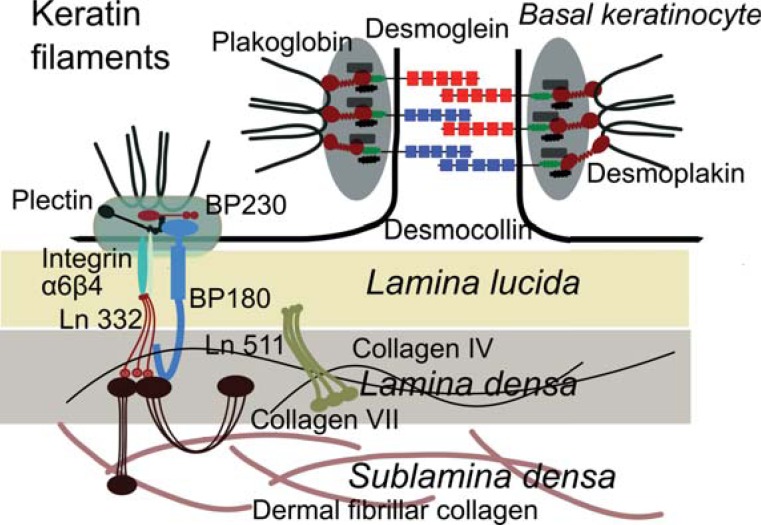
Autoimmune blistering diseases are classified into four major groups, including pemphigus, the pemphigoids, epidermolysis bullosa acquisita, and dermatitis herpetiformis (Table 1) [1, 2]. Autoimmune bullous diseases are organ-specific autoimmune diseases associated with pathogenic autoantibodies against structural proteins that maintain cell-cell and cell-matrix adhesions in the skin and mucous membranes [1, 3]. Cell-cell adhesion in the epidermis is mainly maintained by desmosomes and adherens junctions. The extracellular portions of desmosomal cadherins link neighboring keratinocytes, whereas their intracellular regions bind to desmosomal plaque proteins, which mediate the interaction of desmosomes with the keratin intermediate filament cytoskeleton. Major autoantigens in the pemphigus group of diseases include desmogleins, desmocollins and the plaque proteins desmoplakin, periplakin and envoplakin (Fig. 1) [1, 4]. Structural components of the basement membrane that maintain cell-matrix adhesion and may function as autoantigens in subepidermal blistering diseases include the intracellular plectin and BP230, which interacts with the transmembrane hemidesmosomal
Table 1.
Major Autoantigens in Bullous Diseases
| Disease | Autoantigen |
|---|---|
| Pemphigus Diseases | |
| Pemphigus vulgaris | Desmoglein 3, desmoglein 1 |
| Pemphigus foliaceus | Desmoglein 1 |
| Pemphigus erythematosus | Desmoglein 1, 3, ANAs |
| Paraneoplastic pemphigus | Desmoglein 1, desmoglein 3, desmoplakin, envoplakin, periplakin, BP230, alpha-2-macroglobuline-like-1, plectin, desmocollins 1-3 |
| IgA pemphigus | Desmocollin 1-3, desmoglein 3 |
| Pemphigoid Diseases | |
| Bullous pemphigoid | BP180, BP230 |
| Pemphigoid gestationis | BP180, BP230 |
| Mucous membrane pemphigoid | BP180, Laminin 332, Α6Β4 integrin |
| Linear IgA disease | LAD-1 (BP180), BP230 |
| Anti-p200 pemphigoid | p200 antigen (Laminin Γ1) |
| Epidermolysis bullosa acquisita | Collagen VII |
| Dermatitis herpetiformis | Tissue/epidermal transglutaminase |
Fig. (1).
Schematic representation of major skin autoantigens. The autoantigens shown here are molecules involved in maintaining the cell-cell and cell-matrix adhesion. The transmembrane desmosomal cadherins of neighboring cells, desmogleins and desmocollins, confer adhesion by homo- and heterophilic interaction in the extracellular space. On the cytoplasmic sides of the desmosome, the carboxy-terminal regions of cadherins are rooted in the desmosomal plaques composed of proteins belonging to the armadillo and plakins superfamilies, such as desmoplakin, which bind to the intermediate keratin filaments. The hemidesmosomes are important for the stable anchorage of basal keratinocytes to the underlying basement membrane. The intracellular portion of transmembrane hemidesmosomal proteins, incuding collagen XVII and integrin α6β4, binds to intracellular plaque proteins BP230 and plectin, which link hemidesmosomes to keratin intermediate filaments. Collagen XVII/BP180 and α6β4 integrin bind extracellularly to the extracellular matrix protein laminin (Ln) 332, a major component of the lamina densa. Laminin γ1 chain, present in the vessel walls and at the epidermal basement membrane as in laminin 511, may function as autoantigen. Finally, collagen VII is the main constituent of the anchoring fibrils, which connect lamina densa to the collagen fibers of the upper dermis.
components collagen XVII/BP180 and α6β4 integrin. Laminin 332 in the lower lamina lucida and lamina densa is a known ligand for α6β4 integrin. Beside other ubiquitous proteins like perlecan and nidogen, laminin 332 (previously known as epiligrin or laminin 5) and collagen IV form a network in the lamina densa [5]. Laminin γ1 chain, present in laminins 511 and 311 was identified as target of autoantibodies in anti-p200 pemphigoid. In the epidermal basement membrane, laminin γ1 interacts with integrins α3β1 and α6β4. Both laminin 332 and its ligand collagen VII of the anchoring fibrils, may be targeted by autoantibodies in subepidermal blistering diseases [1, 3, 5].
Due to major advances over the last few decades in identifying the autoantigens in autoimmune blistering disease, rapid and specific laboratory diagnostic tests have become reality and are currently widely available.
Astute clinical observation and skillful histopathological examination are essential for suspecting an autoimmune blistering disease [1]. The clinical examination should include careful evaluation of skin and mucosal surfaces. The Nikolsky sign should be tested by applying pressure to the perilesional or normal skin to determine if blisters can be extended or induced in normal-appearing skin, characteristic of the pemphigus group of diseases [6, 7]. The Tzanck smear is a simple and inexpensive ancillary diagnostic tool that can provide rapid cytologic information. Optimally, the test is performed on a fresh blister (< 24 hrs-old). Material is gently scraped from the base of a vesicle, blister, or pustule, onto a slide and is allowed to air dry and then stain with different dyes, including Giemsa, toluidine blue, and methylene blue [8, 9]. The routine histological examination is performed on a biopsy of a fresh vesicle or blister (< 1 day-old), and helps to reveal the level of blister formation as well as the presence and features of the inflammatory infiltrate [10].
However, diagnosis of an autoimmune blistering disease requires detection of tissue-bound and/or circulating autoantibodies to confirm the autoimmune nature of disease. Deposits of immunoreactants (typically immunoglobulins and complement components) in the perilesional skin are detected by direct immunofluorescence (IF) microscopy, which remains the gold standard for the diagnosis of autoimmune bullous diseases [10, 11]. An accurate diagnosis further relies on the characterization of autoantibody specificity using different immunoassays, including indirect IF, immunoblotting, enzyme-linked immunosorbent assay (ELISA), and immunoprecipitation [1, 10].
By indirect IF microscopy circulating antibodies are detected in the patients' sera by incubating with epithelial substrates such as human skin, esophagus and bladder. The indirect IF on salt-split skin, obtained by incubation of human skin in a 1M NaCl solution, showing a cleavage within the lamina lucida delivers “semi-molecular” information on the identity of the autoantigens at the dermal-epidermal junction based on their localization on the epidermal or dermal side of the artificial cleavage [10, 12].
The enzyme-linked immunosorbent assay (ELISA) is a sensitive and easy-to-perform test allowing for the characterization of the autoantibody specificity. Several immunoassays using purified native and recombinant proteins have been developed for detection of autoantibodies specific for the main autoantigens in the autoimmune blistering diseases (Table 2). Autoantibodies against specific antigens may be detected also by immunoblotting, which may be performed using both recombinant antigens and extracts of skin or cultured skin cells and is most relevant especially when no ELISA systems are available [1].
Table 2.
Quantitative Immunoassays for the Detection of Autoantibodies in Autoimmune Blistering Skin Diseases
| Autoantigen | Epitope(s) | Disease(s) | Commercially Available |
References |
|---|---|---|---|---|
| Desmoglein 1 | Ectodomain | Pemphigus | yes | [26, 178] |
| Desmoglein 3 | Ectodomain | Pemphigus | yes | [26, 178] |
| Envoplakin | Full-length | Paraneoplastic pemphigus | yes | [179-181] |
| Periplakin | Full-length | Paraneoplastic pemphigus | no | [179, 180] |
| BP180/collagen XVII | NC16A domain | Pemphigoid (IgG, IgE) | yes | [92, 95, 182-184] |
| 4xNC16A domain | Pemphigoid (IgG) | yes | [62] | |
| Ectodomain | Pemphigoid (IgA) | no | [138] | |
| BP230 | Fragments covering the full-lenght of BP230 | Pemphigoid (IgG) | yes | [93] |
| Laminin Γ1 (p200) | C-terminal regiÓn | Anti-p200 pemphigoid (IgG) | no | [150] |
| Collagen VII | NC1 domain | Epidermolysis bullosa acquisita (IgG) | yes | [185, 186] |
| NC1, NC2 domains | Epidermolysis bullosa acquisita (IgG) | yes | [159] | |
| NC1, NC2, hinge domains | Epidermolysis bullosa acquisita (IgG) | no | [161] | |
| Transglutaminase, tissue |
Full-length | Dermatitis herpetiformis (IgA) | yes | [166, 187] |
| Transglutaminase, tissue |
Deamidated gliadin-analogous fusion peptides | Dermatitis herpetiformis (IgA) | yes | [188] |
| Transglutaminase, epidermal |
Dermatitis herpetiformis (IgA) | yes | [167] |
Immunoprecipitation is the technique of precipitating an autoantigen out of solution using patient serum. Serum is mixed with an extract of radioactively-labeled keratinocytes or their medium and the formed immune complexes are recovered by adding protein A/G-beads [1]. This method was used to identify several autoantigens and was historically the gold standard diagnostic test in paraneoplastic pemphigus and anti-epiligrin (laminin 332) mucous membrane pemphigoid [1, 13, 14].
Using these methods autoimmune blistering may be easily differentiated from blistering due to other causes, including infections, genodermatoses, metabolic and other inflammatory diseases. Incomplete phenotypes, disease associations and particular pathological constellations may occasionally however make diagnosis a challenging task. By considering for instance that vesiculo-bullous eruption due to acute herpes or zoster infection may occasionally occur especially in elderly and severely immunosuppressed patients with autoimmune blistering disease, the informed practitioner may avoid the “disease flare” trap [15, 16]. In the following sections, we review the clinical and histologic presentation of the autoimmune blistering diseases, followed by the molecular studies available for their diagnosis.
PEMPHIGUS DISEASES
The term pemphigus is the latinized form of the Greek πέμφιξ (pemphix) meaning bubble or blister and was first used by Wichmann at the end of the 18th century to describe bullous diseases [17, 18]. Pemphigus comprises a group of life-threatening autoimmune blistering conditions characterized by acantholytic intraepithelial blister and caused by autoantibodies against intercellular adhesion molecules [1, 19]. Different clinical forms of pemphigus are characterized by their distinctive autoantigens, histo- and immunopathological findings. A characteristic histolopathological feature of pemphigus is acantholysis, which results from the loss of cell-cell adhesion and is defined as detachment of individual or grouped keratinocytes [1, 19].
PEMPHIGUS VULGARIS
Pemphigus vulgaris (PV) is characterized by suprabasal acantholytic blister formation and autoantibodies against the keratinocyte surface proteins [1]. Several autoantigens have been described in PV, including desmoglein 3, desmoglein 1, and less frequently, desmocollin 3, acetycholine α9 receptor and pemphaxin [20-26]. The profile of autoantibodies against desmogleins 1 and 3 correlates well with the clinical form of PV [27]. Autoantibodies against desmoglein 3 are present in patients with mucosal-dominant PV, while reactivity against desmogleins 1 and 3 is characteristic of muco-cutaneous PV [21, 27]. The levels of IgG, but also IgE autoantibodies against desmoglein 3 correlate with disease activity in PV patients [26, 28]. While their detection may be helpful for diagnosing pemphigus, the pathogenic relevance of IgA and IgE autoantibodies against desmogleins has not been experimentally demonstrated. IgG4 autoantibodies in pemphigus vulgaris are indicative of active disease, whereas IgG1 autoantibodies are mainly found in remission [29].
The production of pathogenic autoantibodies in pemphigus is T cell-dependent. Autoreactive Th2 cell responses directed against the extracellular domain of desmoglein 1 and 3 have been conclusively documented in pemphigus patients [30, 31]. PV can be also considered as an autoimmune disorder associated with a Treg dysfunction since PV patients have less desmoglein 3-reactive type 1 regulatory T cells than healthy controls [32].
Pemphigus vulgaris may be precipitated by drugs and UV exposure (Table 3) [33-36]. Thiol drugs, such as penicillamine and captopril, are the most common inciting agents, but further drugs, including penicillins, cephalosporins, enalapril, rifampin, and nonsteroidal antiinflammatory agents were reported to be associated with pemphigus [33-35].
Table 3.
Drugs Reported as Putative Triggers of Autoimmune Blistering Diseases
| Drugs | Triggered Disease | Evidence Level* | References |
|---|---|---|---|
| Antibiotics | |||
| Vancomycin | LAD | 3 | [189-203] |
| Trimethoprim-sulfamethoxazole | LAD | 3 | [204] |
| Penicillin G | LAD, anti-p200 | 3 | [205, 206] |
| Ampicillin-Sulbactam | LAD | 3 | [207] |
| Lithium carbonate | LAD | 3 | [208] |
| Phenytoin | LAD | 3 | [189] |
| Amiodarone | LAD | 3 | [209] |
| Atorvastatin | LAD | 3 | [210] |
| Nonsteroidal Anti-Inflammatory Drugs | |||
| Acetylsalicylic acid | BP | 3 | [211] |
| Diclofenac | LAD | 3 | [212, 213] |
| Penicillamine | PV, PF, PE, BP, MMP, EBA | 3 | [214, 215] |
| PUVA | BP, PV, PF | 3 | [216-220] |
| UV | PF, BP, EBA | 3 | [221-223] |
From Scottish Intercollegiate Guidelines Network (SIGN; http://www.sign.ac.uk/guidelines/fulltext/50/annexb.html).
Clinically, PV usually involves initially the oral cavity and is characterized by flaccid blisters and erosions causing pain that may result in weight loss and malnutrition. Nasal, vaginal and anal mucosa may be also affected in PV. Therefore, the diagnosis of PV should be considered in all patients with mucosal erosive lesions. In patients with mucocutaneos disease blisters also affect the skin. Skin blisters are typically flaccid and easily eroded and can arise on healthy-appearing or on erythematous skin (Fig. 2a). Blisters may be painful or, less frequently, itchy. Erosions in the skin folds may develop into vegetative lesions, typical for the clinical form of PV known as pemphigus vegetans. In a very small number of patients with PV, classified as cutaneous-type PV, no mucous membrane involvement is observed, despite autoantibodies against both desmogleins 1 and 3 [21, 27, 37]. Pemphigus herpetiformis is another rare clinical variant of PV, which manifests as cutaneous vesicles in a herpetiform pattern with rare mucosal involvement and autoantibodies against desmoglein 3 [1, 38].
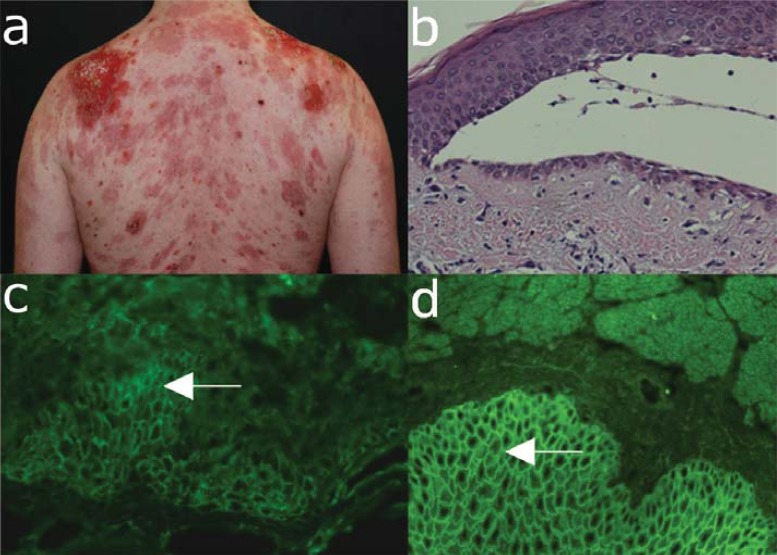
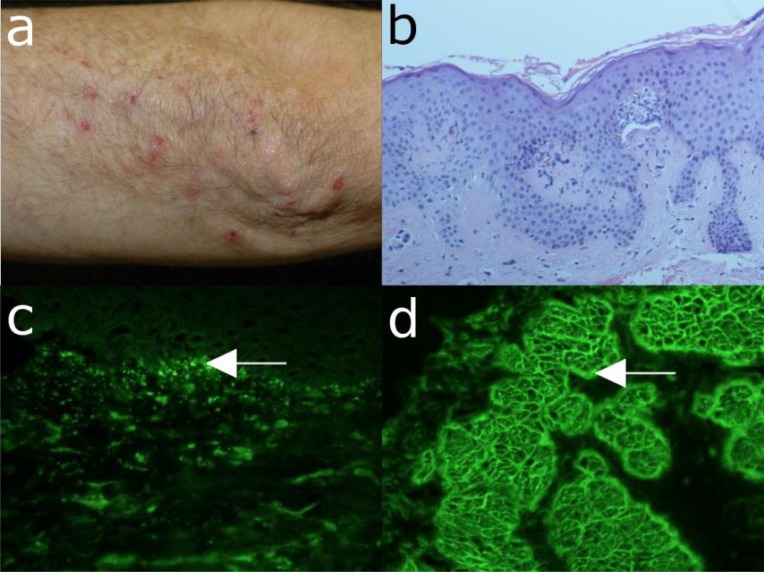
Fig. (2).
Major clinical and laboratory findings in pemphigus vulgaris. (a) Extensive erosions with crusts and hyperpigmentation on the back of a 34-year old male patient with muco-cutaneous pemphigus vulgaris. (b) Histopathological examination reveals suprabasal acantholysis with modest inflammatory infiltrate. A single layer of basal keratinocytes remains attached to the basement membrane as a “row of tombstones”. (c) Direct immunofluorescence microscopy analysis of a perilesional skin biopsy shows deposits of IgG with an intercellular pattern in the epidermis. (d) Serum IgG autoantibodies binding with an intercellular pattern are detected by indirect immunofluorescence microscopy on monkey oesophagus (all magnification 200x).
Diagnosis of PV should be considered in patients with persistent blisters and erosions of mucous membranes and skin. This suspicion is further strengthened by a positive Nikolsky sign. The diagnosis is secured by histology demonstrating suprabasal acantholysis and detection of tissue-bound IgG with an intercellular (“cobblestone”, “fishnet”) pattern by direct IF microscopy and of circulating IgG autoantitbodies binding to the intercellular junctions of epithelial cells by indirect IF microscopy on monkey esophagus and recognizing desmoglein 3 by ELISA (Table 4).
Table 4.
Diagnostic Criteria for Pemphigus Vulgaris
| Investigation | Finding |
|---|---|
| Clinic | Mucosal and skin blistering, inflammation, erosions |
| Histology | Acantholysis with little inflammatory infiltrate, intraepithelial separation (suprabasal layer), “row of tombstones” |
| Direct immunofluorescence microscopy |
Intraepidermal deposits of IgG (+/- C3) with an intercellular pattern |
| Indirect immunofluorescence microscopy (esophagus) |
Binding of IgG autoantibodies to epithelial cells with an intercellular pattern |
| ELISA | IgG autoantibodies specific for desmoglein 3 (mucosal) +/- desmoglein 1 (mucocutaneous) |
Histopathological examination typically reveals intraepithelial cleavage with acantholysis, occasionally associated with a sparse inflammatory infiltrate (Fig. 2b). The split formation occurs mainly in the suprabasal layer and basal keratinocytes remain attached to the basement membrane suggesting a “row of tombstones”. By direct immunofluorescence microscopy of patient perilesional skin intercellular deposits of IgG and occasionally C3 are found (Fig. 2c) [1].
Serum IgG autoantibodies binding with an intercellular pattern to epithelium are revealed by indirect IF microscopy, which can yield a semi-quantitative autoantibody titer (Fig. 2d). While different substrates were used for the detection of pemphigus autoantibodies, monkey esophagus has gained a wide acceptance as a sensitive substrate. The molecular specificity of pemphigus autoantibodies may be analyzed using sensitive and specific immunoassays, which are commercially available (Table 2) [26]. ELISA systems using recombinant desmogleins for detecting circulating autoantibodies are essential for the initial diagnosis and allow monitoring the pathogenic autoantibody levels during clinical follow-up.
PEMPHIGUS FOLIACEUS
Pemphigus foliaceus (PF) is a superficial variant of pemphigus showing cutaneous lesions and virtually no involvement of mucous membranes associated with subcorneal cleavage and autoantibodies against desmo-glein 1 [1]. Additional clinical forms of superficial pem-phigus, including pemphigus erythematosus, endemic pemphigus foliaceus (fogo selvagem), and drug-induced pemphigus foliaceus, share clinical, histo- and immuno-pathological features and may be classified as subtypes of PF. The main autoantigen of PF is desmoglein 1 [39]. Desmoglein 1-specific pathogenic autoantibodies in patients with PF mainly belong to the IgG4 isotype [40].
While the cause of most sporadic PF is still elusive, the induction of fogo selvagem appears to be related to environmental factors (e.g., molecular mimicry due to infections transmitted by insects) [41-43]. In certain patients, PF may have been precipitated by extensive UV exposure, burns or by various drugs, including penicillamine, inhibitors of angiotensin convertase, cephalosporins, and non-steroidal anti-inflammatory agents (Table 3).
The blistering lesions, which show preference for seborrhoeic areas, usually start on the trunk, face, and scalp. The onset of PF is usually characterized by scattered, small superficial blisters, which rapidly transform into scaly, crusted erosions with a puff pastry-like or cornflake appearance (Fig. 3a). The Nikolsky sign is positive. Untreated, the lesions confluate and may progress to an exfoliative generalized erythroderma. PF, like PV, is a chronic disease, but associated with less mortality. While spontaneous remissions are possible, without adequate treatment, the lesions may persist for several years.
Fig. (3).
Major clinical and laboratory findings in pemphigus foliaceus. (a) Erythema, blisters and erosions in a 61-year old male patient with pemphigus foliaceus. (b) Histopathological examination reveals sub-corneal acantholysis and an inflammatory infiltrate consisting mainly of neutrophil granulocytes. (c) Deposits of IgG with a cobblestone pattern within the epidermis by direct immunofluorescence microscopy analysis of a skin biopsy. (d) By indirect immunofluorescence microscopy on monkey oesophagus, serum IgG autoantibodies are detected, which bind with an intercellular pattern to epithelium (all magnification 200x).
The diagnosis of PF is suggested by superficial skin blisters and erosions without mucosal involvement, and subcorneal cleavage by histopathology. The diagnosis is confirmed by demonstrating intercellular deposition of tissue-bound and circulating autoantibodies by direct and indirect IF microscopy, respectively. The molecular specificity of circulating autoantibodies is further assessed by ELISA using recombinant desmoglein 1 (Table 5).
Table 5.
Diagnostic Criteria for Pemphigus Foliaceus
| Investigation | Finding |
|---|---|
| Clinic | Fragile blisters, crusty erosions (seborrhoeic areas) |
| Histology | Subcorneal cleavage with acantholysis |
| Direct immunofluorescence microscopy | Intraepidermal deposits of IgG (+/- C3) with an intercellular pattern |
| Indirect immunofluorescence microscopy (esophagus) | Binding of IgG autoantibodies to epithelial cells with an intercellular pattern |
| ELISA | Desmoglein 1-specific IgG autoantibodies |
Histopathologically PF is characterized by subcorneal acantholysis, with or without an eosinophilic or neutrophilic inflammatory infiltrate (Fig. 3b). Intercellular deposits of IgG and C3 are revealed by direct IF microscopy (Fig. 3c), while serum IgG autoantibodies are shown to bind to substrates such as esophagus and human skin with an intercellular pattern by indirect IF microscopy (Fig. 3d).
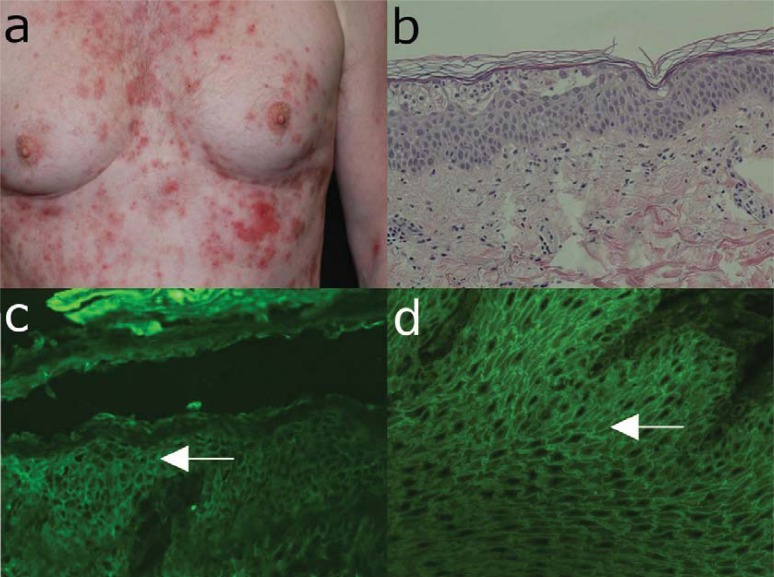
IgG autoantibodies recognizing desmoglein 1, but not desmoglein 3, are measured in serum of PF patients by ELISA (Table 2; Fig. 4a). In PF, the levels of desmoglein 1-specific autoantibodies correlate well with disease activity and are thus helpful for monitoring serologic and clinical activity during the course of the disease of individual patients (Fig. 4b) [26].
Fig. (4).
Detection of desmoglein-specific autoantibodies by ELISA. (a) Pemphigus vulgaris (PV) may present with only mucosal (m) lesions and autoantibodies against desmoglein (Dsg) 3 or with mucocutaneous (m/c) involvement and autoantibodies to both Dsg 1 and 3. Pemphigus foliaceus (PF) patients show only skin lesions and autoantibodies exclusively directed to desmoglein (Dsg) 1. (b) Monitoring of Dsg1- and Dsg3-specific IgG autoantibodies during therapy with prednisolone, azathioprine (AZA), and mycophenolate mofetil (MMF). The gray area represents the disease activity as represented by the PDAI (pemphigus disease area index) scores [177].
PARANEOPLASTIC PEMPHIGUS
Paraneoplastic pemphigus (PNP), first described by Anhalt et al. in 1990, is an autoimmune multi-organ syndrome associated with neoplasia and autoantibodies against desmosomes [13]. In addition to the mucocutaneous disease, which shares important features with pemphigus vulgaris, pulmonary involvement presenting as bronchiolitis obliterans is a rare, but potentially fatal manifestation of PNP. Based on the multi-organ involvement, the alternative name of paraneoplastic autoimmune multi-organ syndrome (PAMS) has been suggested for this paraneoplastic condition [44, 45].
While PNP is usually associated with malignant tumours, especially lymphoproliferative diseases, it may also occur in association with benign neoplasms (Table 6). There is extensive evidence clearly showing that PNP is an obligate paraneoplastic syndrome, strongly suggesting that neoplasms are directly linked to autoimmunity. While the mechanisms of epithelial autoimmunity induction by tumours are not well understood [46, 47], the development of autoantibodies to multiple epithelial proteins could be explained by epitope spreading [48, 49]. The influence of tumour progression and treatment on the autoimmune disease course is variable [46, 47, 50].
Table 6.
Tumors Associated with Paraneoplastic Pemphigus
| Neoplasia | Frequency (%) | References |
|---|---|---|
| Non-Hodgkin lymphoma | 38.6 | [224] |
| Chronic lymphocytic leukemia | 18.4 | [224] |
| Castleman disease | 18.4 | [224] |
| 77 | [225]1 | |
| Hodgkin lymphoma | 0.6 | [224, 226, 227] |
| Thymoma | 6-30 | [50, 228, 229] |
| Waldenstrom's macroglobulinemia | 6 | [224] |
| Carcinomas | 8.6 | [224] |
| Sarcomas | 6.2 | [224] |
| Malignant melanoma | 0.6 | [224] |
| Systemic mastocytosis | ? | [230] |
In a Chinese population.
Typically, PNP patients suffer from severe mucosal involvement with often extensive, intractable stomatitis. The earliest and most constant clinical findings in PNP are painful erosions of the oropharynx. Crusted erosions on the vermilion of the lips are typical and similar to that seen in persons with Stevens-Johnson syndrome. Occasionally, genital, nasal and ocular mucosal surfaces are also affected [51-54]. The cutaneous eruption of PNP includes the typical pemphigus presentation with erythema, blistering, and erosions with positive Nikolski sign, as well as lichenoid lesions resembling erythema multiforme, graft versus host disease, and lichen planus, may be present (Fig. 5a).
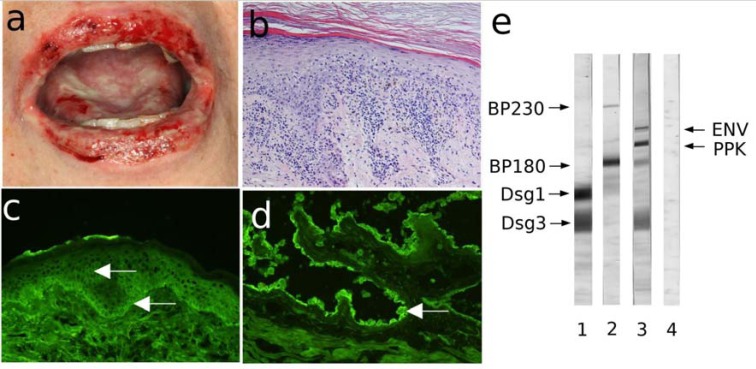
Fig. (5).
Characteristic findings in paraneoplastic pemphigus. (a) Hemorrhagic erosions with crusts on the lips and oral cavity of a patient with non-Hodgkin lymphoma. (b) Interface dermatitis by histopathology (H&E staining). (c) Immunofluorescence (IF) microscopy analysis of a perilesional skin biopsy reveals deposits of IgG at the dermal-epidermal junction and at the intercellular spaces of keratinocytes. (d) Further serological testing by indirect IF microscopy shows binding of IgG autoantibodies to rat bladder urothelium (magnification, 200x). (e) Extract of cultured keratinocytes fractionated by 7.5% SDS-PAGE was transferred to nitrocellulose, and incubated with sera from patients with pemphigus vulgaris (lane 1), bullous pemphigoid (lane 2), paraneoplastic pemphigus serum (lane 3), and normal human serum (lane 4). PNP serum reacts specifically with envoplakin (210 kD, upper arrow) and periplakin (190 kD, lower arrow). The control serum shows no specific reactivity. Migration position for BP230, BP180, Desmoglein (Dsg) 1 and 3 are depicted on the left side of the panel.
In a minority of patients with PNP pulmonary involvement manifests itself as obstructive lung disease and progresses to bronchiolitis obliterans, which responds poorly to immunosuppressive therapy and is a major cause of death, although chest radiograph findings are often normal [55].
Painful, progressive stomatitis with skin blistering and/or lichenoid lesions and constrictive bronchiolitis are suggestive of PNP. Importantly, both the mucocutaneous disease and the constrictive bronchiolitis in PNP patients may be present prior to the discovery of the underlying neoplasm [45]. In addition, while the immunopathological diagnosis of an autoimmune blistering disease is straightforward, it may be difficult to distinguish PNP from “ordinary” pemphigus vulgaris. Therefore, a high degree of suspicion of PNP should trigger specialized diagnostic procedures, including, but not limited, to the demonstration of periplakin- and envoplakin-specific antibodies by ELISA, immunoprecipitation and/or immunoblotting as well as studies to identify the underlying tumour (Table 7) [52].
Table 7.
Diagnostic Criteria for Paraneoplastic Pemphigus
| Investigation | Finding |
|---|---|
| Clinic | Severe stomatitis, cheilitis, multiform lesions, acral distribution |
| Obligate association with neoplasia | |
| Histology | Intraepidermal acantholytic blisters and/or lichenoid inflammation |
| Direct immunofluorescence microscopy | Intraepidermal deposits of IgG (+/- C3) with an intercellular pattern Linear deposits of IgG and C3 at the basement membrane |
| Indirect immunofluorescence microscopy (esophagus) | Binding of IgG autoantibodies to epithelial cells with an intercellular pattern |
| Immunoprecipitation | Desmoglein 1,3, desmoplakin, envoplakin, periplakin, BP230, alpha-2-macroglobuline-like-1, plectin, desmocollins 1-3 |
| ELISA/Immunoblotting | IgG against envoplakin, periplakin, desmoglein 1, desmoglein 3 |
Histopathological examination can reveal intraepithelial separation with acantholysis and/or an interface dermatitis (Fig. 5b). Direct IF microscopy shows deposits of IgG and C3 with an intercellular pattern within the epidermis and also with a linear pattern along the basement membrane. By indirect IF microscopy serum IgG autoantibodies bind with an intercellular pattern on esophagus and may also stain the basement membrane zone. A more specific immunopathologic finding in PNP is the strong binding of IgG autoantibodies to the transitional epithelium of the bladder, which is rich in plakins [56].
The characterization of the molecular specificity of autoantibodies in PNP patients is is difficult because of the multiple targets of the paraneoplastic autoimmune responses. Autoantibodies recognize several keratinocyte proteins, including desmoglein 3 (130 kDa), desmoglein 1 (160 kDa), desmoplakin I (250 kDa), envoplakin (210 kDa), periplakin (190 kDa), bullous pemphigoid antigen 1 (BP230) (230 kDa), the protease inhibitor alpha-2-macroglobulin-like-1 (170 kD), and plectin (500 kDa) [13, 57-60]. Historically the gold standard for autoantibody detection in PNP was immunoprecipitation using radioactively-labeled keratinocytes, immunoblotting and ELISA using envo- and periplakin are also increasingly employed for diagnostic purposes (Table 2) [61, 62]. However, the fact that ELISA and immunoblotting necessitate different recombinant proteins as well as epidermal and keratinocyte extracts as substrates limits their use as time- and cost-effective tools for the PNP diagnosis.
IgA PEMPHIGUS
IgA pemphigus is a clinical pemphigus variant associated with IgA autoantibodies to the surface of keratinocytes [1]. The incidence and prevalence of IgA pemphigus are not known, but are certainly very low [63]. Patients with IgA pemphigus may present with different manifestations, usually assigned to a subcorneal pustular dermatosis or intraepidermal neutrophilic IgA dermatosis type of disease [63].
Circulating IgA autoantibodies in subcorneal pustular dermatosis type of IgA pemphigus target desmocollins [64, 65]. In contrast, the IgA autoimmune response in patients with intraepidermal neutrophilic dermatosis variant appears to be more heterogeneous. While desmogleins 1 and 3 may represent minor antigens [66-68], immunoelectron microscopy studies suggest that IgA autoantibodies in these patients recognize a not yet identified non-desmosomal transmembranous protein [69]. The pathogenic potential of the IgA autoantibodies have not yet been clearly demonstrated and, in the absence of animal models of the disease, the pathomechanisms of blister formation in IgA pemphigus are not fully understood [3, 70].
IgA pemphigus is clinically characterized by vesicles and pustules with a subacute clinical onset (Fig. 6a). The primary lesion is usually a vesicle or blister, which transforms into a pustule. The trunk and extremities are commonly involved, but lesions may also occur on the scalp, retroauricular and intertriginous areas [63].
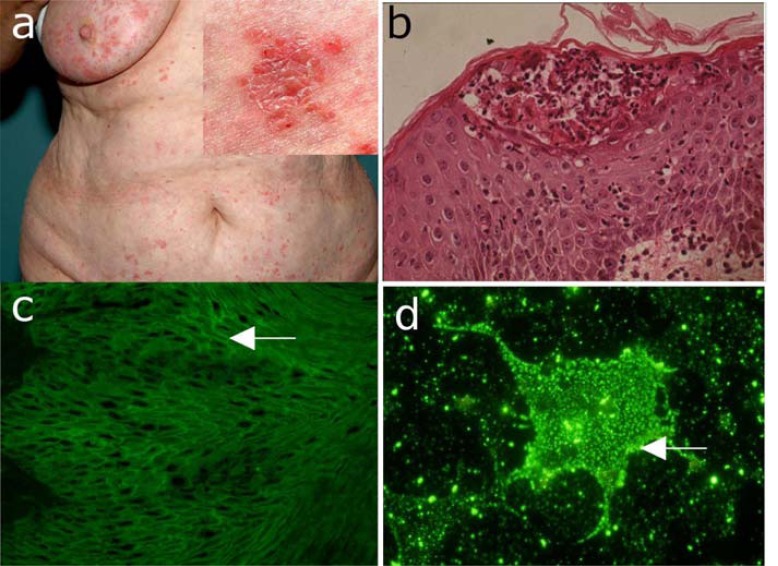
Fig. (6).
IgA pemphigus. (a) Clinical picture of a 56-year old woman with IgA pemphigus showing pustules on the abdomen. Inset: close-up view showing pustules, blisters, erosions, and crusts on an erythematous background. (b) Histopathological examination reveals subcorneal acantholysis with an inflammatory infiltrate consisting mainly of neutrophils. (c) IgA autoantibody binding with an intercellular pattern on monkey esophagus by indirect immunofluorescence (IF) microscopy. (d) Indirect IF microscopy using COS-7 cells transfected with desmocollin 1-cDNA as substrate reveals autoantigen-specific IgA serum autoantibodies.
IgA pemphigus should be suspected in patients with vesiculopustular lesions and neutrophil-rich intraepidermal cleavage by histopathology. Further work-up by direct IF reveals intercellular IgA deposition within the epidermis. Indirect IF microscopy on monkey esophagus allows the detection of circulating IgA autoantibodies. IgA autoantibodies in subcorneal pustular dermatosis-type disease may be detected by indirect IF microscopy on desmocollin 1-transfected COS-7 cells. The autoantigen(s) of intraepidermal neutrophilic dermatosis is still elusive, which has prevented the development of diagnostic molecular immunoassay for this subtype of IgA pemphigus (Table 8).
Table 8.
Diagnostic Criteria for IgA Pemphigus
| Investigation | Finding |
|---|---|
| Clinic | Vesiculopustular eruption. |
| Histology | Intraepidermal pustules with low acantholysis and neutrophilic infiltrates in the epidermis and upper dermis |
| Direct immunofluorescence (IF) microscopy | Epidermal IgA deposits with an intercellular pattern |
| Indirect IF microscopy (esophagus) | Binding of IgA autoantibodies to epithelial cells with an intercellular pattern |
| Indirect IF microscopy (desmocollin-transfected COS-7 cells)/ELISA | IgA autoantibodies against desmocollins 1-3 |
Typical histopathological findings of IgA pemphigus are intraepidermal pustules with a subcorneal localization or within the entire or mid epidermis associated with rare acantholysis and an infiltrate of neutrophil granulocytes in the upper dermis and epidermis (Fig. 6b).
Direct IF microscopy shows IgA deposition with an intercellular pattern in the epidermis, which is occasionally more pronounced in the upper layers. Weaker deposits for IgG and/or C3 with the same staining pattern may be also present. Indirect IF microscopy on monkey esophagus shows binding of IgA autoantibodies with an intercellular pattern (Fig. 6c). Since indirect IF microscopy has a sensitivity of about only 50% in IgA pemphigus, a more sensitive IF molecular assay has been developed using desmocollin-transfected COS-7 cells [65]. An ELISA using recombinant desmocollin has been developed, but its diagnostic sensitivity appears to be lower when compared with the indirect IF using desmocollin-transfected COS-7 cells [71]. Immunoblotting using a desmosome-enriched fraction of a bovine snout epidermal extract can be helpful to detect IgA autoantibodies against desmocollin, altough the sensitivity is similarly low [64]. Therefore, the overall importance of the immunoblotting for the IgA pemphigus diagnosis is limited and reserved to specialized laboratories.
PEMPHIGOID DISEASES
The pemphigoids are a heterogeneous group of subepidermal autoimmune blistering diseases associated with autoantibodies targeting components of the anchoring filaments [1]. The major clinical variants of the pemphigoid group include bullous pemphigoid (BP), pemphigoid gestationis (PG), linear IgA disease (LAD), mucous membrane pemphigoid (MMP) and anti-p200 pemphigoid with an approximate annual incidence of 7, 0.5, 0.5, 1 and undefined cases in one million, respectively [72-74].
BULLOUS PEMPHIGOID
Bullous pemphigoid (BP) is a subepidermal blistering disease characterized by autoimmunity against hemidesmosmes [75]. BP is the most common autoimmune blistering disease in North America and Western Europe [72-74]. A more recent population-based cohort study found the incidence of bullous pemphigoid to be 4.3 cases per 100,000 person-years in the United Kingdom [73]. BP was first described as a separate entity from pemphigus in 1953 by Lever [76]. While most cases are idiopathic, BP has been reported to be precipitated by ultraviolet irradiation, x-ray therapy, drugs (Table 3), and, particularly in children, following vaccination.
Autoantibodies in BP are mainly directed against the transmembrane hemidesmosomal antigens BP180/collagen XVII (bullous pemphigoid antigen of 180 kDa) and the intracellular plakin BP230 (bullous pemphigoid antigen of 230 kDa) [77, 78]. In a minority of BP patients, in addition to the reactivity to BP180 or BP230, further antigens, including plectin and α6 integrin, may be targets of autoantibodies [79, 80]. The transmembrane collagen XVII/BP180 shows a type II orientation with its non-collagenous N-terminus intracellularly located and a long extracellular domain consisting of 15 interrupted collagenous regions. The 16th non-collagenous (NC16A) domain is the immunodominant region of BP180 in BP and PG [81, 82]. Therefore, recombinant forms of this region are mainly used for detecting specific autoantibodies in approximately 85 % of the patients (Table 2). Extensive clinical and experimental evidence suggests that autoantibodies against BP180, rather than those directed against the intracellularly located BP230, induce skin blistering by inflammatory mechanisms involving activation of complement and granulocytes [3, 83].
The onset of BP may be either subacute or acute and is associated with intense pruritus. In some patients, BP shows a prodromal stage with persistent urticarial or eczematous lesions [84]. Clinically, patients with full-blown BP present with generalized inflammatory skin blistering. Typically, tense blisters, which heal without scarring or milia formation, arise on an erythematous or urticarial background, on the distal extremities, the trunk and intertriginous areas (Fig.7a). A localized variant of BP, often triggered by local trauma [85-90] or radiotherapy [91], may be seen in a subset of patients. Involvement of the oral and ocular mucosa is uncommon and, when present, of minor clinical significance. Different rare clinical variants of BP are summarized in Table 9.
Fig. (7).
Bullous pemphigoid. (a) Blisters, erosions with crusts on an erythematous background in a 72-years old male patient with bullous pemphigoid. Inset: close-up view of blistering skin. (b) The histopathological examination reveals subepidermal cleavage with a inflammatory infiltrate consisting predominantly of eosinophils and neutrophils. (c) Direct immunofluorescence microscopy of perilesional skin shows C3c deposition at the dermo-epidermal junction of a patient with bullous pemphigoid. (d) Serum IgG autoantibodies from a bullous pemphigoid patient binding at the epidermal side of 1M NaCl-split skin by indirect immunofluorescence microscopy (all magnification 200x).
Table 9.
Clinical Variants of Bullous Pemphigoid (BP)
| Clinical Form | Characteristic Findings | References |
|---|---|---|
| Infant/childhood BP | Bullae on erythematous background in infancy | [231, 232] |
| Pemphigoid nodularis | Prurigo nodularis lesions associated with tissue-bound and circulating pemphigoid autoantibodies |
[233-235] |
| Erythrodermic pemphigoid | Erythroderma associated with with tissue-bound and serum pemphigoid autoantibodies |
[236, 237] |
| Dyshidrosiform pemphigoid | Dyshidrosiform palmoplantar lesions associated with tissue-bound and circulating pemphigoid autoantibodies |
[238, 239] |
| Vegetating pemphigoid | Erythematous, erosive, and vegetating plaques in intertriginous areas associated with tissue-bound and circulating pemphigoid autoantibodies |
[240] |
| Lichen planus pemphigoides | Lichen planus-like papules with blisters associated tissue-bound and serum pemphigoid autoantibodies |
[241-244] |
BP should be suspected in elderly patients presenting with generalized, itchy erythematous papules urticaria and/or skin blisters, which are subepidermal and associated with inflammatory cell infiltrates dominated by eosinophil or neutrophil granulocytes. Demonstration of linear deposits of IgG and C3 at the dermal-epidermal junction of patients' perilesional skin and circulating IgG autoantibodies binding to the epidermal side of 1 M NaCl-split skin by indirect IF microscopy confirms the diagnosis of a pemphigoid disease. Measurement of circulating autoantibodies against BP180 and BP230 by ELISA is helpful for diagnosis and may be used for disease monitoring and guiding management decisions (Table 10).
Table 10.
Diagnostic Criteria for Bullous Pemphigoid
| Investigation | Finding |
|---|---|
| Clinic | Tense blisters, erythematous plaques, pruritic papules. |
| Histology | Sub-epidermal blister with a inflammatory infiltrate consisting predominantly of eosinophils and neutrophils |
| Direct immunofluorescence microscopy | Linear C3 and IgG deposits at the dermo-epidermal junction |
| Indirect immunofluorescence microscopy on salt-split-skin | Binding of IgG autoantibodies to the epidermal side |
| ELISA / Immunoblot | BP180- and/or BP230-specific IgG autoantibodies |
Histopathology analysis of patients’ lesional skin reveals a subepidermal cleavage typically associated with a dense inflammatory infiltrate dominated by neutrophils and eosinophils (Fig. 7b). In some BP patients, dermal-epidermal separation is associated with only sparse infiltrates of inflammatory cells. The mechanisms of blister formation in this “paucicellular form” of BP have not yet been investigated [83].
By direct IF microscopy of patients’ perilesional skin, linear deposits of C3 and IgG are detected at the dermal-epidermal junction (Fig. 7c). Indirect IF microscopy on salt-split skin reveals circulating autoantibodies binding to the epidermal side of the artificially cleaved substrate (Fig. 7d). This technique allows to efficiently differentiate BP from several subepidermal autoimmune blistering diseases with autoantibodies binding to the dermal side of salt-split skin [10, 11].
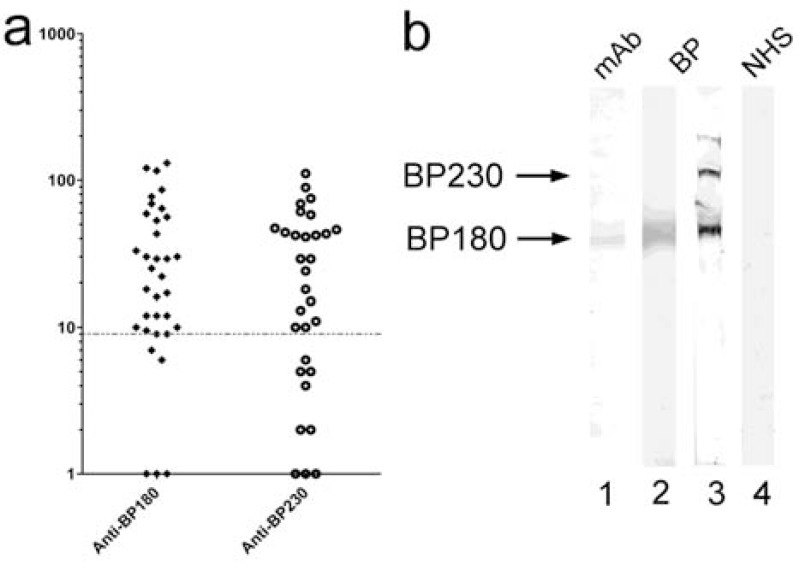
Currently, ELISA systems using recombinant BP180 and BP230 are widely employed to characterize the molecular specificity of IgG autoantibodies in BP patients (Table 2; Fig. 8a) [62, 92, 93]. IgE autoantibodies against BP180 appear to correlate with disease activity and may be useful for diagnosis and monitoring [94-96]. Alternatively, BP180- and BP230-specific IgG autoantibodies may be detected by immunoblotting using epidermal or keratinocyte extracts (Fig. 8b) [1].
Fig. (8).
Molecular specificity of autoantibodies in bullous pemphigoid (BP). (a) Sera from patients with BP were tested by ELISA using a recombinant form of the 16th noncollagenous (NC16) A domain of the bullous pemphigoid (BP) antigen 180 and with recombinant BP230 as described [92, 93]. The dotted line represents the cut-off of the assay. (b) An extract of cultured keratinocytes was fractionated by 7.5% SDS-PAGE, transferred to nitrocellulose, and incubated with a BP180-specific monoclonal antibody (lane 1), serum from patients with BP (lanes 2–3), and serum from a healthy control (NHS; lane 4). The BP serum in lane 2 reacts with bullous pemphigoid antigen 180 (BP180, 180kDa, lower arrow) only. The BP serum depicted in lane 3 reacts with both bullous pemphigoid antigen 230 (BP230, 230 kDa, upper arrow) and BP180. Control serum shows no specific reactivity (lane 4).
PEMPHIGOID GESTATIONIS
PG is a rare blistering disease occurring during pregnancy or gestational trophoblastic diseases and is characterized by autoimmunity against hemides-mosomal proteins [97]. Its incidence is approximately 1 in 20,000 to 50,000 pregnancies. PG is associated with HLA-DR3 (61-80%) and HLA-DR4 (52%), or both (43-50%), and virtually all patients with a history of PG have demonstrable anti-HLA antibodies. PG patients show autoantibodies against BP180 and, less frequently, against BP230 [78, 98, 99]. These serum autoantibodies, initially designated as the herpes gestationis factor, mainly belong to the IgG1 subclass and activate the complement system by the classical activation pathway ex vivo [100-102]. Interestingly, the autoantibody response in PG patients is more restricted to epitopes within the BP180-NC16A compared with BP [103]. Existing clinical and experimental evidence suggests that binding of BP180-specific autoantibodies to the basement membrane triggers the activation of Fcγ-dependent inflammatory pathways resulting in tissue damage and subepidermal blister formation [3].
Clinically, PG is characterized by an acute onset of itchy urticarial papules, vesicles and blisters on the abdomen and trunk, which typically occur during late pregnancy or the immediate post-partum period and worsen with subsequent pregnancies [104]. Usually, patients experience intense, relentless pruritus, which often interferes with daily activities. Symptoms can fade near the end of pregnancy, but extensive flares at or immediately after delivery are not uncommon. PG usually resolves spontaneously within weeks to months after delivery, but persistence of disease activity for years post-partum has also been reported [105, 106]. In up to 10% of the newborn babies of PG patients a mild rash may develop, which resolves spontaneously in several weeks [107, 108].
PG should be suspected in all pregnant women with pruritic dermatoses. The immunopathological findings, which are similar to those of BP, allow PG to be distinguished from other pregnancy dermatoses, such as from pruritic urticarial papules and plaques of pregnancy, prurigo of pregnancy, allergic contact dermatitis, and drug eruptions [109-111]. The diagnosis of PG is basically made by demonstrating a pemphigoid in a pregnant patient. Thus, BP and PG share essentially the same diagnostic criteria and monitoring tools (Table 9).
In patients with bullous PG, subepidermal cleavage and a rich inflammatory infiltrate dominated by eosinophils are found by routine histopathological analysis. Direct IF microscopy typically reveals strong linear C3 deposits at the basement membrane zone in perilesional skin biopsy. IgG deposits are less intense and may not be detected in over 50% of the patients. The binding of IgG autoantibodies to the epidermal side of the salt-split is demonstrated by indirect IF microscopy. Indirect IF microscopy may be also used to assess the ability of circulating autoantibodies to fix complement ex vivo. The test is performed by incubating of cryosections of normal human skin with patient serum, followed by addition of fresh human normal serum as a source of complement [100, 101, 112]. Although detection of complement-fixing autoantibodies in PG patients by the complement-binding test is highly sensitive, the method is not widely used in the routine diagnosis [10].
Autoantibodies against BP180 in PG may be detected by immunoblotting using epidermal and keratinocyte extracts and ELISA using recombinant forms of the NC16A domain of BP180 [112].
MUCOUS MEMBRANE PEMPHIGOID
Mucous membrane pemphigoid (MMP) is an autoimmune blistering disease involving the mucosae and potentially also the non-mucosal skin [1, 113]. Scarring of the mucous membranes in MMP is common, hence the previous designation cicatricial pemphigoid, and may lead to severe life-threatening sequelae. Oral, nasal, ocular, laryngeal, esophageal and anogenital mucosal membranes may be involved. In a subset of patients showing IgG reactivity to laminin 332 a significant association with neoplasia has been reported [114]. Typically, a more aggressive immunosuppressive regimen is required to halt disease progression.
Autoantibodies of different isotypes, including different IgG subclasses and IgA target several autoantigens of the dermal-epidermal junction, including BP180 [115, 116], BP230 [117], laminin 332 [14], α6β4 integrin [118] and collagen VII [119, 120]. Circulating autoantibodies in individual patients are usually directed to a single target antigen. Approximately 2/3 of the MMP patients demonstrate autoantibodeis against BP180 and up to 1/3 against laminin 332 [117, 121]. The occurrence of autoantibodies against α6β4 integrin in MMP has been repeatedly reported, but their prevalence is unknown [122, 123].
MMP is characterized by bullous lesions of the mucous membranes and, less commonly the skin, associated with moderate pruritus or burning sensation. The ensuing erosions are often painful, heal poorly with scarring. The clinical manifestations of MMP are heterogenous and dependent on the mucosal site involved [124]. Oral and conjunctival membranes are most commonly affected. Involvement of the oropharynx may result in hoarseness or dysphagia. Esophageal lesions with progressive scarring disease may lead to stenosis. Patients with ocular involvement may present with pain or with the sensation of grittiness in the eye, conjunctivitis and/or erosions. Patients often present after ocular surgery, especially for cataracts. Early changes include keratinization of the conjunctiva and shortening of the fornices. Later, patients develop entropion with subsequent trichiasis. With progressive scarring, patients may develop symblepharon, synechiae, and ankyloblepharon. Lacrimal gland and duct involvement leads to decreased tear and mucous production leading to ocular dryness and further trauma. The ultimate sequelae of ocular involvement are opacification and blindness. Nasal involvement may manifest as epistaxis, nasal crusting, and discomfort. Other mucosal sites, such as the perianal area or the genitalia, may be involved causing strictures and urogenital dysfunction.
Skin lesions develop in approximately one third of patients with MMP, manifesting as tense vesicles or bullae that may be hemorrhagic or pruritic. Blisters may heal with scarring or milia. Scalp involvement may lead to alopecia.
A chronic recurrent vesiculobullous eruption that heals with scarring and occurs predominantly on the head and neck without significant mucosal involvement was initially designated as Brunsting-Perry pemphigoid [125]. However, the histologic, immunofluorescence and immunoelectron microscopic features in patients with this clinical variant do not differ compared with other MMP variants [125].
The diagnosis of MMP should be considered in all cases of chronic erosions or blistering of mucosal surfaces, especially when associated with scarring and progressive function loss. The diagnosis is confirmed by demonstration of IgG and C3 deposits at the basement membrane by direct IF microscopy. A negative indirect IF microscopy does not exclude the diagnosis of MMP because often the autoantibody titers are too low to be detected by this method. Characterization of the molecular specificity of autoantibodies has important clinical consequences and may be performed by ELISA or immunoblotting (Table 11).
Table 11.
Diagnostic Criteria for Mucous Membrane Pemphigoid
| Investigation | Finding |
|---|---|
| Clinic | Mucosal erosions and ulcers with scarring |
| Histology | Subepithelial cleavage with sparse mixed leucocytic infiltrate |
| Direct immunofluorescence microscopy | Linear IgG and C3 deposits at the dermo-epidermal junction |
| Indirect immunofluorescence microscopy on salt-split-skin | IgG/IgA binding on the epidermal or dermal side |
| ELISA / Immunoblot | IgG/IgA autoantibodies specific to BP180, laminin 332, Α6Β4 integrin |
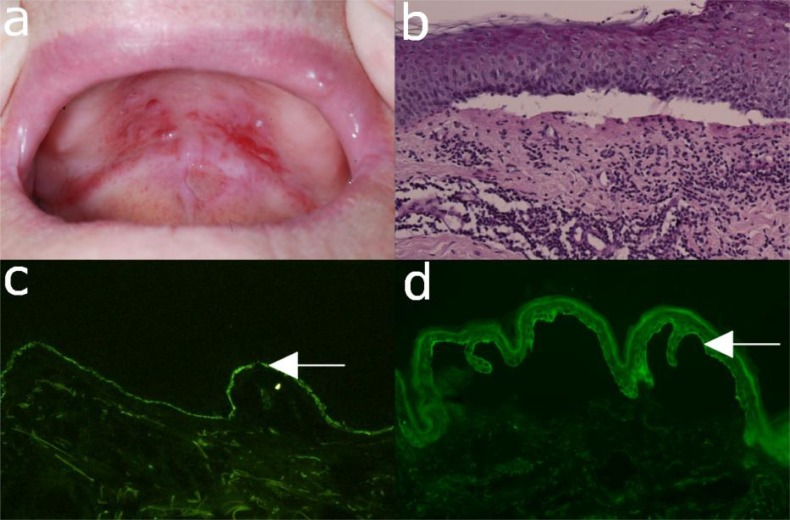
Histopathological examination of patients’ lesional skin reveals subepidermal blisters and a mixed inflammatory infiltrate. Commonly, monocytes, histiocytes, plasma cells as well as eosinophils and neutrophils are seen in mucosal biopsies (Fig. 9b) [126].
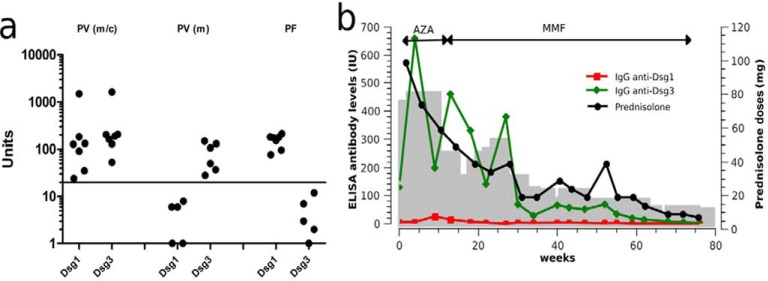
Fig. (9).
Mucous membrane pemphigoid. (a) Buccal erosions in a 77-year old female with mucous membrane pemphigoid. (b) Histopathological examination of mucosa reveals a sub-epidermal blister and a mixed leukocytic infiltrate. (c) Direct immunofluorescence microscopy shows IgG deposits at the dermo-epidermal junction of a patient with mucous membrane pemphigoid. (d) Serum IgG autoantibodies binding to the epidermal side of 1M NaCL-split skin by indirect immunofluorescence microscopy (magnification 200x).
Direct IF microscopy of perilesional skin reveals continuous IgG, C3 or IgA deposition along the epidermal basement membrane (Fig. 9c). Indirect IF microscopy on 1 M NaCl-split human skin may show binding of IgG and/or IgA on the epidermal or dermal side of the cleavage, but is often negative due to low serum reactivity in MMP (Fig. 9d) [1, 10]. Immunoprecipitation, immunoblotting and ELISA are important assays in the diagnosis of MMP because about 50% of the patients’ sera show negative results in indirect IF microscopy on 1 M NaCl separated human skin. Immunoprecipitation of cultured keratinocytes for detection of serum antibodies to laminin 332 as well as immunoblotting with extracellular matrix of cultured human kerytinocytes or purified laminin 332 are highly sensitive and may be used for antibody detection [127]. Autoantibodies are mainly directed against the a3 chain of laminin 332 [128]. In two case series of MMP with a6b4 integrin reactivity, patients with mainly oral involvement show autoantibodies to a6 integrin, whereas ocular pemphigoid is associated with reactivity to b4 integrin [129, 130].
LINEAR IgA DISEASE
Linear IgA disease (LAD) is a subepidermal blistering disease characterized by linear IgA deposits along the epidermal basement membrane zone. It was first described in 1901 by Bowen, but not recognized as separate entity until 1979, when it was separated from dermatitis herpetiformis (DH) [131]. LAD has two peaks of onset; it is the most frequent autoimmune blistering disease in children, but also occurs in adults. Occasionally, LAD appears to be triggered by administration of drugs, most commonly vancomycin (Table 3) [132].
LAD is clinically and immunopathologically a heterogenous disease and may actually represent a group of IgA-mediated subepidermal autoimmune blistering disorders rather than a single nosologic entity. While in most patients, IgA autoantibodies bind to the epidermal side of the salt-split skin by IF microscopy, staining of the dermal side of the artificial split may be also detected. Different target antigens of the lamina lucida-type of LAD have been reported, including a 97 kDa protein (LABD97) extracted from epidermis [133] and a 120 kDa polypeptide (LAD-1) secreted into the medium of cultured human keratinocytes [134, 135]. Based on biochemical studies and peptide sequence analyses, it was subsequently shown that LABD97 and LAD-1 are proteolytic cleavage products of the BP180 ectodomain [136, 137]. Based on cumulative findings of the last decades, the name IgA pemphigoid was suggested to be a more adequate designation for the lamina lucida-type of LAD [138]. The lamina densa-type of LAD is characterized by IgA autoantibodies recognizing dermal proteins of 180 and 285 kDa [86]. Since in some patients, IgA antibodies were shown to bind to the anchoring fibrils and to specifically recognize collagen VII, a new term of IgA-mediated epidermolysis bullosa acquisita (EBA) was proposed for this subtype of linear IgA disease [139].
The pathomechanisms of subepidermal blister formation by IgA autoantibodies are poorly understood [3]. Very recently, it was shown that IgA autoantibodies from patients with LAD induce granulocyte-dependent dermal-epidermal separation in cryosections of human skin [140].
The clinical presentation of LAD is heterogeneous and may mimic other autoimmune blistering diseases such as bullous pemphigoid and dermatitis herpetiformis. Cutaneous manifestations in patients with LAD include erythematous papules, urticarial plaques or vesicobullous eruptions. Lesions may appear as tense arciform bullae in a ‘cluster of jewels’ configuration or as grouped papulovesicles. Frequently, LAD patients develop mucosal involvement with oral and/or ocular erosions (Fig. 10a) [1].
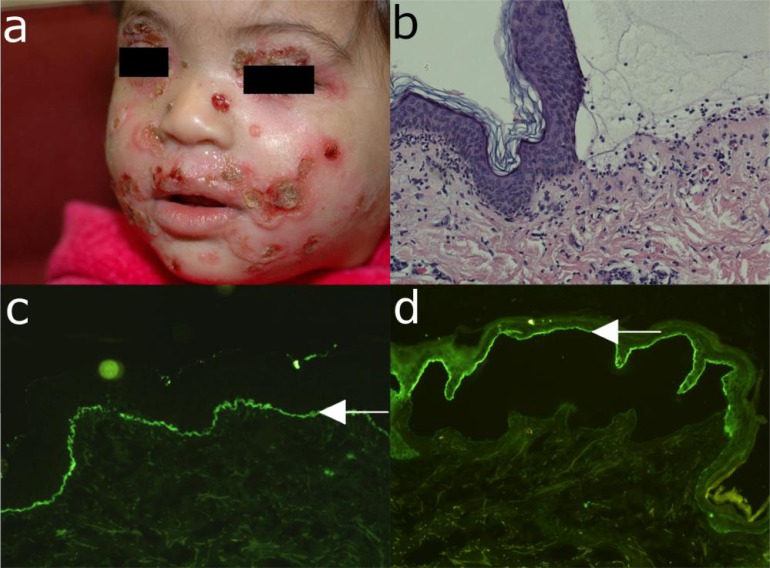
Fig. (10).
Linear IgA disease. (a) Erythema, blisters, erosions and crusts in a 4-year old child with linear IgA disease. (b) Histopathological examination reveals subepidermal cleavage and a rich inflammatory infiltrate dominated by neutrophils. (c) Direct immunofluorescence microscopy analysis of perilesional skin shows linear IgA deposition at the dermo-epidermal junction. (d) Serum IgA-autoantibodies bind to the epidermal side of 1M NaCl-split skin by indirect immunofluorescence microscopy (all magnification 200x).
LAD should be suspected in all children with blistering skin diseases and in adults with grouped tense blisters or erosions. The diagnosis is made by demonstrating linear IgA deposits at the dermal-epidermal junction by direct IF microscopy (Table 12). Further characterization of the molecular target of the IgA autoantibodies by indirect IF microscopy on salt-split skin, immunoblotting and ELISA is essential for an exact diagnosis and may have prognostic and therapeutic implications (Table 2).
Table 12.
Diagnostic Criteria for Linear IgA Disease
| Investigation | Finding |
|---|---|
| Clinic | Polymorphic picture with erythema, blisters, erosions on skin and mucosa |
| Histology | Subepidermal blisters, neutrophils accumulating at the papillary tips |
| Direct immunofluorescence microscopy | Linear IgA deposits at the dermo-epidermal junction |
| Indirect immunofluorescence microscopy (salt-split-skin) | Binding of IgA autoantibodies to the epidermal side |
| ELISA / Immunoblot | IgA against the shed ectodomain of BP180 (LAD-1) |
Histopathological examination reveals subepidermal cleavage and a dense inflammatory infiltrate mainly consisting of neutrophils (Fig. 10b). Direct IF microscopy reveals linear IgA deposition along the epidermal basement membrane (Fig. 10c). By indirect IF microscopy on 1 M NaCl-split skin, IgA autoantibodies from LAD patients bind to the epidermal or dermal side of the split (Fig. 10d).
The molecular specificity of IgA autoantibodies may be further characterized by ELISA and immunoblotting. Immunoblotting using concentrated supernatant of cultured keratinocytes or recombinant BP180 ectodomain is a highly sensitive method to detect IgA autoantibodies against the shed ectodomain of BP180 (Fig. 11a) [134, 138, 141]. Detection of collagen VII-specific IgA autoantibodies requires the use of dermal extracts or recombinant collagen VII as substrate for immunoblotting [139, 142]. ELISA systems using recombinant BP180 and collagen VII have been developed for measuring IgG and IgA autoantibodies (Fig. 11b) [138].
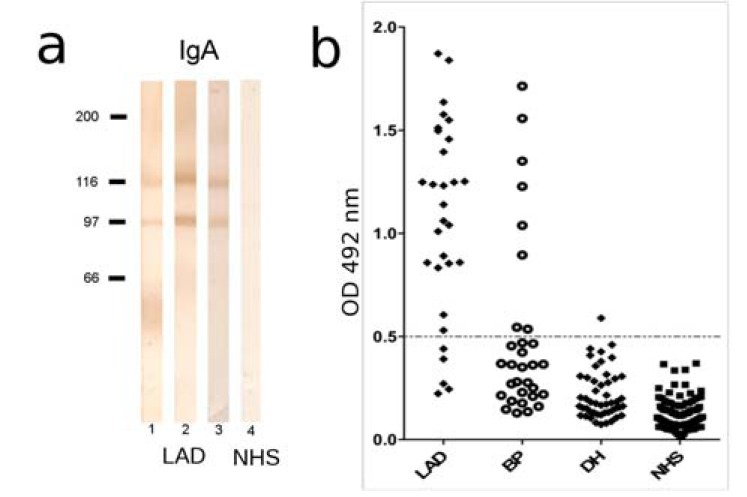
Fig. (11).
Molecular specificity of IgA autoantibodies in pemphigoid diseases. (a) Spent medium of cultured keratinocytes was concentrated by ammonium sulfate precipitation, electrophoretically separated by 8% SDSPAGE, transferred on nitrocellulose and immunoblotted with serum from linear IgA disease (LAD) patients (lanes 1-3) and control serum (NHS) (lane 4). Bound autoantibodies were visualized using a peroxidase-labeled secondary antibody specific for human IgA. The shed ectodomain of BP180 of 120 kDa (LAD-1) and its 97 kDa degradation product (LABD97) are indicated by arrow and arrow head, respectively. (b) ELISA reactivity with the recombinant BP180 ectodomain of IgA autoantibodies from LAD, bullous pemphigoid (BP), dermatitis herpetiformis (DH) patients and age-matched, healthy donors (NHS). The cut-off of the assay is represented by a dashed line. Scatter plot adapted from [138].
ANTI-p200 PEMPHIGOID
Anti-p200 pemphigoid is an autoimmune subepidermal blistering disease, characterized by autoantibodies against a 200-kDa protein (p200) of the epidermal basement membrane, recently identified as the laminin γ1 chain [143-145]. Clinically, most reported cases present with tense blisters and urticarial eruptions, which resemble BP or the inflammatory form of EBA. These patients show IgG and C3 deposits at the dermal-epidermal junction by direct IF microscopy and circulating IgG autoantibodies staining the dermal side of salt-split skin by indirect IF microscopy [143, 144]. By immunobloting, these autoantibodies recognize a protein of 200 kDa in dermal extract [143, 144].
Research of the last two decades provided extensive evidence that p200 is distinct from all other known autoantigens within the dermal–epidermal anchoring complex, including collagen XVII/BP180, BP230, α6β4 integrin, laminin 332, and collagen VII [146, 147]. Recent studies using dermal extracts separated by 2D electrophoresis followed by mass spectrometry analysis of proteins spots recognized by the patients' sera identified laminin γ1 chain as the target autoantigen [144]. Interestingly, patients with anti-p200 pemphigoid show skin blisters, but show no pathology in other organs, although laminin γ1 is widely expressed in different basement membrane zones. A likely explanation of this finding is that laminin γ1 in the epidermal basement membrane zone may have different posttranslational modifications, such as glycosylation, compared with laminin γ1 expressed in blood vessels. Differences in posttranslational modification may allow further possible explanations for the organ specificity of the disease [144, 145]. The pathogenicity of laminin γ1-specific autoantibodies has not yet been demonstrated in ex vivo or animal models [148].
Anti-p200 pemphigoid should be suspected in patients with inflammatory autoimmune subepidermal blistering diseases, especially in cases with BP-like appearance and circulating IgG autoantibodies staining the dermal side of salt-split skin by indirect IF microscopy. The diagnosis is confirmed by detecting autoantibodies against a 200 kDa protein or recognizing laminin γ1 by immunoblotting with dermal extracts or ELISA with recombinant protein, respectively (Table 13).
Table 13.
Diagnostic Criteria for Anti-p200 Pemphigoid
| Investigation | Finding |
|---|---|
| Clinic | Widespread bullous-pemphigoid-like blistering |
| Histology | Subepidermal cleavage with neutrophilic infiltrate |
| Direct immunofluorescence microscopy | Linear IgG and C3 deposits at the dermal-epidermal junction |
| Indirect immunofluorescence microscopy on salt-split-skin | Linear binding at the dermal side of the dermal-epidermal junction |
| ELISA / immunoblot | Laminin Γ1-specific IgG |
The histopathology of anti-p200 pemphigoid reveals subepidermal cleavage usually associated with a dense inflammatory infiltrate dominated by neutrophils. In a few patients, eosinophilic granulocytes may be present within the inflammatory infiltrate, resulting in a microscopic appearance suggestive of BP [149].
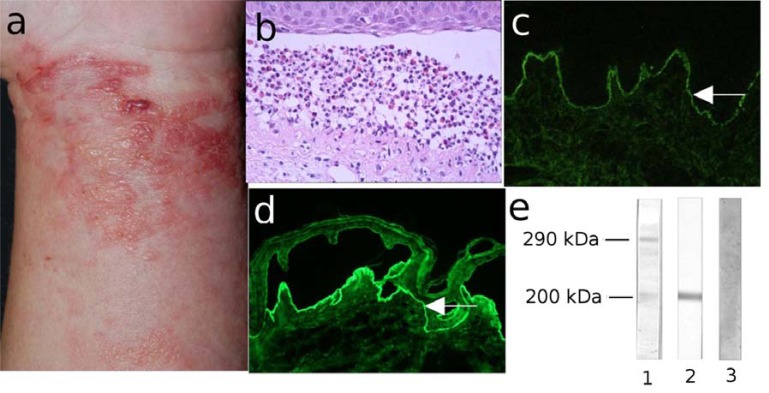
Direct IF microscopy of perilesional skin biopsies from patients with anti-p200 pemphigoid shows linear deposits of IgG and C3 along the epidermal basement membrane (Fig. 12b). Serum IgG autoantibodies binding to the dermal side of the salt-split are demonstrated by indirect IF microscopy (Fig. 12c). By immunoblotting, sera from all patients with anti-p200 pemphigoid recognize a 200-kDa protein (p200) in dermal extracts (Fig. 12d). Autoantibodies against laminin γ1 may be measured by ELISA using a recombinant form of the C-terminus of the antigen (Table 2) [150].
Fig. (12).
Anti-p200 pemphigoid (a) Erythema, blisters, erosions and crusts in a 53-year old patient with anti-p200 pemphigoid. (b) Histopathological examination reveals subepidermal cleavage and a neutrophil-rich inflammatory infiltrate. (c) Direct immunofluorescence (IF) microscopy analysis of perilesional skin shows linear IgG deposition at the dermo-epidermal junction. (d) Serum IgG autoantibodies bind to the dermal side of 1M NaCl-split skin by indirect IF microscopy (all magnification 200x). (e) Dermal extracts were separated by 6% SDS-PAGE, transferred on nitrocellulose and immunoblotted with serum from patients with epidermolysis bullosa acquisita (EBA; lane 1), anti-p200 pemphigoid (p200; lane 2) and normal human serum (NHS, lane 3).
EPIDERMOLYSIS BULLOSA ACQUISITA
Epidermolysis bullosa acquisita (EBA) is a severe chronic blistering disease of skin and mucous membranes characterized by subepidermal blisters and tissue-bound and circulating autoantibodies against collagen VII, the main constituent of anchoring fibrils [1, 151]. The yearly incidence of EBA is at least 0.2%/year/million and is present in about 5% of unselected patients with subepidermal blistering diseases and autoantibodies against the epidermal basement membrane zone. EBA is a clinically heterogeneous disease which may present with an inflammatory or non-inflammatory phenotype [1, 152]. The blister-inducing potential of autoantibodies against collagen VII has been clearly demonstrated and mutually complementary ex vivo and animal models have been established for this disease [153].
Mechanobullous form of EBA may show features highly reminiscent of hereditary dystrophic epidermolysis bullosa, a disease caused by genetic defects in collagen VII. This form is characterized by extreme skin fragility, trauma-induced blisters and erosions localized to the extensor skin surface, healing with scars and milia. The inflammatory subtype of EBA was described, clinically mimicking BP or LAD (Fig. 13a). EBA patients presenting with an inflammatory phenotype at the onset can later manifest with non -inflammatory features [154, 155].
Fig. (13).
Diagnostic features of epidermolysis bullosa acquisita (EBA). (a) Clinical picture of a 61-year old female patient with the inflammatory form of EBA showing erythema, tense blisters, erosions and crusts on the lateral abdomen. (b) Histopathology analysis of the lesional skin shows dermal-epidermal separation and a neutrophil-rich inflammatory infiltrate. (c) Direct immunofluorescence microscopy of perilesional skin reveals deposits of IgG along the basement membrane zone. (d) Indirect immunofluorescence microscopy on 1M NaCl split-skin shows binding of IgG autoantibodies to the dermal side of the dermal-epidermal junction (magnification 200x).
The involvement of mucosal surfaces, especially in the oral cavity, but also of the nasal, conjunctival, pharyngeal, and laryngeal mucosae, is present in the majority of EBA patients [156]. Although often subclinical, the spectrum of mucosal involvement in EBA resembles MMP and can lead to similar complications, including ankyloglossia, periodontal disease, scarring and crusting of nasal mucosa, symblepharon, obstruction of nasolacrimal ducts, deformation of the epiglottis, impaired phonation, dysphagia, esophageal strictures, and supraglottic stenosis requiring emergency tracheostomy [156]. EBA is often associated with inflammatory bowel disease and a significant percentage of patients with Crohn disease or ulcerative colitis show collagen VII-specific autoantibodies [157].
The diagnosis of EBA should be suspected in adult patients with skin fragility, trauma-induced blisters, scarring, milia and nail dystrophy. The inflammatory form of EBA may be clinically and histopathologically indistinguishable from other pemphigoid diseases. The diagnosis of EBA in all patients is made by demonstrating IgG or IgA autoantibodies against the dermal side of salt-split skin by indirect IF microscopy, which recognize collagen VII as detected by ELISA or immunoblotting (Table 14).
Table 14.
Diagnostic Criteria for Epidermolysis Bullosa Acquisita
| Investigation | Finding |
|---|---|
| Clinic | Non-inflammatory form: skin and mucosal fragility, trauma-induced blistering on predilection sites, scarring, skin atrophy, milia formation |
| Inflammatory form: bullous pemphigoid-like generalized eruption with tense blisters on an erythematous background | |
| Histology | Subepidermal bullae with neutrophilic or sparse inflammatory infiltrate |
| Direct immunofluorescence (IF) microscopy | Linear IgG and C3 deposits at the dermal-epidermal junction |
| Indirect IF microscopy (salt-split-skin) | Linear binding at the dermal side of the dermal-epidermal junction |
| ELISA / immunoblot | Collagen VII-specific IgG or IgA |
Histopathological examination of patients’ lesional skin reveals subepidermal cleavage associated with neutrophilic infiltrates of variable densities in the upper dermis (Fig. 13b). By direct IF microscopy, linear IgG and C3 deposits are found along the epidermal basement membrane (Fig. 13c). Indirect IF microscopy on human salt-split skin reveals circulating IgG and/or IgA autoantibodies binding to the blisters floor (Fig. 13d).
Autoantibodies from EBA patients recognize collagen VII of 290 kDa or its immunodominant region, the non-collagenous domanin 1, by immunoblotting with dermal extracts or recombinant protein, respectively. ELISA systems using different recombinant form of collagen VII for detection of specific autoantibodies have been developed and are commercially available (Table 2) [158-161].
DERMATITIS HERPETIFORMIS
Dermatitis herpetiformis (DH) is a chronic subepidermal blistering skin disease characterized by pruritic papulo-vesicular lesions, typical immunopathological findings, and clinically a good response to sulfone therapy [162, 163]. DH is associated with distinct HLA haplotypes (DR3 and Dqw2) and is currently regarded as a specific skin manifestation of celiac disease [162-164].
DH patients present with diffuse, symmetrical, grouped polymorphic lesions consisting of erythema, urticarial plaques, papules, clustered herpetiform vesicles and erosions. The most commonly involved sites are the extensor surfaces of the elbows (90%), knees (30%), shoulders, buttocks, sacral region, and face (Fig. 14a). The skin lesions commonly associate with and may be preceded by intense itching and/or burning sensation causing excoriations [163, 165]. The associated gluten-sensitive enteropathy in DH is often asymptomatic or may manifest with abdominal pain, diarrhoea, iron deficiency and reduced growth rates in children [163, 165].
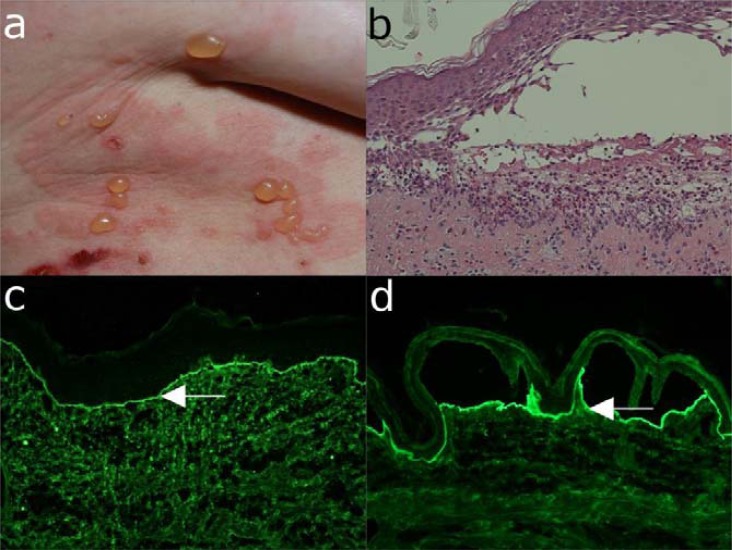
Fig. (14).
Major clinical, histo- and immunopathological features of dermatitis herpetiformis. (a) Multiple excoriated papules, erosions and crusts on the elbow of a 44-year old patient with dermatitis herpetiformis. (b) Histopathological examination shows infiltration of neutrophils with incipient formation of papillary microabscesses and dermal-epidermal separation. (c) Direct immunofluorescence microscopy of a biopsy of non-affected skin reveals granular IgA deposits at the basement membrane. (d) By indirect immunofluorescence microscopy on monkey esophagus, anti-endomysial IgA antibodies are detected in the serum of a patient with dermatitis herpetiformis.
DH is a subepidermal autoimmune blistering disease associated with a gluten-sensitive enteropathy and with characteristic granular IgA deposits in the upper dermis. In its prebullous stage, DH may present with only pruritus and excoriations and should be distinguished from other pruritic dermatoses, including atopic dermatitis, scabies, papular urticaria, impetigo, acute dermatitis, nodular prurigo, urticaria and polymorphic erythema by performing a direct IF microscopy analysis. Serological tests confirm the diagnosis and are very useful to clearly differentiate DH from other autoimmune blistering diseases such as LAD and BP. In addition, the remission of disease under gluten-free diet and disease relapses or flares
induced by gluten ingestion represent a true “ex juvantibus” diagnostic criterion of DH (Table 15).
Table 15.
Diagnostic Criteria for Dermatitis Herpetiformis
| Investigation | Finding |
|---|---|
| Clinic | Symmetrically distributed, eroded and crusted papulo-vesicles or blisters on the extensor surfaces and buttocks. Intense itching. |
| Histology | Subepidermal separation, granulocytes (mainly neutrophils and few eosinophils) with formation of papillary microabscesses |
| Direct immunofluorescence (IF) microscopy | Granular IgA deposits at the epidermal basement-membrane (accentuation at the tips of dermal papillae) |
| Indirect IF microscopy (monkey esophagus) | Anti-endomysial IgA antibodies |
| ELISA | IgA specific for epidermal/tissue transglutaminase |
Histopathological examination in patients' lesional skin reveals an inflammatory infiltrate in the upper dermis and at the dermo-epidermal junction dominated by neutrophils and eosinophils. These granulocytes form typical papillary microabscesses which then lead to blister formation in these areas (Fig. 14b).
Direct IF microscopy from biopsies of uninvolved skin provide optimal results in DH and reveal granular deposits of IgA along the basement membrane, usually with accentuation in the dermal papillae (Fig. 14c). Serum IgA autoantibodies reacting with endomysium may be detected in indirect IF microscopy on monkey esophagus (Fig. 14d). IgA autoantibodies specifically recognize the epidermal transglutaminase (TG3) and cross-react with tissue transglutaminase (TG2) and are a useful marker of bowel damage and diet adherence in DH/celiac disease patients (Table 2) [166, 167].
These diagnostic measures, especially when the immunopathologic tests are partly negative, but strong suspicion of DH remains, may be complemented by an aggressive gluten challenge after a gluten-free diet for at least 1 month. Triggering a flare of the skin eruption in 1-2 days by this “ex juvantibus” test provides a strong further support for a diagnosis of DH [165].
Although not essential for diagnosis, a series of ancillary investigations may be performed for a more accurate global assessment of the patient with DH, including a small bowel biopsy, HLA testing, screening for autoimmune diseases (e.g., thyroid, antinuclear, and citrullinated peptide-specific autoantibodies) and evaluation of malabsorption [165, 168, 169].
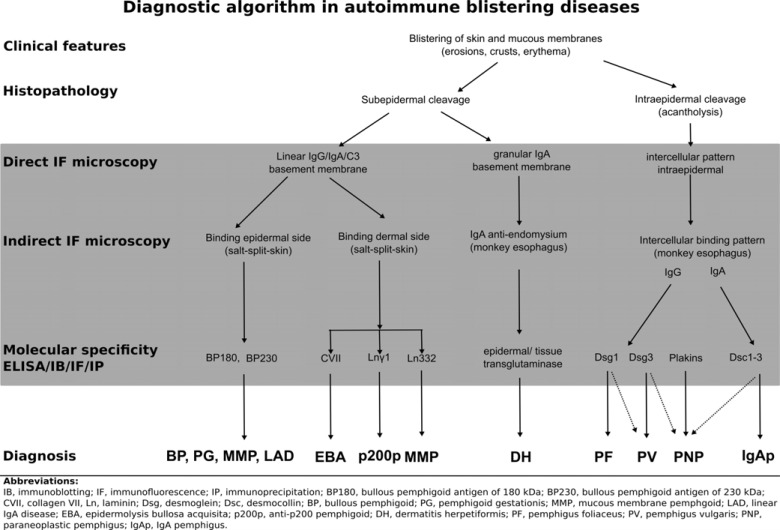
Due to its reliability and efficiency, detection of tissue-bound and serum autoantibodies plays an essential diagnostic role in autoimmune blistering diseases. Subsequent characterization of the molecular specificity of autoantibodies allows for developing robust diagnostic algorithms (Fig. 15), which can help streamlining the laboratory diagnosis of this group of diseases.
Fig. (15).
Diagnostic algorithm for autoimmune bullous diseases.
PERSPECTIVES FOR THE MOLECULAR DIAG-NOSIS OF AUTOIMMUNE BLISTERING DIS-EASES
The future development of state-of-the-art diagnostics for autoimmune diseases are heavily dependent on continuous in-depth fundamental and translational research. The main autoantigens have been already identified and cloned offering an excellent basis for the development of commercial test kits for the detection of autoantibodies with different specificity, including against laminin 332 and desmocollins. While most of target antigens are characterized, antigen(s) of the intraepidermal neutrophilic dermatosis type of IgA pemphigus and the lamina densa type of LAD as well as minor antigens of other autoimmune blistering diseases still need to be identified. An important, only partly characterized, aspect is the pathogenic potential of autoantibodies, which may be dependent on their different intrinsic features. A detailed definition of pathogenic human autoantibodies would allow the development of quantitative tests, which would ideally reflect disease activity in patients.
A further important avenue for improvement is related to automated pre-analytic and analytic steps and data collection for IF microscopy, ELISA and immunoblotting. While based on the simple concept of detecting structures using probes conjugated with fluorescent dyes, in its present form, IF is time-consuming, and requires manual handling as well as interpretation of the data by trained personnel. Relatively extensive experience is needed to properly record and interpret findings obtained by IF. In addition, IF-based tests are encumbered by a relatively low test-to-test fidelity owing to factors relating to the method itself (e.g. origin and preparation of the substrate) or to the interpreter. A promising alternative to the use of standard fluorescence microscopes for direct IF microscopy is the microarray scanner, which allows multiple antibodies to be visualized simultaneously, obtaining a larger field of view, and facilitating digital recording of images [170]. The need for standardization may be addressed by robotic preparation of slides and development of a computer-aided IF pattern analysis system [171-174]. Advanced systems are currently being developed that provide fully automated readings of IF images and software algorithms for the mathematical description of the IF patterns. Although full automated IF tests are difficult to imagine at present, the emerging automatic systems may be used for screening and classification of autoantibodies in routine diagnosis of systemic and organ-specific autoimmune diseases. In this respect, computer-aided diagnosis systems could support the diagnosis made by specialists, and improve the reproducibility of IF by overcoming its limitations, especially the inter-observer variability. In addition, these systems should pave the way for economic data-processing of IF assays. In the long-term, more sophisticated pattern-recognition algorithms and novel calibration systems should improve standardized quantification of IF image interpretation [171-174]. Further miniaturization and automation of the IF diagnostic tests may be achieved by devising complexes or microarrays of substrates containing the antigens [175, 176]. Thus, small sections of different organ substrates, including salt-split skin, esophagus, and bladder may be placed on the same slide and incubated with one diluted sample of the patient’s serum. IF assays using cells expressing recombinant antigens may partly replace the use of ELISAs, immunoblotting, and immunoprecipitation in the diagnosis of autoimmune diseases. Such cell chips containing spotted cell microarrays may be constructed by growing and treating cells under normal tissue culture conditions, formaldehyde fixing, and printing microsamples of each culture onto replicate glass slides [176]. These tests using collections of up to hundreds of antigens are amenable to full automation and high-throughput screening for autoantibodies, and should greatly reduce the costs involved.
CONCLUDING REMARKS
Autoantibodies against structural components maintaining cell-cell and cell matrix adhesion induce tissue damage and are exquisite diagnostic markers of autoimmune blistering diseases. The target antigens of blister-inducing autoantibodies have been extensively characterized over the past decades. Detection of tissue-bound and serum autoantibodies and characteri-zation of their molecular specificity allows for a rapid and accurate diagnosis of autoimmune blistering diseases. Various IF methods as well as molecular immunoassays, including ELISA and immunoblotting, became an essential part of the modern diagnostic algorithms for these disorders. Fundamental and translational research combining pathogenetic studies, bioinformatic analyses, automation and high throughput approaches will greatly facilitate the development of a next generation of improved diagnostic tools.
ACKNOWLEDGEMENTS
The work of the authors is supported by grants from the Deutsche Forschungsgemeinschaft SI-1281/4-1 and SI-1281/5-1 (CS), from the European Community's Seventh Framework Programme [FP7-2007-2013] under grant agreement No. HEALTH-F4-2011-282095 (CS), and from the Medical Faculty of the University of Freiburg (CS). The materials used for figures were not previously published and were generated at the authors' affiliations.
ABBREVIATIONS
- BP
= Bullous pemphigoid
- DH
= Dermatitis herpetiformis
- EBA
= Epidermolysis bullosa acquisita
- ELISA
= Enzyme-linked immunosorbent assay
- IF
= Immunofluorescence
- LAD
= Linear IgA disease
- MMP
= Mucous membrane pemphigoid
- PF
= Pemphigus foliaceus
- PNP
= Paraneoplastic pemphigus
- PV
= Pemphigus vulgaris
CONFLICT OF INTEREST
The authors confirm that this article content has no conflicts of interest.
REFERENCES
- 1.Mihai S, Sitaru C. Immunopathology and molecular diagnosis of autoimmune bullous diseases. J Cell Mol Med. 2007;11:462–481. doi: 10.1111/j.1582-4934.2007.00033.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kneisel A, Hertl M. Autoimmune bullous skin diseases.Part 1 Clinical manifestations. J Dtsch Dermatol Ges. 2011;9:844–56. doi: 10.1111/j.1610-0387.2011.07793.x. [DOI] [PubMed] [Google Scholar]
- 3.Sitaru C, Zillikens D. Mechanisms of blister induction by autoantibodies. Exp Dermatol. 2005;14:861–875. doi: 10.1111/j.1600-0625.2005.00367.x. [DOI] [PubMed] [Google Scholar]
- 4.Waschke J. The desmosome and pemphigus. Histochem Cell Biol. 2008;130:21–54. doi: 10.1007/s00418-008-0420-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.VanAgtmael T, Bruckner-Tuderman L. Basement membranes and human disease. Cell Tissue Res. 2010;339:167–188. doi: 10.1007/s00441-009-0866-y. [DOI] [PubMed] [Google Scholar]
- 6.Arndt KA, Feingold DS. The sign of Pyotr Vasilyewich Nikolsky. N Engl J Med. 1970;282:1154–1155. doi: 10.1056/NEJM197005142822011. [DOI] [PubMed] [Google Scholar]
- 7.Doubleday CW. Who is Nikolsky and what does his sign mean. J Am Acad Dermatol. 1987;16:1054–1055. doi: 10.1016/s0190-9622(87)80419-x. [DOI] [PubMed] [Google Scholar]
- 8.Kelly B, Shimoni T. Reintroducing the Tzanck smear. Am J Clin Dermatol. 2009;10:141–152. doi: 10.2165/00128071-200910030-00001. [DOI] [PubMed] [Google Scholar]
- 9.Durdu M, Baba M, Seçkin D. The value of Tzanck smear test in diagnosis of erosive vesicular bullous and pustular skin lesions. J Am Acad Dermatol. 2008;59:958–964. doi: 10.1016/j.jaad.2008.07.059. [DOI] [PubMed] [Google Scholar]
- 10.Florea F, Sitaru C. Relevance of immunofluorescence methods in clinical dermatology. CML Dermatology. 2011;15:29–45. [Google Scholar]
- 11.Gammon WR, Briggaman RA, Inman AO, Queen LL, Wheeler CE. Differentiating anti-lamina lucida and anti-sublamina densa anti-BMZ antibodies by indirect immunofluorescence on 1. M sodium chloride-separated skin. J Invest Dermatol. 1984;82:139–144. doi: 10.1111/1523-1747.ep12259692. [DOI] [PubMed] [Google Scholar]
- 12.Gammon WR, Briggaman RA, et al. Inman AO3 Differentiating anti-lamina lucida and anti-sublamina densa anti-bmz antibodies by indirect immunofluorescence on 1. m sodium chloride-separated skin. J. Invest Dermatol. 1984;82:139–144. doi: 10.1111/1523-1747.ep12259692. [DOI] [PubMed] [Google Scholar]
- 13.Anhalt GJ, Kim SC, Stanley JR, et al. Paraneoplastic pemphigus.An autoimmune mucocutaneous disease associated with neoplasia. N Engl J Med. 1990;323:1729–1735. doi: 10.1056/NEJM199012203232503. [DOI] [PubMed] [Google Scholar]
- 14.Domloge-Hultsch N, Gammon WR, Briggaman RA, Gil SG, Carter WG, Yancey KB. Epiligrin the major human keratinocyte integrin ligand is a target in both an acquired autoimmune and an inherited subepidermal blistering skin disease. J Clin Invest. 1992;90:1628–1633. doi: 10.1172/JCI116033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Caldarola G, Kneisel A, Hertl M, Feliciani C. Herpes simplex virus infection in pemphigus vulgaris clinical and immunological considerations. Eur J Dermatol. 2008;18:440–443. doi: 10.1684/ejd.2008.0439. [DOI] [PubMed] [Google Scholar]
- 16.Stevenson ML, Levitt JO. Acute zoster in known pemphigus vulgaris and bullous pemphigoid avoiding the "disease flare" trap. J Am Acad Dermatol. 2011;64:e125–6. doi: 10.1016/j.jaad.2010.11.013. [DOI] [PubMed] [Google Scholar]
- 17.Raith L. [Johann Ernst Wichmann an unjustly little-known dermatologist of the 18th century. Dermatol Monatsschr. 1983;169:725–727. [PubMed] [Google Scholar]
- 18.Holubar K. Pemphigus a disease of man and animal.Historical and other perspectives. Int J Dermatol. 1988;27:516–520. doi: 10.1111/j.1365-4362.1988.tb00937.x. [DOI] [PubMed] [Google Scholar]
- 19.Stanley JR, Amagai M. Pemphigus bullous impetigo and the staphylococcal scalded-skin syndrome. N Engl J Med. 2006;355:1800–1810. doi: 10.1056/NEJMra061111. [DOI] [PubMed] [Google Scholar]
- 20.Amagai M, Klaus-Kovtun V, Stanley JR. Autoantibodies against a novel epithelial cadherin in pemphigus vulgaris a disease of cell adhesion. Cell. 1991;67:869–877. doi: 10.1016/0092-8674(91)90360-b. [DOI] [PubMed] [Google Scholar]
- 21.Ding X, Aoki V, Mascaro JMJ, Lopez-Swiderski A, Diaz LA, Fairley JA. Mucosal and mucocutaneous (generalized) pemphigus vulgaris show distinct autoantibody profiles. J Invest Dermatol. 1997;109:592–596. doi: 10.1111/1523-1747.ep12337524. [DOI] [PubMed] [Google Scholar]
- 22.Nguyen VT, Ndoye A, Grando SA. Pemphigus vulgaris antibody identifies pemphaxin.A novel keratinocyte annexin-like molecule binding acetylcholine. J Biol Chem. 2000;275:29466–29476. doi: 10.1074/jbc.M003174200. [DOI] [PubMed] [Google Scholar]
- 23.Nguyen VT, Ndoye A, Grando SA. Novel human alpha9 acetylcholine receptor regulating keratinocyte adhesion is targeted by Pemphigus vulgaris autoimmunity. Am J Pathol. 2000;157:1377–1391. doi: 10.1016/s0002-9440(10)64651-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rafei D, Müller R, Ishii N, Llamazares M, Hashimoto T, Hertl M, Eming R. IgG autoantibodies against desmocollin 3 in pemphigus sera induce loss of keratinocyte adhesion. Am J Pathol. 2011;178:718–723. doi: 10.1016/j.ajpath.2010.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mao X, Nagler AR, Farber SA, Choi EJ, Jackson LH, Leiferman KM, Ishii N, Hashimoto T, Amagai M, Zone JJ, Payne AS. Autoimmunity to desmocollin 3 in pemphigus vulgaris. Am J Pathol. 2010;177:2724–2730. doi: 10.2353/ajpath.2010.100483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ishii K, Amagai M, Hall RP, et al. Characterization of autoantibodies in pemphigus using antigen-specific enzyme-linked immunosorbent assays with baculovirus-expressed recombinant desmogleins. J Immunol. 1997;159:2010–2017. [PubMed] [Google Scholar]
- 27.Amagai M, Tsunoda K, Zillikens D, Nagai T, Nishikawa T. The clinical phenotype of pemphigus is defined by the anti-desmoglein autoantibody profile. J Am Acad Dermatol. 1999;40:167–170. doi: 10.1016/s0190-9622(99)70183-0. [DOI] [PubMed] [Google Scholar]
- 28.Nagel A, Lang A, Engel D, et al. Clinical activity of pemphigus vulgaris relates to IgE autoantibodies against desmoglein 3. Clin Immunol. 2010;134:320–330. doi: 10.1016/j.clim.2009.11.006. [DOI] [PubMed] [Google Scholar]
- 29.Dhandha MM, Seiffert-Sinha K, Sinha AA. Specific immunoglobulin isotypes correlate with disease activity morphology duration and hla association in pemphigus vulgaris. Autoimmunity. 2012;45:516–526. doi: 10.3109/08916934.2012.702811. [DOI] [PubMed] [Google Scholar]
- 30.Hertl M, Eming R, Veldman C. T cell control in autoimmune bullous skin disorders. J. Clin. Invest. 2006;116:1159–1166. doi: 10.1172/JCI28547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sinha AA. Constructing immunoprofiles to deconstruct disease complexity in pemphigus. Autoimmunity. 2012;45:36–43. doi: 10.3109/08916934.2011.606445. [DOI] [PubMed] [Google Scholar]
- 32.Veldman C, Höhne A, Dieckmann D, et al. Type i regulatory t cells specific for desmoglein 3 are more frequently detected in healthy individuals than in patients with pemphigus vulgaris. J. Immunol. 2004;172: 6468–6475. doi: 10.4049/jimmunol.172.10.6468. [DOI] [PubMed] [Google Scholar]
- 33.Brenner S, Bialy-Golan A, Ruocco V. Drug-induced pemphigus. Clin. Dermatol. 1998;16:393–397. doi: 10.1016/s0738-081x(98)00010-8. [DOI] [PubMed] [Google Scholar]
- 34.Brenner S, Goldberg I. Drug-induced pemphigus. Clin Dermatol. 2011;29:455–457. doi: 10.1016/j.clindermatol.2011.01.016. [DOI] [PubMed] [Google Scholar]
- 35.Feng S, Zhou W, Zhang J, et al. Analysis of 6 cases of drug-induced pemphigus. Eur J Dermatol. 2011;21:696–699. doi: 10.1684/ejd.2011.1428. [DOI] [PubMed] [Google Scholar]
- 36.Fryer EJ, Lebwohl M. Pemphigus vulgaris after initiation of psoralen and uva therapy for psoriasis. J. Am Acad Dermatol. 1994;30:651–653. doi: 10.1016/s0190-9622(09)80116-3. [DOI] [PubMed] [Google Scholar]
- 37.Jamora MJJ, Jiao D, Bystryn J. Antibodies to desmoglein 1 and 3 and the clinical phenotype of pemphigus vulgaris. J Am Acad Dermatol. 2003;48:976–977. doi: 10.1067/mjd.2003.438. [DOI] [PubMed] [Google Scholar]
- 38.Lebeau S, Müller R, Masouyé I, Hertl M, Borradori L. Pemphigus herpetiformis analysis of the autoantibody profile during the disease course with changes in the clinical phenotype. Clin Exp Dermatol. 2010;35:366–372. doi: 10.1111/j.1365-2230.2009.03525.x. [DOI] [PubMed] [Google Scholar]
- 39.Eyre RW, Stanley JR. Identification of pemphigus vulgaris antigen extracted from normal human epidermis and comparison with pemphigus foliaceus antigen. J Clin Invest. 1988;81:807–812. doi: 10.1172/JCI113387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rock B, Martins CR, Theofilopoulos AN, et al. The pathogenic effect of IgG4 autoantibodies in endemic pemphigus foliaceus (fogo selvagem). N Engl J Med. 1989;320:1463–1469. doi: 10.1056/NEJM198906013202206. [DOI] [PubMed] [Google Scholar]
- 41.Aoki V, Sousa JXJ, Diaz LA. Pathogenesis of endemic pemphigus foliaceus. Dermatol Clin. 2011;29:413–8. doi: 10.1016/j.det.2011.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Aoki V, Millikan RC, Rivitti EA, Hans-Filho G, Eaton DP, Warren SJP, Li N, Hilario-Vargas J, Hoffmann RG, Diaz LA. Environmental risk factors in endemic pemphigus foliaceus (fogo selvagem). J Investig Dermatol Symp Proc. 2004;9:34–40. doi: 10.1111/j.1087-0024.2004.00833.x. [DOI] [PubMed] [Google Scholar]
- 43.Qian Y, Jeong JS, Maldonado M, et al. Cutting edge brazilian pemphigus foliaceus anti-desmoglein 1 autoantibodies cross-react with sand fly salivary ljm11 antigen. J. Immunol. 2012;189:1535–1539. doi: 10.4049/jimmunol.1200842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nguyen VT, Ndoye A, Bassler KD, et al. Classification clinical manifestations and immunopathological mechanisms of the epithelial variant of paraneoplastic autoimmune multiorgan syndrome a reappraisal of paraneoplastic pemphigus. Arch Dermatol. 2001;137:193–206. [PubMed] [Google Scholar]
- 45.Maldonado F, Pittelkow MR, Ryu JH. Constrictive bronchiolitis associated with paraneoplastic autoimmune multi-organ syndrome. Respirology. 2009;14:129–133. doi: 10.1111/j.1440-1843.2008.01397.x. [DOI] [PubMed] [Google Scholar]
- 46.Anhalt GJ. Paraneoplastic pemphigus the role of tumours and drugs. Br J Dermatol. 2001;144:1102–1104. doi: 10.1046/j.1365-2133.2001.04272.x. [DOI] [PubMed] [Google Scholar]
- 47.Maverakis E, Goodarzi H, Wehrli LN, Ono Y, Garcia MS. The Etiology of Paraneoplastic Autoimmunity. Clin Rev Allergy Immunol. 2011;42:135–144. doi: 10.1007/s12016-010-8248-5. [DOI] [PubMed] [Google Scholar]
- 48.Vanderlugt CJ, Miller SD. Epitope spreading. Curr Opin Immunol. 1996;8:831–836. doi: 10.1016/S0952-7915(96)80012-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chan LS, Vanderlugt CJ, Hashimoto T, et al. Epitope spreading: lessons from autoimmune skin diseases. J Invest Dermatol. 1998;110:103–109. doi: 10.1046/j.1523-1747.1998.00107.x. [DOI] [PubMed] [Google Scholar]
- 50.Zhang J, Qiao Q, Chen X, et al. Improved outcomes after complete resection of underlying tumors for patients with paraneoplastic pemphigus a single-center experience of 22 cases. J Cancer Res Clin Oncol. 2011;137:229–234. doi: 10.1007/s00432-010-0874-z. [DOI] [PubMed] [Google Scholar]
- 51.Meyers SJ, Varley GA, Meisler DM, Camisa C, Wander AH. Conjunctival involvement in paraneoplastic pemphigus. Am J Ophthalmol. 1992;114:621–624. doi: 10.1016/s0002-9394(14)74494-0. [DOI] [PubMed] [Google Scholar]
- 52.Anhalt GJ. Paraneoplastic pemphigus. J Investig Dermatol Symp Proc. 2004;9:29–33. doi: 10.1111/j.1087-0024.2004.00832.x. [DOI] [PubMed] [Google Scholar]
- 53.Frew JW, Murrell DF. Paraneoplastic pemphigus (paraneoplastic autoimmune multiorgan syndrome) clinical presentations and pathogenesis. Dermatol Clin. 2011;29:419–25. doi: 10.1016/j.det.2011.03.018. [DOI] [PubMed] [Google Scholar]
- 54.Zhu X, Zhang B. Paraneoplastic pemphigus. J Dermatol. 2007;34:503–511. doi: 10.1111/j.1346-8138.2007.00322.x. [DOI] [PubMed] [Google Scholar]
- 55.Nousari HC, Deterding R, Wojtczack H, et al. The mechanism of respiratory failure in paraneoplastic pemphigus. N Engl J Med. 1999;340:1406–1410. doi: 10.1056/NEJM199905063401805. [DOI] [PubMed] [Google Scholar]
- 56.Helou J, Allbritton J, Anhalt GJ. Accuracy of indirect immunofluorescence testing in the diagnosis of paraneoplastic pemphigus. J Am Acad Dermatol. 1995;32:441–447. doi: 10.1016/0190-9622(95)90066-7. [DOI] [PubMed] [Google Scholar]
- 57.Kim SC, Kwon YD, Lee IJ, Chang SN, Lee TG. cDNA cloning of the 210-kDa paraneoplastic pemphigus antigen reveals that envoplakin is a component of the antigen complex. J Invest Dermatol. 1997;109:365–369. doi: 10.1111/1523-1747.ep12336235. [DOI] [PubMed] [Google Scholar]
- 58.Kiyokawa C, Ruhrberg C, Nie Z, et al. Envoplakin and periplakin are components of the paraneoplastic pemphigus antigen complex. J Invest Dermatol. 1998;111:1236–1238. doi: 10.1046/j.1523-1747.1998.00449.x. [DOI] [PubMed] [Google Scholar]
- 59.Mahoney MG, Aho S, Uitto J, Stanley JR. The members of the plakin family of proteins recognized by paraneoplastic pemphigus antibodies include periplakin. J Invest Dermatol. 1998;111:308–313. doi: 10.1046/j.1523-1747.1998.00279.x. [DOI] [PubMed] [Google Scholar]
- 60.Schepens I, Jaunin F, Begre N, et al. The protease inhibitor alpha-2-macroglobulin-like-1 is the p170 antigen recognized by paraneoplastic pemphigus autoantibodies in human. PLoS ONE. 2010;5:e12250. doi: 10.1371/journal.pone.0012250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hashimoto T, Amagai M, Watanabe K, et al. Characterization of paraneoplastic pemphigus autoantigens by immunoblot analysis. J Invest Dermatol. 1995;104:829–834. doi: 10.1111/1523-1747.ep12607012. [DOI] [PubMed] [Google Scholar]
- 62.Sitaru C, Dähnrich C, Probst C, et al. Enzyme-linked immunosorbent assay using multimers of the 16th non-collagenous domain of the BP180 antigen for sensitive and specific detection of pemphigoid autoantibodies. Exp Dermatol. 2007;16:770–777. doi: 10.1111/j.1600-0625.2007.00592.x. [DOI] [PubMed] [Google Scholar]
- 63.Tsuruta D, Ishii N, Hamada T, et al. IgA pemphigus. Clin Dermatol. 2011;29:437–442. doi: 10.1016/j.clindermatol.2011.01.014. [DOI] [PubMed] [Google Scholar]
- 64.Hashimoto T, Ebihara T, Nishikawa T. Studies of autoantigens recognized by IgA anti-keratinocyte cell surface antibodies. J Dermatol Sci. 1996;12:10–17. doi: 10.1016/0923-1811(95)00449-1. [DOI] [PubMed] [Google Scholar]
- 65.Hashimoto T, Kiyokawa C, Mori O, et al. Human desmocollin 1 (Dsc1) is an autoantigen for the subcorneal pustular dermatosis type of IgA pemphigus. J Invest Dermatol. 1997;109:127–131. doi: 10.1111/1523-1747.ep12319025. [DOI] [PubMed] [Google Scholar]
- 66.Kárpáti S, Amagai M, Liu WL, Dmochowski M, Hashimoto T, Horváth A. Identification of desmoglein 1 as autoantigen in a patient with intraepidermal neutrophilic IgA dermatosis type of IgA pemphigus. Exp Dermatol. 2000;9:224–228. doi: 10.1034/j.1600-0625.2000.009003224.x. [DOI] [PubMed] [Google Scholar]
- 67.Hashimoto T, Komai A, Futei Y, Nishikawa T, Amagai M. Detection of IgA autoantibodies to desmogleins by an enzyme-linked immunosorbent assay the presence of new minor subtypes of IgA pemphigus. Arch Dermatol. 2001;137:735–738. [PubMed] [Google Scholar]
- 68.Wang J, Kwon J, Ding X, Fairley JA, Woodley DT, Chan LS. Nonsecretory IgA1 autoantibodies targeting desmosomal component desmoglein 3 in intraepidermal neutrophilic IgA dermatosis. Am J Pathol. 1997;150:1901–1907. [PMC free article] [PubMed] [Google Scholar]
- 69.Ishii N, Ishida-Yamamoto A, Hashimoto T. Immunolocalization of target autoantigens in IgA pemphigus. Clin Exp Dermatol. 2004;29:62–66. doi: 10.1111/j.1365-2230.2004.01436.x. [DOI] [PubMed] [Google Scholar]
- 70.Supapannachart N, Mutasim DF. The distribution of IgA pemphigus antigen in human skin and the role of IgA anti-cell surface antibodies in the induction of intraepidermal acantholysis. Arch Dermatol. 1993;129:605–608. [PubMed] [Google Scholar]
- 71.Hashimoto T, Yasumoto S, Nagata Y, Okamoto T, Fujita S. Clinical histopathological and immunological distinction in two cases of IgA pemphigus. Clin Exp Dermatol. 2002;27:636–640. doi: 10.1046/j.1365-2230.2002.01061.x. [DOI] [PubMed] [Google Scholar]
- 72.Bernard P, Vaillant L, Labeille B, et al. Incidence and distribution of subepidermal autoimmune bullous skin diseases in three French regions.Bullous Diseases French Study Group. Arch Dermatol. 1995;131:48–52. [PubMed] [Google Scholar]
- 73.Langan SM, Smeeth L, Hubbard R, Fleming KM, Smith CJP, West J. Bullous pemphigoid and pemphigus vulgaris incidence and mortality in the UK population based cohort study. BMJ. 2008;337:a180. doi: 10.1136/bmj.a180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Baican A, Baican C, Chiriac G, et al. Pemphigus vulgaris is the most common autoimmune bullous disease in Northwestern Romania. Int J Dermatol. 2010;49:768–774. doi: 10.1111/j.1365-4632.2009.04345.x. [DOI] [PubMed] [Google Scholar]
- 75.Olasz EB, Yancey KB. Bullous pemphigoid and related subepidermal autoimmune blistering diseases. Curr Dir Autoimmun. 2008;10:141–166. doi: 10.1159/000131452. [DOI] [PubMed] [Google Scholar]
- 76.Lever W. Pemphigus. Medicine. 1953;32:2–132. doi: 10.1097/00005792-195302000-00001. [DOI] [PubMed] [Google Scholar]
- 77.Stanley JR, Hawley-Nelson P, Yuspa SH, Shevach EM, Katz SI. Characterization of bullous pemphigoid antigen a unique basement membrane protein of stratified squamous epithelia. Cell. 1981;24:897–903. doi: 10.1016/0092-8674(81)90115-x. [DOI] [PubMed] [Google Scholar]
- 78.Diaz LA, Ratrie H, Saunders WS, et al. Isolation of a human epidermal cDNA corresponding to the 180-kDa autoantigen recognized by bullous pemphigoid and herpes gestationis sera.Immunolocalization of this protein to the hemidesmosome. . J Clin Invest. 1990;86:1088–1094. doi: 10.1172/JCI114812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Laffitte E, Favre B, Fontao L, et al. Plectin an unusual target antigen in bullous pemphigoid. Br J Dermatol. 2001;144:136–138. doi: 10.1046/j.1365-2133.2001.03963.x. [DOI] [PubMed] [Google Scholar]
- 80.Kiss M, Perényi A, Marczinovits I, et al. Autoantibodies to human alpha6 integrin in patients with bullous pemphigoid. Ann N Y Acad Sci. 2005;1051:104–110. doi: 10.1196/annals.1361.051. [DOI] [PubMed] [Google Scholar]
- 81.Giudice GJ, Emery DJ, Zelickson BD, Anhalt GJ, Liu Z, Diaz LA. Bullous pemphigoid and herpes gestationis autoantibodies recognize a common non-collagenous site on the {BP}180 ectodomain. J Immunol. 1993;151:5742–5750. [PubMed] [Google Scholar]
- 82.Murakami H, Amagai M, Higashiyama M, et al. Analysis of antigens recognized by autoantibodies in herpes gestationis.Usefulness of immunoblotting using a fusion protein representing an extracellular domain of the 180 kD bullous pemphigoid antigen. J Dermatol Sci. 1996;13:112–117. doi: 10.1016/s0923-1811(96)00509-9. [DOI] [PubMed] [Google Scholar]
- 83.Sitaru C. Bullous pemphigoid a prototypical antibody-mediated organ-specific autoimmune disease. J Invest Dermatol. 2009;129:822–824. doi: 10.1038/jid.2009.12. [DOI] [PubMed] [Google Scholar]
- 84.Feliciani C, Caldarola G, Kneisel A, et al. IgG autoantibody reactivity against bullous pemphigoid (BP) 180 and BP230 in elderly patients with pruritic dermatoses. Br J Dermatol. 2009;161:306–312. doi: 10.1111/j.1365-2133.2009.09266.x. [DOI] [PubMed] [Google Scholar]
- 85.Quartey-Papafio CM, Hudson PM. Bullous pemphigoid initially localized to sites of burns (scalds) in a patient on sulphasalazine for ulcerative colitis. Clin Exp Dermatol. 1994;19:281. doi: 10.1111/j.1365-2230.1994.tb01192.x. [DOI] [PubMed] [Google Scholar]
- 86.VandeMaele DM, Reilly JC. Bullous pemphigoid at colostomy site report of a case. Dis Colon Rectum. 1997;40:370–371. doi: 10.1007/BF02050431. [DOI] [PubMed] [Google Scholar]
- 87.Torchia D, Caproni M, Ketabchi S, Antiga E, Fabbri P. Bullous pemphigoid initially localized around a urostomy. Int J Dermatol. 2006;45:1387–1389. doi: 10.1111/j.1365-4632.2006.03118.x. [DOI] [PubMed] [Google Scholar]
- 88.Batalla A, Peón G, DelaTorre C. Localized bullous pemphigoid at urostomy site. Indian J Dermatol Venereol Leprol. 2011;77:625. doi: 10.4103/0378-6323.84067. [DOI] [PubMed] [Google Scholar]
- 89.Pardo J, Rodrguez-Serna M, Mercader P, Fortea JM. Localized bullous pemphigoid overlying a fistula for hemodialysis. J Am Acad Dermatol. 2004;51:S131–2. doi: 10.1016/j.jaad.2004.03.024. [DOI] [PubMed] [Google Scholar]
- 90.Brodell RT, Korman NJ. Stump pemphigoid. Cutis. 1996;57:245–246. [PubMed] [Google Scholar]
- 91.Melani L, Giomi B, Antiga E, Torchia D, Caproni M, Fabbri P. Radiation therapy as a trigger factor for initially localized bullous pemphigoid. Breast J. 2005;11:485–486. doi: 10.1111/j.1075-122X.2005.00150.x. [DOI] [PubMed] [Google Scholar]
- 92.Kobayashi M, Amagai M, Kuroda-Kinoshita K, et al. BP180 ELISA using bacterial recombinant NC16a protein as a diagnostic and monitoring tool for bullous pemphigoid. J Dermatol Sci. 2002;30:224–232. doi: 10.1016/s0923-1811(02)00109-3. [DOI] [PubMed] [Google Scholar]
- 93.Yoshida M, Hamada T, Amagai M, et al. Enzyme-linked immunosorbent assay using bacterial recombinant proteins of human BP230 as a diagnostic tool for bullous pemphigoid. J Dermatol Sci. 2006;41:21–30. doi: 10.1016/j.jdermsci.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 94.Iwata Y, Komura K, Kodera M, et al. Correlation of IgE autoantibody to BP180 with a severe form of bullous pemphigoid. Arch Dermatol. 2008;144:41–48. doi: 10.1001/archdermatol.2007.9. [DOI] [PubMed] [Google Scholar]
- 95.Messingham KAN, Noe MH, Chapman MA, Giudice GJ, Fairley JA. A novel ELISA reveals high frequencies of BP180-specific IgE production in bullous pemphigoid. J Immunol Methods. 2009;346:18–25. doi: 10.1016/j.jim.2009.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Dresow SK, Sitaru C, Recke A, Oostingh GJ, Zillikens D, Gibbs BF. IgE autoantibodies against the intracellular domain of BP180. Br J Dermatol. 2009;160:429–432. doi: 10.1111/j.1365-2133.2008.08858.x. [DOI] [PubMed] [Google Scholar]
- 97.Intong LRA, Murrell DF. Pemphigoid gestationis: pathogenesis and clinical features. Dermatol Clin. 2011;29:447–52. doi: 10.1016/j.det.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 98.Morrison LH, Labib RS, Zone JJ, Diaz LA, Anhalt GJ. Herpes gestationis autoantibodies recognize a 180-kD human epidermal antigen. J Clin Invest. 1988;81:2023–2026. doi: 10.1172/JCI113554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Kelly SE, Bhogal BS, Wojnarowska F, Whitehead P, Leigh IM, Black MM. Western blot analysis of the antigen in pemphigoid gestationis. Br J Dermatol. 1990;122:445–449. doi: 10.1111/j.1365-2133.1990.tb14720.x. [DOI] [PubMed] [Google Scholar]
- 100.Katz SI, Hertz KC, Yaoita H. Herpes gestationis.Immunopathology and characterization of the HG factor. J Clin Invest. 1976;57:1434–1441. doi: 10.1172/JCI108413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Jordon RE, Heine KG, Tappeiner G, Bushkell LL, Provost TT. The immunopathology of herpes gestationis.Immunofluorescence studies and characterization of "HG factor". J Clin Invest. 1976;57:1426–1431. doi: 10.1172/JCI108412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Kelly SE, Cerio R, Bhogal BS, Black MM. The distribution of IgG subclasses in pemphigoid gestationis.PG factor is an IgG1 autoantibody. J Invest Dermatol. 1989;92:695–698. doi: 10.1111/1523-1747.ep12696884. [DOI] [PubMed] [Google Scholar]
- 103.Sitaru C, Powell J, Shimanovich I, et al. Pemphigoid gestationis maternal sera recognize epitopes restricted to the N-terminal portion of the extracellular domain of BP180 not present on its shed ectodomain. Br J Dermatol. 2003;149:420–422. doi: 10.1046/j.1365-2133.2003.05427.x. [DOI] [PubMed] [Google Scholar]
- 104.Carruthers JA. Herpes gestationis clinical features of immunologically proved cases. Am J Obstet Gynecol. 1978;131:865–867. doi: 10.1016/s0002-9378(16)33133-7. [DOI] [PubMed] [Google Scholar]
- 105.Amato L, Mei S, Gallerani I, Moretti S, Fabbri P. A case of chronic herpes gestationis persistent disease or conversion to bullous pemphigoid. J Am Acad Dermatol. 2003;49:302–307. doi: 10.1067/s0190-9622(03)00412-2. [DOI] [PubMed] [Google Scholar]
- 106.Boulinguez S, Bédane C, Prost C, Bernard P, Labbé L, Bonnetblanc JM. Chronic pemphigoid gestationis comparative clinical and immunopathological study of 10 patients. Dermatology. 2003;206:113–119. doi: 10.1159/000068467. [DOI] [PubMed] [Google Scholar]
- 107.Semkova K, Black M. Pemphigoid gestationis: current insights into pathogenesis and treatment. Eur J Obstet Gynecol Reprod Biol. 2009;145:138–144. doi: 10.1016/j.ejogrb.2009.05.012. [DOI] [PubMed] [Google Scholar]
- 108.Jenkins RE, Hern S, Black MM. Clinical features and management of 87 patients with pemphigoid gestationis. Clin Exp Dermatol. 1999;24:255–259. doi: 10.1046/j.1365-2230.1999.00472.x. [DOI] [PubMed] [Google Scholar]
- 109.Ambros-Rudolph CM, Müllegger RR, Vaughan-Jones SA, Kerl H, Black MM. The specific dermatoses of pregnancy revisited and reclassified results of a retrospective two-center study on 505 pregnant patients. J Am Acad Dermatol. 2006;54:395–404. doi: 10.1016/j.jaad.2005.12.012. [DOI] [PubMed] [Google Scholar]
- 110.Roth M. Pregnancy dermatoses diagnosis management and controversies. Am J Clin Dermatol. 2011;12:25–41. doi: 10.2165/11532010-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 111.Beard MP, Millington GWM. Recent developments in the specific dermatoses of pregnancy. Clin Exp Dermatol. 2011;37:1–4. doi: 10.1111/j.1365-2230.2011.04173.x. [DOI] [PubMed] [Google Scholar]
- 112.Sitaru C, Powell J, Messer G, Bröcker E, Wojnarowska F, Zillikens D. Immunoblotting and enzyme-linked immunosorbent assay for the diagnosis of pemphigoid gestationis. Obstet Gynecol. 2004;103:757–763. doi: 10.1097/01.AOG.0000115506.76104.ad. [DOI] [PubMed] [Google Scholar]
- 113.Chan LS, Ahmed AR, Anhalt GJ, et al. The first international consensus on mucous membrane pemphigoid definition diagnostic criteria pathogenic factors medical treatment and prognostic indicators. Arch Dermatol. 2002;138:370–379. doi: 10.1001/archderm.138.3.370. [DOI] [PubMed] [Google Scholar]
- 114.Egan CA, Lazarova Z, Darling TN, Yee C, Coté T, Yancey KB. Anti-epiligrin cicatricial pemphigoid and relative risk for cancer. Lancet. 2001;357:1850–1851. doi: 10.1016/S0140-6736(00)04971-0. [DOI] [PubMed] [Google Scholar]
- 115.Bernard P, Prost C, Durepaire N, Basset-Seguin N, Didierjean L, Saurat JH. The major cicatricial pemphigoid antigen is a 180-kD protein that shows immunologic cross-reactivities with the bullous pemphigoid antigen. J Invest Dermatol. 1992;99:174–179. doi: 10.1111/1523-1747.ep12616797. [DOI] [PubMed] [Google Scholar]
- 116.Balding SD, Prost C, Diaz LA, et al. Cicatricial pemphigoid autoantibodies react with multiple sites on the BP180 extracellular domain. J Invest Dermatol. 1996;106:141–146. doi: 10.1111/1523-1747.ep12329728. [DOI] [PubMed] [Google Scholar]
- 117.Murakami H, Nishioka S, Setterfield J, et al. Analysis of antigens targeted by circulating IgG and IgA autoantibodies in 50 patients with cicatricial pemphigoid. J Dermatol Sci. 1998;17:39–44. doi: 10.1016/s0923-1811(97)00067-4. [DOI] [PubMed] [Google Scholar]
- 118.Tyagi S, Bhol K, Natarajan K, Livir-Rallatos C, Foster CS, Ahmed AR. Ocular cicatricial pemphigoid antigen partial sequence and biochemical characterization. Proc Natl Acad Sci USA. 1996;93:14714–14719. doi: 10.1073/pnas.93.25.14714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Caux F, Kirtschig G, Lemarchand-Venencie F, et al. IgA-epidermolysis bullosa acquisita in a child resulting in blindness. Br J Dermatol. 1997;137:270–275. doi: 10.1046/j.1365-2133.1997.18191915.x. [DOI] [PubMed] [Google Scholar]
- 120.Wieme N, Lambert J, Moerman M, Geerts ML, Temmerman L, Naeyaert JM. Epidermolysis bullosa acquisita with combined features of bullous pemphigoid and cicatricial pemphigoid. Dermatology. 1999;198:310–313. doi: 10.1159/000018139. [DOI] [PubMed] [Google Scholar]
- 121.Schmidt E, Skrobek C, Kromminga A, et al. Cicatricial pemphigoid: IgA and IgG autoantibodies target epitopes on both intra- and extracellular domains of bullous pemphigoid antigen 180. Br J Dermatol. 2001;145:778–783. doi: 10.1046/j.1365-2133.2001.04471.x. [DOI] [PubMed] [Google Scholar]
- 122.Leverkus M, Bhol K, Hirako Y, et al. Cicatricial pemphigoid with circulating autoantibodies to beta4 integrin bullous pemphigoid 180 and bullous pemphigoid 230. Br J Dermatol. 2001;145:998–1004. doi: 10.1046/j.1365-2133.2001.04543.x. [DOI] [PubMed] [Google Scholar]
- 123.Rashid KA, Gürcan HM, Ahmed AR. Antigen specificity in subsets of mucous membrane pemphigoid. J Invest Dermatol. 2006;126:2631–2636. doi: 10.1038/sj.jid.5700465. [DOI] [PubMed] [Google Scholar]
- 124.Egan CA, Lazarova Z, Darling TN, Yee C, Yancey KB. Anti-epiligrin cicatricial pemphigoid clinical findings immunopathogenesis and significant associations. Medicine (Baltimore). 2003;82:177–186. doi: 10.1097/01.md.0000076003.64510.00. [DOI] [PubMed] [Google Scholar]
- 125.Hanno R, Foster DR, Bean SF. Brunsting-Perry cicatricial pemphigoid associated with bullous pemphigoid. J Am Acad Dermatol. 1980;3:470–473. doi: 10.1016/s0190-9622(80)80111-3. [DOI] [PubMed] [Google Scholar]
- 126.Rose C, Schmidt E, Kerstan A, et al. Histopathology of anti-laminin 5 mucous membrane pemphigoid. J Am Acad Dermatol. 2009;61:433–440. doi: 10.1016/j.jaad.2009.02.012. [DOI] [PubMed] [Google Scholar]
- 127.Lazarova Z, Sitaru C, Zillikens D, Yancey KB. Comparative analysis of methods for detection of anti-laminin 5 autoantibodies in patients with anti-epiligrin cicatricial pemphigoid. J Am Acad Dermatol. 2004;51:886–892. doi: 10.1016/j.jaad.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 128.Lazarova Z, Yee C, Lazar J, Yancey KB. IgG autoantibodies in patients with anti-epiligrin cicatricial pemphigoid recognize the G domain of the laminin 5 alpha-subunit. Clin Immunol. 2001;101:100–105. doi: 10.1006/clim.2001.5091. [DOI] [PubMed] [Google Scholar]
- 129.Bhol KC, Dans MJ, Simmons RK, Foster CS, Giancotti FG, Ahmed AR. The autoantibodies to alpha 6 beta 4 integrin of patients affected by ocular cicatricial pemphigoid recognize predominantly epitopes within the large cytoplasmic domain of human beta 4. J Immunol. 2000;165:2824–2829. doi: 10.4049/jimmunol.165.5.2824. [DOI] [PubMed] [Google Scholar]
- 130.Bhol KC, Goss L, Kumari S, Colon JE, Ahmed AR. Autoantibodies to human alpha6 integrin in patients with oral pemphigoid. J Dent Res. 2001;80:1711–1715. doi: 10.1177/00220345010800080601. [DOI] [PubMed] [Google Scholar]
- 131.Chorzelski TP, Jablonska S. IgA linear dermatosis of childhood (chronic bullous disease of childhood). Br J Dermatol. 1979;101:535–542. doi: 10.1111/j.1365-2133.1979.tb11882.x. [DOI] [PubMed] [Google Scholar]
- 132.Fortuna G, Salas-Alanis JC, Guidetti E, Marinkovich MP. A critical reappraisal of the current data on drug-induced linear immuglobulin A bullous dermatosis.A real and separate nosological entity. J Am Acad Dermatol. 2012;66(6):988–94. doi: 10.1016/j.jaad.2011.09.018. [DOI] [PubMed] [Google Scholar]
- 133.Zone JJ, Taylor TB, Kadunce DP, Meyer LJ. Identification of the cutaneous basement membrane zone antigen and isolation of antibody in linear immunoglobulin A bullous dermatosis. J Clin Invest. 1990;85:812–820. doi: 10.1172/JCI114508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Marinkovich MP, Taylor TB, Keene DR, Burgeson RE, Zone JJ. LAD-1 the linear IgA bullous dermatosis autoantigen is a novel 120-kDa anchoring filament protein synthesized by epidermal cells. J Invest Dermatol. 1996;106:734–738. doi: 10.1111/1523-1747.ep12345782. [DOI] [PubMed] [Google Scholar]
- 135.Pas HH Kloosterhuis GJ, Heeres K, vanderMeer JB, Jonkman MF. Bullous pemphigoid and linear IgA dermatosis sera recognize a similar 120-kDa keratinocyte collagenous glycoprotein with antigenic cross-reactivity to BP180. J Invest Dermatol. 1997;108:423–429. doi: 10.1111/1523-1747.ep12289703. [DOI] [PubMed] [Google Scholar]
- 136.Hirako Y, Usukura J, Uematsu J, Hashimoto T, Kitajima Y, Owaribe K. Cleavage of BP180 a 180-kDa bullous pemphigoid antigen yields a 120-kDa collagenous extracellular polypeptide. J Biol Chem. 1998;273:9711–9717. doi: 10.1074/jbc.273.16.9711. [DOI] [PubMed] [Google Scholar]
- 137.Schäcke H, Schumann H, Hammami-Hauasli N, Raghunath M, Bruckner-Tuderman L. Two forms of collagen XVII in keratinocytes.A full-length transmembrane protein and a soluble ectodomain. . J Biol Chem. 1998;273:25937–25943. doi: 10.1074/jbc.273.40.25937. [DOI] [PubMed] [Google Scholar]
- 138.Csorba K, Schmidt S, Florea F, et al. Development of an ELISA for sensitive and specific detection of IgA autoantibodies against BP180 in pemphigoid diseases. Orphanet J Rare Dis. 2011;6:31. doi: 10.1186/1750-1172-6-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Vodegel RM, deJong MCJM, Pas HH, Jonkman MF. IgA-mediated epidermolysis bullosa acquisita two cases and review of the literature. J Am Acad Dermatol. 2002;47:919–925. doi: 10.1067/mjd.2002.125079. [DOI] [PubMed] [Google Scholar]
- 140.van der, Steen LP, Bakema JE, Sesarman A, et al. Blocking fca receptor i on granulocytes prevents tissue damage induced by iga autoantibodies. J. Immunol. 2012;189:1594–1601. doi: 10.4049/jimmunol.1101763. [DOI] [PubMed] [Google Scholar]
- 141.Schumann H, Baetge J, Tasanen K, et al. The shed ectodomain of collagen XVII/BP180 is targeted by autoantibodies in different blistering skin diseases. Am J Pathol. 2000;156:685–695. doi: 10.1016/S0002-9440(10)64772-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Florea F, Torio-Padron N, Hashimoto T, Sitaru C. Non-scarring skin blistering disease and mucosal lesions with IgA autoantibodies reactive with collagen VII and IgG reactivity with laminin ?2. Br J Dermatol. 2012;167(4):938–41. doi: 10.1111/j.1365-2133.2012.10946.x. [DOI] [PubMed] [Google Scholar]
- 143.Zillikens D, Kawahara Y, Ishiko A, et al. A novel subepidermal blistering disease with autoantibodies to a 200-kDa antigen of the basement membrane zone. J Invest Dermatol. 1996;106:1333–1338. doi: 10.1111/1523-1747.ep12349283. [DOI] [PubMed] [Google Scholar]
- 144.Dainichi T, Kurono S, Ohyama B, et al. Anti-laminin gamma-1 pemphigoid. Proc Natl Acad Sci USA. 2009;106:2800–2805. doi: 10.1073/pnas.0809230106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Dainichi T, Koga H, Tsuji T, et al. From anti-p200 pemphigoid to anti-laminin gamma1 pemphigoid. J Dermatol. 2010;37:231–238. doi: 10.1111/j.1346-8138.2009.00793.x. [DOI] [PubMed] [Google Scholar]
- 146.Zillikens D, Ishiko A, Jonkman MF, et al. Autoantibodies in anti-p200 pemphigoid stain skin lacking laminin 5 and type VII collagen. Br J Dermatol. 2000;143:1043–1049. doi: 10.1046/j.1365-2133.2000.03841.x. [DOI] [PubMed] [Google Scholar]
- 147.Liu Y, Shimizu H, Hashimoto T. Immunofluorescence studies using skin sections of recessive dystrophic epidermolysis bullosa patients indicated that the antigen of anti-p200 pemphigoid is not a fragment of type VII collagen. J Dermatol Sci. 2003;32:125–129. doi: 10.1016/s0923-1811(03)00092-6. [DOI] [PubMed] [Google Scholar]
- 148.Koga H, Ishii N, Dainichi T, et al. An attempt to develop mouse model for anti-laminin ?1 pemphigoid. J Dermatol Sci. 2013;70:108–15. doi: 10.1016/j.jdermsci.2013.01.001. [DOI] [PubMed] [Google Scholar]
- 149.Dilling A, Rose C, Hashimoto T, Zillikens D, Shimanovich I. Anti-p200 pemphigoid a novel autoimmune subepidermal blistering disease. J Dermatol. 2007;34:1–8. doi: 10.1111/j.1346-8138.2007.00208.x. [DOI] [PubMed] [Google Scholar]
- 150.Groth S, Recke A, Vafia K, et al. Development of a simple enzyme-linked immunosorbent assay for the detection of autoantibodies in anti-p200 pemphigoid. Br J Dermatol. 2011;164:76–82. doi: 10.1111/j.1365-2133.2010.10056.x. [DOI] [PubMed] [Google Scholar]
- 151.Woodley DT, Briggaman RA, O'Keefe EJ, Inman AO, Queen LL, Gammon WR. Identification of the skin basement-membrane autoantigen in epidermolysis bullosa acquisita. N Engl J Med. 1984;310:1007–1013. doi: 10.1056/NEJM198404193101602. [DOI] [PubMed] [Google Scholar]
- 152.Ishii N, Hamada T, Dainichi T, et al. Epidermolysis bullosa acquisita: what's new. J Dermatol. 2010;37:220–230. doi: 10.1111/j.1346-8138.2009.00799.x. [DOI] [PubMed] [Google Scholar]
- 153.Sitaru C. Experimental models of epidermolysis bullosa acquisita. Exp Dermatol. 2007;16:520–531. doi: 10.1111/j.1600-0625.2007.00564.x. [DOI] [PubMed] [Google Scholar]
- 154.Remington J, Chen M, Burnett J, Woodley DT. Autoimmunity to type VII collagen epidermolysis bullosa acquisita. Curr Dir Autoimmun. 2008;10:195–205. doi: 10.1159/000131455. [DOI] [PubMed] [Google Scholar]
- 155.Caux F. Diagnosis and clinical features of epidermolysis bullosa acquisita. Dermatol Clin. 2011;29:485–91. doi: 10.1016/j.det.2011.03.017. [DOI] [PubMed] [Google Scholar]
- 156.Luke MC, Darling TN, Hsu R, et al. Mucosal morbidity in patients with epidermolysis bullosa acquisita. Arch Dermatol. 1999;135:954–959. doi: 10.1001/archderm.135.8.954. [DOI] [PubMed] [Google Scholar]
- 157.Hundorfean G, Neurath MF, Sitaru C. Autoimmunity against type VII collagen in inflammatory bowel disease. J Cell Mol Med. 2010;14:2393–2403. doi: 10.1111/j.1582-4934.2009.00959.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Chen M, Chan LS, Cai X, O'Toole EA, Sample JC, Woodley DT. Development of an ELISA for rapid detection of anti-type VII collagen autoantibodies in epidermolysis bullosa acquisita. J Invest Dermatol. 1997;108:68–72. doi: 10.1111/1523-1747.ep12285634. [DOI] [PubMed] [Google Scholar]
- 159.Saleh MA, Ishii K, Kim Y, et al. Development of NC1 and NC2 domains of type VII collagen ELISA for the diagnosis and analysis of the time course of epidermolysis bullosa acquisita patients. J Dermatol Sci. 2011;62:169–175. doi: 10.1016/j.jdermsci.2011.03.003. [DOI] [PubMed] [Google Scholar]
- 160.Pendaries V, Gasc G, Titeux M, et al. Immune reactivity to type VII collagen implications for gene therapy of recessive dystrophic epidermolysis bullosa. Gene Ther. 2010;17:930–937. doi: 10.1038/gt.2010.36. [DOI] [PubMed] [Google Scholar]
- 161.Licarete E, Ganz S, Recknagel M, et al. Prevalence of collagen VII-specific autoantibodies in patients with autoimmune and inflammatory diseases. BMC Immunol. 2012;13:16. doi: 10.1186/1471-2172-13-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Reunala TL. Dermatitis herpetiformis. Clin Dermatol. 2001;19:728–736. doi: 10.1016/s0738-081x(00)00184-x. [DOI] [PubMed] [Google Scholar]
- 163.Kárpáti S. An exception within the group of autoimmune blistering diseases dermatitis herpetiformis the gluten-sensitive dermopathy. Dermatol Clin. 2011;29:463–8. doi: 10.1016/j.det.2011.03.019. [DOI] [PubMed] [Google Scholar]
- 164.Reunala T. Dermatitis herpetiformis coeliac disease of the skin. Ann Med. 1998;30:416–418. doi: 10.3109/07853899809002482. [DOI] [PubMed] [Google Scholar]
- 165.Caproni M, Antiga E, Melani L, Fabbri P. Guidelines for the diagnosis and treatment of dermatitis herpetiformis. J Eur Acad Dermatol Venereol. 2009;23:633–638. doi: 10.1111/j.1468-3083.2009.03188.x. [DOI] [PubMed] [Google Scholar]
- 166.Dieterich W, Laag E, Bruckner-Tuderman L, et al. Antibodies to tissue transglutaminase as serologic markers in patients with dermatitis herpetiformis. J Invest Dermatol. 1999;113:133–136. doi: 10.1046/j.1523-1747.1999.00627.x. [DOI] [PubMed] [Google Scholar]
- 167.Sárdy M, Kárpáti S, Merkl B, Paulsson M, Smyth N. Epidermal transglutaminase (TGase 3) is the autoantigen of dermatitis herpetiformis. J Exp Med. 2002;195:747–757. doi: 10.1084/jem.20011299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Zettinig G, Weissel M, Flores J, et al. Dermatitis herpetiformis is associated with atrophic but not with goitrous variant of hashimoto's thyroiditis. Eur. J Clin Invest. 2000;30:53–57. doi: 10.1046/j.1365-2362.2000.00590.x. [DOI] [PubMed] [Google Scholar]
- 169.Nakajima K. Recent advances in dermatitis herpetiformis. Clin Dev Immunol. 2012;2012:914162. doi: 10.1155/2012/914162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Iwamoto S, Iwamoto AT, Cha J, et al. The utility of the DNA microarray scanner to simplify the immunofluorescence evaluation of autoimmune bullous diseases. Am J Dermatopathol. 2009;31:218–222. doi: 10.1097/DAD.0b013e31818ffde1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Hiemann R, Büttner T, Krieger T, Roggenbuck D, Sack U, Conrad K. Challenges of automated screening and differentiation of non-organ specific autoantibodies on HEp-2 cells. Autoimmun Rev. 2009;9:17–22. doi: 10.1016/j.autrev.2009.02.033. [DOI] [PubMed] [Google Scholar]
- 172.Sack U, Knoechner S, Warschkau H, Pigla U, Emmrich F, Kamprad M. Computer-assisted classification of HEp-2 immunofluorescence patterns in autoimmune diagnostics. Autoimmun Rev. 2003;2:298–304. doi: 10.1016/s1568-9972(03)00067-3. [DOI] [PubMed] [Google Scholar]
- 173.Rigon A, Soda P, Zennaro D, Iannello G, Afeltra A. Indirect immunofluorescence in autoimmune diseases assessment of digital images for diagnostic purpose. Cytometry B Clin Cytom. 2007;72:472–477. doi: 10.1002/cyto.b.20356. [DOI] [PubMed] [Google Scholar]
- 174.Soda P, Iannello G. Aggregation of classifiers for staining pattern recognition in antinuclear autoantibodies analysis. IEEE Trans Inf Technol Biomed. 2009;13:322–329. doi: 10.1109/TITB.2008.2010855. [DOI] [PubMed] [Google Scholar]
- 175.Rimm DL, Camp RL, Charette LA, Costa J, Olsen DA, Reiss M. Tissue microarray a new technology for amplification of tissue resources. Cancer J. 2001;7:24–31. [PubMed] [Google Scholar]
- 176.Hart T, Zhao A, Garg A, Bolusani S, Marcotte EM. Human cell chips adapting DNA microarray spotting technology to cell-based imaging assays. PLoS ONE. 2009;4:e7088. doi: 10.1371/journal.pone.0007088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Rosenbach M, Murrell DF, Bystryn J, et al. Reliability and convergent validity of two outcome instruments for pemphigus. J Invest Dermatol. 2009;129:2404–2410. doi: 10.1038/jid.2009.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Schmidt E, Dähnrich C, Rosemann A, et al. Novel ELISA systems for antibodies to desmoglein 1 and 3 correlation of disease activity with serum autoantibody levels in individual pemphigus patients. Exp Dermatol. 2010;19:458–463. doi: 10.1111/j.1600-0625.2010.01069.x. [DOI] [PubMed] [Google Scholar]
- 179.Huang Y, Bu D, Zhu Y. Sensitive enzyme-linked immunosorbent assay for detection of circulating anti-peri and envo autoantibodies in patients with paraneoplastic pemphigus. J Invest Dermatol. 2008;128:S63. [Google Scholar]
- 180.Probst C, Schlumberger W, Stöcker W, et al. Development of ELISA for the specific determination of autoantibodies against envoplakin and periplakin in paraneoplastic pemphigus. Clin Chim Acta. 2009;410:13–18. doi: 10.1016/j.cca.2009.08.022. [DOI] [PubMed] [Google Scholar]
- 181.Mouquet H, Drenovska K, Lartigue A, et al. Detection and characterization of anti-envoplakin linker autoantibodies in paraneoplastic pemphigus using specific bead-based assay. Clin Immunol. 2008;129:304–312. doi: 10.1016/j.clim.2008.07.021. [DOI] [PubMed] [Google Scholar]
- 182.Giudice GJ, Wilske KC, Anhalt GJ, et al. Development of an ELISA to detect anti-BP180 autoantibodies in bullous pemphigoid and herpes gestationis. J Invest Dermatol. 1994;102:878–881. doi: 10.1111/1523-1747.ep12382738. [DOI] [PubMed] [Google Scholar]
- 183.Zillikens D, Mascaro JM, Rose PA, et al. A highly sensitive enzyme-linked immunosorbent assay for the detection of circulating anti-BP180 autoantibodies in patients with bullous pemphigoid. J Invest Dermatol. 1997;109:679–683. doi: 10.1111/1523-1747.ep12338088. [DOI] [PubMed] [Google Scholar]
- 184.Ishiura N, Fujimoto M, Watanabe R, et al. Serum levels of IgE anti-BP180 and anti-BP230 autoantibodies in patients with bullous pemphigoid. J Dermatol Sci. 2008;49:153–161. doi: 10.1016/j.jdermsci.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 185.Chen M, Chan LS, Cai X, O'Toole EA, Sample JC, Woodley DT. Development of an ELISA for rapid detection of anti-type VII collagen autoantibodies in epidermolysis bullosa acquisita. J Invest Dermatol. 1997;108:68–72. doi: 10.1111/1523-1747.ep12285634. [DOI] [PubMed] [Google Scholar]
- 186.Komorowski L, Müller R, Vorobyev A, et al. Sensitive and specific assays for routine serological diagnosis of epidermolysis bullosa acquisita. J Am Acad Dermatol. 2013;68:e89–95. doi: 10.1016/j.jaad.2011.12.032. [DOI] [PubMed] [Google Scholar]
- 187.Adornetto G, Volpe G, DeStefano A, et al. An ELIME assay for the rapid diagnosis of coeliac disease. Anal Bioanal Chem. 2012;403:1191–4. doi: 10.1007/s00216-011-5702-z. [DOI] [PubMed] [Google Scholar]
- 188.Kasperkiewicz M, Dähnrich C, Probst C, et al. Novel assay for detecting celiac disease-associated autoantibodies in dermatitis herpetiformis using deamidated gliadin-analogous fusion peptides. J Am Acad Dermatol. 2012;66:583–588. doi: 10.1016/j.jaad.2011.02.025. [DOI] [PubMed] [Google Scholar]
- 189.Acostamadiedo JM, Perniciaro C. Rogers RS3.Phenytoin-induced linear IgA bullous disease. J Am Acad Dermatol. 1998;38:352–356. doi: 10.1016/s0190-9622(98)70582-1. [DOI] [PubMed] [Google Scholar]
- 190.Armstrong AW, Fazeli A, Yeh SW, Mackool BT, Liu V. Vancomycin-induced linear IgA disease manifesting as bullous erythema multiforme. J Cutan Pathol. 2004;31:393–397. doi: 10.1111/j.0303-6987.2004.00190.x. [DOI] [PubMed] [Google Scholar]
- 191.Bitman LM, Grossman ME, Ross H. Bullous drug eruption treated with amputation.A challenging case of vancomycin-induced linear IgA disease. . Arch Dermatol. 1996;132:1289–1290. [PubMed] [Google Scholar]
- 192.Brinkmeier T, Angelkort B, Frosch PJ, Herbst RA. [Vancomycin-induced linear IgA dermatosis]. J Dtsch Dermatol Ges. 2003;1:212–214. doi: 10.1046/j.1610-0387.2003.02037.x. [DOI] [PubMed] [Google Scholar]
- 193.Khan I, Hughes R, Curran S, Marren P. Drug-associated linear IgA disease mimicking toxic epidermal necrolysis. Clin Exp Dermatol. 2009;34:715–717. doi: 10.1111/j.1365-2230.2008.03011.x. [DOI] [PubMed] [Google Scholar]
- 194.Montagnac R, Reguiaï Z, Méhaut S, Bressieux JM, Schillinger F. [Drug induced linear IgA bullous dermatosis]. Nephrologie. 2003;24:287–292. [PubMed] [Google Scholar]
- 195.Palmer RA, Ogg G, Allen J, et al. Vancomycin-induced linear IgA disease with autoantibodies to BP180 and LAD285. Br J Dermatol. 2001;145:816–820. doi: 10.1046/j.1365-2133.2001.04492.x. [DOI] [PubMed] [Google Scholar]
- 196.Whitworth JM, Thomas I, Peltz SA, Sullivan BC, Wolf AH, Cytryn AS. Vancomycin-induced linear IgA bullous dermatosis (LABD). J Am Acad Dermatol. 1996;34:890–891. doi: 10.1016/s0190-9622(96)90073-0. [DOI] [PubMed] [Google Scholar]
- 197.Baden LA, Apovian C, Imber MJ, Dover JS. Vancomycin-induced linear IgA bullous dermatosis. Arch Dermatol. 1988;124:1186–1188. [PubMed] [Google Scholar]
- 198.Carpenter S, Berg D, Sidhu-Malik N. Hall RP 3rd, Rico MJ.Vancomycin-associated linear IgA dermatosis. A report of three cases. J Am Acad Dermatol. 1992;26:45–48. doi: 10.1016/0190-9622(92)70004-y. [DOI] [PubMed] [Google Scholar]
- 199.Piketty C, Meeus F, Nochy D, Poux JM, Jacquot C, Bariety J. Linear IgA dermatosis related to vancomycin. Br J Dermatol. 1994;130:130–131. doi: 10.1111/j.1365-2133.1994.tb06904.x. [DOI] [PubMed] [Google Scholar]
- 200.Geissmann C, Beylot-Barry M, Doutre MS, Beylot C. Drug-induced linear IgA bullous dermatosis. J Am Acad Dermatol. 1995;32:296. doi: 10.1016/0190-9622(95)90156-6. [DOI] [PubMed] [Google Scholar]
- 201.Richards SS, Hall S, Yokel B, Whitmore SE. A bullous eruption in an elderly woman.Vancomycin-associated linear IgA dermatosis (LAD). . Arch Dermatol. 1995;131:1447–8. doi: 10.1001/archderm.131.12.1447b. [DOI] [PubMed] [Google Scholar]
- 202.Espagne E, Prost C, Chosidow O, Saïag P, Revuz J, Roujeau JC. [Linear IgA drug-induced dermatosis.Report of 3 cases]. . Ann Dermatol Venereol. 1990;117:898–899. [PubMed] [Google Scholar]
- 203.Jawitz RS, Krach K, Schapiro B. A vesiculobullous eruption in a hospitalized patient.Diagnosis. Drug-induced linear IgA bullous dermatosis (LAD) with eosinophils. Arch Dermatol. 2011;147:1443–1448. doi: 10.1001/archderm.147.12.1443-c. [DOI] [PubMed] [Google Scholar]
- 204.Kuechle MK, Stegemeir E, Maynard B, Gibson LE, Leiferman KM, Peters MS. Drug-induced linear IgA bullous dermatosis: report of six cases and review of the literature. J Am Acad Dermatol. 1994;30:187–192. doi: 10.1016/s0190-9622(94)70015-x. [DOI] [PubMed] [Google Scholar]
- 205.Combemale P, Gavaud C, Cozzani E, Nicolas JF, Guennoc B, Dusseau JY. [Linear IgA dermatosis induced by penicillin G]. Ann Dermatol Venereol. 1993;120:847–848. [PubMed] [Google Scholar]
- 206.Wozniak K, Kowalewski C, Hashimoto T, Ishii N, Glinska-Wielochowska M, Schwartz RA. Penicillin-induced anti-p200 pemphigoid an unusual morphology. Acta Derm Venereol. 2006;86:443–446. doi: 10.2340/00015555-0117. [DOI] [PubMed] [Google Scholar]
- 207.Shimanovich I, Rose C, Sitaru C, Bröcker E, Zillikens D. Localized linear IgA disease induced by ampicillin sulbactam. J Am Acad Dermatol. 2004;51:95–98. doi: 10.1016/j.jaad.2004.03.027. [DOI] [PubMed] [Google Scholar]
- 208.McWhirter JD, Hashimoto K, Fayne S, Ito K. Linear IgA bullous dermatosis related to lithium carbonate. Arch Dermatol. 1987;123:1120–1122. [PubMed] [Google Scholar]
- 209.Primka EJ3rd, Liranzo MO, Bergfeld WF, Dijkstra JW. Amiodarone-induced linear IgA disease. J Am Acad Dermatol. 1994;31:809–811. doi: 10.1016/s0190-9622(09)80051-0. [DOI] [PubMed] [Google Scholar]
- 210.König C, Eickert A, Scharfetter-Kochanek K, Krieg T, Hunzelmann N. Linear IgA bullous dermatosis induced by atorvastatin. J Am Acad Dermatol. 2001;44:689–692. doi: 10.1067/mjd.2001.113462. [DOI] [PubMed] [Google Scholar]
- 211.Durdu M, Baba M, Seçkin D. A case of bullous pemphigoid induced by aspirin. J Am Acad Dermatol. 2011;65:443–444. doi: 10.1016/j.jaad.2010.02.032. [DOI] [PubMed] [Google Scholar]
- 212.Gabrielsen TO, Staerfelt F, Thune PO. Drug-induced bullous dermatosis with linear IgA deposits along the basement membrane. Acta Derm Venereol. 1981;61:439–441. [PubMed] [Google Scholar]
- 213.Valsecchi R, Serra M, Tornaghi A, Cainelli T. [Drug-induced bullous dermatosis with linear IgA]. G Ital Dermatol Venereol. 1982;117:221–223. [PubMed] [Google Scholar]
- 214.Bialy-Golan A, Brenner S. Penicillamine-induced bullous dermatoses. J Am Acad Dermatol. 1996;35:732–742. doi: 10.1016/s0190-9622(96)90729-x. [DOI] [PubMed] [Google Scholar]
- 215.Brenner S, Wolf R, Ruocco V. Drug-induced pemphigus. I. A survey. Clin Dermatol. 1993;11:501–505. doi: 10.1016/0738-081x(93)90157-8. [DOI] [PubMed] [Google Scholar]
- 216.Aghassi D, Dover JS. Pemphigus foliaceus induced by psoralen-UV-A. Arch Dermatol. 1998;134:1300–1301. doi: 10.1001/archderm.134.10.1300-a. [DOI] [PubMed] [Google Scholar]
- 217.Fryer EJ, Lebwohl M. Pemphigus vulgaris after initiation of psoralen and UVA therapy for psoriasis. J Am Acad Dermatol. 1994;30:651–653. doi: 10.1016/s0190-9622(09)80116-3. [DOI] [PubMed] [Google Scholar]
- 218.Perl S, Rappersberger K, Födinger D, Anegg B, Hönigsmann H, Ortel B. Bullous pemphigoid induced by PUVA therapy. Dermatology. 1996;193:245–247. doi: 10.1159/000246255. [DOI] [PubMed] [Google Scholar]
- 219.Abel EA, Bennett A. Bullous pemphigoid.Occurrence in psoriasis treated with psoralens plus long-wave ultraviolet radiation. Arch Dermatol. 1979;115:988–989. doi: 10.1001/archderm.115.8.988. [DOI] [PubMed] [Google Scholar]
- 220.Robinson JK, Baughman RD, Provost TT. Bullous pemphigoid induced by PUVA therapy.Is this the aetiology of the acral bullae produced during PUVA treatment. Br J Dermatol. 1978;99:709–713. doi: 10.1111/j.1365-2133.1978.tb07067.x. [DOI] [PubMed] [Google Scholar]
- 221.Deschamps P, Pedailles S, Michel M, Leroy D. Photo-induction of lesions in a patient with pemphigus erythematosus. Photodermatol. 1984;1:38–41. [PubMed] [Google Scholar]
- 222.Sanchez-Palacios C, Chan LS. Development of pemphigus herpetiformis in a patient with psoriasis receiving UV-light treatment. J Cutan Pathol. 2004;31:346–349. doi: 10.1111/j.0303-6987.2004.0188.x. [DOI] [PubMed] [Google Scholar]
- 223.Jappe U, Zillikens D, Bonnekoh B, Gollnick H. Epidermolysis bullosa acquisita with ultraviolet radiationsensitivity. Br J Dermatol. 2000;142:517–520. doi: 10.1046/j.1365-2133.2000.03368.x. [DOI] [PubMed] [Google Scholar]
- 224.Kaplan I, Hodak E, Ackerman L, Mimouni D, Anhalt GJ, Calderon S. Neoplasms associated with paraneoplastic pemphigus a review with emphasis on non-hematologic malignancy and oral mucosal manifestations. Oral Oncol. 2004;40:553–562. doi: 10.1016/j.oraloncology.2003.09.020. [DOI] [PubMed] [Google Scholar]
- 225.Wang J, Zhu X, Li R, et al. Paraneoplastic pemphigus associated with Castleman tumor a commonly reported subtype of paraneoplastic pemphigus in China. Arch Dermatol. 2005;141:1285–1293. doi: 10.1001/archderm.141.10.1285. [DOI] [PubMed] [Google Scholar]
- 226.Dega H, Laporte JL, Joly P, et al. Paraneoplastic pemphigus associated with Hodgkin's disease. Br J Dermatol. 1998;138:196–198. doi: 10.1046/j.1365-2133.1998.02056.x. [DOI] [PubMed] [Google Scholar]
- 227.Tilakaratne W, Dissanayake M. Paraneoplastic pemphigus a case report and review of literature. Oral Dis. 2005;11:326–329. doi: 10.1111/j.1601-0825.2005.01116.x. [DOI] [PubMed] [Google Scholar]
- 228.Wang J, Bu DF, Li T, et al. Autoantibody production from a thymoma and a follicular dendritic cell sarcoma associated with paraneoplastic pemphigus. Br J Dermatol. 2005;153:558–564. doi: 10.1111/j.1365-2133.2005.06599.x. [DOI] [PubMed] [Google Scholar]
- 229.McKee PH, McClelland M, Sandford JC. Co-existence of pemphigus anti-skeletal muscle antibody and a retroperitoneal paraganglioma. Br J Dermatol. 1978;99:441–445. doi: 10.1111/j.1365-2133.1978.tb06185.x. [DOI] [PubMed] [Google Scholar]
- 230.Eccersley LRJ, Hoffbrand AV, Rustin MHA, McNamara CJ. Paraneoplastic pemphigus associated with systemic mastocytosis. Am J Hematol. 2009;84:847–848. doi: 10.1002/ajh.21462. [DOI] [PubMed] [Google Scholar]
- 231.Trüeb RM, Didierjean L, Fellas A, Elias A, Borradori L. Childhood bullous pemphigoid report of a case with characterization of the targeted antigens. J Am Acad Dermatol. 1999;40:338–344. doi: 10.1016/s0190-9622(99)70481-0. [DOI] [PubMed] [Google Scholar]
- 232.Chimanovitch I, Hamm H, Georgi M, et al. Bullous pemphigoid of childhood autoantibodies target the same epitopes within the NC16A domain of BP180 as autoantibodies in bullous pemphigoid of adulthood. Arch Dermatol. 2000;136:527–532. doi: 10.1001/archderm.136.4.527. [DOI] [PubMed] [Google Scholar]
- 233.Cliff S, Holden CA. Pemphigoid nodularis a report of three cases and review of the literature. Br J Dermatol. 1997;136:398–401. [PubMed] [Google Scholar]
- 234.Powell AM, Albert S, Gratian MJ, Bittencourt R, Bhogal BS, Black MM. Pemphigoid nodularis (non-bullous) a clinicopathological study of five cases. Br J Dermatol. 2002;147:343–349. doi: 10.1046/j.1365-2133.2002.04754.x. [DOI] [PubMed] [Google Scholar]
- 235.Schmidt E, Sitaru C, Schubert B, et al. Subacute prurigo variant of bullous pemphigoid autoantibodies show the same specificity compared with classic bullous pemphigoid. J Am Acad Dermatol. 2002;47:133–136. doi: 10.1067/mjd.2002.120445. [DOI] [PubMed] [Google Scholar]
- 236.Korman NJ, Woods SG. Erythrodermic bullous pemphigoid is a clinical variant of bullous pemphigoid. Br J Dermatol. 1995;133:967–971. doi: 10.1111/j.1365-2133.1995.tb06935.x. [DOI] [PubMed] [Google Scholar]
- 237.Alonso-Llamazares J, Dietrich SM, Gibson LE. Bullous pemphigoid presenting as exfoliative erythroderma. J Am Acad Dermatol. 1998;39:827–830. doi: 10.1016/s0190-9622(98)70358-5. [DOI] [PubMed] [Google Scholar]
- 238.Levine N, Freilich A, Barland P. Localized pemphigoid simulating dyshidrosiform dermatitis. Arch Dermatol. 1979;115:320–321. [PubMed] [Google Scholar]
- 239.Caldarola G, Fania L, Cozzani E, Feliciani C, DeSimone C. Dyshidrosiform pemphigoid a well-defined clinical entity. Eur J Dermatol. 2011;21:112–113. doi: 10.1684/ejd.2010.1172. [DOI] [PubMed] [Google Scholar]
- 240.Chan LS, Dorman MA, Agha A, Suzuki T, Cooper KD, Hashimoto K. Pemphigoid vegetans represents a bullous pemphigoid variant.Patient's IgG autoantibodies identify the major bullous pemphigoid antigen. J Am Acad Dermatol. 1993;28:331–335. doi: 10.1016/0190-9622(93)70048-x. [DOI] [PubMed] [Google Scholar]
- 241.Mora RG, Nesbitt LTJ, Brantley JB. Lichen planus pemphigoides clinical and immunofluorescent findings in four cases. J Am Acad Dermatol. 1983;8:331–336. doi: 10.1016/s0190-9622(83)70035-6. [DOI] [PubMed] [Google Scholar]
- 242.Lang PGJ, Maize JC. Coexisting lichen planus and bullous pemphigoid or lichen planus pemphigoides. J Am Acad Dermatol. 1983;9:133–140. doi: 10.1016/s0190-9622(83)70119-2. [DOI] [PubMed] [Google Scholar]
- 243.Maceyko RF, Camisa C, Bergfeld WF, Valenzuela R. Oral and cutaneous lichen planus pemphigoides. J Am Acad Dermatol. 1992;27:889–892. doi: 10.1016/0190-9622(92)70275-k. [DOI] [PubMed] [Google Scholar]
- 244.Cohen DM, Ben-Amitai D, Feinmesser M, Zvulunov A. Childhood lichen planus pemphigoides a case report and review of the literature. Pediatr Dermatol. 2009;26:569–574. doi: 10.1111/j.1525-1470.2009.00988.x. [DOI] [PubMed] [Google Scholar]