Abstract
Objectives
Patients with acute myocardial infarction (AMI) who are admitted to hospitals without coronary revascularization are frequently transferred to hospitals with this capability. We sought to determine if the timeliness of hospital transfer and quality of destination hospitals differed between black and white patients.
Methods
We evaluated all white and black Medicare beneficiaries admitted with AMI at non-revascularization hospitals in 2006 who were transferred to a revascularization hospital. We compared hospital length of stay prior to transfer and the transfer destination's 30-day risk-standardized mortality rate (RSMR) for AMI between black and white patients. We used hierarchical regression to adjust for patient characteristics and examine within- and across-hospital effects of race on 30-day mortality and length of stay prior to transfer.
Results
A total of 25,947 (42%) white and 2,345 (37%) black patients with AMI were transferred from 857 urban and 774 rural non-revascularization hospitals to 928 revascularization hospitals. Median (IQR) length of stay prior to transfer was 1 day (1-3) for white patients and 2 days (1-4) for black patients (p<0.001). In adjusted models, black patients tended to be transferred more slowly than white patients, a finding due to both across-hospital and within-hospital effects. For example, within an given urban hospital black patients were transferred an additional 0.24 days (95% CI 0.03-0.44) later than white patients. Additionally, the lengths of stay prior to transfer for all patients at urban hospitals increased by 0.37 days (95% CI 0.28-0.47) for every 20% increase in the proportion of AMI patients who were black. These results were attenuated in rural hospitals. The RSMR of the revascularization hospital to which patients were ultimately sent did not differ between black and white patients
Conclusions
Black patients are transferred more slowly to revascularization hospitals after AMI than white patients, resulting from both less timely transfers within hospitals as well as admission to hospitals with greater delays in transfer; however, 30-day mortality of the revascularization hospital to which both groups were sent to appeared similar. Race-based delays in transfer may contribute to known racial disparities in outcomes of AMI.
Keywords: Healthcare Disparities, Patient Transfer, Critical Care, Cardiovascular Diseases, Quality Indicators
Introduction
An extensive body of evidence documents racial and ethnic disparities in the patterns of cardiovascular care.1-10 The majority of prior research into the root causes of disparities in cardiovascular care focused on the role of the individual practitioner, or how care within a hospital differs across race and ethnicity.11, 12 Yet recent work demonstrates that the health care system, particularly the hospital, also contributes to racial and ethnic inequalities in cardiovascular care.7, 13 Multiple studies illustrate that hospitals that disproportionately serve black patients have fewer resources and often provide worse care to all patients with acute myocardial infarction (AMI), regardless of race.14, 15
These issues may also play out in the interhospital transfer of patients with AMI, but this important process has never been examined in this light. Most hospitals lack the capacity to revascularize AMI patients, and 75,000 patients with AMI are admitted to such hospitals annually in Medicare alone.16 Guidelines suggest that patients with ST-elevation MI should be transferred to a revascularization center early in their course, in many cases prior to admission.17 In addition, most non-ST-elevation MI patients also likely benefit from prompt transfer to a revascularization center within 48 hours or upon failure of medical therapy, usually after an initial admission to the non-revascularization hospital.18 Differential transfer patterns by race may therefore influence disparities in access to care and outcomes, and -- since many revascularized patients arrive for their procedure as transfers from another hospital – differential transfer may be responsible for many black patients receiving revascularization in hospitals with worse risk adjusted mortality.13, 19 Several studies suggest that black patients may be less likely to be transferred to revascularization hospitals, and when transferred are more likely to be sent 48 hours after admission compared to white patients.20-23 However, the magnitude of transfer delay (i.e. hours or days) is not clear, nor is the extent to which these differences in transfer timing are attributable to practice patterns within a hospital or across hospitals. Further, although it has been shown that potential transfer destinations vary widely in the quality of care that they provide,13, 16 there has been no systematic study of racial differentials in where patients are sent.
Given the essential – and likely growing – role of interhospital transfer in the care of AMI patients, we sought to use this as a model system in which to understand the processes of care that may lead to cardiovascular disparities. We hypothesized that racial differences might be present in three distinct ways during the transfer process. First, we hypothesized that black patients would be transferred more slowly than white patients within any given hospital.20-23 Second, we hypothesized that hospitals with a higher percentage of black patients would transfer all of their patients more slowly than those serving more predominantly white patient populations.7 Third, we hypothesized that, once transferred, black patients would be transferred to hospitals with worse 30-day risk-standardized mortality rates than would white patients.13, 19
Methods
Study design, data sources and study population
We performed a retrospective cohort analysis utilizing all fee-for-service Medicare beneficiaries in the 2006 Medicare Provider Analysis and Review (MedPAR) files admitted with a new primary diagnosis of AMI, defined as ICD-9-CM code of 410.xx (excluding 410.x2, prior diagnosis of AMI). We defined revascularization hospitals as those that performed at least 5 coronary bypass grafting (CABG) and percutaneous coronary intervention (PCI) procedures during the year.24, 25 For this analysis, we only included patients initially admitted to non-revascularization hospitals with at least 10 AMI admissions during the calendar year in order to allow more reliable estimates of our outcomes of interest. We excluded patients from hospitals that performed PCI but did not perform CABG because such facilities receive very few transfers from non-revascularization hospitals and have distinct rationales for transferring out patients, such as rescue CABG after failed PCI.26
We defined interhospital transfers as temporally adjacent hospitalizations in the same patient at two different facilities; the discharge day for the nonrevascularization hospital had to be the same or one day less than the admitting date of the revascularization hospital.27, 28 Data on hospital geographic location and academic affiliation were obtained from the 2005 American Hospital Association (AHA) Annual Survey.29 We defined hospitals as being an urban or rural facility based on metropolitan statistical area.
Race is recorded in Medicare's administrative files primarily using data provided to the Social Security Administration by self-report. The sensitivity of this variable for white and black persons is > 95% but considerably lower (<60%) for others.30 Thus, we limited the analysis to patients self-identified as white or black. Socioeconomic data was obtained by linking patient ZIP code to the 2000 US Census.
We used 30-day risk-standardized mortality rates (RSMR) for AMI from publically available data for each hospital during 2006 on the website Hospital Compare.31 Briefly, risk-adjusted mortality rates are calculated from Medicare inpatient and outpatient claims data using hierarchical regression models of each hospitals mortality rate.32, 33 We calculated length of stay (LOS) as the total number of days spent in the transferring hospital prior to transfer.
We limited our analyses to AMI patients at hospitals in the 50 states and the District of Columbia. We also excluded those patients treated at nonrevascularization hospitals with incomplete data on facility characteristics (n=18).
Statistical analysis
To determine the association between race and the timeliness of transfer, we compared the adjusted mean differences in the LOS at the transferring hospital across race groups using linear mixed models.34 Because we were interested in determining whether hospitals that serve greater proportions of black patients systematically transfer their patients more slowly, we partitioned the covariate for race into two components – a within-center component and an across-center component.35 This partitioning allowed us to fit a conditional model using a random effects framework. The across-center component was a variable representing the proportion of AMI patients who are black (pi) presenting to that particular hospital. Thus, all patients presenting to that hospital, regardless of race, have the same value for pi. The within-center component is simply the individual's own racial group (xij) represented as a dichotomous indicator variable; we included this in the model as a group-mean-centered variable. Both variables were modeled simultaneously in a regression where LOS prior to transfer was the outcome. The coefficient for the across-center variable describes the mean difference in LOS, regardless of an individual's race, for a unit change in the proportion of black patients with AMI between centers. The coefficient for the within-center variable describes the mean difference in LOS for black vs. white patients who are transferred from the same center.
To examine the association between race and the quality of transfer, we compared the adjusted mean RSMR at the revascularization hospital to which the patient was ultimately sent across race groups after decomposing the race variable into within- and across-center components as described above. We used linear mixed models with transferring hospital entered as a random effect.
All models were adjusted for age, gender, total volume of black or white AMI patients presenting to the transferring hospital, day of the week on date of admission, patient use of critical care services, and the ZIP code-level percent below poverty and median household income assigned to each patient, unless specified. Black versus white comparisons were stratified by urban/rural status of the transferring hospital by including an interaction term.
We performed several sensitivity analyses to determine the robustness of our findings to various assumptions. First, we limited the cohort to only patients who actually received a PCI or CABG at the receiving hospital (n=17,760). Second, we repeated the original RSMR analysis after limiting the cohort to patients who were transferred on the same day they presented with AMI (n=4,260).
Analyses were conducted using Stata 11 (StataCorp. College Station, TX). Tests of significance used a two sided p≤0.05. The Institutional Review Board for the University of Michigan approved the study.
Results
There were 61,799 white and 6,294 black patients admitted with AMI to 857 urban and 774 rural, non-revascularization hospitals in Medicare in 2006. Of these patients, 25,947 white (42.0%) and 2,345 black (37.3%) patients were transferred to revascularization hospitals (p<0.001). Baseline demographic characteristics for patients who were transferred to revascularization hospitals are presented in Table 1. Black patients were younger, more often male, and resided lower socioeconomic areas. Forty-seven percent of hospitals in the analysis were rural. The care of black AMI patients was highly concentrated. Only 13% of rural hospitals admitted more than five or more black patients with AMI during the one-year study period, and 26% of urban hospitals admitted five or more black patients with AMI. Additional hospital and aggregate patient characteristics for rural and urban hospitals are presented in eTable 1 (Supplemental Digital Content).
Table 1.
Characteristics of Medicare patients transferred from non-revascularization to revascularization hospitals
| Characteristic | White (n=25947) | Black (n=2345) | p value |
|---|---|---|---|
| Age, years | 75 (9) | 70 (11) | <0.001 |
| Female, % | 55 | 47 | <0.001 |
| Critically ill, % | 30 | 28 | 0.27 |
| Distance to receiving hospital, miles, median (IQR) | 26.2 (12-45) | 16.1 (6.4-36) | <0.001 |
| Socioeconomic characteristics | |||
| Present to rural hospital % | 42 | 32 | <0.001 |
| % below poverty*, mean (SD) | 12 (7) | 19 (10) | <0.001 |
| Median household income*, thousands $US, mean (SD) | 41.2 (15) | 35.4 (13) | <0.001 |
| % with less than high-school education*, mean (SD) | 21 (10) | 28 (11) | <0.001 |
data abstracted at level of ZIP code
IQR, interquartile range; SD, standard deviation
Black patients had significantly longer mean and median lengths-of-stay in the sending hospital prior to transfer than white patients (Table 2). After multivariable adjustment, black patients tended to be transferred more slowly than white patients, a finding due to both within-hospital and across-hospital and effects. Within any given urban hospital, black patients were transferred an additional 0.24 days (95% CI 0.03-0.44) later than white patients. Further, urban hospitals where a greater proportion of admitted patients with AMI are black tended to transfer all patients more slowly, regardless of the race of the individual. The lengths of stay prior to transfer for all patients in these hospitals increased by 0.37 days (95% CI 0.28-0.47) for every 20% increase in the proportion of admitted AMI patients who were black. Rural hospitals did not exhibit an association between pre-transfer LOS and the proportion of admitted AMI patients who were black (0.08 days per 20% increase in % of AMI patients who are black, 95% CI −0.01-0.17); however, even within these rural hospitals, statistically significant black vs. white differences persisted at the patient-level (0.23 days, 95% CI 0.05-0.41 for black versus white patients within a hospital).
Table 2.
Unadjusted outcomes for white and black patients who are transferred to revascularization hospitals
| Characteristic | White (n=25947) | Black (n=2345) | p value |
|---|---|---|---|
| AMI risk-standardized mortality rate at receiving hospital, mean (95% CI) | 15.9 (15.8-15.9) | 15.9 (15.8-16.0) | 0.054 |
| Quintile of AMI risk-standardized mortality rate at receiving hospital (%) | 0.07 | ||
| 1 (10.8 -14.7%) | 32.5 | 32.2 | |
| 2 (14.8 -15.7%) | 19.5 | 19.6 | |
| 3 (15.8 -16.5%) | 15.9 | 15.2 | |
| 4 (16.6 -17.5%) | 16.3 | 18.4 | |
| 5 (17.6 - 22.1%) | 15.9 | 14.5 | |
| LOS at sending hospital, days | |||
| median (IQR) | 1 (1-3) | 2 (1-4) | <0.001 |
| mean (SD) | 2.39 (2.8) | 3.04 (3.6) | <0.001 |
| LOS at receiving hospital, days | |||
| median (IQR) | 4 (2-8) | 4 (2-8) | 0.29 |
| mean (SD) | 6.28 (7.4) | 6.70 (8.2) | 0.02 |
| PCI or CABG at receiving hospital, % | 63 | 57 | <0.001 |
AMI, acute myocardial infarction; CABG, coronary artery bypass graft; LOS, length of stay; PCI, percutaneous coronary intervention; Sd, standard deviation
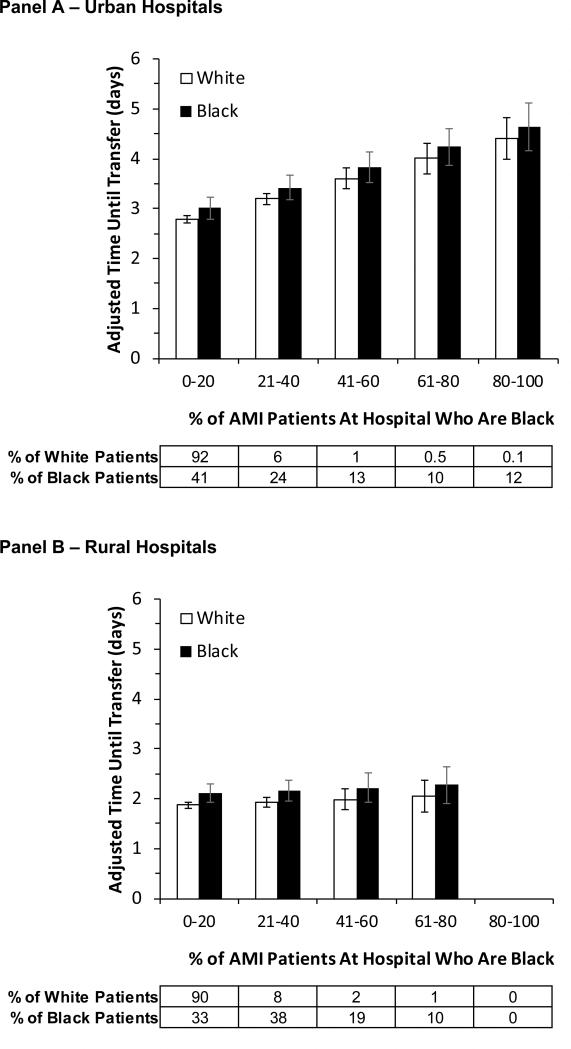
These within- and across-hospital effects are additive, and can result in large differences in timing of transfer across race groups (Figure). For example, black patients presenting to an urban hospital where only 80% of AMI patients are black would, on average, be transferred 1.12 days later than a white patient presenting to an urban hospital where 20% of AMI patients are black.
Figure.
Effect of race on within-center and across-center differences in the timeliness of transfer for urban and rural non-revascularization hospitals. Each panel presents the adjusted length of stay for black (black) and white (gray) patients at urban (Panel A) and rural (Panel B) non-revascularization hospitals prior to transfer as a function of the percent of all AMI patients presenting to that hospital who are black. The difference between the black and white bars represents the difference in adjusted length of stay for black and white patients presenting to the same hospital. Adjusted lengths of stay are presented when all other covariates in the model are set to their means.
On unadjusted analysis, there were no differences in the 30-day risk-standardized mortality rate (RSMR) at hospitals to which black and white patient transfers were sent to, whether comparing means (15.9% vs 15.9%, respectively, p=0.054) or across quintiles of RSMR (p=0.07) (Table 2). Adjusted marginal estimates for the RSMR were 15.7% (95% CI 15.6-15.8%) for black and 15.7% (95% CI 15.6-15.8%) for white patients. This result did not differ by the proportion of black patients(p=0.65) or by urban/rural status of the transferring hospital (p value for interaction = 0.076).
On sensitivity analysis, differences in LOS did not significantly change when the analysis was limited to only patients who were revascularized at the receiving hospital (eTable 2). There were also no consistent differences in RSMR across race groups when restricting the analysis to patients transferred on the day of presentation or to only those revascularized once transferred (eTable 3).
Discussion
Among Medicare beneficiaries in 2006, we found evidence for two of our three hypotheses about the mechanisms generating racial differentials in transfer patterns. We found that black patients admitted to non-revascularization hospitals were less likely to be transferred to revascularization hospitals. When transferred, black patients were transferred more slowly to revascularization hospitals than white patients, resulting from both differential transfer times within any given hospital and, more importantly, because hospitals that see a large proportion of black patients transfer all patients more slowly. These within and across hospital differences in the timing of transfer support our first two hypotheses. However, contrary to our third hypothesis, there were no systematic differences in the quality of the revascularization hospitals to which black or white patients were sent. Together these data suggest that within-hospital processes play a much less of a role in generating racial differentials, whereas differences between hospitals may be quite important.
Our work extends a new body of literature showing that differences between hospitals can play a critical role in maintaining racial differences in care – that is, that the differences in care between hospitals are in some cases substantially greater than the differences in care within a given hospital.36-38 Several processes of care delivered to patients with AMI show broader racial differentials between rather than within hospitals.7, 39 To our knowledge, our study is the first study that quantifies the differentials in interhospital transfer for percutaneous coronary intervention, and how hospitals may accentuate such differentials.20-23 These findings have important implications for how we think about interventions to reduce racial disparities in cardiovascular care – they strongly argue that remediation focused on racism or individual providers will be limited in its ability to change population outcomes, even if it is able to fully achieve the salutary outcome of eliminating within hospital differences in treatment.
There are several potential explanations for the greater delays in transfer at hospitals serving larger minority populations.40 Prior research indicates that hospitals caring for greater proportions of black patients are more likely to care for Medicaid patients and have lower nurse-to-patient ratios.41 Strapped by financial constraints, safety-net hospitals may forego development of a “quality improvement culture” or limit adoption of computer order entry or electronic medical records, infrastructure which may improve the quality of care.42 Such factors may work in concert to reduce the quality of care delivered at these hospitals and may contribute to the rural/urban differences we observed. An appropriate next step in cardiovascular care is to characterize and address the organizational factors that allow such delays to exist and to determine the impact of these delays clinical outcomes.
Our study has several important limitations. First, we excluded patients of all races other than black or white. We also excluded enrollees participating in a Medicare advantage plan and other Medicare beneficiaries under 65 years. Because insurers outside of Medicare may orchestrate transfers with different economic or clinical incentives, we wanted to hold constant the effects of insurance in order to try to avoid confounding of race by insurance status.43 Further work is needed to elucidate transfer patterns across race outside of Medicare. We were also unable to fully characterize the factors driving the transfer decision or the reasons why black patients were transferred less frequently (e.g. differential mortality prior to transfer, severity of AMI). Because we had minimal data about this decision making process, we focused on the downstream effects after the transfer was made. Finally, the valid comparison of whether or not to transfer black and white patients requires ensuring that other differences between black and white patients have been accounted for. We were unable to fully adjust for potential differences in the presenting symptoms, underlying risk of poor outcome, comborbitidies, and treatment preferences between black and white patients. The observed differences in transfer timing may reflect delayed transfer of black patients who would benefit from early revascularization or earlier transfer of white patients who subsequently received inappropriate revascularization. Subsequent analyses addressing our research questions should better address these limitations.
Conclusions
We determined that black patients who present to non-revascularization hospitals with AMI are transferred to revascularization hospitals more slowly than white patients. This delay operates particularly at the hospital level because black patients are more likely to be admitted to hospitals with greater delays in transfer. These results suggest that an important mechanism for population-level racial disparities may be that hospitals that disproportionally care for black patients may perpetuate racial differences in AMI treatment.
Supplementary Material
Acknowledgments
Funding source: This work was supported in part by the Robert Wood Johnson Foundation Clinical Scholars Program (Dr. Cooke) and the National Institutes of Health (K08 HL091249)
Footnotes
List of Supplemental Digital Content
Supplemental digital content.doc
References
- 1.Agency for Healthcare Research and Quality . 2009 National Healthcare Disparities Report. U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality; Rockville, MD: Mar, 2010. AHRQ Pub. No. 10-0004. [Google Scholar]
- 2.Canto JG, Allison JJ, Kiefe CI, et al. Relation of race and sex to the use of reperfusion therapy in Medicare beneficiaries with acute myocardial infarction. N Engl J Med. 2000;342:1094–1100. doi: 10.1056/NEJM200004133421505. [DOI] [PubMed] [Google Scholar]
- 3.Conigliaro J, Whittle J, Good CB, et al. Understanding racial variation in the use of coronary revascularization procedures: the role of clinical factors. Arch Intern Med. 2000;160:1329–1335. doi: 10.1001/archinte.160.9.1329. [DOI] [PubMed] [Google Scholar]
- 4.Ford E, Newman J, Deosaransingh K. Racial and ethnic differences in the use of cardiovascular procedures: findings from the California Cooperative Cardiovascular Project. Am J Public Health. 2000;90:1128–1134. doi: 10.2105/ajph.90.7.1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kressin NR, Petersen LA. Racial differences in the use of invasive cardiovascular procedures: review of the literature and prescription for future research. Ann Intern Med. 2001;135:352–366. doi: 10.7326/0003-4819-135-5-200109040-00012. [DOI] [PubMed] [Google Scholar]
- 6.Smedley BD, Stith AY, Nelson AR, Institute of Medicine (U.S.) Unequal treatment : confronting racial and ethnic disparities in health care. National Academy Press; Washington, D.C.: 2003. Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. p. xvi.p. 764. [PubMed] [Google Scholar]
- 7.Barnato AE, Lucas FL, Staiger D, et al. Hospital-level racial disparities in acute myocardial infarction treatment and outcomes. Med Care. 2005;43:308–319. doi: 10.1097/01.mlr.0000156848.62086.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sonel AF, Good CB, Mulgund J, et al. Racial variations in treatment and outcomes of black and white patients with high-risk non-ST-elevation acute coronary syndromes: insights from CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the ACC/AHA Guidelines?). Circulation. 2005;111:1225–1232. doi: 10.1161/01.CIR.0000157732.03358.64. [DOI] [PubMed] [Google Scholar]
- 9.Popescu I, Vaughan-Sarrazin MS, Rosenthal GE. Certificate of need regulations and use of coronary revascularization after acute myocardial infarction. Jama. 2006;295:2141–2147. doi: 10.1001/jama.295.18.2141. [DOI] [PubMed] [Google Scholar]
- 10.Peterson ED, Shah BR, Parsons L, et al. Trends in quality of care for patients with acute myocardial infarction in the National Registry of Myocardial Infarction from 1990 to 2006. Am Heart J. 2008;156:1045–1055. doi: 10.1016/j.ahj.2008.07.028. [DOI] [PubMed] [Google Scholar]
- 11.Bradley EH, Herrin J, Wang Y, et al. Racial and ethnic differences in time to acute reperfusion therapy for patients hospitalized with myocardial infarction. Jama. 2004;292:1563–1572. doi: 10.1001/jama.292.13.1563. [DOI] [PubMed] [Google Scholar]
- 12.Trivedi AN, Zaslavsky AM, Schneider EC, Ayanian JZ. Relationship between quality of care and racial disparities in Medicare health plans. Jama. 2006;296:1998–2004. doi: 10.1001/jama.296.16.1998. [DOI] [PubMed] [Google Scholar]
- 13.Popescu I, Nallamothu BK, Vaughan-Sarrazin MS, Cram P. Racial differences in admissions to high-quality hospitals for coronary heart disease. Arch Intern Med. 2010;170:1209–1215. doi: 10.1001/archinternmed.2010.227. [DOI] [PubMed] [Google Scholar]
- 14.Sarrazin MS, Campbell ME, Richardson KK, Rosenthal GE. Racial segregation and disparities in health care delivery: conceptual model and empirical assessment. Health Serv Res. 2009;44:1424–1444. doi: 10.1111/j.1475-6773.2009.00977.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Skinner J, Chandra A, Staiger D, et al. Mortality after acute myocardial infarction in hospitals that disproportionately treat black patients. Circulation. 2005;112:2634–2641. doi: 10.1161/CIRCULATIONAHA.105.543231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Iwashyna TJ, Kahn JM, Hayward RA, Nallamothu BK. Interhospital transfers among Medicare beneficiaries admitted for acute myocardial infarction at nonrevascularization hospitals. Circ Cardiovasc Qual Outcomes. 2010;3:468–475. doi: 10.1161/CIRCOUTCOMES.110.957993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kushner FG, Hand M, Smith SC, Jr., et al. 2009 Focused Updates: ACC/AHA Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction (updating the 2004 Guideline and 2007 Focused Update) and ACC/AHA/SCAI Guidelines on Percutaneous Coronary Intervention (updating the 2005 Guideline and 2007 Focused Update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2009;120:2271–2306. doi: 10.1161/CIRCULATIONAHA.109.192663. [DOI] [PubMed] [Google Scholar]
- 18.Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non ST-Elevation Myocardial Infarction): developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons: endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. Circulation. 2007;116:e148–304. doi: 10.1161/CIRCULATIONAHA.107.181940. [DOI] [PubMed] [Google Scholar]
- 19.Nallamothu BK, Lu X, Vaughan-Sarrazin MS, Cram P. Coronary revascularization at specialty cardiac hospitals and peer general hospitals in black Medicare beneficiaries. Circ Cardiovasc Qual Outcomes. 2008;1:116–122. doi: 10.1161/CIRCOUTCOMES.108.800086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Blustein J, Arons RR, Shea S. Sequential events contributing to variations in cardiac revascularization rates. Med Care. 1995;33:864–880. doi: 10.1097/00005650-199508000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Gurwitz JH, Goldberg RJ, Malmgren JA, et al. Hospital transfer of patients with acute myocardial infarction: the effects of age, race, and insurance type. Am J Med. 2002;112:528–534. doi: 10.1016/s0002-9343(02)01072-0. [DOI] [PubMed] [Google Scholar]
- 22.Popescu I, Vaughan-Sarrazin MS, Rosenthal GE. Differences in mortality and use of revascularization in black and white patients with acute MI admitted to hospitals with and without revascularization services. Jama. 2007;297:2489–2495. doi: 10.1001/jama.297.22.2489. [DOI] [PubMed] [Google Scholar]
- 23.Roe MT, Chen AY, Delong ER, et al. Patterns of transfer for patients with non-ST-segment elevation acute coronary syndrome from community to tertiary care hospitals. Am Heart J. 2008;156:185–192. doi: 10.1016/j.ahj.2008.01.033. [DOI] [PubMed] [Google Scholar]
- 24.Magid DJ, Calonge BN, Rumsfeld JS, et al. Relation between hospital primary angioplasty volume and mortality for patients with acute MI treated with primary angioplasty vs thrombolytic therapy. Jama. 2000;284:3131–3138. doi: 10.1001/jama.284.24.3131. [DOI] [PubMed] [Google Scholar]
- 25.Nallamothu BK, Young J, Gurm HS, et al. Recent trends in hospital utilization for acute myocardial infarction and coronary revascularization in the United States. Am J Cardiol. 2007;99:749–753. doi: 10.1016/j.amjcard.2006.10.029. [DOI] [PubMed] [Google Scholar]
- 26.Kutcher MA, Klein LW, Ou FS, et al. Percutaneous coronary interventions in facilities without cardiac surgery on site: a report from the National Cardiovascular Data Registry (NCDR). J Am Coll Cardiol. 2009;54:16–24. doi: 10.1016/j.jacc.2009.03.038. [DOI] [PubMed] [Google Scholar]
- 27.Iwashyna TJ, Christie JD, Kahn JM, Asch DA. Uncharted paths: hospital networks in critical care. Chest. 2009;135:827–833. doi: 10.1378/chest.08-1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Iwashyna TJ, Christie JD, Moody J, et al. The structure of critical care transfer networks. Med Care. 2009;47:787–793. doi: 10.1097/MLR.0b013e318197b1f5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.American Hospital Association . American Hospital Association Annual Survey Database for Fiscal Year 2005. American Hospital Association; Chicago: 2005. [Google Scholar]
- 30.Waldo DP. Accuracy and bias of race/ethnicity codes in the Medicare enrollment database. Health Care Finan. Rev. 2004;26:61–72. [PMC free article] [PubMed] [Google Scholar]
- 31.U.S. Department of Health and Human Services Hospital Compare. www.hospitalcompare.hhs.gov.
- 32.Krumholz HM, Wang Y, Mattera JA, et al. An administrative claims model suitable for profiling hospital performance based on 30-day mortality rates among patients with heart failure. Circulation. 2006;113:1693–1701. doi: 10.1161/CIRCULATIONAHA.105.611194. [DOI] [PubMed] [Google Scholar]
- 33.Krumholz HM, Normand SL. Public reporting of 30-day mortality for patients hospitalized with acute myocardial infarction and heart failure. Circulation. 2008;118:1394–1397. doi: 10.1161/CIRCULATIONAHA.108.804880. [DOI] [PubMed] [Google Scholar]
- 34.Lumley T, Diehr P, Emerson S, Chen L. The importance of the normality assumption in large public health data sets. Annu Rev Public Health. 2002;23:151–169. doi: 10.1146/annurev.publhealth.23.100901.140546. [DOI] [PubMed] [Google Scholar]
- 35.Berlin JA, Kimmel SE, Ten Have TR, Sammel MD. An empirical comparison of several clustered data approaches under confounding due to cluster effects in the analysis of complications of coronary angioplasty. Biometrics. 1999;55:470–476. doi: 10.1111/j.0006-341x.1999.00470.x. [DOI] [PubMed] [Google Scholar]
- 36.Barnato AE, Berhane Z, Weissfeld LA, et al. Racial variation in end-of-life intensive care use: a race or hospital effect? Health Serv Res. 2006;41:2219–2237. doi: 10.1111/j.1475-6773.2006.00598.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hasnain-Wynia R, Baker DW, Nerenz D, et al. Disparities in health care are driven by where minority patients seek care: examination of the hospital quality alliance measures. Arch Intern Med. 2007;167:1233–1239. doi: 10.1001/archinte.167.12.1233. [DOI] [PubMed] [Google Scholar]
- 38.Lucas FL, Stukel TA, Morris AM, et al. Race and surgical mortality in the United States. Ann Surg. 2006;243:281–286. doi: 10.1097/01.sla.0000197560.92456.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sarrazin MV, Campbell M, Rosenthal GE. Racial differences in hospital use after acute myocardial infarction: does residential segregation play a role? Health Aff (Millwood) 2009;28:w368–378. doi: 10.1377/hlthaff.28.2.w368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cooke CR, Kahn JM. Deconstructing racial and ethnic disparities in critical care. Crit Care Med. 2010;38:978–980. doi: 10.1097/CCM.0b013e3181cc15d3. [DOI] [PubMed] [Google Scholar]
- 41.Jha AK, Orav EJ, Li Z, Epstein AM. Concentration and quality of hospitals that care for elderly black patients. Arch Intern Med. 2007;167:1177–1182. doi: 10.1001/archinte.167.11.1177. [DOI] [PubMed] [Google Scholar]
- 42.Amarasingham R, Plantinga L, Diener-West M, et al. Clinical information technologies and inpatient outcomes: a multiple hospital study. Arch Intern Med. 2009;169:108–114. doi: 10.1001/archinternmed.2008.520. [DOI] [PubMed] [Google Scholar]
- 43.Lyon SM, Benson NM, Iwashyna TJ, et al. The Effect Of Health Insurance On Intensive Care Mortality And Procedural Utilization [abstract]. Am J Respir Crit Care Med. 2010;181:A5344. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.